Effect of Carbohydrate-Enriched Drink Compared to Fasting on Hemodynamics in Healthy Volunteers. A Randomized Trial
Abstract
1. Introduction
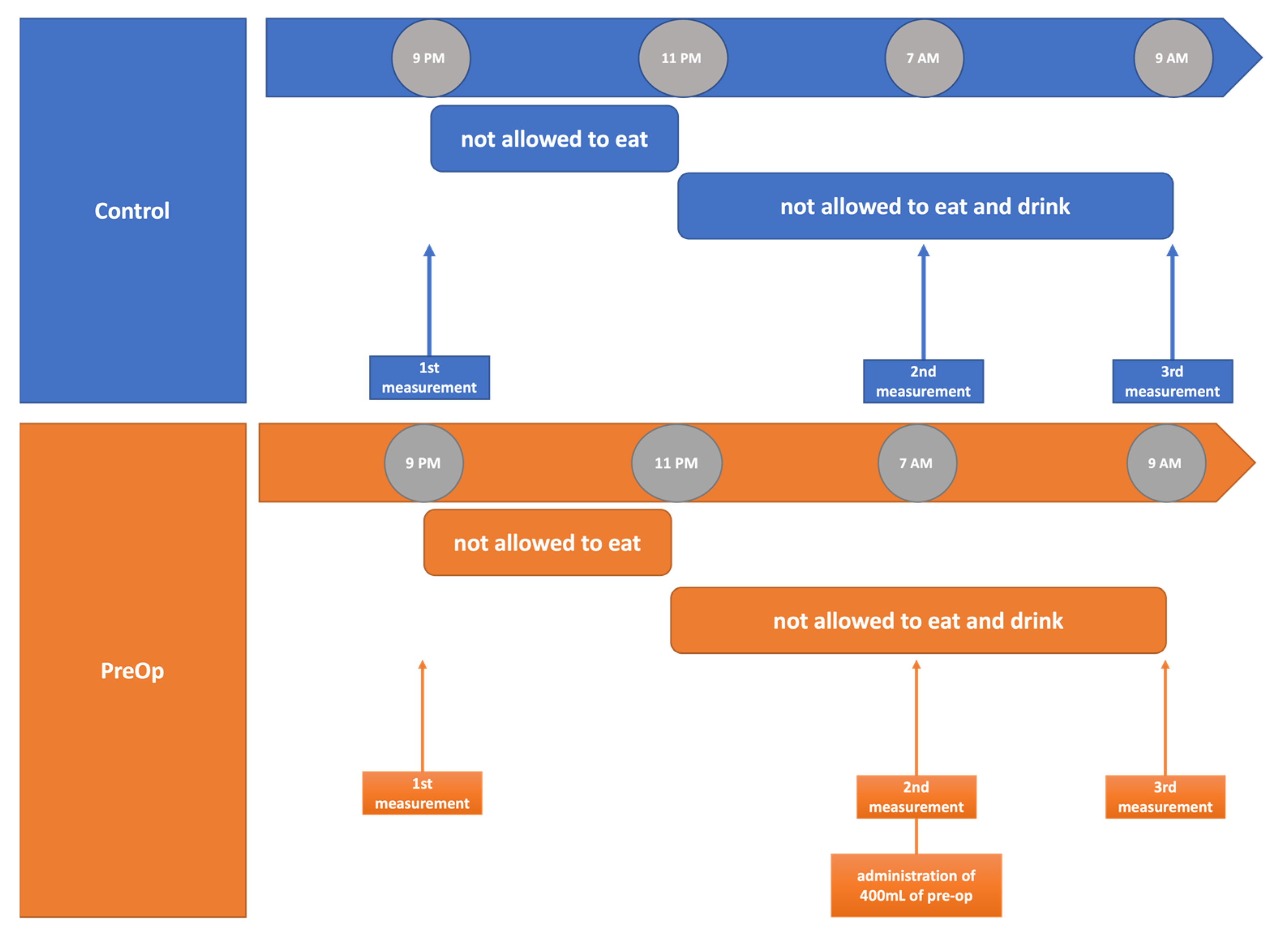
2. Materials and Methods
2.1. Participants
2.2. Impedance Cardiography
2.3. Carbohydrate Drink
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maltby, J.R. Fasting from midnight—The history behind the dogma. Best Pract. Res. Clin. Anaesthesiol. 2006, 20, 363–378. [Google Scholar] [CrossRef] [PubMed]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.G.; et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin. Nutr. 2021, 40, 4745–4761. [Google Scholar] [CrossRef] [PubMed]
- Anesthesiologists, A.S. Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures. Anesthesiology 2017, 126, 376–393. [Google Scholar]
- El-Sharkawy, A.M.; Daliya, P.; Lewis-Lloyd, C.; Adiamah, A.; Malcolm, F.L.; Boyd-Carson, H.; Couch, D.; Herrod, P.J.; Hossain, T.; Couch, J.; et al. Fasting and surgery timing (FaST) audit. Clin. Nutr. 2021, 40, 1405–1412. [Google Scholar] [CrossRef]
- de Aguilar-Nascimento, J.E. Reducing preoperative fasting time: A trend based on evidence. World J. Gastrointest. Surg. 2010, 2, 57. [Google Scholar] [CrossRef]
- Li, Y.; He, R.; Ying, X.; Hahn, R.G. Dehydration, Hemodynamics and fluid volume optimization after induction of general anesthesia. Clinics 2014, 69, 809–816. [Google Scholar] [CrossRef]
- Gutierrez, D.S.G.; Gutiérrez, J.J.V.; Ruiz-Villa, J.O. Cardiac output estimation based on arterial and venous blood gas analysis: Proposal of a monitoring method. Anaesthesiol. Intensive Ther. 2021, 53, 179–183. [Google Scholar] [CrossRef]
- Miller, T.E.; Roche, A.M.; Mythen, M. Fluid management and goal-directed therapy as an adjunct to Enhanced Recovery after Surgery (ERAS). Can. J. Anesth. 2015, 62, 158–168. [Google Scholar] [CrossRef]
- Nygren, J.; Thacker, J.; Carli, F.; Fearon, K.C.; Norderval, S.; Lobo, D.N.; Ljungqvist, O.; Soop, M.; Ramirez, J. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced recovery after surgery (ERAS®) society recommendations. World J. Surg. 2013, 31, 801–816. Available online: https://pubmed.ncbi.nlm.nih.gov/23052796/ (accessed on 1 November 2020). [CrossRef]
- Nygren, J.; Thorell, A.; Ljungqvist, O. Preoperative oral carbohydrate therapy. Curr. Opin. Anaesthesiol. 2015, 28, 364–369. [Google Scholar] [CrossRef]
- Nygren, J. The metabolic effects of fasting and surgery. Best Pract. Res. Clin. Anaesthesiol. 2006, 20, 429–438. Available online: https://pubmed.ncbi.nlm.nih.gov/17080694/ (accessed on 31 October 2020). [CrossRef]
