Randomized Clinical Trial Evaluating AcceptME—A Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High Risk for Eating Disorders
Abstract
:1. Introduction
2. Materials and Methods
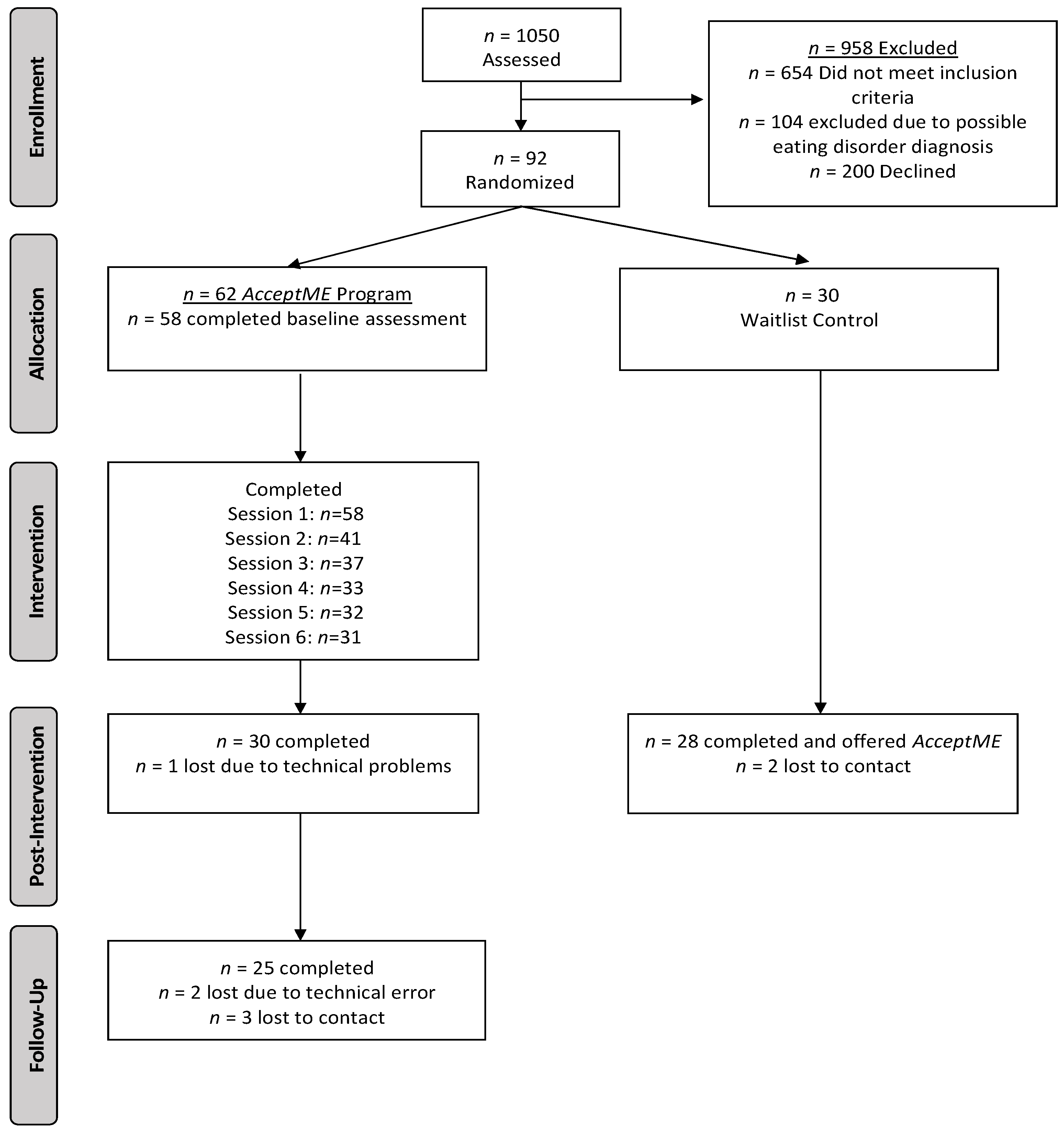
2.1. Participants
2.2. Procedure
AcceptME Program Description
2.3. Measures
Statistical Analyses
3. Results
3.1. Group Equivalence Prior to Intervention
3.2. Comparison of Outcome and Process Variable at Baseline between Program Completers and Non-Completers
3.3. Repeated Measures Analysis of Variance of Group by Time on Outcomes
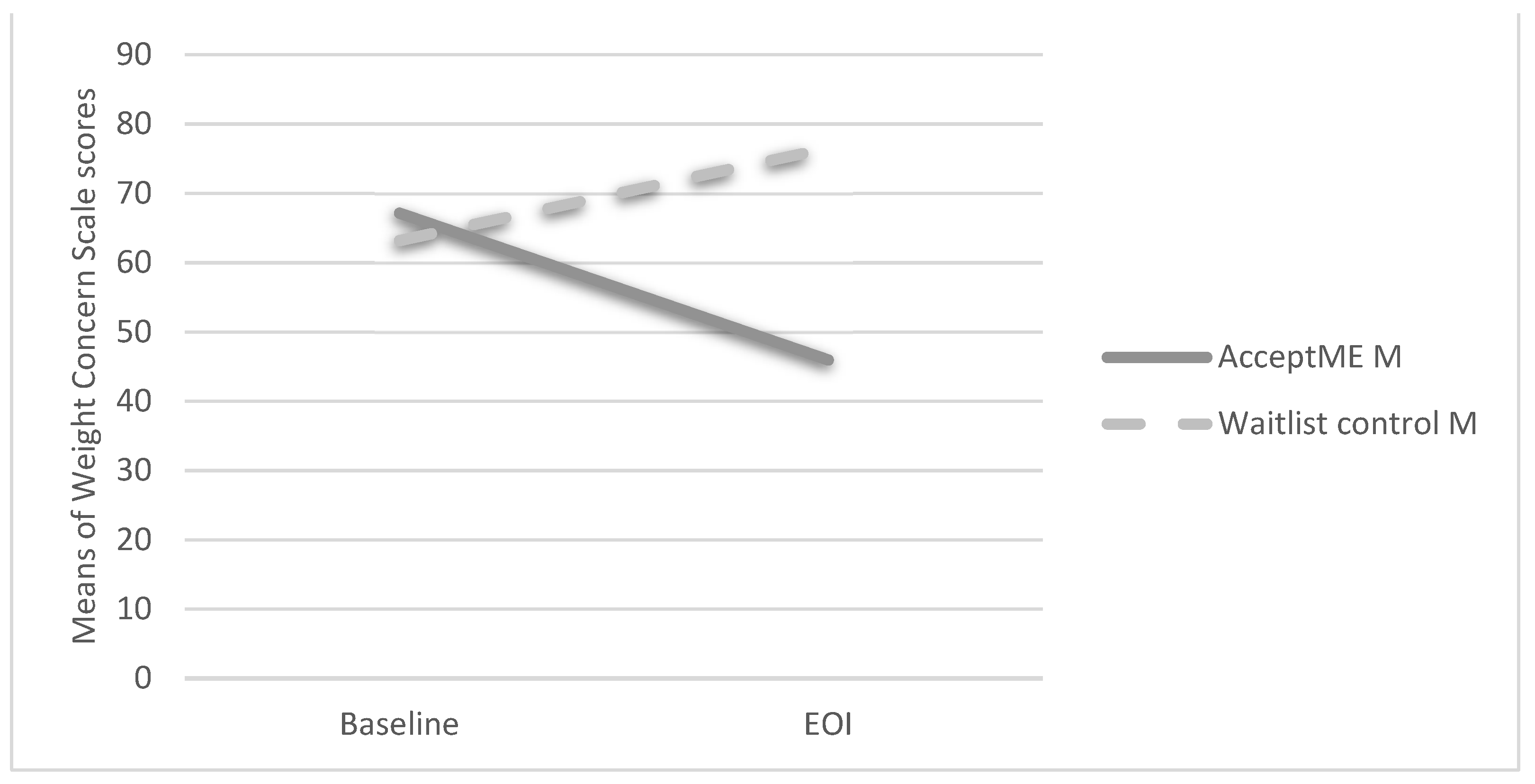
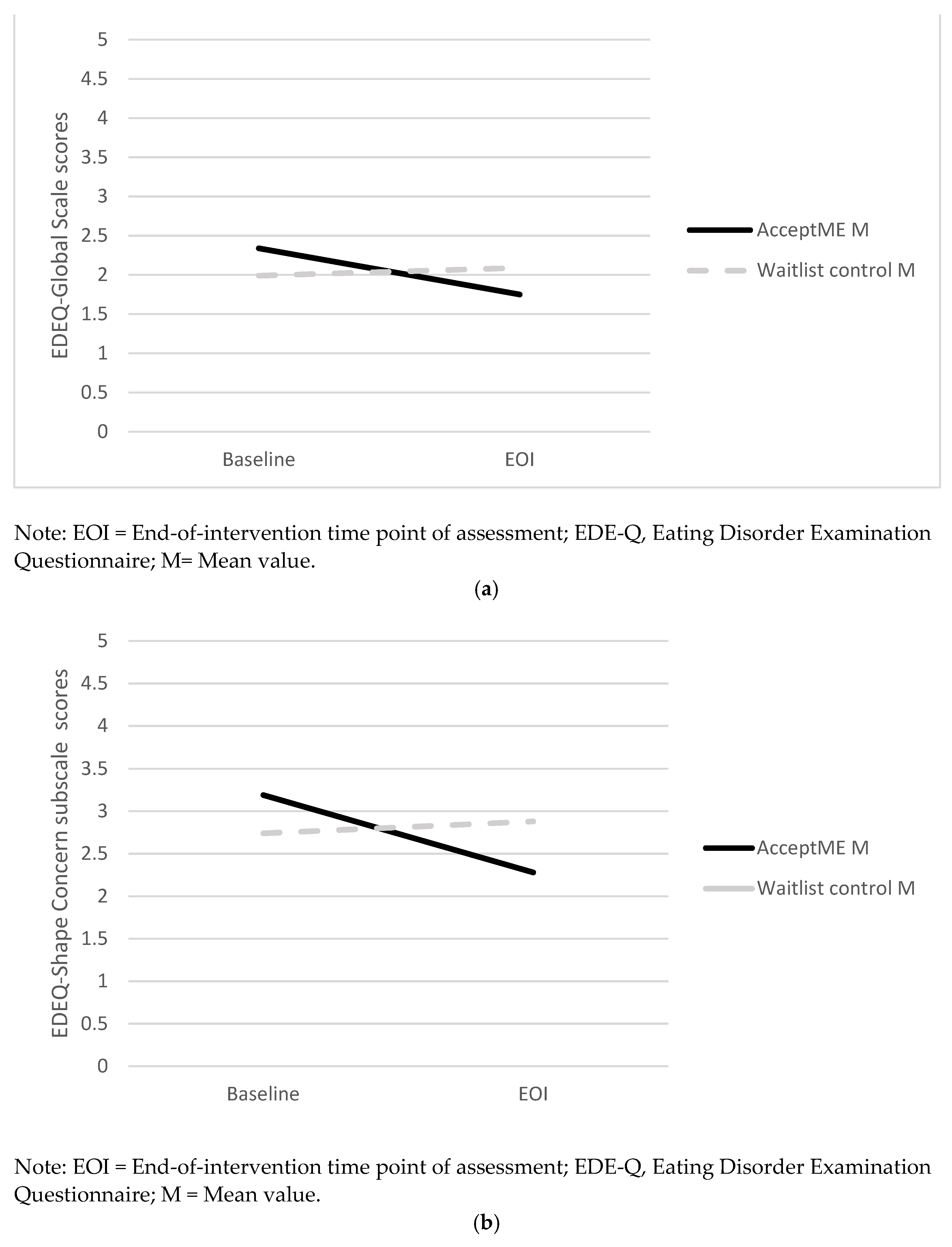
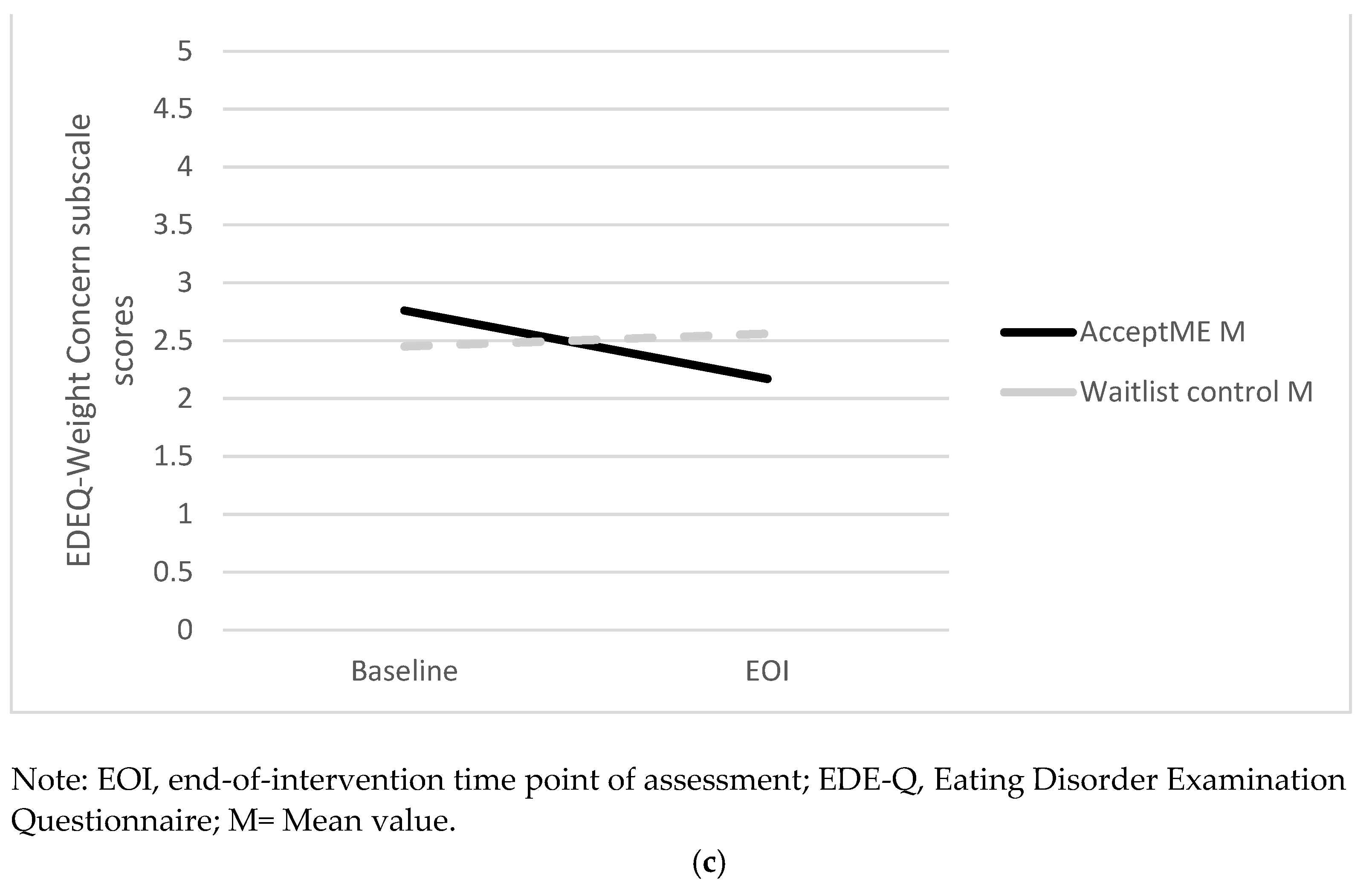
3.4. Analysis across Time (Baseline, EOI, 1-Month Follow-Up) for AcceptME Group Only
3.5. Odds Ratios for Meeting Criteria for at-Risk at EOI
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stice, E.; Becker, C.B.; Yokum, S. Eating disorder prevention: Current evidence-base and future directions. Int. J. Eat. Disord. 2013, 46, 478–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanderlinden, J. Many roads lead to Rome: Why does cognitive behavioural therapy remain unsuccessful for many eating disorder patients? Eur. Eat. Disord. Rev. 2008, 16, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Cooper, Z.; Doll, H.A.; O’Connor, M.E.; Palmer, R.L.; Dalle Grave, R. Enhanced cognitive behaviour therapy for adults with anorexia nervosa: A UK-Italy study. Behav. Res. Ther. 