Prognostic Factors in Staged Bilateral Total Knee Arthroplasty—A Retrospective Case Series Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Methods
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of Total Hip and Knee Replacement in the United States. J. Bone Jt. Surg. Am. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Bedard, N.A.; Elkins, J.M.; Brown, T.S. Effect of COVID-19 on Hip and Knee Arthroplasty Surgical Volume in the United States. J. Arthroplast. 2020, 35, S45–S48. [Google Scholar] [CrossRef]
- Gademan, M.G.; Hofstede, S.N.; Vliet Vlieland, T.P.; Nelissen, R.G.; de Mheen, P.J.M.-v. Indication criteria for total hip or knee arthroplasty in osteoarthritis: A state-of-the-science overview. BMC Musculoskelet. Disord. 2016, 17, 463. [Google Scholar] [CrossRef] [PubMed]
- Price, A.J.; Alvand, A.; Troelsen, A.; Katz, J.N.; Hooper, G.; Gray, A.; Carr, A.; Beard, D. Knee replacement. Lancet 2018, 392, 1672–1682. [Google Scholar] [CrossRef]
- Chen, F.; Li, R.; Lall, A.; Schwechter, E.M. Primary Total Knee Arthroplasty for Distal Femur Fractures: A Systematic Review of Indications, Implants, Techniques, and Results. Am. J. Orthop. 2017, 46, E163–E171. [Google Scholar]
- Wang, S.; Zhang, Y.; Li, J. Clinical application of unicompartmental knee arthroplasty and total knee arthroplasty in patient with bilateral knee osteoarthritis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2020, 34, 1568–1573. [Google Scholar] [CrossRef]
- Liu, L.; Liu, H.; Zhang, H.; Song, J.; Zhang, L. Bilateral total knee arthroplasty: Simultaneous or staged? A systematic review and meta-analysis. Medicine 2019, 98, e15931. [Google Scholar] [CrossRef]
- Warren, J.A.; Siddiqi, A.; Krebs, V.E.; Molloy, R.; Higuera, C.A.; Piuzzi, N.S. Bilateral Simultaneous Total Knee Arthroplasty May Not Be Safe Even in the Healthiest Patients. J. Bone Jt. Surg. Am. 2021, 103, 303–311. [Google Scholar] [CrossRef]