- Smith, M.D.; Mccall, J.; Plank, L.; Herbison, G.P.; Soop, M.; Nygren, J. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst. Rev. 2014, 14, CD009161. [Google Scholar] [CrossRef] [PubMed]
- Amer, M.A.; Smith, M.D.; Herbison, G.P.; Plank, L.D.; McCall, J.L. Network meta-analysis of the effect of preoperative carbohydrate loading on recovery after elective surgery. Br. J. Surg. 2017, 104, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Kukliński, J.; Steckiewicz, K.P.; Sekuła, B.; Aszkiełowicz, A.; Owczuk, R. The influence of fasting and carbohydrate-enriched drink administration on body water amount and distribution: A volunteer randomized study. Perioper. Med. 2021, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Pang, Q.; Hendrickx, J.; Liu, H.L.; Poelaert, J. Contemporary perioperative haemodynamic monitoring. Anaesthesiol. Intensive Ther. 2019, 51, 147–158. [Google Scholar] [CrossRef]
- Mansouri, S.; Alhadidi, T.; Chabchoub, S.; Ben Salah, R. Impedance cardiography: Recent applications and developments. Biomed. Res. 2018, 29, 3542–3552. [Google Scholar] [CrossRef]
- Cleymaet, R.; Scheinok, T.; Maes, H.; Stas, A.; Malbrain, L.; De Laet, I.; Schoonheydt, K.; Dits, H.; van Regenmortel, N.; Mekeirele, M.; et al. Prognostic value of bioelectrical impedance analysis for assessment of fluid overload in ICU patients: A pilot study. Anaesthesiol. Intensive Ther. 2021, 53, 10–17. [Google Scholar] [CrossRef]
- Gijsen, M.; Simons, E.; de Cock, P.; Malbrain, M.L.N.G.; Wauters, J.; Spriet, I. Reproducibility of fluid status measured by bioelectrical impedance analysis in healthy volunteers: A key requirement to monitor fluid status in the intensive care unit. Anaesthesiol. Intensive Ther. 2021, 53, 193–199. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Kim, B.-R.; Lee, K.-H.; Kim, K.-W.; Kim, J.-H.; Lee, S.-Y.; Kim, K.-T.; Choe, W.-J.; Park, J.-S.; Kim, J.-W. Comparison of cardiac output derived from FloTracTM/VigileoTM and impedance cardiography during major abdominal surgery. J. Int. Med. Res. 2013, 41, 1342–1349. [Google Scholar] [CrossRef]
- Scherhag, A.; Kaden, J.J.; Kentschke, E.; Sueselbeck, T.; Borggrefe, M. Comparison of impedance cardiography and thermodilution-derived measurements of stroke volume and cardiac output at rest and during exercise testing. Cardiovasc. Drugs Ther. 2005, 19, 141–147. [Google Scholar] [CrossRef]
- Kim, G.E.; Kim, S.Y.; Kim, S.J.; Yun, S.Y.; Jung, H.H.; Kang, Y.S.; Koo, B.N. Accuracy and efficacy of impedance cardiography as a non-invasive cardiac function monitor. Yonsei Med. J. 2019, 60, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Fuller, H.D. The validity of cardiac output measurment by thoracic impedance: A meta-analysis. Clin. Investig. Med. 1992, 15, 103–112. [Google Scholar]