2013, 51, R2–R8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manlick, C.F.; Cochran, S.V.; Koon, J. Acceptance and commitment therapy for eating disorders: Rationale and literature review. J. Contemp. Psychother. 2013, 43, 115–122. [Google Scholar] [CrossRef]
- Merwin, R.M.; Timko, C.A.; Moskovich, A.A.; Ingle, K.K.; Bulik, C.M.; Zucker, N.L. Psychological inflexibility and Symptom Expression in Anorexia Nervosa. Eat. Disord. 2011, 19, 62–82. [Google Scholar] [CrossRef]
- Koushiou, M.; Nicolaou, K.; Karekla, M. Inducing negative affect using film clips with general and eating disorder-related content. Eat. Weight Disord. 2018, 23, 775–784. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: An Experimental Approach to Behavior Change; The Guilford Press: New York, NY, USA, 2011; ISBN 1572309555. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; The Guilford Press: New York, NY, USA, 2011; ISBN 978-1-60918-962-4 (Hardcover). 978-1-60918-964-8 (PDF). [Google Scholar]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and Commitment Therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Linardon, J.; Fairburn, C.G.; Fitzsimmons-Craft, E.E.; Wilfley, D.E.; Brennan, L. The empirical status of the third-wave behaviour therapies for the treatment of eating disorders: A systematic review. Clin. Psychol. Rev. 2017, 58, 125–140. [Google Scholar] [CrossRef]
