Association between Long-Term Change in Arterial Stiffness and Cardiovascular Outcomes in Kidney Transplant Recipients: Insights from the TRANSARTE Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurement of PWV
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients
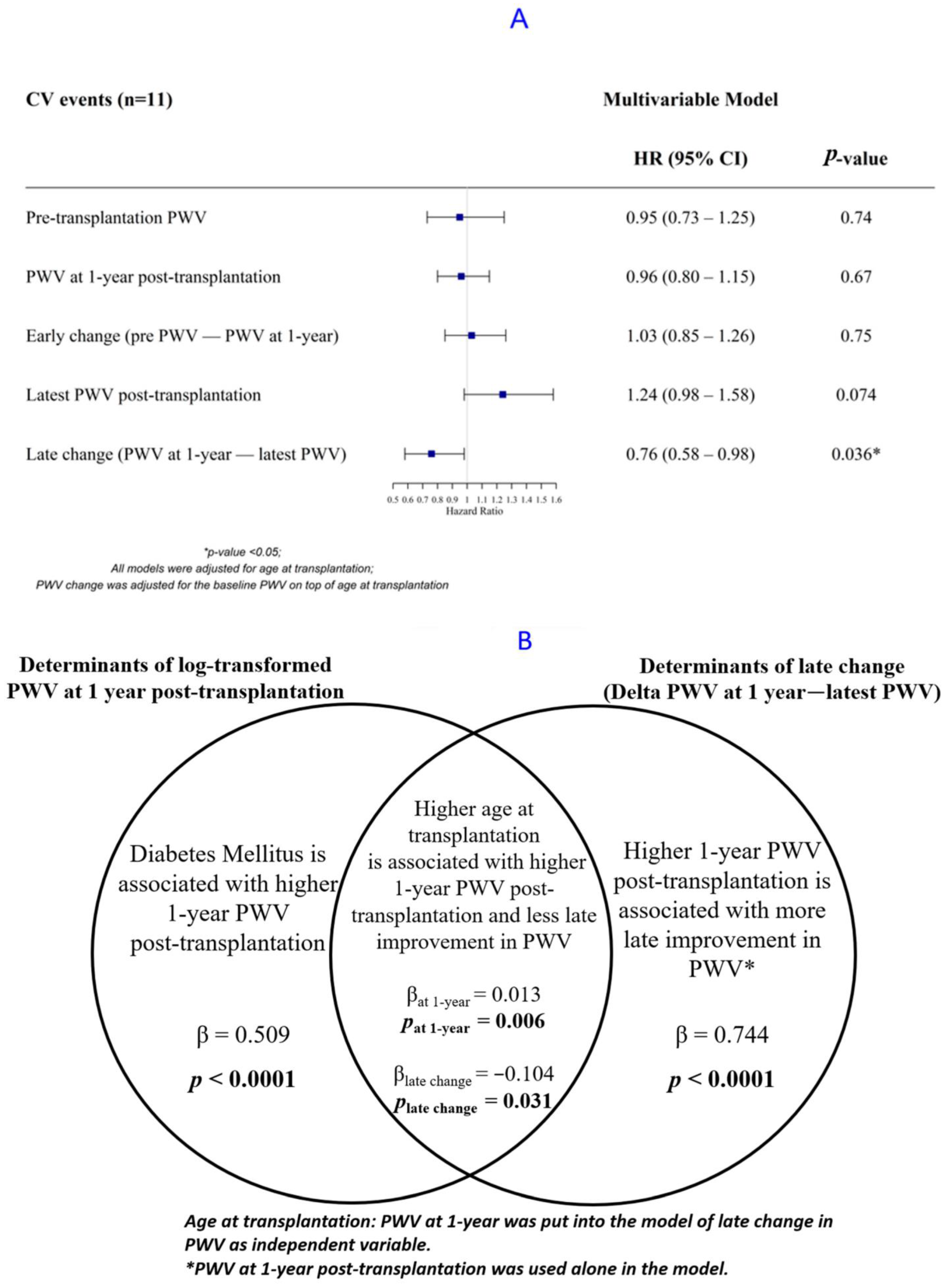
3.2. Association of PWV with CV Events
3.3. Determinants of PWV Using Backward Linear Regression
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Desjardins, M.P.; Sidibe, A.; Fortier, C.; Mac-Way, F.; De Serres, S.; Lariviere, R.; Spronck, B.; Goupil, R.; Agharazii, M. Impact of kidney transplantation on aortic stiffness and aortic stiffness index beta0. J. Hypertens. 2019, 37, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Boutouyrie, P.; Fliser, D.; Goldsmith, D.; Covic, A.; Wiecek, A.; Ortiz, A.; Martinez-Castelao, A.; Lindholm, B.; Massy, Z.A.; Suleymanlar, G.; et al. Assessment of arterial stiffness for clinical and epidemiological studies: Methodological considerations for validation and entry into the European Renal and Cardiovascular Medicine registry. Nephrol. Dial. Transpl. 2014, 29, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Claes, K.J.; Heye, S.; Bammens, B.; Kuypers, D.R.; Meijers, B.; Naesens, M.; Vanrenterghem, Y.; Evenepoel, P. Aortic calcifications and arterial stiffness as predictors of cardiovascular events in incident renal transplant recipients. Transpl. Int. 2013, 26, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Dahle, D.O.; Eide, I.A.; Asberg, A.; Leivestad, T.; Holdaas, H.; Jenssen, T.G.; Fagerland, M.W.; Pihlstrom, H.; Mjoen, G.; Hartmann, A. Aortic Stiffness in a Mortality Risk Calculator for Kidney Transplant Recipients. Transplantation 2015, 99, 1730–1737. [Google Scholar] [CrossRef] [PubMed]
- Ignace, S.; Utescu, M.S.; De Serres, S.A.; Marquis, K.; Gaudreault-Tremblay, M.M.; Lariviere, R.; Cote, I.; Houde, I.; Lebel, M.; Agharazii, M. Age-related and blood pressure-independent reduction in aortic stiffness after kidney transplantation. J. Hypertens. 2011, 29, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Seung, J.; Lee, J.H.; Chung, B.H.; Yang, C.W. Clinical Significance of Pre-Transplant Arterial Stiffness and the Impact of Kidney Transplantation on Arterial Stiffness. PLoS ONE 2015, 10, e0139138. [Google Scholar] [CrossRef] [PubMed]
- Sidibe, A.; Fortier, C.; Desjardins, M.P.; Zomahoun, H.T.V.; Boutin, A.; Mac-Way, F.; De Serres, S.; Agharazii, M. Reduction of Arterial Stiffness After Kidney Transplantation: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2017, 6, e007235. [Google Scholar] [CrossRef] [PubMed]