- Obaid-ur-Rahman; Hafeez, S.; Amin, M.S.; Ameen, J.; Adnan, R. Unilateral versus simultaneous bilateral total knee arthro-plasty: A comparative study. J. Pak. Med. Assoc. 2021, 71 (Suppl. S5), S21–S25. [Google Scholar]
- Grace, T.R.; Tsay, E.L.; Roberts, H.J.; Vail, T.P.; Ward, D.T. Staged Bilateral Total Knee Arthroplasty: Increased Risk of Recurring Complications. J. Bone Jt. Surg. Am. 2020, 102, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Iqbal, Z.A.; Anwer, S.; Anwar, D. Comparison of simultaneous bilateral versus unilateral total knee re-placement on pain levels and functional recovery. BMC Musculoskelet. Disord. 2020, 21, 246. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Lo, N.N.; Jiang, L.; Chong, H.C.; Tay, D.K.; Chin, P.L.; Chia, S.L.; Yeo, S.J. Simultaneous versus staged bilateral unicom-partmental knee replacement. Bone Jt. J. 2013, 95-B, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Pfeil, J.; Hohle, P.; Rehbein, P. Bilateral endoprosthetic total hip or knee arthroplasty. Dtsch. Arztebl. Int. 2011, 108, 463–468. [Google Scholar] [CrossRef]
- Kim, Y.H.; Choi, Y.W.; Kim, J.S. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J. Bone Jt. Surg. Br. 2009, 91, 64–68. [Google Scholar] [CrossRef]
- Memtsoudis, S.G.; Ma, Y.; Chiu, Y.L.; Poultsides, L.; Gonzalez Della Valle, A.; Mazumdar, M. Bilateral total knee arthroplasty: Risk factors for major morbidity and mortality. Anesth. Analg. 2011, 113, 784–790. [Google Scholar] [CrossRef]
- Scott, C.E.; Murray, R.C.; MacDonald, D.J.; Biant, L.C. Staged bilateral total knee replacement: Changes in expectations and outcomes between the first and second operations. Bone Jt. J. 2014, 96-B, 752–758. [Google Scholar] [CrossRef]
- Ahd, J.H.; Kang, D.M.; Choi, K.J. Bilateral simultaneous unicompartmental knee arthroplasty versus unilateral total knee arthroplasty: A comparison of the amount of blood loss and transfusion, perioperative complications, hospital stay, and functional recovery. Orthop. Traumatol. Surg. Res. 2017, 103, 1041–1045. [Google Scholar] [CrossRef]