- Raaijmakers, E.; Faes, T.J.C.; Scholten, R.J.P.M.; Goovaerts, H.G.; Heethaar, R.M. A meta-analysis of three decades of validating thoracic impedance cardiography. Crit. Care Med. 1999, 27, 1203–1213. [Google Scholar] [CrossRef] [PubMed]
- Peyton, P.J.; Chong, S.W. Minimally invasive measurement of cardiac output during surgery and critical care: A meta-analysis of accuracy and precision. Anesthesiology 2010, 113, 1220–1235. Available online: http://pubs.asahq.org/anesthesiology/article-pdf/113/5/1220/252362/0000542-201011000-00037.pdf (accessed on 26 January 2022). [CrossRef]
- Zhang, Y.; Wang, Y.; Shi, J.; Hua, Z.; Xu, J. Cardiac output measurements via echocardiography versus thermodilution: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0222105. [Google Scholar] [CrossRef]
- Daralammouri, Y.; Ayoub, K.; Badrieh, N.; Lauer, B. A hybrid approach for quantifying aortic valve stenosis using impedance cardiography and echocardiography. BMC Cardiovasc. Disord. 2016, 16, 19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, F.; Tsang, R.C.C.; Jones, A.Y.M.; Zhou, M.; Xue, K.; Chen, M.; Wang, Y. Cardiodynamic variables measured by impedance cardiography during a 6-minute walk test are reliable predictors of peak oxygen consumption in young healthy adults. PLoS ONE 2021, 16, e0252219. [Google Scholar] [CrossRef]
- Kubota, S.; Endo, Y.; Kubota, M.; Ishizuka, Y.; Furudate, T. Effects of trunk posture in Fowler’s position on hemodynamics. Auton. Neurosci. Basic Clin. 2015, 189, 56–59. [Google Scholar] [CrossRef]
- Wu, T.W.; Lien, R.I.; Seri, I.; Noori, S. Changes in cardiac output and cerebral oxygenation during prone and supine sleep positioning in healthy term infants. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F483–F489. [Google Scholar] [CrossRef]
- Ma, M.; Noori, S.; Maarek, J.M.; Holschneider, D.P.; Rubinstein, E.H.; Seri, I. Prone positioning decreases cardiac output and increases systemic vascular resistance in neonates. J. Perinatol. 2015, 35, 424–427. [Google Scholar] [CrossRef]
- Paviotti, G.; Todero, S.; Demarini, S. Cardiac output decreases and systemic vascular resistance increases in newborns placed in the left-lateral position. J. Perinatol. 2017, 37, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Borodiciene, J.; Gudaityte, J.; Macas, A. Lithotomy versus jack-knife position on haemodynamic parameters assessed by impedance cardiography during anorectal surgery under low dose spinal anaesthesia: A randomized controlled trial. BMC Anesthesiol. 2015, 15, 74. [Google Scholar] [CrossRef] [PubMed]