- Linardon, J.; Gleeson, J.; Yap, K.; Murphy, K.; Brennan, L. Meta-analysis of the effects of third-wave behavioural interventions on disordered eating and body image concerns: Implications for eating disorder prevention. Cogn. Behav. Ther. 2019, 48, 15–38. [Google Scholar] [CrossRef]
- Linardon, J.; Shatte, A.; Messer, M.; Firth, J.; Fuller-Tyszkiewicz, M. E-mental health interventions for the treatment and prevention of eating disorders: An updated systematic review and meta-analysis. J. Consult. Clin. Psychol. 2020, 88, 994–1007. [Google Scholar] [CrossRef]
- Juarascio, A.; Shaw, J.; Forman, E.; Timko, C.A.; Herbert, J.; Butryn, M.; Bunnell, D.; Matteucci, A.; Lowe, M. Acceptance and Commitment Therapy as a Novel Treatment for Eating Disorders: An Initial Test of Efficacy and Mediation. Behav. Modif. 2013, 37, 459–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearson, A.N.; Follette, V.M.; Hayes, S.C. A Pilot Study of Acceptance and Commitment Therapy as a Workshop Intervention for Body Dissatisfaction and Disordered Eating Attitudes. Cogn. Behav. Pract. 2012, 19, 181–197. [Google Scholar] [CrossRef]
- Juarascio, A.S.; Forman, E.M.; Herbert, J.D. Acceptance and commitment therapy versus cognitive therapy for the treatment of comorbid eating pathology. Behav. Modif. 2010, 34, 175–190. [Google Scholar] [CrossRef] [PubMed]
