Septic History Limits the Outcome of Tibiotalocalcaneal Arthrodesis
Abstract
1. Introduction
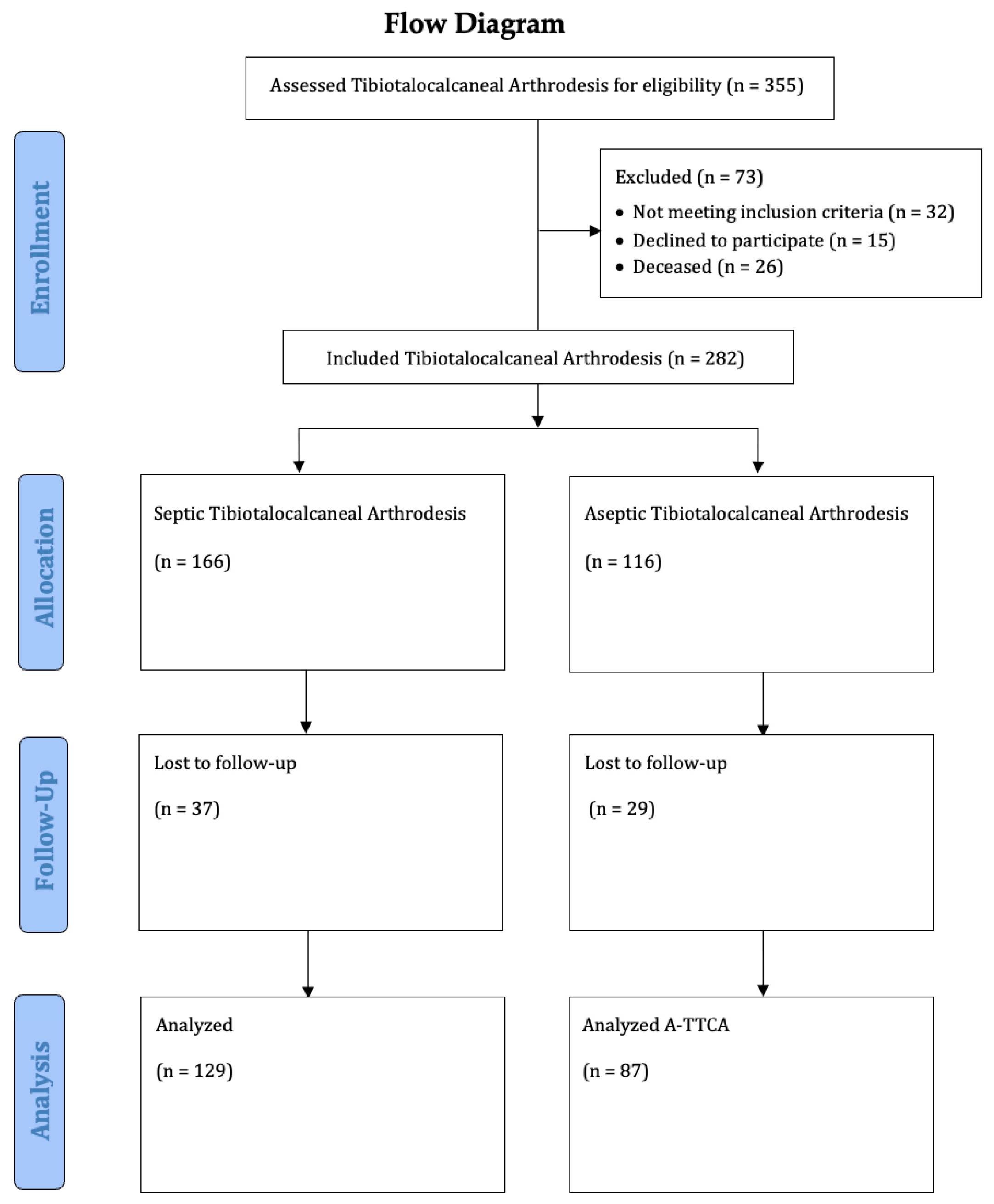
2. Patients and Methods
2.1. Population
2.2. Inclusion and Exclusion Criteria
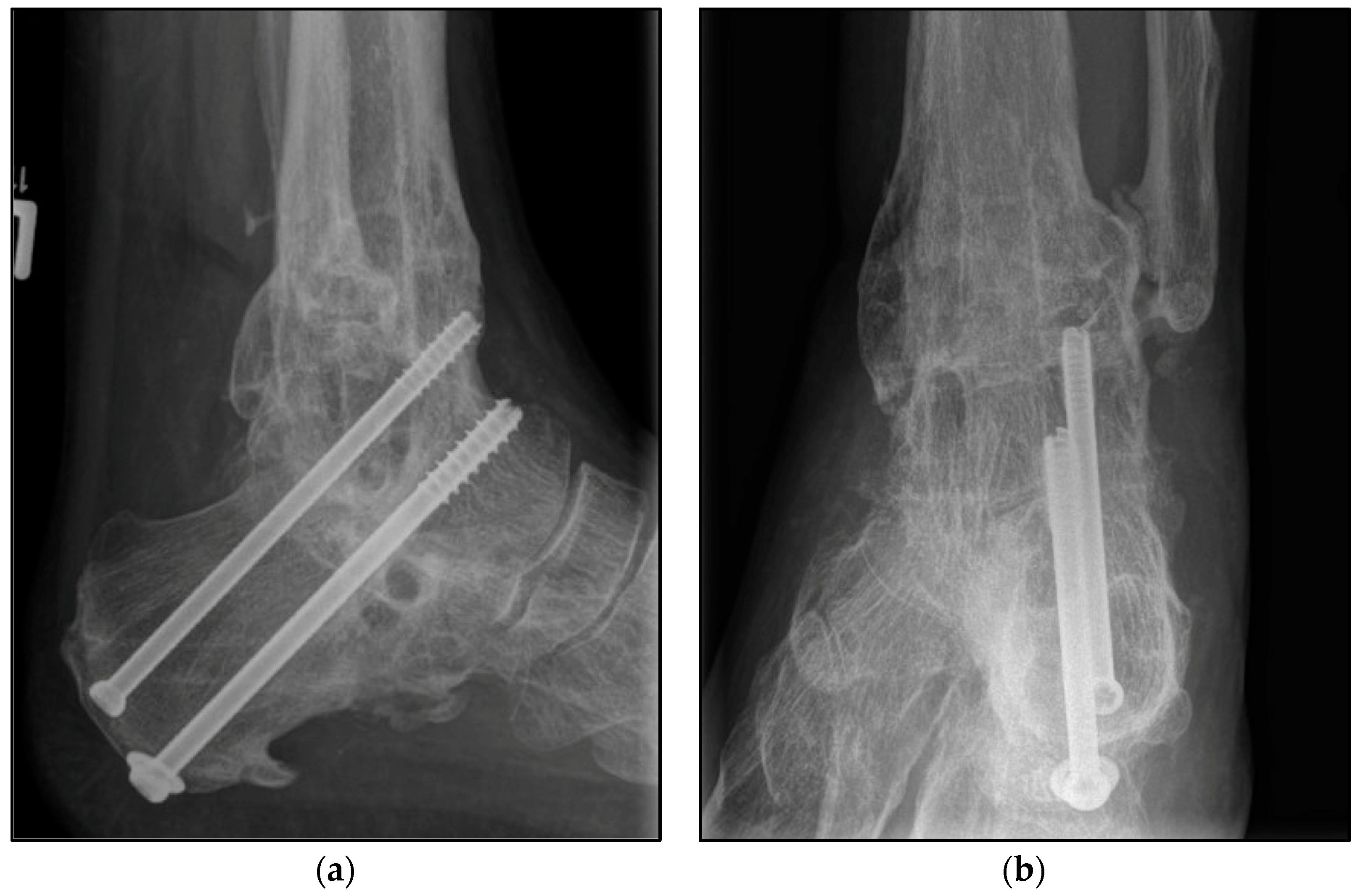
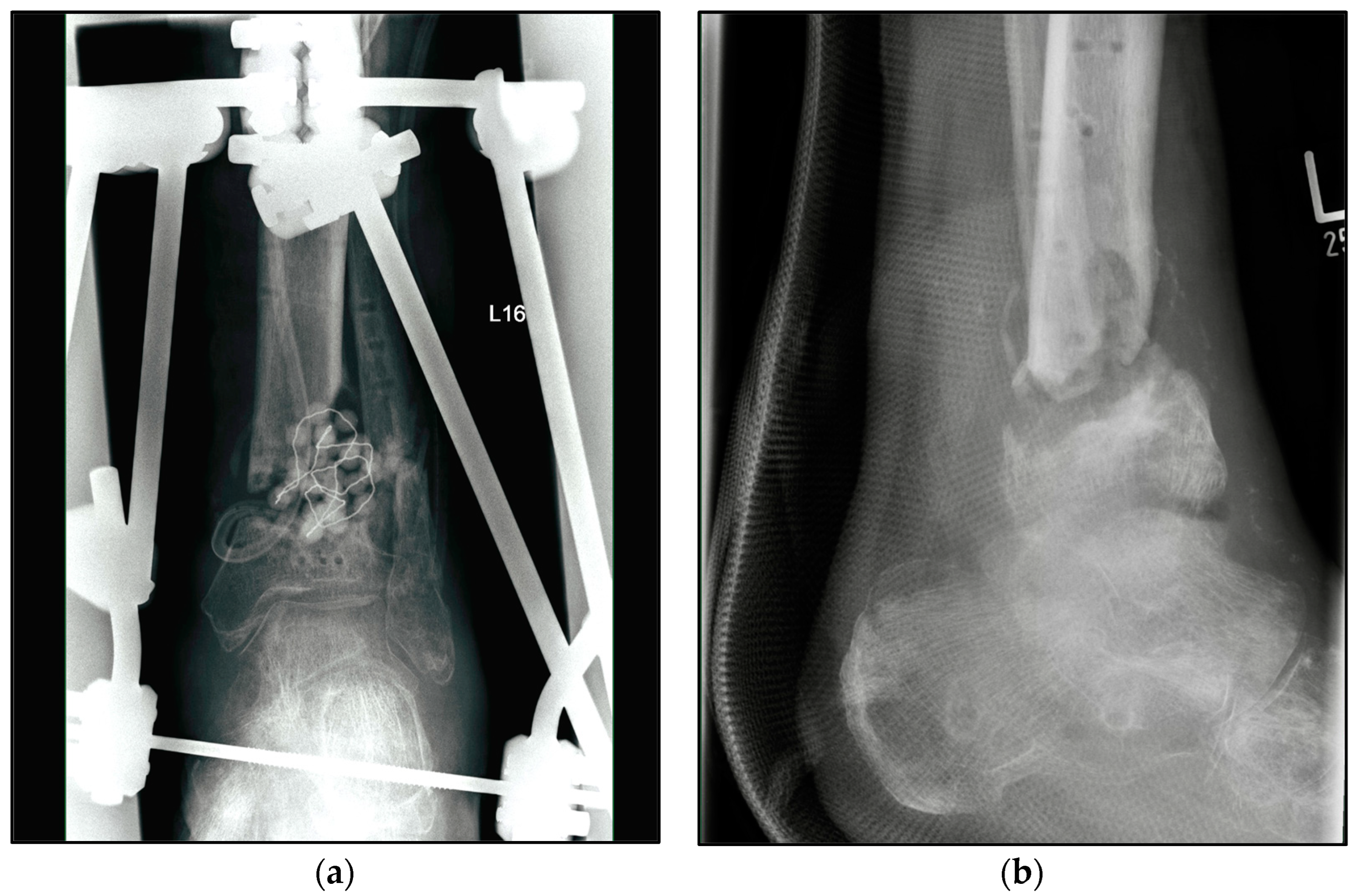
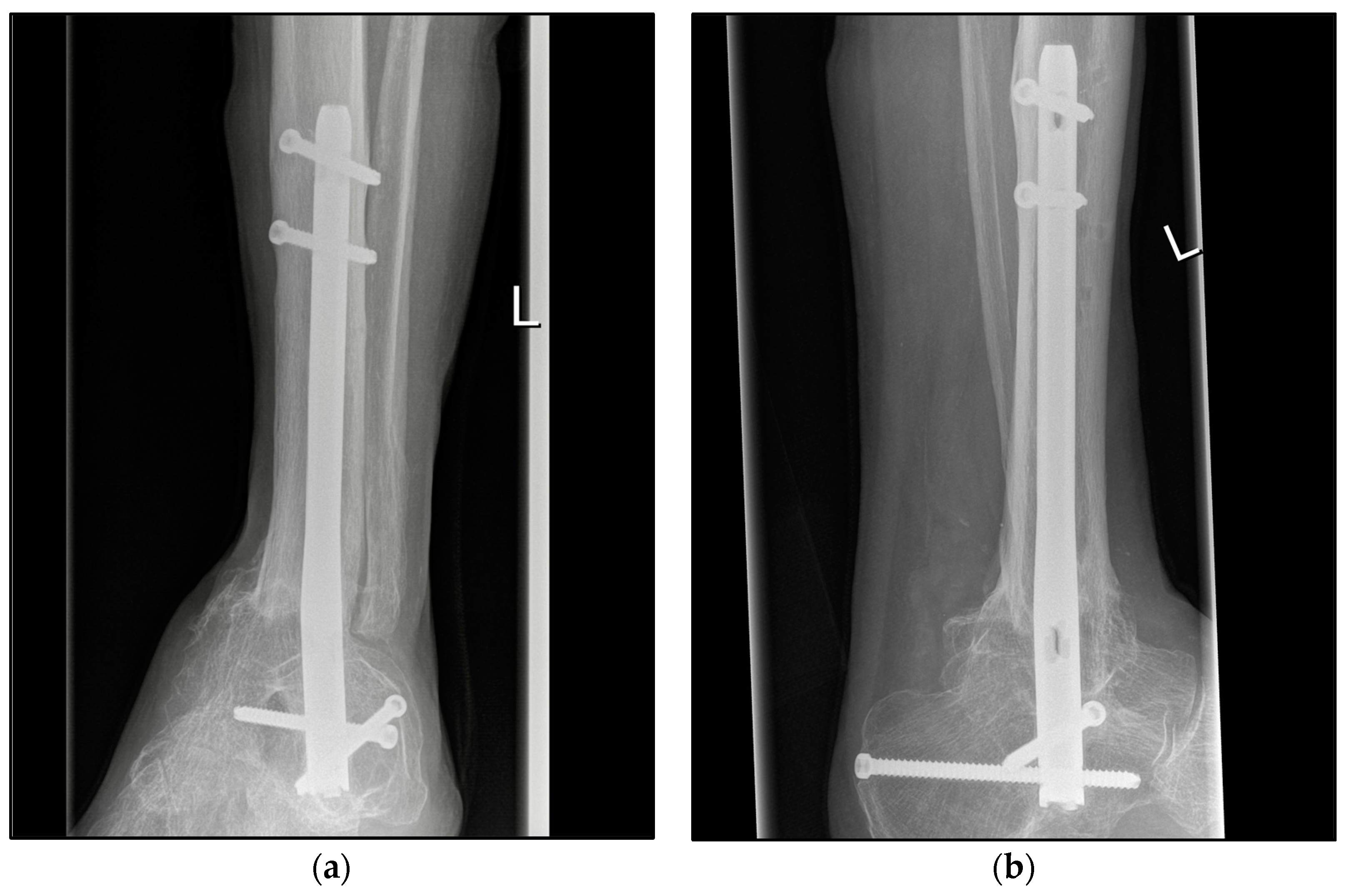
2.3. Surgical Procedure
2.4. Rehabilitation Protocol
2.5. Assessment Methods
2.6. Statistical Analysis
3. Results
Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Horisberger, M.; Valderrabano, V.; Hintermann, B. Posttraumatic ankle osteoarthritis after ankle-related fractures. J. Orthop. Trauma 2009, 23, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Klug, A.; Faul, P.; Hoffmann, R.; Manegold, S.; Gramlich, Y. Superiority of upper ankle arthrodesis over total ankle replacement in the treatment of end-stage posttraumatic ankle arthrosis. Arch. Orthop. Trauma Surg. 2022, 142, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, C.L.; Salamon, M.L.; Blanchard, G.M.; Huff, T.; Hayes, A.; Buckwalter, J.A.; Amendola, A. Epidemiology of ankle arthritis: Report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop. J. 2005, 25, 44–46. [Google Scholar] [PubMed]
- Valderrabano, V.; Horisberger, M.; Russell, I.; Dougall, H.; Hintermann, B. Etiology of ankle osteoarthritis. Clin. Orthop. Relat. Res. 2009, 467, 1800–1806. [Google Scholar] [CrossRef]
- Cibura, C.; Lotzien, S.; Yilmaz, E.; Baecker, H.; Schildhauer, T.A.; Gessmann, J. Simultaneous septic arthrodesis of the tibiotalar and subtalar joints with the Ilizarov external fixator-an analysis of 13 patients. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1063–1070. [Google Scholar] [CrossRef]
