Therapeutic Effects of the Pilates Method in Patients with Multiple Sclerosis: A Systematic Review
Abstract
:1. Introduction
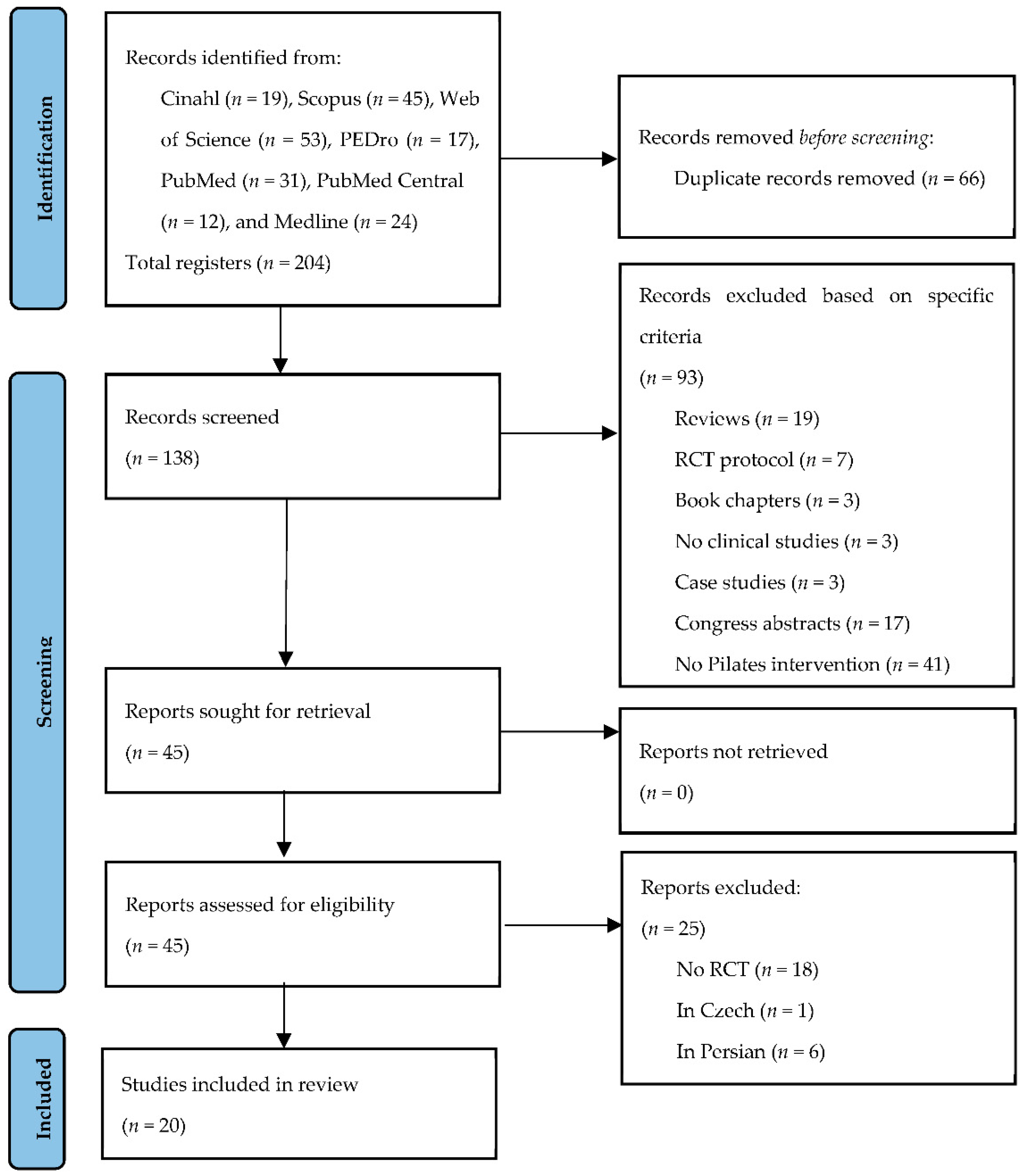
2. Materials and Methods
2.1. Search Process
2.2. Selection Procedure and Eligibility Criteria
2.3. Data Extraction
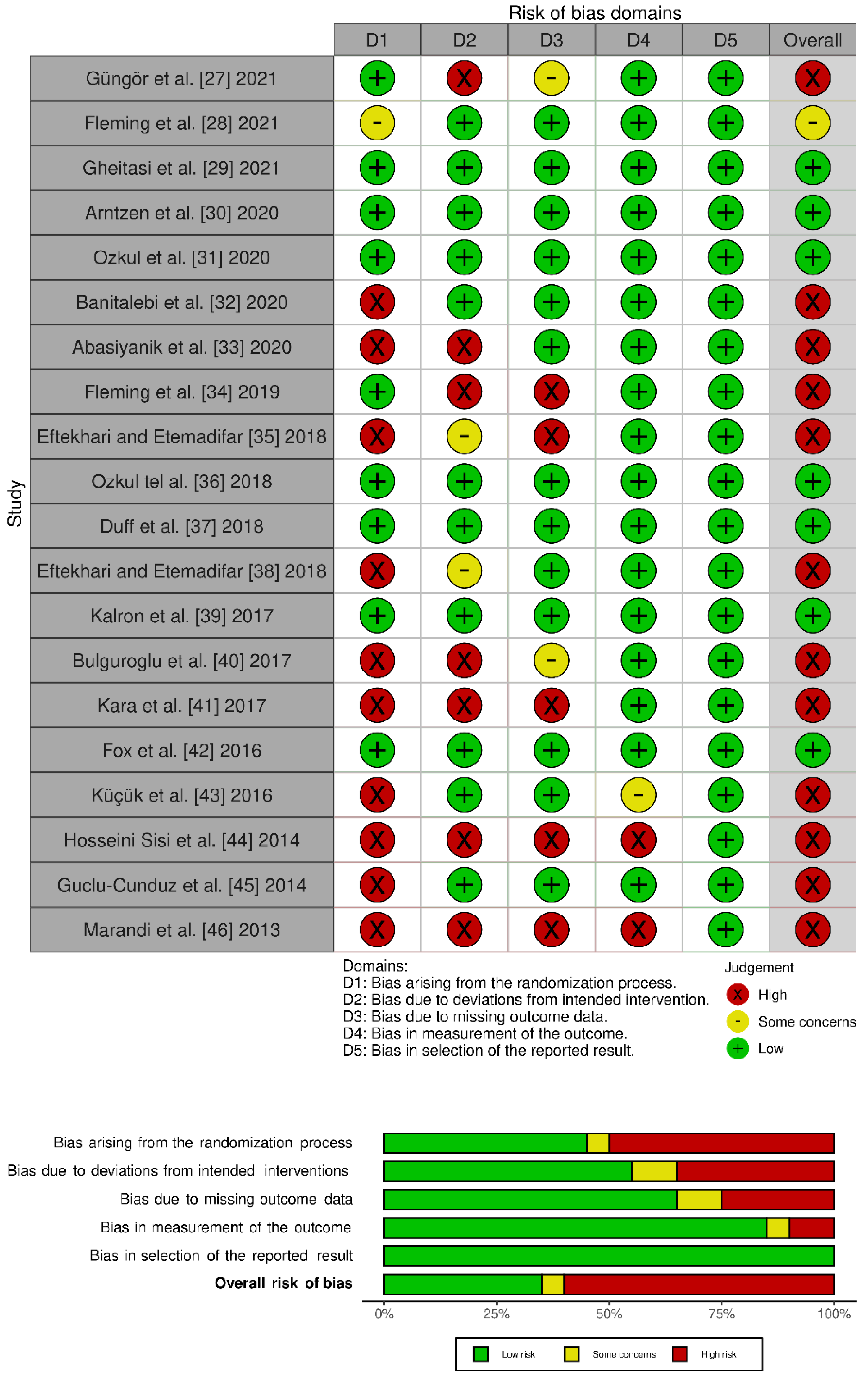
2.4. Assessment of Methodological Quality
3. Results
4. Discussion
4.1. Balance
4.2. Gait/Walking
4.3. Physical-Functional Conditions
4.4. Fatigue
4.5. Quality of Life
4.6. Cognitive/Psychological Function
4.7. Attendance/Adherence
4.8. Sample Characteristics
4.9. Characteristics of the Pilates Interventions
4.10. Adverse Effects and Dropouts
4.11. Methodological Quality of the Studies
4.12. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldenberg, M.M. Multiple sclerosis review. Pharm. Ther. 2012, 37, 175–184. [Google Scholar]
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2018, 26, 27–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reich, D.S.; Lucchinetti, C.F.; Calabresi, P.A. Multiple Sclerosis. N. Engl. J. Med. 2018, 378, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Wallin, M.T.; Culpepper, W.J.; Nichols, E.; Bhutta, Z.A.; Gebrehiwot, T.T.; Hay, S.I.; Khalil, I.A.; Krohn, K.J.; Liang, X.; Naghavi, M.; et al. Global, regional, and national burden of multiple sclerosis 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 269–285. [Google Scholar] [CrossRef] [Green Version]
- Amatya, B.; Khan, F.; Galea, M. Rehabilitation for people with multiple sclerosis: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2019, 1, CD012732. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sørensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F.; et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heine, M.; Van De Port, I.; Rietberg, M.B.; van Wegen, E.E.H.; Kwakkel, G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst. Rev. 2015, 9, CD009956. [Google Scholar] [CrossRef]
- Nilsagård, Y.; Gunn, H.; Freeman, J.; Hoang, P.; Lord, S.; Mazumder, R.; Cameron, M. Falls in people with MS—an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult. Scler. J. 2014, 21, 92–100. [Google Scholar] [CrossRef] [Green Version]
- Rietberg, M.B.; Brooks, D.; Uitdehaag, B.M.; Kwakkel, G. Exercise therapy for multiple sclerosis. Cochrane Database Syst. Rev. 2005, 2005, CD003980. [Google Scholar] [CrossRef]