- Kendrick, J.B.; Kaye, A.D.; Tong, Y.; Belani, K.; Urman, R.D.; Hoffman, C.; Liu, H. Goal-directed fluid therapy in the perioperative setting. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, S29–S34. [Google Scholar] [PubMed]
- Anandraja, R.; Ranjith Karthekeyan, B. A comparative study of haemodynamic effects of single-blinded orotracheal intubations with intubating laryngeal mask airway, Macintosh and McGrath video laryngoscopes. Anaesthesiol. Intensive Ther. 2021, 53, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Bijker, J.B.; Van Klei, W.A.; Kappen, T.H.; Van Wolfswinkel, L.; Moons, K.G.M.; Kalkman, C.J. Incidence of intraoperative hypotension as a function of the chosen definition: Literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 2007, 107, 213–220. [Google Scholar] [CrossRef]
- Zepeda-Najar, C.; Palacios-Astudillo, R.X.; Chávez-Hernández, J.D.; Lino-Silva, L.S.; Salcedo-Hernández, R.A. Prognostic impact of microsatellite instability in gastric cancer. Wspolczesna Onkol. 2021, 25, 68–71. [Google Scholar] [CrossRef]
- Soop, M.; Nygren, J.; Thorell, A.; Weidenhielm, L.; Lundberg, M.; Hammarqvist, F.; Ljungqvist, O. Preoperative oral carbohydrate treatment attenuates endogenous glucose release 3 days after surgery. Clin. Nutr. 2004, 23, 733–741. [Google Scholar] [CrossRef]
- Yuill, K.A.; Richardson, R.A.; Davidson, H.I.M.; Garden, O.J.; Parks, R.W. The administration of an oral carbohydrate-containing fluid prior to major elective upper-gastrointestinal surgery preserves skeletal muscle mass postoperatively—A randomised clinical trial. Clin. Nutr. 2005, 24, 32–37. [Google Scholar] [CrossRef]
- Hausel, J.; Nygren, J.; Lagerkranser, M.; Hellström, P.M.; Hammarqvist, F.; Almström, C.; Lindh, A.; Thorell, A.; Ljungqvist, O. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth. Analg. 2001, 93, 1344–1350. [Google Scholar] [CrossRef]
- Alves, D.R.; Ribeiras, R. Does fasting influence preload responsiveness in ASA 1 and 2 volunteers? Braz. J. Anesthesiol. 2017, 67, 172–179. [Google Scholar] [CrossRef]
- Rontoyanni, V.G.; Werner, K.; Sanders, T.A.B.; Hall, W.L. Differential acute effects of carbohydrate- and protein-rich drinks compared with water on cardiac output during rest and exercise in healthy young men. Appl. Physiol. Nutr. Metab. 2015, 40, 803–810. [Google Scholar] [CrossRef] [PubMed]
| Variable | Control (n = 50) Number [%] Mean (SD) | Pre-op (n = 50) Number [%] Mean (SD) | p Value |
|---|---|---|---|
| Female | 27 (54%) | 32 (64%) | 0.4162 |
| Age (y) | 23.70 (3.51) | 23.72 (3.12) | 0.9761 |
| Height (cm) | 173.50 (10.12) | 173.30 (9.26) | 0.9263 |
| Weight (kg) | 72.45 (15.86) | 67.53 (11.84) | 0.0819 |