- Easley, M.E.; Montijo, H.E.; Wilson, J.B.; Fitch, R.D.; Nunley, J.A., 2nd. Revision tibiotalar arthrodesis. J. Bone Jt. Surg. Am. 2008, 90, 1212–1223. [Google Scholar] [CrossRef]
- Gross, J.B.; Belleville, R.; Nespola, A.; Poircuitte, J.M.; Coudane, H.; Mainard, D.; Galois, L. Influencing factors of functional result and bone union in tibiotalocalcaneal arthrodesis with intramedullary locking nail: A retrospective series of 30 cases. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 627–633. [Google Scholar] [CrossRef]
- Kappler, C.; Staubach, R.; Abdulazim, A.; Kemmerer, M.; Walter, G.; Hoffmann, R. Hindfoot arthrodesis for post-infectious ankle destruction using an intramedullary retrograde hindfoot nail. Unfallchirurg 2014, 117, 348–354. [Google Scholar] [CrossRef]
- Wang, S.; Li, B.; Yu, X.; Wu, H.; Liu, L. Is Ankle Arthrodesis With an Ilizarov External Fixator an Effective Treatment for Septic Ankle Arthritis? A Study With a Minimum of 6 Years of Follow-up. Clin. Orthop. Relat. Res. 2023, 481, 717–725. [Google Scholar] [CrossRef]
- Suda, A.J.; Richter, A.; Abou-Nouar, G.; Jazzazi, M.; Tinelli, M.; Bischel, O.E. Arthrodesis for septic arthritis of the ankle: Risk factors and complications. Arch. Orthop. Trauma Surg. 2016, 136, 1343–1348. [Google Scholar] [CrossRef]
- Rosen, A.B.; Jaffri, A.; Mitchell, A.; Koldenhoven, R.M.; Powden, C.J.; Fraser, J.J.; Simon, J.E.; Hoch, M.; Burcal, C.J. Association of Ankle Sprain Frequency With Body Mass and Self-Reported Function: A Pooled Multisite Analysis. J. Sport Rehabil. 