Selecting the Best Combined Biological Therapy for Refractory Inflammatory Bowel Disease Patients
Abstract
:1. Introduction
2. Global Efficacy and Safety of CoT
3. Usefulness and Safety of Biologic Combinations
- (a)
- Ustekinumab plus vedolizumab
- (b)
- Anti-TNF plus vedolizumab
- (c)
- Other combinations
- (d)
- Safety
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raine, T.; Bonovas, S.; Burisch, J.; Kucharzik, T.; Adamina, M.; Annese, V.; Bachmann, O.; Bettenworth, D.; Chaparro, M.; Czuber-Dochan, W.; et al. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Medical Treatment. J. Crohn’s Colitis 2021, 16, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Bonovas, S.; Doherty, G.; Kucharzik, T.; Gisbert, J.P.; Raine, T.; Adamina, M.; Armuzzi, A.; Bachmann, O.; Bager, P.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Medical Treatment. J. Crohn’s Colitis 2020, 14, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Colombel, J.F.; Reinisch, W.; Mantzaris, G.J.; Kornbluth, A.; Rutgeerts, P.; Tang, K.L.; Oortwijn, A.; Bevelander, G.S.; Cornillie, F.J.; Sandborn, W.J. Randomised clinical trial: Deep remission in biologic and immunomodulator naïve patients with Crohn’s disease—A SONIC post hoc analysis. Aliment. Pharmacol. Ther. 2015, 41, 734–746. [Google Scholar] [CrossRef] [PubMed]
- Hirten, R.P.; Iacucci, M.; Shah, S.; Ghosh, S.; Colombel, J.F. Combining Biologics in Inflammatory Bowel Disease and Other Immune Mediated Inflammatory Disorders. Clin. Gastroenterol. Hepatol. 2018, 16, 1374–1384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grieco, M.J.; Remzi, F.H. Surgical Management of Ulcerative Colitis. Gastroenterol. Clin. N. Am. 2020, 49, 753–768. [Google Scholar] [CrossRef] [PubMed]
- Ricart, E. Current status of mesenchymal stem cell therapy and bone marrow transplantation in IBD. Dig. Dis. 2012, 30, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Gold, S.L.; Steinlauf, A.F. Therapy in Patients With Inflammatory Bowel Disease: A Review of the Literature. Gastroenterol. Hepatol. 2021, 17, 406–414. [Google Scholar]
- Ahmed, W.; Galati, J.; Kumar, A.; Christos, P.J.; Longman, R.; Lukin, D.J.; Scherl, E.; Battat, R. Dual Biologic or Small Molecule Therapy for Treatment of Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2021, 20, e361–e379. [Google Scholar] [CrossRef]
- Ribaldone, D.G.; Pellicano, R.; Vernero, M.; Caviglia, G.P.; Saracco, G.M.; Morino, M.; Astegiano, M. Dual biological therapy with anti-TNF, vedolizumab or ustekinumab in inflammatory bowel disease: A systematic review with pool analysis. Scand. J. Gastroenterol. 2019, 54, 407–413. [Google Scholar] [CrossRef]