- Rovňák, M.; Hrubina, M.; Šiarnik, P.; Sýkora, J.; Melišík, M.; Nečas, L. Bilateral versus unilateral total knee replacement-comparison of clinical and functional results in two-year follow-up. Rozhl. Chir. 2022, 101, 278–283. [Google Scholar] [CrossRef]
- Fabi, D.W.; Mohan, V.; Goldstein, W.M.; Dunn, J.H.; Murphy, B.P. Unilateral vs. bilateral total knee arthroplasty risk factors increasing morbidity. J. Arthroplast. 2011, 26, 668–673. [Google Scholar] [CrossRef]
- Gill, S.D.; Hatton, A.; de Steiger, R.; Page, R.S. One-Surgeon vs. Two-Surgeon Single-Anesthetic Bilateral Total Knee Arthro-plasty: Revision and Mortality Rates From the Australian Orthopedic Association National Joint Replacement Regis-try. J. Arthroplast. 2020, 35, 1852–1856. [Google Scholar] [CrossRef] [PubMed]
- Kazubski, K.; Tomczyk, Ł.; Ciszewski, M.; Witkowski, J.; Reichert, P.; Morasiewicz, P. The Symmetry and Predictive Factors in Two-Stage Bilateral Hip Replacement Procedures. Symmetry 2021, 13, 1472. [Google Scholar] [CrossRef]
- De Luca, M.L.; Ciccarello, M.; Martorana, M.; Infantino, D.; Letizia Mauro, G.; Bonarelli, S.; Benedetti, M.G. Pain monitoring and management in a rehabilitation setting after total joint replacement. Medicine 2018, 97, e12484. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.T.; Mufarrih, S.H.; Ali, A.; Noordin, S. Predictors of an increased length of stay following Total Knee Arthroplasty-Survey Report. J. Pak. Med. Assoc. 2019, 69, 1159–1163. [Google Scholar] [PubMed]
- Halawi, M.J.; Vovos, T.J.; Green, C.L.; Wellman, S.S.; Attarian, D.E.; Bolognesi, M.P. Preoperative predictors of extended hospital length of stay following total knee arthroplasty. J. Arthroplast. 2015, 30, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Xia, C.; Li, Q.; Yao, C.; Yao, Y.; Chen, D.; Jiang, Q. Perioperative predictors of prolonged length of hospital stay following total knee arthroplasty: A retrospective study from a single center in China. BMC Musculoskelet. Disord. 2020, 21, 62. [Google Scholar] [CrossRef] [PubMed]