2022, 31, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Vuurberg, G.; Altink, N.; Rajai, M.; Blankevoort, L.; Kerkhoffs, G. Weight, BMI and stability are risk factors associated with lateral ankle sprains and chronic ankle instability: A meta-analysis. J. ISAKOS 2019, 4, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Cullen, P.; Möller, H.; Woodward, M.; Senserrick, T.; Boufous, S.; Rogers, K.; Brown, J.; Ivers, R. Are there sex differences in crash and crash-related injury between men and women? A 13-year cohort study of young drivers in Australia. SSM Popul. Health 2021, 14, 100816. [Google Scholar] [CrossRef] [PubMed]
- Simske, N.M.; Audet, M.A.; Kim, C.Y.; Vallier, H.A. Open ankle fractures are associated with complications and reoperations. OTA Int. 2019, 2, e042. [Google Scholar] [CrossRef] [PubMed]
- Ovaska, M.T.; Madanat, R.; Honkamaa, M.; Makinen, T.J. Contemporary demographics and complications of patients treated for open ankle fractures. Injury 2015, 46, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
- Bugler, K.E.; Clement, N.D.; Duckworth, A.D.; White, T.O.; McQueen, M.M.; Court-Brown, C.M. Open ankle fractures: Who gets them and why? Arch. Orthop. Trauma Surg. 2015, 135, 297–303. [Google Scholar] [CrossRef]
- Herrera-Pérez, M.; González-Martín, D.; Vallejo-Márquez, M.; Godoy-Santos, A.L.; Valderrabano, V.; Tejero, S. Ankle Osteoarthritis Aetiology. J. Clin. Med. 2021, 10, 4489. [Google Scholar] [CrossRef]
- Klouche, S.; El-Masri, F.; Graff, W.; Mamoudy, P. Arthrodesis with internal fixation of the infected ankle. J. Foot Ankle Surg. 2011, 50, 25–30. [Google Scholar] [CrossRef]
- Gaedke, I.E.; Wiebking, U.; O’Loughlin, P.F.; Krettek, C.; Gaulke, R. Clinical and Radiological Mid- to Long-term Outcomes Following Ankle Fusion. In Vivo 2018, 32, 1463–1471. [Google Scholar] [CrossRef]
- Frey, C.; Halikus, N.M.; Vu-Rose, T.; Ebramzadeh, E. A Review of Ankle Arthrodesis: Predisposing Factors to Nonunion. Foot Ankle Int. 1994, 15, 581–584. [Google Scholar] [CrossRef]