- Timko, C.A.; Zucker, N.L.; Herbert, J.D.; Rodriguez, D.; Merwin, R.M. An open trial of Acceptance-based Separated Family Treatment (ASFT) for adolescents with anorexia nervosa. Behav. Res. Ther. 2015, 69, 63–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinto-Gouveia, J.; Carvalho, S.A.; Palmeira, L.; Castilho, P.; Duarte, C.; Ferreira, C.; Duarte, J.; Cunha, M.; Matos, M.; Costa, J. Incorporating psychoeducation, mindfulness and self-compassion in a new programme for binge eating (BEfree): Exploring processes of change. J. Health Psychol. 2019, 24, 466–479. [Google Scholar] [CrossRef]
- Fogelkvist, M.; Gustafsson, S.A.; Kjellin, L.; Parling, T. Acceptance and commitment therapy to reduce eating disorder symptoms and body image problems in patients with residual eating disorder symptoms: A randomized controlled trial. Body Image 2020, 32, 155–166. [Google Scholar] [CrossRef]
- Parling, T.; Cernvall, M.; Ramklint, M.; Holmgren, S.; Ghaderi, A. A randomised trial of Acceptance and Commitment Therapy for Anorexia Nervosa after daycare treatment, including five-year follow-up. BMC Psychiatry 2016, 16, 272. [Google Scholar] [CrossRef] [Green Version]
- Pellizzer, M.L.; Waller, G.; Wade, T.D. Body image flexibility: A predictor and moderator of outcome in transdiagnostic outpatient eating disorder treatment. Int. J. Eat. Disord. 2018, 51, 368–372. [Google Scholar] [CrossRef]
- Rogers, C.B.; Webb, J.B.; Jafari, N. A systematic review of the roles of body image flexibility as correlate, moderator, mediator, and in intervention science (2011–2018). Body Image 2018, 27, 43–60. [Google Scholar] [CrossRef]