- Dalgas, U.; Stenager, E.; Ingemann-Hansen, T. Review: Multiple sclerosis and physical exercise: Recommendations for the application of resistance-, endurance- and combined training. Mult. Scler. J. 2008, 14, 35–53. [Google Scholar] [CrossRef]
- Motl, R.W.; Sandroff, B. Benefits of Exercise Training in Multiple Sclerosis. Curr. Neurol. Neurosci. Rep. 2015, 15, 62. [Google Scholar] [CrossRef] [PubMed]
- Petajan, J.H.; White, A.T. Recommendations for physical activity in patients with multiple sclerosis. Sports Med. 1999, 27, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Snook, E.M.; Motl, R.W. Effect of Exercise Training on Walking Mobility in Multiple Sclerosis: A Meta-Analysis. Neurorehabilit. Neural Repair 2008, 23, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Padgett, P.K.; Kasser, S.L. Exercise for Managing the Symptoms of Multiple Sclerosis. Phys. Ther. 2013, 93, 723–728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearson, M.; Dieberg, G.; Smart, N. Exercise as a Therapy for Improvement of Walking Ability in Adults with Multiple Sclerosis: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2015, 96, 1339–1348.e7. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Sandroff, B.; Kwakkel, G.; Dalgas, U.; Feinstein, A.; Heesen, C.; Feys, P.; Thompson, A. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017, 16, 848–856. [Google Scholar] [CrossRef]
- Khan, F.; Amatya, B. Rehabilitation in Multiple Sclerosis: A Systematic Review of Systematic Reviews. Arch. Phys. Med. Rehabil. 2016, 98, 353–367. [Google Scholar] [CrossRef]
- Demaneuf, T.; Aitken, Z.; Karahalios, A.; Leong, T.I.; De Livera, A.M.; Jelinek, G.A.; Weiland, T.; Marck, C.H. Effectiveness of Exercise Interventions for Pain Reduction in People with Multiple Sclerosis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2018, 100, 128–139. [Google Scholar] [CrossRef]
- Tallner, A.; Waschbisch, A.; Wenny, I.; Schwab, S.; Hentschke, C.; Pfeifer, K.; Mäurer, M. Multiple sclerosis relapses are not associated with exercise. Mult. Scler. J. 2011, 18, 232–235. [Google Scholar] [CrossRef] [Green Version]
- Pilutti, L.A.; Platta, M.E.; Motl, R.W.; Latimer, A. The safety of exercise training in multiple sclerosis: A systematic review. J. Neurol. Sci. 2014, 343, 3–7. [Google Scholar] [CrossRef]