- Zak, L.; Wozasek, G.E. Tibio-talo-calcaneal fusion after limb salvage procedures-A retrospective study. Injury 2017, 48, 1684–1688. [Google Scholar] [CrossRef]
- Klaue, K.; Wichelhaus, A.; Maik, P.; Mittlmeier, T. The circular arc shaped nail for fixing the tibiotalocalcaneal arthrodesis. After clinical results. Injury 2019, 50 (Suppl. S3), 23–31. [Google Scholar] [CrossRef] [PubMed]
- Popelka, S.; Vavrik, P.; Landor, I.; Bek, J.; Popelka ml, S.; Hromadka, R. [Tibio-talo-calcaneal arthrodesis with the retrograde intramedullary nail MEDIN]. Acta Chir. Orthop. Traumatol. Cech. 2013, 80, 400–406. [Google Scholar]
- Rüschenschmidt, M.; Glombitza, M.; Dahmen, J.; Hax, P.-M.; Lefering, R.; Steinhausen, E. External versus internal fixation for arthrodesis of chronic ankle joint infections—A comparative retrospective study. Foot Ankle Surg. 2020, 26, 398–404. [Google Scholar] [CrossRef]
- Jeng, C.; Campbell, J.; Tang, E.; Cerrato, R.; Myerson, M. Tibiotalocalcaneal Arthrodesis With Bulk Femoral Head Allograft for Salvage of Large Defects in the Ankle. Foot Ankle Int. Am. Orthop. Foot Ankle Soc. Swiss Foot Ankle Soc. 2013, 34, 1256–1266. [Google Scholar] [CrossRef]
- Lee, T.Y.; Wu, C.C.; Yang, K.C.; Yeh, K.T.; Chen, I.H.; Wang, C.C. Midterm outcomes of midfoot and hindfoot arthrodesis with strut allograft for Muller-Weiss disease. BMC Musculoskelet. Disord. 2022, 23, 715. [Google Scholar] [CrossRef]
- Fuchs, S.; Sandmann, C.; Skwara, A.; Chylarecki, C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J. Bone Jt. Surg. Br. 2003, 85, 994–998. [Google Scholar] [CrossRef]