| Variable Mean ± Standard Deviation | First Operation | Second Operation | p-Value |
|---|---|---|---|
| Duration of hospital stay [days] | 6.43 ± 1.98 | 5.5 ± 1.69 | 0.211 * |
| Time of anesthesia during surgery [minutes] | 117.04 ± 9.23 | 118.06 ± 8.29 | 0.457 * |
| Femur implant size | 5.43 ± 1.46 | 5.2 ± 1.28 | 0.54 * |
| Tibia implant size | 5.36 ± 1.55 | 5.25 ± 1.52 | 0.382 * |
| Tibial polyethylene insert size | 9.45 ± 0.66 | 9.34 ± 0.61 | 0.422 * |
| Number of complications per patient | 0.13 ± 0.34 | 0.06 ± 0.25 | 0.371 * |
| Variable | Correlation Coefficient | p-Value * |
|---|---|---|
| Duration of hospital stay [days] | 0.281 | 0.0640 |
| Time of anesthesia during surgery [minutes] | 0.464 | 0.0014 |
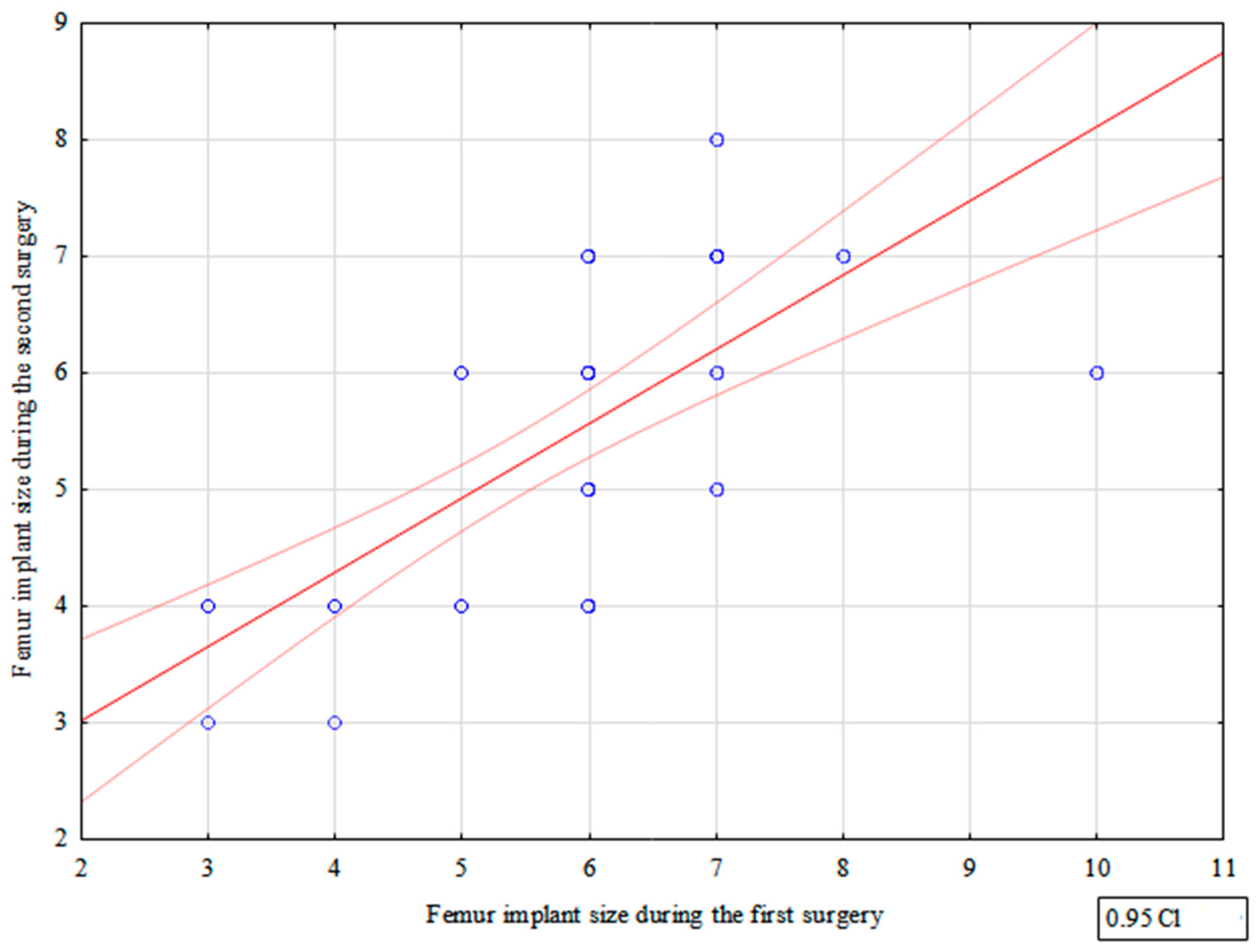
| Femur implant size | 0.790 | p < 0.0001 |
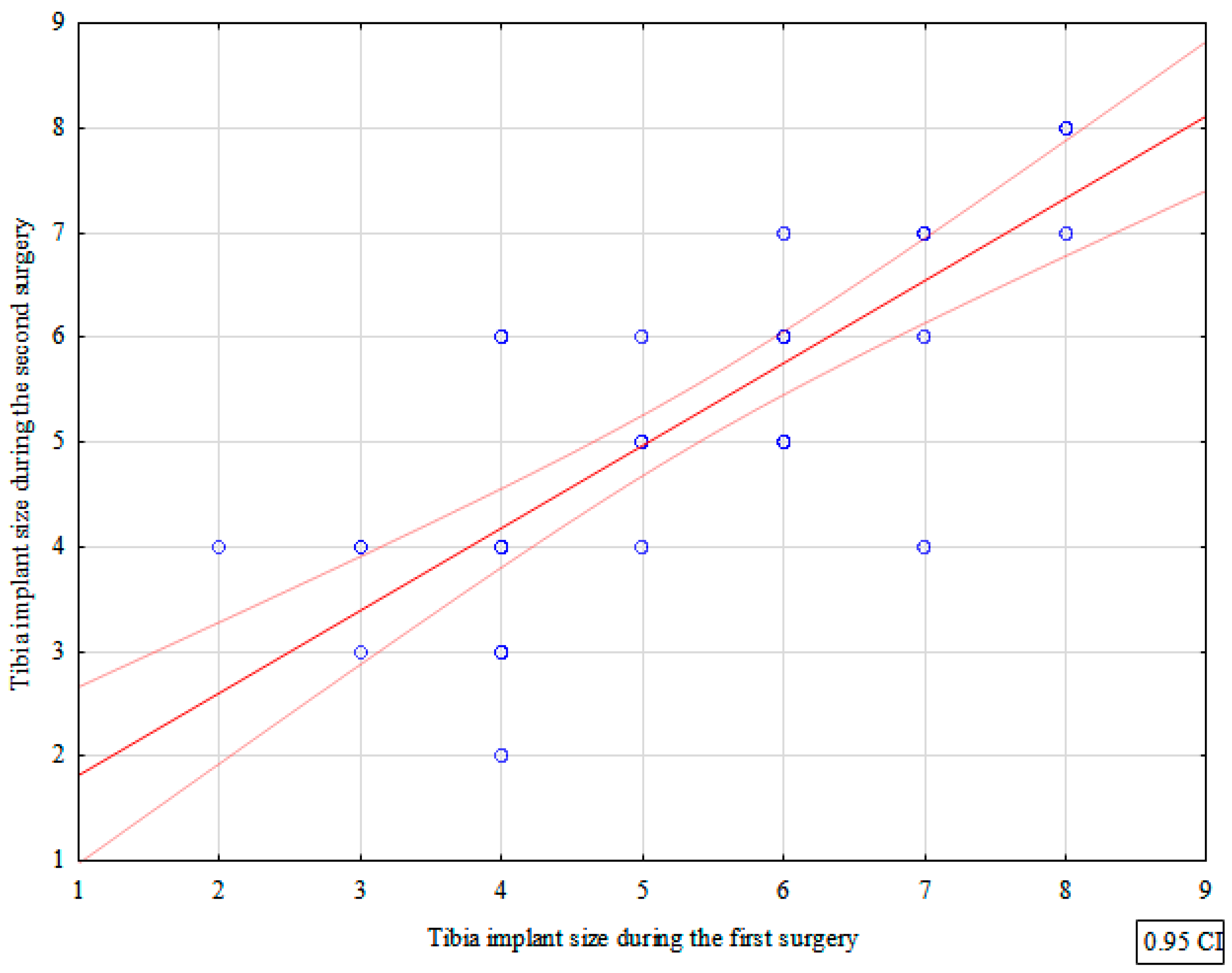
| Tibia implant size | 0.820 | p < 0.0001 |
| Tibial polyethylene insert size | 0.379 | 0.0109 |
| Number of complications per patient | 0.418 | 0.0047 |
| Patient Number | Duration of Hospital Stay [Days] | Femur Implant Size | Tibia Implant Size | Tibial Polyethylene Insert Size | Time of Anesthesia during Surgery [Minutes] | Complications | Order of Surgery | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Surgery | Second Surgery | First Surgery | Second Surgery | First Surgery | Second Surgery | First Surgery | Second Surgery | First Surgery | Second Surgery | First Surgery | Second Surgery | First | Second | |
| 1 | 10 | 7 | 7 | 6 | 7 | 6 | 11 | 9 | 135 | 140 | 1 | 0 | R | L |
| 2 | 10 | 10 | 10 | 6 | 7 | 7 | 10 | 9 | 155 | 130 | 1 | 1 | R | L |
| 3 | 7 | 4 | 6 | 6 | 7 | 7 | 9 | 9 | 120 | 115 | 0 | 0 | R | L |