- Stice, E.; Shaw, H.; Marti, C.N. A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annu. Rev. Clin. Psychol. 2007, 3, 207–231. [Google Scholar] [CrossRef]
- Hoek, H.W.; Van Hoeken, D. Review of the Prevalence and Incidence of Eating Disorders. Int. J. Eat. Disord. 2003, 34, 383–396. [Google Scholar] [CrossRef] [PubMed]
- Dölemeyer, R.; Tietjen, A.; Kersting, A.; Wagner, B. Internet-based interventions for eating disorders in adults: A systematic review. BMC Psychiatry 2013, 13, 207. [Google Scholar] [CrossRef] [Green Version]
- Newton, M.S.; Ciliska, D. Internet-based innovations for the prevention of eating disorders: A systematic review. Eat. Disord. 2006, 14, 365–384. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.; Ducharme, P.; Rotenberg, A.; Gonzalez-Heydrich, J. “rAGE-Control”: A Game to Build Emotional Strength. Games Health J. 2013, 2, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Deterding, S.; Dixon, D.; Khaled, R.; Nacke, L. From Game DESIGN elements to Gamefulness: Defining “Gamification”. In Proceedings of the 15th International Academic MindTrek Conference: Envisioning Future Media Environments, Tampere, Finland, 28–30 September 2011; pp. 9–15. [Google Scholar] [CrossRef]
- Karekla, M.; Nikolaou, P.; Merwin, R. Randomized Clinical Trial Evaluating a Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High-Risk for Eating Disorders. 2022. Available online: https://www.preprints.org/manuscript/202202.0228/v1 (accessed on 25 January 2022).