- Melilli, E.; Manonelles, A.; Montero, N.; Grinyo, J.; Martinez-Castelao, A.; Bestard, O.; Cruzado, J. Impact of immunosuppressive therapy on arterial stiffness in kidney transplantation: Are all treatments the same? Clin. Kidney J. 2018, 11, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Karras, A.; Boutouyrie, P.; Briet, M.; Bozec, E.; Haymann, J.P.; Legendre, C.; McMahon, L.P.; Delahousse, M. Reversal of Arterial Stiffness and Maladaptative Arterial Remodeling After Kidney Transplantation. J. Am. Heart Assoc. 2017, 6, e006078. [Google Scholar] [CrossRef] [PubMed]
- Bachelet-Rousseau, C.; Kearney-Schwartz, A.; Frimat, L.; Fay, R.; Kessler, M.; Benetos, A. Evolution of arterial stiffness after kidney transplantation. Nephrol. Dial. Transpl. 2011, 26, 3386–3391. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cheddani, L.; Radulescu, C.; Chaignon, M.; Karras, A.; Neuzillet, Y.; Duong, J.P.; Tabibzadeh, N.; Letavernier, E.; Delahousse, M.; Haymann, J.P. From arterial stiffness to kidney graft microvasculature: Mortality and graft survival within a cohort of 220 kidney transplant recipients. PLoS ONE 2018, 13, e0195928. [Google Scholar] [CrossRef] [PubMed]
- Kolonko, A.; Chudek, J.; Szotowska, M.; Kuczera, P.; Wiecek, A. Cardiovascular Risk Factors and Markers of Atherosclerosis in Stable Kidney Transplant Recipients. Transpl. Proc. 2016, 48, 1543–1550. [Google Scholar] [CrossRef] [PubMed]
- Birdwell, K.A.; Jaffe, G.; Bian, A.; Wu, P.; Ikizler, T.A. Assessment of arterial stiffness using pulse wave velocity in tacrolimus users the first year post kidney transplantation: A prospective cohort study. BMC Nephrol. 2015, 16, 93. [Google Scholar] [CrossRef] [PubMed]
- Korogiannou, M.; Xagas, E.; Marinaki, S.; Sarafidis, P.; Boletis, J.N. Arterial Stiffness in Patients with Renal Transplantation; Associations with Co-morbid Conditions, Evolution, and Prognostic Importance for Cardiovascular and Renal Outcomes. Front. Cardiovasc. Med. 2019, 6, 67. [Google Scholar] [CrossRef] [PubMed]
| Overall Population N = 40 | |
|---|---|
| Baseline characteristics | |
| Female (%) | 19 (47.5) |
| Age at transplantation (years) | 53 [47–60] |
| Medical history | |
| Hypercholesterolemia (%) | 20 (50.0) |
| Smoking (%) | 16 (40.0) |
| Diabetes (%) | 5 (12.5) |
| History of angina or myocardial infarction (%) | 2 (5.0) |
| Previous Strokes (%) | 2 (5.0) |
| Cause of ESRD (%) | |
| Diabetes | 2 (5.0) |
| Glomerulopathy | 7 (17.5) |
| Malformation | 8 (20.0) |
| Polycystic kidney disease | 10 (25.0) |
| Vascular | 6 (15.0) |
| Other | 7 (17.5) |
| Pre-transplantation dialysis (%) | 30 (75.0) |
| Hemodialysis (%) | 23 (76.7) |
| Peritoneal dialysis (%) | 7 (23.3) |
| Dialysis duration (years) | 2.7 [2.1–3.5] |
| Transplantation characteristics | |
| Calcineurin inhibitors (%) | 38 (95.0) |
| Cyclosporine (%) | 21 (55.3) |
| Tacrolimus (%) | 17 (44.7) |