- Jonas, S.C.; Young, A.F.; Curwen, C.H.; McCann, P.A. Functional outcome following tibio-talar-calcaneal nailing for unstable osteoporotic ankle fractures. Injury 2013, 44, 994–997. [Google Scholar] [CrossRef]
- Georgiannos, D.; Lampridis, V.; Bisbinas, I. Fragility fractures of the ankle in the elderly: Open reduction and internal fixation versus tibio-talo-calcaneal nailing: Short-term results of a prospective randomized-controlled study. Injury 2017, 48, 519–524. [Google Scholar] [CrossRef]
| Characteristic | Septic TTCA (n = 129) | Aseptic TTCA (n = 87) | All (n = 216) | p | |
|---|---|---|---|---|---|
| Follow-up (months) | Mean | 85.10 | 68.87 | 78.61 | 0.003 |
| SEM | 3.36 | 4.42 | 2.73 | ||
| Minimum | 18.00 | 12.00 | 12.00 | ||
| Maximum | 154.00 | 151.00 | 154.00 | ||
| Age, years | Mean | 63.59 | 64.68 | 64.02 | 0.528 |
| SEM | 1.02 | 1.47 | 0.85 | ||
| Minimum | 27.00 | 30.00 | 27.00 | ||
| Maximum | 89.00 | 93.00 | 93.00 | ||
| BMI, kg/m2 | Mean | 30.34 | 29.95 | 30.18 | 0.660 |
| SEM | 0.56 | 0.68 | 0.43 | ||
| Minimum | 16.40 | 18.80 | 16.40 | ||
| Maximum | 58.30 | 49.60 | 58.30 | ||
| Sex, n (%) | Male | 84 (65.12) | 51 (58.62) | 135 (62.50) | 0.336 |
| Female | 45 (34.88) | 36 (41.38) | 81 (37.50) | ||
| Affected side, n (%) | Left | 67 (51.94) | 44 (50.58) | 111 (51.39) | 0.845 |
| Right | 62 (48.06) | 43 (49.42) | 105 (48.61) | ||
| Smoker, n (%) | Yes | 34 (26.36) | 17 (19.54) | 51 (23.61) | 0.266 |
| No | 92 (71.32) | 67 (77.01) | 159 (73.61) | ||
| n.a. | 3 (2.33) | 3 (3.45) | 6 (2.78) | ||
| Pre-existing conditions (multiple answers), n (%) | Metabolic-syndrome-associated | 52 (41.27) | 30 (35.71) | 82 (37.96) | 0.063 |
| Rheumatism | 7 (5.43) | 3 (3.45) | 10 (4.63) | ||
| Others | 25 (19.38) | 19 (21.84) | 44 (20.37) | ||
| None | 30 (23.26) | 15 (17.24) | 45 (20.83) |