- Karekla, M.; Kasinopoulos, O.; Neto, D.D.; Ebert, D.D.; Van Daele, T.; Nordgreen, T.; Höfer, S.; Oeverland, S.; Jensen, K.L. Best Practices and Recommendations for Digital Interventions to Improve Engagement and Adherence in Chronic Illness Sufferers. Eur. Psychol. 2019, 24, 49–67. [Google Scholar] [CrossRef]
- Killen, J.D.; Hayward, C.H.; Haydel, F.; Wilson, D.; Hammer, L.; Kraemer, H.; Blair-Greiner, A.; Strachowski, D. Weight concerns influence the development of eating disorders. J. Consult. Clin. Psychol. 1996, 64, 936–940. [Google Scholar] [CrossRef]
- Stice, E.; Telch, C.F.; Rizvi, S.L. Development and validation of the eating disorder diagnostic scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol. Assess. 2000, 12, 123–131. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Norman, P.A.; Welch, S.L.; O’Connor, M.E.; Doll, H.A.; Peveler, R.C. A Prospective Study of Outcome in Bulimia Nervosa and the Long-term Effects of Three Psychological Treatments. Arch. Gen. Psychiatry 1995, 52, 304–312. [Google Scholar] [CrossRef]
- Rizvi, S.L.; Peterson, C.B.; Crow, S.J.; Agras, W.S. Test-retest reliability of the Eating Disorder Examination. Int. J. Eat. Disord. 2000, 28, 311–316. [Google Scholar] [CrossRef]
- Rosen, J.C.; Vara, L.; Wendt, S.; Leitenberg, H. Validity studies of the eating disorder examination. Int. J. Eat. Disord. 1990, 9, 519–528. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef]
- Juarascio, A.; Shaw, J.; Forman, E.M.; Timko, C.A.; Herbert, J.D.; Butryn, M.L.; Lowe, M. Acceptance and Commitment Therapy for eating disorders: Clinical applications of a group treatment. J. Context. Behav. Sci. 2013, 2, 85–94. [Google Scholar] [CrossRef]
- Patrick, D.L.; Edwards, T.C.; Topolski, T.D. Adolescent quality of life, part II: Initial validation of a new instrument. J. Adolesc. 2002, 25, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Cooper, P.J.; Taylor, M.J.; Cooper, Z.; Fairbum, C.G. The development and validation of the body shape questionnaire. Int. J. Eat. Disord. 1987, 6, 485–494. [Google Scholar] [CrossRef]
- Pook, M.; Tuschen-Caffier, B.; Brähler, E. Evaluation and comparison of different versions of the Body Shape Questionnaire. Psychiatry Res. 2008, 158, 67–73. [Google Scholar] [CrossRef]
- Welch, E.; Lagerström, M.; Ghaderi, A. Body Shape Questionnaire: Psychometric properties of the short version (BSQ-8C) and norms from the general Swedish population. Body Image 2012, 9, 547–550. [Google Scholar] [CrossRef]
- Sandoz, E.K.; Wilson, K.G.; Merwin, R.M.; Kate Kellum, K. Assessment of body image flexibility: The Body Image-Acceptance and Action Questionnaire. J. Context. Behav. Sci. 2013, 2, 39–48. [Google Scholar] [CrossRef]
- Karekla, M.; Mavraki, E.Z.; Nikolaou, P.; Koushiou, M. Validation of the Greek version of the body image-acceptance and action questionnaire. Eur. J. Couns. Psychol. 2020, 8, 93–107. [Google Scholar] [CrossRef]
- Rosen, J.C.; Srebnik, D.; Saltzberg, E.; Wendt, S. Development of a body image avoidance questionnaire—Consequences (body image avoiding behaviours). Psychol. Assess. 1991, 3, 32–37. [Google Scholar] [CrossRef]
- Atkinson, M.J.; Wade, T.D. Does mindfulness have potential in eating disorders prevention? A preliminary controlled trial with young adult women. Early Interv. Psychiatry 2016, 10, 234–245. [Google Scholar] [CrossRef]
- Jacobi, C.; Völker, U.; Trockel, M.T.; Taylor, C.B. Effects of an Internet-based intervention for subthreshold eating disorders: A randomized controlled trial. Behav. Res. Ther. 2012, 50, 93–99. [Google Scholar] [CrossRef]
- Kass, A.E.; Trockel, M.; Safer, D.L.; Sinton, M.M.; Cunning, D.; Rizk, M.T.; Genkin, B.H.; Weisman, H.L.; Bailey, J.O.; Jacobi, C.; et al. Internet-based preventive intervention for reducing eating disorder risk: A randomized controlled trial comparing guided with unguided self-help. Behav. Res. Ther. 2014, 63, 90–98. [Google Scholar] [CrossRef] [Green Version]