| Donor type | |
| Living donor (%) | 6 (15.0) |
| Deceased donor (%) | 34 (85.0) |
| Standard-criteria donors (SCD) | 17 (51.5) |
| Expanded-criteria donors (ECD) | 16 (48.5) |
| Arterial stiffness characteristics | |
| Duration between pre-transplantation PWV and transplantation (months) | 7 [2–11] |
| Pre-transplantation PWV (m/s) | 8.9 ± 2.5 |
| Pre-transplantation mean arterial blood pressure (mmHg) | 101 ± 14 |
| Duration between transplantation and 1-year post-transplantation PWV (months) | 13 [11–25] |
| 1-year post-transplantation PWV (m/s) | 9.0 ± 2.8 |
| 1-year post-transplantation mean arterial blood pressure (mmHg) | 94 ± 12 |
| Duration between transplantation and the latest post-transplantation PWV (months) | 52 [37–62] |
| The latest post-transplantation PWV (m/s) | 8.9 ± 2.4 |
| The latest post-transplantation mean arterial blood pressure (mmHg) | 91 ± 12 |
| Post-transplantation characteristics | |
| eGFR at 1 year | 48.5 [40.5–54.3] |
| eGFR at the last contact | |
| All patients | 48.0 [25.8–53.8] |
| Not back to dialysis patients | 48.5 [42.3–56.8] |
| Follow-up time (years) | 10.9 [8.2–12.0] |
| Back to dialysis or preemptive re-transplantation (%) | 6 (15.0) |
| Death (%) | 12 (30.0) |
| CV events post-transplantation (%) | 11 (27.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salib, M.; Simon, A.; Girerd, N.; Kearney-Schwartz, A.; Rossignol, P.; Benetos, A.; Frimat, L.; Girerd, S. Association between Long-Term Change in Arterial Stiffness and Cardiovascular Outcomes in Kidney Transplant Recipients: Insights from the TRANSARTE Study. J. Clin. Med. 2022, 11, 1410. https://doi.org/10.3390/jcm11051410
Salib M, Simon A, Girerd N, Kearney-Schwartz A, Rossignol P, Benetos A, Frimat L, Girerd S. Association between Long-Term Change in Arterial Stiffness and Cardiovascular Outcomes in Kidney Transplant Recipients: Insights from the TRANSARTE Study. Journal of Clinical Medicine. 2022; 11(5):1410. https://doi.org/10.3390/jcm11051410
Chicago/Turabian StyleSalib, Madonna, Arnaud Simon, Nicolas Girerd, Anna Kearney-Schwartz, Patrick Rossignol, Athanase Benetos, Luc Frimat, and Sophie Girerd. 2022. "Association between Long-Term Change in Arterial Stiffness and Cardiovascular Outcomes in Kidney Transplant Recipients: Insights from the TRANSARTE Study" Journal of Clinical Medicine 11, no. 5: 1410. https://doi.org/10.3390/jcm11051410
APA StyleSalib, M., Simon, A., Girerd, N., Kearney-Schwartz, A., Rossignol, P., Benetos, A., Frimat, L., & Girerd, S. (2022). Association between Long-Term Change in Arterial Stiffness and Cardiovascular Outcomes in Kidney Transplant Recipients: Insights from the TRANSARTE Study. Journal of Clinical Medicine, 11(5), 1410. https://doi.org/10.3390/jcm11051410