| Predisposing Factors, Multiple Answers | Septic TTCA (n = 129) | Aseptic TTCA (n = 87) | All (n = 216) | p | |
|---|---|---|---|---|---|
| Mechanism, n (%) | Fall from height | 43 (33.33) | 26 (29.89) | 69 (31.94) | 0.697 |
| Distortion | 29 (22.48) | 14 (16.09) | 43 (19.91) | ||
| Traffic accident | 30 (23.26) | 21 (24.14) | 51 (23.61) | ||
| Others | 26 (20.63) | 26 (29.89) | 52 (24.07) | ||
| Ankle fracture, n (%) | Yes | 43 (33.33) | 25 (28.74) | 68 (31.48) | 0.478 |
| No | 86 (66.67) | 62 (71.27) | 148 (68.52) | ||
| Talar fracture, n (%) | Yes | 6 (4.65) | 18 (20.70) | 24 (11.11) | 0.001 |
| No | 123 (95.35) | 69 (79.30) | 192 (88.89) | ||
| Tibial plafond fractures, n (%) | Yes | 47 (36.43) | 5 (5.75) | 52 (24.08) | 0.001 |
| No | 82 (63.57) | 82 (94.25) | 164 (75.92) | ||
| Open fracture, n (%) | Yes | 32 (24.81) | 7 (8.05) | 39 (18.06) | <0.001 |
| No | 97 (75.19) | 80 (91.95) | 177 (81.94) | ||
| Gustilo Grade I | 2 (1.55) | 0 (0.00) | 2 (0.93) | ||
| Gustilo Grade II | 12 (9.30) | 3 (3.45) | 15 (6.94) | ||
| Gustilo Grade III | 18 (13.95) | 4 (4.59) | 22 (10.19) | ||
| Delayed union tibial, n (%) | Yes | 58 (44.96) | 17 (19.54) | 75 (34.72) | <0.001 |
| No | 71 (55.04) | 70 (80.46) | 141 (65.28) | ||
| Chronic ankle instability, n (%) | Yes | 8 (6.20) | 7 (8.05) | 15 (6.94) | 0.603 |
| No | 121 (93.80) | 80 (91.95) | 201 (93.06) | ||
| Chronic syndesmotic instability, n (%) | Yes | 4 (3.10) | 6 (6.90) | 10 (4.63) | 0.120 |
| No | 125 (96.90) | 81 (93.10) | 206 (95.37) | ||
| Failed total ankle replacement, n (%) | Yes | 17 (13.18) | 12 (13.79) | 29 (13.43) | 0.897 |
| No | 112 (86.82) | 75 (86.21) | 187 (86.57) | ||
| Deformities of the lower limb, n (%) | Valgus deformity | 1 (0.78) | 9 (10.35) | 10 (4.63) | <0.001 |