- Wells, C.; Kolt, G.; Bialocerkowski, A. Defining Pilates exercise: A systematic review. Complement. Ther. Med. 2012, 20, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Ferreira, A.; Fernandes, J.; Laranjo, L.; Bernardo, L.M.; Silva, A. A Systematic Review of the Effects of Pilates Method of Exercise in Healthy People. Arch. Phys. Med. Rehabil. 2011, 92, 2071–2081. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, K.; Wu, P.-J.; Whillier, S. Is Pilates an effective rehabilitation tool? A systematic review. J. Bodyw. Mov. Ther. 2017, 22, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [Green Version]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke Rehabilitation Evidence-Based Review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Güngör, F.; Tarakci, E.; Özdemir-Acar, Z.; Soysal, A. The effects of supervised versus home Pilates-based core stability training on lower extremity muscle strength and postural sway in people with multiple sclerosis. Mult. Scler. J. 2021, 28. [Google Scholar] [CrossRef]
- Fleming, K.M.; Coote, S.B.; Herring, M.P. Home-based Pilates for symptoms of anxiety, depression and fatigue among persons with multiple sclerosis: An 8-week randomized controlled trial. Mult. Scler. J. 2021, 27, 2267–2279. [Google Scholar] [CrossRef]
- Gheitasi, M.; Bayattork, M.; Andersen, L.L.; Imani, S.; Daneshfar, A. Effect of twelve weeks pilates training on functional balance of male patients with multiple sclerosis: Randomized controlled trial. J. Bodyw. Mov. Ther. 2020, 25, 41–45. [Google Scholar] [CrossRef]
- Arntzen, E.C.; Straume, B.; Odeh, F.; Feys, P.; Normann, B. Group-based, individualized, comprehensive core stability and balance intervention provides immediate and long-term improvements in walking in individuals with multiple sclerosis: A randomized controlled trial. Physiother. Res. Int. 2019, 25, e1798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozkul, C.; Guclu-Gunduz, A.; Eldemir, K.; Apaydin, Y.; Yazici, G.; Irkec, C. Combined exercise training improves cognitive functions in multiple sclerosis patients with cognitive impairment: A single-blinded randomized controlled trial. Mult. Scler. Relat. Disord. 2020, 45, 102419. [Google Scholar] [CrossRef] [PubMed]
- Banitalebi, E.; Ghahfarrokhi, M.M.; Negaresh, R.; Kazemi, A.; Faramarzi, M.; Motl, R.W.; Zimmer, P. Exercise improves neurotrophins in multiple sclerosis independent of disability status. Mult. Scler. Relat. Disord. 2020, 43, 102143. [Google Scholar] [CrossRef] [PubMed]