- Stice, E.; Rohde, P.; Shaw, H.; Gau, J.M. Clinician-led, peer-led, and internet-delivered dissonance-based eating disorder prevention programs: Acute effectiveness of these delivery modalities. J. Cons. Clin. 2017, 85, 883–895. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Rohde, P.; Shaw, H.; Gau, J.M. Clinician-led, peer-led, and internet-delivered dissonance-based eating disorder prevention programs: Effectiveness of these delivery modalities through 4-year follow-up. J. Cons. Clin. 2020, 88, 481–494. [Google Scholar] [CrossRef] [PubMed]
- Fitzsimmons-Craft, E.E.; Taylor, C.B.; Graham, A.K.; Sadeh-Sharvit, S.; Balantekin, K.N.; Eichen, D.M.; Monterubio, G.E.; Goel, N.J.; Flatt, R.E.; Karam, A.M.; et al. Effectiveness of a digital cognitive behavior therapy–guided self-help intervention for eating disorders in college women: A cluster randomized clinical trial. JAMA Netw. Open 2020, 3, e2015633. [Google Scholar] [CrossRef]
- Watson, H.; Joyce, T.; French, E.; Willan, V.; Kane, R.T.; Tanner-Smith, E.E.; McCormack, J.; Dawkins, H.; Hoiles, K.; Egan, S.J. Prevention of eating disorders: A systematic review of randomized, controlled trials. Int. J. Eat. Dis. 2016, 49, 833–862. [Google Scholar] [CrossRef] [PubMed]
- Bauer, S.; Moessner, M.; Wolf, M.; Haug, S.; Kordy, H. ES [S] PRIT—An internet-based programme for the prevention and early intervention of eating disorders in college students. Br. J. Guid. Couns. 2009, 37, 327–336. [Google Scholar] [CrossRef]
- Kindermann, S.; Moessner, M.; Ozer, F.; Bauer, S. Associations between eating disorder related symptoms and participants’ utilization of an individualized Internet-based prevention and early intervention program. Int. Eat. Dis. 2017, 50, 1215–1221. [Google Scholar] [CrossRef]
- Cotter, E.W.; Hornack, S.E.; Fotang, J.P.; Pettit, E.; Mirza, N.M. A pilot open-label feasibility trial examining an adjunctive mindfulness intervention for adolescents with obesity. Pilot Feasibility Stud. 2020, 6, 79. [Google Scholar] [CrossRef]
- Hoang, M.T.; Do, H.N.; Dang, T.Q.; Do, H.T.; Nguyen, T.T.; Nguyen, L.H.; Nguyen, C.T.; Doan, L.P.; Vu, G.T.; Van Ngo, T.; et al. Cross-cultural adaptation and measurement properties of Youth Quality of Life Instrument Short Form (YQOL-SF) in a developing South- East Asian country. PLoS ONE 2021, 16, e0253075. [Google Scholar] [CrossRef]
- Merwin, R.M.; Wilson, K. Understanding and Treating Eating Disorders: An ACT Perspective. In Acceptance and Commitment Therapy: Contemporary Theory, Research, and Practice; Australian Academic Press: Sydney, Australia, 2009; pp. 87–117. ISBN 9781921513145. [Google Scholar]
- Merwin, R.M.; Zucker, N.L.; Wilson, K.G. ACT for Anorexia Nervosa: A Guide for Clinicians; The Guilford Press: New York, NY, USA, 2019; ISBN 9781462540341 (Paperback). 9781462540358 (Hardcover). [Google Scholar]
- Tecuta, L.; Gardini, V.; Schumann, R.; Ballardini, D.; Tomba, E. Irrational Beliefs and Their Role in Specific and Non-Specific Eating Disorder Symptomatology and Cognitive Reappraisal in Eating Disorders. J. Clin. Med. 2021, 10, 3525. [Google Scholar] [CrossRef]
- Pruccoli, J.; Rosa, S.; Cesaroni, C.A.; Malaspina, E.; Parmeggiani, A. Association among Autistic Traits, Treatment Intensity and Outcomes in Adolescents with Anorexia Nervosa: Preliminary Results. J. Clin. Med. 2021, 10, 3605. [Google Scholar] [CrossRef] [PubMed]
- Karekla, M.; Savvides, S.N.; Gloster, A. An Avatar-led Intervention Promotes Smoking Cessation in Young Adults: A Pilot Randomized Clinical Trial. Ann. Behav. Med. 2020, 54, 747–760. [Google Scholar] [CrossRef] [PubMed]
- Saekow, J.; Jones, M.; Gibbs, E.; Jacobi, C.; Fitzsimmons-Craft, E.E.; Wilfley, D.; Taylor, C.B. StudentBodies-eating disorders: A randomized controlled trial of a coached online intervention for subclinical eating disorders. Internet Interv. 2015, 2, 419–428. [Google Scholar] [CrossRef] [Green Version]