| Variable | 0 h Median (IQR) Mean (SD) | 10 h Median (IQR) Mean (SD) | 12 h Median (IQR) Mean (SD) | p Value (0 h vs. 10 h) | p Value (Control vs. Pre-op) | |
|---|---|---|---|---|---|---|
| Control | Pre-op | |||||
| SBP (mmHg) | 119.50 (12.21) | 114.80 (11.04) | 112.90 (10.99) | 111.30 (10.35) | 0.0052 | 0.4386 |
| DBP (mmHg) | 72.37 (7.76) | 68.77 (6.32) | 68.70 (6.81) | 68.60 (6.82) | 0.0004 | 0.9417 |
| HR (bmp) | 69.50 (63.00–77.00) | 67.91 (11.95) | 62.18 (9.81) | 63.60 (10.22) | 0.1466 | 0.4802 |
| Variable | 0 h Median (IQR) Mean (SD) | 10 h Median (IQR) Mean (SD) | 12 h Median (IQR) Mean (SD) | p Value (0 h vs. 10 h) | p Value (Control vs. Pre-op) | |
|---|---|---|---|---|---|---|
| Control | Pre-op | |||||
| SVV (%) | 15 (11–18) | 14.5 (11–19) | 14.5 (11–21) | 14 (11.75–17) | 0.6982 | 0.6167 |
| SV (mL) | 104 (23.85) | 102.9 (23.33) | 110 (23.61) | 105.3 (21.72) | 0.7419 | 0.3007 |
| SI (mL m−2) | 56.45 (9.47) | 56.15 (8.9) | 58 (54–63) | 57.5 (53–62.25) | 0.8177 | 0.5035 |
| CO (L min−1) | 7.28 (1.76) | 6.87 (1.51) | 6.77 (1.47) | 6.61 (1.39) | 0.0776 | 0.5766 |
| CI (L min−1 m−2) | 3.94 (0.67) | 3.76 (0.65) | 3.65 (0.56) | 3.68 (0.64) | 0.0569 | 0.8815 |
| SVRI (dyn s cm−5 m2) | 1640 (1423–1847) | 1661 (314.2) | 1688 (269) | 1681 (306.2) | 0.9985 | 0.9036 |
| SVR (dyn s cm−5) | 893 (740–1120) | 904 (784.3–1064) | 931.7 (198.4) | 943.6 (184.8) | 0.9441 | 0.7588 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kukliński, J.; Steckiewicz, K.P.; Piwowarczyk, S.P.; Kreczko, M.J.; Aszkiełowicz, A.; Owczuk, R. Effect of Carbohydrate-Enriched Drink Compared to Fasting on Hemodynamics in Healthy Volunteers. A Randomized Trial. J. Clin. Med. 2022, 11, 825. https://doi.org/10.3390/jcm11030825
Kukliński J, Steckiewicz KP, Piwowarczyk SP, Kreczko MJ, Aszkiełowicz A, Owczuk R. Effect of Carbohydrate-Enriched Drink Compared to Fasting on Hemodynamics in Healthy Volunteers. A Randomized Trial. Journal of Clinical Medicine. 2022; 11(3):825. https://doi.org/10.3390/jcm11030825
Chicago/Turabian StyleKukliński, Jakub, Karol P. Steckiewicz, Sebastian P. Piwowarczyk, Mateusz J. Kreczko, Aleksander Aszkiełowicz, and Radosław Owczuk. 2022. "Effect of Carbohydrate-Enriched Drink Compared to Fasting on Hemodynamics in Healthy Volunteers. A Randomized Trial" Journal of Clinical Medicine 11, no. 3: 825. https://doi.org/10.3390/jcm11030825
APA StyleKukliński, J., Steckiewicz, K. P., Piwowarczyk, S. P., Kreczko, M. J., Aszkiełowicz, A., & Owczuk, R. (2022). Effect of Carbohydrate-Enriched Drink Compared to Fasting on Hemodynamics in Healthy Volunteers. A Randomized Trial. Journal of Clinical Medicine, 11(3), 825. https://doi.org/10.3390/jcm11030825