| 4 | 6 | 5 | 6 | 6 | 7 | 7 | 9 | 9 | 115 | 110 | 0 | 0 | R | L |
| 5 | 5 | 4 | 6 | 7 | 6 | 7 | 9 | 9 | 115 | 120 | 0 | 0 | R | L |
| 6 | 7 | 4 | 3 | 4 | 2 | 4 | 10 | 9 | 105 | 130 | 0 | 0 | R | L |
| 7 | 12 | 10 | 6 | 7 | 4 | 6 | 10 | 10 | 130 | 130 | 1 | 1 | R | L |
| 8 | 5 | 6 | 5 | 4 | 5 | 4 | 9 | 9 | 110 | 110 | 0 | 0 | R | L |
| 9 | 6 | 7 | 8 | 7 | 8 | 7 | 9 | 10 | 110 | 110 | 0 | 0 | R | L |
| 10 | 4 | 4 | 3 | 4 | 4 | 4 | 9 | 9 | 100 | 110 | 0 | 0 | R | L |
| 11 | 4 | 5 | 6 | 6 | 6 | 6 | 9 | 9 | 120 | 120 | 0 | 0 | R | L |
| 12 | 7 | 4 | 6 | 6 | 6 | 5 | 9 | 9 | 110 | 110 | 0 | 0 | R | L |
| 13 | 10 | 7 | 6 | 4 | 3 | 3 | 10 | 9 | 120 | 125 | 1 | 0 | R | L |
| 14 | 9 | 7 | 5 | 4 | 5 | 5 | 9 | 9 | 110 | 115 | 1 | 0 | R | L |
| 15 | 5 | 6 | 4 | 3 | 4 | 4 | 10 | 9 | 115 | 110 | 0 | 0 | R | L |
| 16 | 6 | 7 | 6 | 5 | 6 | 5 | 10 | 11 | 110 | 120 | 0 | 0 | R | L |
| 17 | 5 | 6 | 7 | 7 | 6 | 6 | 9 | 9 | 115 | 120 | 0 | 0 | R | L |
| 18 | 8 | 4 | 4 | 4 | 4 | 4 | 10 | 10 | 110 | 115 | 0 | 0 | R | L |
| 19 | 6 | 4 | 6 | 6 | 7 | 7 | 9 | 9 | 115 | 120 | 0 | 0 | R | L |
| 20 | 4 | 5 | 6 | 6 | 6 | 5 | 9 | 9 | 110 | 110 | 0 | 0 | R | L |
| 21 | 5 | 6 | 4 | 4 | 4 | 3 | 9 | 9 | 110 | 120 | 0 | 0 | R | L |
| 22 | 8 | 6 | 3 | 4 | 4 | 3 | 9 | 9 | 115 | 110 | 0 | 0 | R | L |
| 23 | 7 | 5 | 7 | 7 | 8 | 8 | 10 | 9 | 110 | 120 | 0 | 0 | R | L |
| 24 | 6 | 7 | 6 | 5 | 6 | 5 | 11 | 10 | 115 | 120 | 0 | 0 | R | L |
| 25 | 5 | 6 | 7 | 7 | 6 | 6 | 9 | 9 | 120 | 120 | 0 | 0 | R | L |
| 26 | 8 | 4 | 4 | 4 | 6 | 6 | 9 | 9 | 115 | 115 | 0 | 0 | R | L |
| 27 | 6 | 4 | 6 | 6 | 7 | 7 | 10 | 10 | 120 | 120 | 0 | 0 | R | L |
| 28 | 4 | 5 | 6 | 6 | 7 | 7 | 9 | 9 | 115 | 115 | 0 | 0 | R | L |
| 29 | 7 | 6 | 3 | 4 | 3 | 4 | 9 | 9 | 110 | 110 | 0 | 0 | R | L |
| 30 | 8 | 4 | 4 | 4 | 3 | 4 | 9 | 11 | 120 | 120 | 0 | 0 | L | R |
| 31 | 7 | 8 | 7 | 8 | 8 | 8 | 11 | 9 | 120 | 140 | 0 | 0 | L | R |