| Varus deformity | 6 (4.65) | 23 (26.44) | 29 (13.43) | <0.001 | |
| No | 122 (94.57) | 55 (63.21) | 177 (81.94) | <0.001 | |
| Previous neurological disease, n (%) | Yes | 4 (3.10) | 6 (6.90) | 10 (4.63) | 0.195 |
| No | 125 (96.90) | 81 (93.10) | 206 (95.37) | ||
| Primary arthrosis, n (%) | Yes | 3 (2.33) | 6 (6.90) | 9 (4.17) | 0.100 |
| No | 126 (97.67) | 81 (93.10) | 207 (95.83) | ||
| Others, n (%) | Yes | 23 (17.83) | 14 (16.01) | 37 (17.13) | 0.735 |
| No | 106 (82.17) | 73 (83.99) | 179 (82.87) |
| Measurements | Septic TTCA (n = 129) | Aseptic TTCA (n = 87) | All (n = 216) | p | |
|---|---|---|---|---|---|
| Olerud and Molander | Mean | 39.40 | 48.39 | 43.00 | 0.008 |
| SEM | 2.08 | 2.72 | 1.68 | ||
| Minimum | 0.00 | 0.00 | 0.00 | ||
| Maximum | 100.00 | 85.00 | 100.00 | ||
| FFI-D | Mean | 81.62 | 69.23 | 76.64 | 0.002 |
| SEM | 2.49 | 3.11 | 1.98 | ||
| Minimum | 19.50 | 15.00 | 15.00 | ||
| Maximum | 135.00 | 123.00 | 135.00 | ||
| SF-12 (physical component summary) | Mean | 34.09 | 37.66 | 35.52 | 0.019 |
| SEM | 0.96 | 1.14 | 35.52 | ||
| Minimum | 11.73 | 14.47 | 0.75 | ||
| Maximum | 55.26 | 56.63 | 11.73 | ||
| SF-12 (mental component summary) | Mean | 49.91 | 50.36 | 50.09 | 0.783 |
| SEM | 1.11 | 1.19 | 0.814 | ||
| Minimum | 17.10 | 22.84 | 17.10 | ||
| Maximum | 68.89 | 65.23 | 68.89 | ||
| Number of operations underwent until union, including fracture treatment, n | Mean | 11.23 | 3.83 | 8.29 | <0.001 |
| Minimum | 1 | 1 | 1 | ||
| Maximum | 30 | 25 | 30 | ||
| Complication, revision surgery needed until union (multiple answers), n (%) * | Yes | - | 14 (16.09) | ||
| No | - | 73 (83.91) | |||
| Nonunion | - | 8 (9.19) | |||
| Implant irritation | - | 5 (5.74) | |||