- Taylor, C.B.; Graham, A.K.; Flatt, R.E.; Waldherr, K.; Fitzsimmons-Craft, E.E. Current state of scientific evidence on Internet-based interventions for the treatment of depression, anxiety, eating disorders and substance abuse: An overview of systematic reviews and meta-analyses. Eur. J. Public Health 2021, 31 (Suppl. S1), i3–i10. [Google Scholar] [CrossRef] [PubMed]
| AcceptME Group | Control Group | Interaction Effects | ||||
|---|---|---|---|---|---|---|
| Baseline M (SD) n = 59 | EOI M (SD) n = 29 | Baseline M (SD) n = 29 | EOI M (SD) n = 28 | |||
| WCS | 67.14 (11.93) | 45.95 (25.90) | 63.19 (8.58) | 76.54 (14.85) | F(1,54) = 56.67, p < 0.001, ɳ2 = 0.52 | |
| % score < 52 high-risk cut-off | 0% | 57.10% | 0% | 7.10% | ||
| EDE-Q | ||||||
| Restraint Subscale | 1.82 (1.34) | 1.37 (1.06) | 1.64 (1.19) | 1.70 (0.95) | F(1,54) = 3.81, p = 0.058, ɳ2 = 0.07 | |
| Eating Concern Subscale | 1.59 (1.06) | 1.22 (1.02) | 1.37 (0.92) | 1.27 (0.84) | F(1,54)= 1.08, p > 0.050, ɳ2 = 0.02 | |
| Shape Concern Subscale | 3.18 (1.21) | 2.28 (1.33) | 2.74 (1.07) | 2.88 (1.05) | F(1,54) = 8.49, p < 0.010, ɳ2 = 0.14 | |
| Weight Concern Subscale | 2.76 (1.07) | 2.17 (1.01) | 2.45 (1.00) | 2.56 (1.01) | F(1,54) = 3.81, p = 0.052, ɳ2 = 0.07 | |
| Global | 2.34 (0.93) | 1.75 (0.99) | 1.99 (0.91) | 2.09 (0.66) | F(1,55) = 6.80, p = 0.010, ɳ2 = 0.11 | |
| YQOL-SF | 66.06 (10.05) | 62.71 (22.57) | 68.06 (11.86) | 68.21 (10.10) | F(1,49) = 0.46, p > 0.050, ɳ2 = 0.01 | |
| BSQ-8C | 29.93 (8.35) | 23.34 (11.27) | 26.54 (10.01) | 26.27 (11.35) | F(1,49) = 3.78, p = 0.058, ɳ2 = 0.07 | |
| BI-AAQ | 48.45 (16.90) | 56.76 (15.54) | 48.41 (13.32) | 50.85 (15.10) | F(1,54) = 1.86, p > 0.050, ɳ2 = 0.03 | |
| BIAQ | 35.44 (11.62) | 19.75 (8.58) | 37.54 (18.45) | 23.86 (11.05) | F(1,49) = 0.65, p > 0.050, ɳ2 = 0.01 | |
| Baseline M (SD) n = 25 | EOI M (SD) n = 25 | One-Month Follow-Up M (SD) n = 25 | F-Test | ||
|---|---|---|---|---|---|
| WCS | 56.27 (20.24) a | 44.33 (25.84) b | 40.80 (21.81) b | F(2,23)= 9.30, p < 0.001,ɳ2= 0.45 | |
| EDE-Q | |||||
| Restraint Subscale | 1.57 (1.18) | 1.39 (1.05) | 1.10 (1.01) | F(2,23) = 2.09, p > 0.050, ɳ2 = 0.15 | |
| Eating Concern Subscale | 1.49 (1.02) a | 1.25 (1.06) a | 0.75 (0.87) b | F(2,23)= 12.14, p < 0.001,ɳ2= 0.51 | |
| Shape Concern Subscale | 3.11 (1.16) a | 2.42 (1.34) b | 2.11 (1.12) b | F(2,23)= 9.65, p < 0.001,ɳ2= 0.46 | |
| Weight Concern Subscale | 2.58 (0.99) | 2.17 (1.01) | 1.87 (0.76) | F(2,23)= 10.20, p < 0.001,ɳ2= 0.47 | |
| Global | 2.20 (0.84) a | 1.76 (0.99) b | 1.46 (0.81) bc | F(2,23)= 14.93, p < 0.001,ɳ2= 0.57 | |
| YQOL-SF | 66.07 (10.05) | 62.71 (22.58) | 68.06 (11.86) | F(2,23) = 7.48, p > 0.050, ɳ2 = 0.03 | |
| BSQ-8C | 30.12 (7.92) a | 24.12 (11.56) b | 21.56 (8.91) bc | F(2,23)= 13.38, p < 0.001,ɳ2= 0.54 | |
| BI-AAQ | 49.36 (17.01) a | 57.24 (16.20) b | 63.44 (14.34) bc | F(2,23)= 10.40, p < 0.001,ɳ2= 0.48 | |
| BIAQ | 35.44 (11.32) a | 20.68 (8.53) b | 26.48 (11.12) bc | F(2,23)= 26.64, p < 0.001,ɳ2= 0.70 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karekla, M.; Nikolaou, P.; Merwin, R.M. Randomized Clinical Trial Evaluating AcceptME—A Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High Risk for Eating Disorders. J. Clin. Med. 2022, 11, 1775. https://doi.org/10.3390/jcm11071775
Karekla M, Nikolaou P, Merwin RM. Randomized Clinical Trial Evaluating AcceptME—A Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High Risk for Eating Disorders. Journal of Clinical Medicine. 2022; 11(7):1775. https://doi.org/10.3390/jcm11071775
Chicago/Turabian StyleKarekla, Maria, Patrisia Nikolaou, and Rhonda M. Merwin. 2022. "Randomized Clinical Trial Evaluating AcceptME—A Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High Risk for Eating Disorders" Journal of Clinical Medicine 11, no. 7: 1775. https://doi.org/10.3390/jcm11071775
APA StyleKarekla, M., Nikolaou, P., & Merwin, R. M. (2022). Randomized Clinical Trial Evaluating AcceptME—A Digital Gamified Acceptance and Commitment Early Intervention Program for Individuals at High Risk for Eating Disorders. Journal of Clinical Medicine, 11(7), 1775. https://doi.org/10.3390/jcm11071775