- Goessens, L.; Colombel, J.F.; Outtier, A.; Ferrante, M.; Sabino, J.; Judge, C.; Saeidi, R.; Rabbitt, L.; Armuzzi, A.; Domenech, E.; et al. Safety and efficacy of combining biologics or small molecules for inflammatory bowel disease or immune-mediated inflammatory diseases: A European retrospective observational study. United Eur. Gastroenterol. J. 2021, 9, 1136–1147. [Google Scholar] [CrossRef]
- Yang, E.; Panaccione, N.; Whitmire, N.; Dulai, P.S.; Casteele, N.V.; Singh, S.; Boland, B.S.; Collins, A.; Sandborn, W.J.; Panaccione, R.; et al. Efficacy and Safety of Simultaneous Treatment with Two Biologic Medications in Refractory Crohn’s Disease. Aliment. Pharmacol. Ther. 2020, 51, 1031–1038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwapisz, L.; Raffals, L.E.; Bruining, D.H.; Pardi, D.S.; Tremaine, W.J.; Kane, S.V.; Papadakis, K.A.; Coelho-Prabhu, N.; Kisiel, J.B.; Heron, V.; et al. Combination Biologic Therapy in Inflammatory Bowel Disease: Experience From a Tertiary Care Center. Clin. Gastroenterol. Hepatol. 2021, 19, 616–617. [Google Scholar] [CrossRef] [PubMed]
- Privitera, G.; Onali, S.; Pugliese, D.; Renna, S.; Savarino, E.; Viola, A.; Ribaldone, D.G.; Buda, A.; Bezzio, C.; Fiorino, G.; et al. Dual Targeted Therapy: A Possible Option for the Management of Refractory Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Glassner, K.; Oglat, A.; Duran, A.; Koduru, P.; Perry, C.; Wilhite, A.; Abraham, B.P. The use of combination biological or small molecule therapy in inflammatory bowel disease: A retrospective cohort study. J. Dig. Dis. 2020, 21, 264–271. [Google Scholar] [CrossRef]
- Stone, M.; Morrison, M.; Forster, E. P076 The Role of Dual Biologic Therapy in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2021, 116, S20. [Google Scholar] [CrossRef]
- Gniadecki, R.; Bang, B.; Sand, C. Combination of antitumour necrosis factor-α and anti-interleukin-12/23 antibodies in refractory psoriasis and psoriatic arthritis: A long-term case-series observational study. Br. J. Dermatol. 2016, 174, 1145–1146. [Google Scholar] [CrossRef]
- Hamilton, T. Treatment of psoriatic arthritis and recalcitrant skin disease with combination therapy. J. Drugs Dermatol. 2008, 7, 1089–1093. [Google Scholar]
- Krell, J.M. Use of alefacept and etanercept in 3 patients whose psoriasis failed to respond to etanercept. J. Am. Acad. Dermatol. 2006, 54, 1099–1101. [Google Scholar] [CrossRef]
- Weinblatt, M.; Combe, B.; Covucci, A.; Aranda, R.; Becker, J.C.; Keystone, E. Safety of the selective costimulation modulator abatacept in rheumatoid arthritis patients receiving background biologic and nonbiologic disease-modifying antirheumatic drugs: A one-year randomized, placebo-controlled study. Arthritis Rheum. 2006, 54, 2807–2816. [Google Scholar] [CrossRef]