| TTS | - | 1 (1.15) | |||
| Footwear (multiple answers), n (%) | Orthotic insoles only | 23 (17.83) | 18 (20.69) | 41 (18.98) | 0.012 |
| Shoe adaption | 72 (55.81) | 34 (39.08) | 106 (49.07) | <0.001 | |
| Other | 2 (1.59) | 1 (1.19) | 3 (1.39) | 0.281 | |
| Nothing special | 29 (22.48) | 31 (35.63) | 60 (27.78) | <0.001 | |
| Return to learned profession, n (%) | Yes | 18 (13.95) | 16 (18.39) | 34 (15.74) | 0.802 |
| Permanently unable to work, n (%) | Yes | 52 (41.27) | 15 (17.86) | 67 (31.02) | <0.001 |
| Retraining, part time, and pension, n (%) | Yes | 56 (44.44) | 53 (63.09) | 109 (50.46) | 0.802 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meinert, M.; Colcuc, C.; Herrmann, E.; Harbering, J.; Gramlich, Y.; Blank, M.; Hoffmann, R.; Fischer, S. Septic History Limits the Outcome of Tibiotalocalcaneal Arthrodesis. J. Clin. Med. 2023, 12, 3422. https://doi.org/10.3390/jcm12103422
Meinert M, Colcuc C, Herrmann E, Harbering J, Gramlich Y, Blank M, Hoffmann R, Fischer S. Septic History Limits the Outcome of Tibiotalocalcaneal Arthrodesis. Journal of Clinical Medicine. 2023; 12(10):3422. https://doi.org/10.3390/jcm12103422
Chicago/Turabian StyleMeinert, Magalie, Christian Colcuc, Eva Herrmann, Johannes Harbering, Yves Gramlich, Marc Blank, Reinhard Hoffmann, and Sebastian Fischer. 2023. "Septic History Limits the Outcome of Tibiotalocalcaneal Arthrodesis" Journal of Clinical Medicine 12, no. 10: 3422. https://doi.org/10.3390/jcm12103422
APA StyleMeinert, M., Colcuc, C., Herrmann, E., Harbering, J., Gramlich, Y., Blank, M., Hoffmann, R., & Fischer, S. (2023). Septic History Limits the Outcome of Tibiotalocalcaneal Arthrodesis. Journal of Clinical Medicine, 12(10), 3422. https://doi.org/10.3390/jcm12103422