- Abasıyanık, Z.; Ertekin, Ö.; Kahraman, T.; Yigit, P.; Özakbaş, S. The effects of Clinical Pilates training on walking, balance, fall risk, respiratory, and cognitive functions in persons with multiple sclerosis: A randomized controlled trial. Explore 2020, 16, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Fleming, K.; Coote, S.; Herring, M. The feasibility of Pilates to improve symptoms of anxiety, depression, and fatigue among people with Multiple Sclerosis: An eight-week randomized controlled pilot trial. Psychol. Sport Exerc. 2019, 45, 101573. [Google Scholar] [CrossRef]
- Eftekhari, E.; Etemadifar, M. Impact of Clinical Mat Pilates on Body Composition and Functional Indices in Female Patients with Multiple Sclerosis. Crescent J. Med. Biol. Sci. 2018, 5, 297–305. [Google Scholar]
- Ozkul, C.; Guclu-Gunduz, A.; Irkec, C.; Fidan, I.; Aydin, Y.; Ozkan, T.; Yazici, G. Effect of combined exercise training on serum brain-derived neurotrophic factor, suppressors of cytokine signaling 1 and 3 in patients with multiple sclerosis. J. Neuroimmunol. 2018, 316, 121–129. [Google Scholar] [CrossRef]
- Duff, W.R.; Andrushko, J.; Renshaw, D.W.; Chilibeck, P.D.; Farthing, J.P.; Danielson, J.; Evans, C.D. Impact of Pilates Exercise in Multiple Sclerosis. Int. J. MS Care 2018, 20, 92–100. [Google Scholar] [CrossRef] [Green Version]
- Eftekhari, E.; Etemadifar, M. Interleukin-10 and brain-derived neurotrophic factor responses to the Mat Pilates training in women with multiple sclerosis. Sci. Med. 2018, 28, 31668. [Google Scholar] [CrossRef]
- Kalron, A.; Rosenblum, U.; Frid, L.; Achiron, A. Pilates exercise training vs. physical therapy for improving walking and balance in people with multiple sclerosis: A randomized controlled trial. Clin. Rehabilitation 2016, 31, 319–328. [Google Scholar] [CrossRef]
- Bulguroglu, I.; Guclu-Gunduz, A.; Yazici, G.; Ozkul, C.; Irkec, C.; Nazliel, B.; Batur-Caglayan, H. The effects of Mat Pilates and Reformer Pilates in patients with Multiple Sclerosis: A randomized controlled study. NeuroRehabilitation 2017, 41, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Kara, B.; Küçük, F.; Poyraz, E.C.; Tomruk, M.S.; Idıman, E. Different types of exercise in Multiple Sclerosis: Aerobic exercise or Pilates, a single-blind clinical study. J. Back Musculoskelet. Rehabilitation 2017, 30, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Fox, E.E.; Hough, A.D.; Creanor, S.; Gear, M.; Freeman, J.A. Effects of Pilates-Based Core Stability Training in Ambulant People with Multiple Sclerosis: Multicenter, Assessor-Blinded, Randomized Controlled Trial. Phys. Ther. 2016, 96, 1170–1178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kucuk, F.; Kara, B.; Poyraz, E.C.; Idiman, E. Improvements in cognition, quality of life, and physical performance with clinical Pilates in multiple sclerosis: A randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 761–768. [Google Scholar] [CrossRef] [Green Version]
- Hosseini Sisi, S.Z.; Sadeghi, H.; Massood Nabavi, S. The effects of 8 weeks of rebound therapy and Pilates practices on static and dynamic balances in males with multiple sclerosis. Adv. Environ. Biol. 2014, 7, 4290–4293. [Google Scholar]
- Guclu-Gunduz, A.; Citaker, S.; Irkec, C.; Nazliel, B.; Batur-Caglayan, H.Z. The effects of pilates on balance, mobility and strength in patients with multiple sclerosis. NeuroRehabilitation 2014, 34, 337–342. [Google Scholar] [CrossRef]
- Marandi, S.M.; Nejad, V.S.; Shanazari, Z.; Zolaktaf, V. A Comparison of 12 Weeks of Pilates and Aquatic Training on the Dynamic Balance of Women with Mulitple Sclerosis. Int. J. Prev. Med. 2013, 4, S110–S117. [Google Scholar]
- Sánchez-Lastra, M.A.; Martínez-Aldao, D.; Molina, A.J.; Ayán, C. Pilates for people with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2019, 28, 199–212. [Google Scholar] [CrossRef]
- Middleton, L.E.; Barnes, D.E.; Lui, L.-Y.; Yaffe, K. Physical Activity over the Life Course and Its Association with Cognitive Performance and Impairment in Old Age. J. Am. Geriatr. Soc. 2010, 58, 1322–1326. [Google Scholar] [CrossRef]
- Giesser, B.S. Exercise in the management of persons with multiple sclerosis. Ther. Adv. Neurol. Disord. 2015, 8, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Willey, J.Z.; Gardener, H.; Caunca, M.R.; Moon, Y.P.; Dong, C.; Cheung, Y.K.; Sacco, R.L.; Elkind, M.S.; Wright, C.B. Leisure-time physical activity associates with cognitive decline. Neurology 2016, 86, 1897–1903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanderbeken, I.; Kerckhofs, E. A systematic review of the effect of physical exercise on cognition in stroke and traumatic brain injury patients: The Northern Manhattan Study. NeuroRehabilitation 2017, 40, 33–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques, K.A.P.; Trindade, C.B.B.; Almeida, M.C.V.; Bento-Torres, N.V.O. Pilates for rehabilitation in patients with multiple sclerosis: A systematic review of effects on cognition, health-related physical fitness, general symptoms and quality of life. J. Bodyw. Mov. Ther. 2020, 24, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Washington, F.; Langdon, D. Factors affecting adherence to disease-modifying therapies in multiple sclerosis: Systematic review. J. Neurol. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