- Weinblatt, M.; Schiff, M.; Goldman, A.; Kremer, J.; Luggen, M.; Li, T.; Chen, D.; Becker, J.C. Selective costimulation modulation using abatacept in patients with active rheumatoid arthritis while receiving etanercept: A randomised clinical trial. Ann. Rheum. Dis. 2007, 66, 228–234. [Google Scholar] [CrossRef]
- Greenwald, M.W.; Shergy, W.J.; Kaine, J.L.; Sweetser, M.T.; Gilder, K.; Linnik, M.D. Evaluation of the safety of rituximab in combination with a tumor necrosis factor inhibitor and methotrexate in patients with active rheumatoid arthritis: Results from a randomized controlled trial. Arthritis Rheum. 2011, 63, 622–632. [Google Scholar] [CrossRef] [Green Version]
- Van Vollenhoven, R.F.; Wax, S.; Li, Y.; Tak, P.P. Safety and efficacy of atacicept in combination with rituximab for reducing the signs and symptoms of rheumatoid arthritis: A phase II, randomized, double-blind, placebo-controlled pilot trial. Arthritis Rheumatol. 2015, 67, 2828–2836. [Google Scholar] [CrossRef] [PubMed]
- Olbjørn, C.; Rove, J.B.; Jahnsen, J. Combination of Biological Agents in Moderate to Severe Pediatric Inflammatory Bowel Disease: A Case Series and Review of the Literature. Pediatr. Drugs 2020, 22, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Dolinger, M.; Spencer, E.; Lai, J.; Dunkin, D.; Dubinsky, M. Dual biologic and small molecule therapy for the treatment of refractory pediatric inflammatory bowel disease. Inflamm. Bowel Dis. 2021, 27, 1210–1214. [Google Scholar] [CrossRef] [PubMed]
- Peyrin-Biroulet, L.; Sandborn, W.; Sands, B.E.; Reinisch, W.; Bemelman, W.; Bryant, R.V.; D’Haens, G.; Dotan, I.; Dubinsky, M.; Feagan, B.; et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): Determining Therapeutic Goals for Treat-to-Target. Am. J. Gastroenterol. 2015, 110, 1324–1338. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Ricciuto, A.; Lewis, A.; D’Amico, F.; Dhaliwal, J.; Griffiths, A.M.; Bettenworth, D.; Sandborn, W.J.; Sands, B.E.; Reinisch, W.; et al. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology 2021, 160, 1570–1583. [Google Scholar] [CrossRef]
| Reference | Year | Study Type | Number of Subjects | Disease | Age (Mean) | Disease Duration (Mean Years) | Clinical Evaluation | Endoscopic Evaluation | Adverse Events | Follow-Up (Mean) |
|---|---|---|---|---|---|---|---|---|---|---|
| Goessens et al. [10] | 2021 | Multicentric Retrospective | 98 | 58 CD 40 UC | 26 | 70% response | 50% response | 42% | 8 month | |
| Glassner et al. [14] | 2020 | Unicentric Retrospective | 50 | 32 CD 18 UC 1 IBD-U | 36.7 | 14.8 | 50% remission | 34% remission | 16% | 8 month |
| Kwapisz et al. [12] | 2021 | Unicentric Retrospective | 15 | 14 CD 1 UC | 36 | 12.5 | 73% response | 44% response | 53% | 24 month |
| Privitera et al. [13] | 2020 | Multicentric Retrospective | 16 | 11 CD 5 UC | 38 | 10.5 | 100% response | 18.8% | 7 month | |