| 32 | 5 | 5 | 4 | 4 | 4 | 4 | 11 | 11 | 120 | 140 | 0 | 0 | L | R |
| 33 | 7 | 9 | 5 | 6 | 5 | 5 | 9 | 9 | 110 | 115 | 0 | 1 | L | R |
| 34 | 4 | 6 | 3 | 3 | 4 | 2 | 9 | 9 | 130 | 110 | 0 | 0 | L | R |
| 35 | 3 | 5 | 7 | 5 | 7 | 7 | 9 | 10 | 110 | 110 | 0 | 0 | L | R |
| 36 | 9 | 4 | 6 | 6 | 6 | 6 | 9 | 9 | 130 | 120 | 1 | 0 | L | R |
| 37 | 6 | 4 | 6 | 4 | 7 | 4 | 10 | 9 | 120 | 110 | 0 | 0 | L | R |
| 38 | 7 | 4 | 6 | 6 | 5 | 5 | 9 | 9 | 130 | 120 | 0 | 0 | L | R |
| 39 | 5 | 4 | 4 | 4 | 3 | 4 | 10 | 10 | 110 | 110 | 0 | 0 | L | R |
| 40 | 8 | 6 | 5 | 4 | 4 | 6 | 9 | 10 | 120 | 115 | 0 | 0 | L | R |
| 41 | 8 | 7 | 5 | 6 | 6 | 6 | 10 | 10 | 115 | 120 | 0 | 0 | L | R |
| 42 | 4 | 5 | 5 | 6 | 5 | 6 | 9 | 9 | 115 | 110 | 0 | 0 | L | R |
| 43 | 5 | 3 | 5 | 4 | 4 | 3 | 9 | 9 | 120 | 115 | 0 | 0 | L | R |
| 44 | 5 | 3 | 5 | 4 | 4 | 3 | 9 | 9 | 120 | 120 | 0 | 0 | L | R |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazubski, K.; Tomczyk, Ł.; Bobiński, A.; Morasiewicz, P. Prognostic Factors in Staged Bilateral Total Knee Arthroplasty—A Retrospective Case Series Analysis. J. Clin. Med. 2023, 12, 3547. https://doi.org/10.3390/jcm12103547
Kazubski K, Tomczyk Ł, Bobiński A, Morasiewicz P. Prognostic Factors in Staged Bilateral Total Knee Arthroplasty—A Retrospective Case Series Analysis. Journal of Clinical Medicine. 2023; 12(10):3547. https://doi.org/10.3390/jcm12103547
Chicago/Turabian StyleKazubski, Krystian, Łukasz Tomczyk, Andrzej Bobiński, and Piotr Morasiewicz. 2023. "Prognostic Factors in Staged Bilateral Total Knee Arthroplasty—A Retrospective Case Series Analysis" Journal of Clinical Medicine 12, no. 10: 3547. https://doi.org/10.3390/jcm12103547
APA StyleKazubski, K., Tomczyk, Ł., Bobiński, A., & Morasiewicz, P. (2023). Prognostic Factors in Staged Bilateral Total Knee Arthroplasty—A Retrospective Case Series Analysis. Journal of Clinical Medicine, 12(10), 3547. https://doi.org/10.3390/jcm12103547