| Yang et al. [11] | 2020 | Multicentric Retrospective | 22 | 22 CD | 35 | 50% response | 50% response | 13% | 9 month |
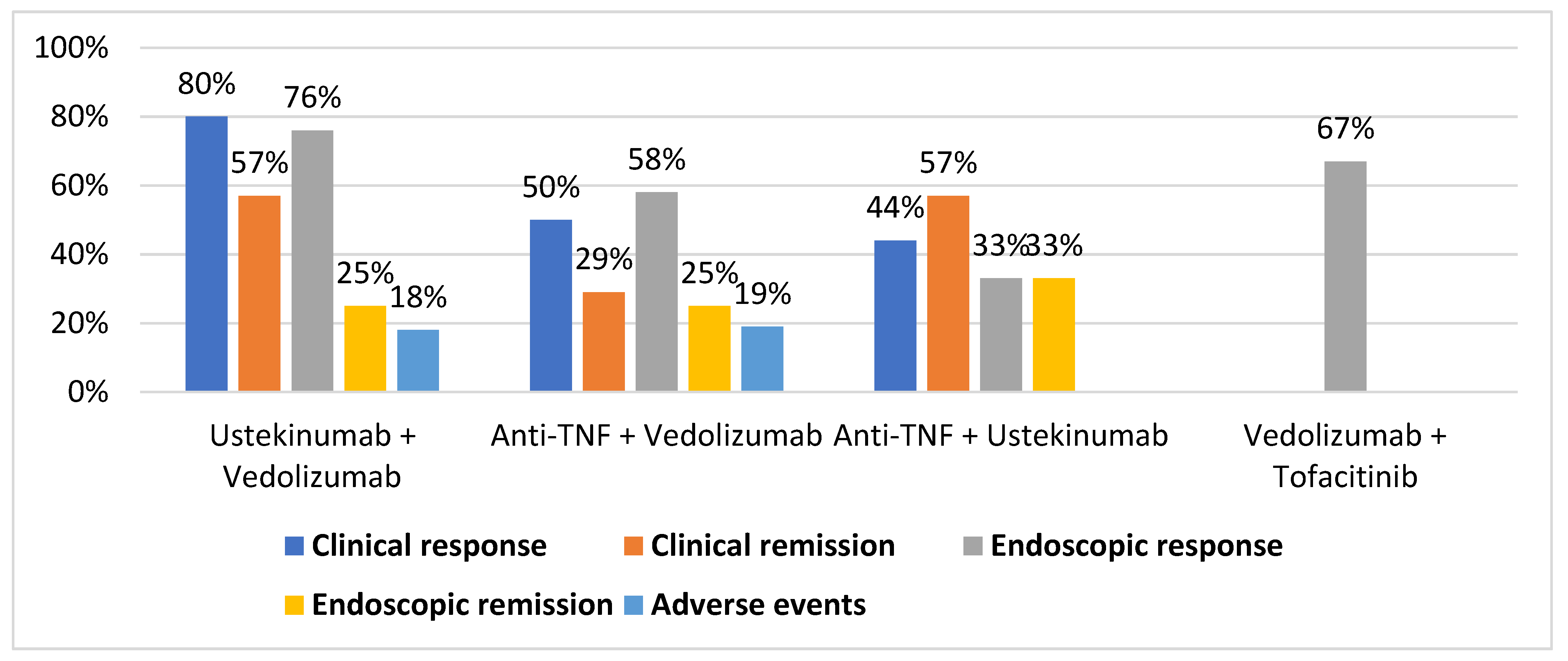
| Clinical Response | Clinical Remission | Endoscopic Response | Endoscopic Remission | Adverse Events | ||
|---|---|---|---|---|---|---|
| Ustekinumab + Vedolizumab | Yang et al. | 5 of 7 | 4 of 7 | 5 of 8 | 2 of 8 | 1 of 8 |
| Kwapisz et al. | 4 of 5 | 0 of 5 | ||||
| Privitera et al. | 3 of 3 | 1 of 3 | ||||
| Glassner et al. | 11 of 13 | |||||
| TOTAL | 12 of 15 (80%) | 4 of 7 (57%) | 16 of 21 (76%) | 2 of 8 (25%) | 2 of 11 (18%) | |
| Anti-TNF + Vedolizumab | Yang et al. | 5 of 12 | 4 of 12 | 4 of 12 | 3 of 12 | 2 of 12 |
| Kwapisz et al. | 5 of 8 | 3 of 8 | ||||
| Privitera et al. | 3 of 6 | 3 of 6 | 1 of 6 | |||
| Glassner et al. | 24 of 36 | |||||
| TOTAL | 13 of 26 (50%) | 7 of 18 (29%) | 28 of 48 (58%) | 3 of 12 (25%) | 5 of 26 (19%) | |
| Anti-TNF + Ustekinumab | Yang et al. | 1 of 3 | 1 of 3 | 1 of 3 | 1 of 3 | |
| Kwapisz et al. | 2 of 2 | |||||
| Privitera et al. | 1 of 4 | 3 of 4 | ||||
| TOTAL | 4 of 9 (44%) | 4 of 7 (57%) | 1 of 3 (33%) | 1 of 3 (33%) | ||
| Secukinumab + Vedolizumab | Privitera et al. | 2 of 2 | ||||
| TOTAL | 2 of 2 (100%) | |||||
| Vedolizumab + Apremilast | Privitera et al. | 1 of 1 | 1 of 1 | |||
| TOTAL | 1 of 1 (100%) | 1 of 1 (100%) | ||||
| Vedolizumab + Tofacitinib | Glassner et al. | 8 of 12 | ||||
| TOTAL | 8 of 12 (67%) |
| Study | VEDO+ USTE | AntiTNF+ VEDO | AntiTNF+ USTE | TOFA+ VEDO | TOFA+ USTE | TOFA+ TNF | Other ** |
|---|---|---|---|---|---|---|---|
| Goessens et al. * [10] | 16 | 36 | 8 | 12 | - | 1 | 8 |
| Glassner et al. [14] | 25 | 7 | 8 | 3 | 9 | 1 | |
| Kwapisz et al. [12] | 5 | 8 | 2 | ||||
| Privitera et al. ** [13] | 3 | 6 | 4 | 3 | |||
| Yang et al. [11] | 8 | 13 | 3 | ||||
| TOTAL | 62 | 75 | 20 | 21 | 3 | 10 | 19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mas, E.B.; Calvo, X.C. Selecting the Best Combined Biological Therapy for Refractory Inflammatory Bowel Disease Patients. J. Clin. Med. 2022, 11, 1076. https://doi.org/10.3390/jcm11041076
Mas EB, Calvo XC. Selecting the Best Combined Biological Therapy for Refractory Inflammatory Bowel Disease Patients. Journal of Clinical Medicine. 2022; 11(4):1076. https://doi.org/10.3390/jcm11041076
Chicago/Turabian StyleMas, Eduard Brunet, and Xavier Calvet Calvo. 2022. "Selecting the Best Combined Biological Therapy for Refractory Inflammatory Bowel Disease Patients" Journal of Clinical Medicine 11, no. 4: 1076. https://doi.org/10.3390/jcm11041076
APA StyleMas, E. B., & Calvo, X. C. (2022). Selecting the Best Combined Biological Therapy for Refractory Inflammatory Bowel Disease Patients. Journal of Clinical Medicine, 11(4), 1076. https://doi.org/10.3390/jcm11041076