| Variables | Main Findings with Pilates Method | Other Findings |
|---|---|---|
| Balance | ||
| Gait | ||
| Physical-functional conditions | ||
| Fatigue |
| |
| Quality of life |
|
|
| Cognitive function | ||
| Psychological function | ||
| Adherence |
| |
| Adverse effects and dropouts |
|
| Study and Year | MS Type (Patients in Pilates Group) | Mean EDSS Score ± sd (Range) | Weeks | Session per Week | Session Duration (min) | Type of Pilates | Pilates Session (Number When Conducted in Group) | Professional | Adverse Events (Case) | Pilates Training Program |
|---|---|---|---|---|---|---|---|---|---|---|
| Güngör et al. [28], 2021 | RRMS (34)/SPMS (8) | (1–5.5) | 8 | 2 | 60–75 | Floor mat work | Individual | Physiotherapist | No | Yes (in Supplementary Material) |
| Fleming et al. [29], 2021 | NA | <3 (PDDS) | 8 | 2 | 60 | Floor mat work | Individual | Certified Pilates instructor | No | Yes (in a previous study) |
| Gheitasi et al. [30], 2021 | NA | 4.6 ± 1.6 (3–5) | 12 | 3 | 60 | Floor mat work | Unclear | NA | No | No |
| Arntzen et al. [31], 2020 | RRMS (32)/PPMS (5)/SPMS (2) | 2.45 ± 1.65 (1–6.5) | 6 | 3 | 60 | Floor mat work | Group (3) | Neurological physiotherapists | Yes (1) | Yes (in a previous study) |
| Ozkul et al. [32], 2020 | RRMS (17) | 1.50 ± 0.77 (<4) | 8 | 3 | 60 | Floor mat work | NA | Physiotherapist | No | Yes |
| Banitalebi et al. [33], 2020 | RRMS (47) | 23 (0–4) + 13 (4.5–6) + 11 (6.5–8) | 12 | 3 | 15/100 | NA | NA | NA | NA | No |
| Abasiyanik et al. [34], 2020 | RRMS (14)/SPMS (2) | 3.06 ± 1.65 (<6) | 8 | 1 (+2 at home) | 55–60 | Floor mat work | Group (2–3) | Certified Pilates physiotherapist | No | Yes |
| Fleming et al. [35], 2019 | NA | <3 (PDDS) | 8 | 2 | 60 | Floor mat work | Individual | Certified Pilates instructor | No | Yes |
| Eftekhari and Etemadifar [36], 2018 | RRMS (13) | 2–6 | 8 | 3 | 50–60 | Floor mat work | NA | NA | NA | Yes |
| Ozkul tel al. [37], 2018 | RRMS | 1 (0.87–2.12) | 8 | 3 | 60 | Floor mat work | NA | Physiotherapist | Yes (3) | Yes |
| Duff et al. [38], 2018 | RRMS (14)/PPMS (1) | 2.1 ± 1.8 (range 0–5, PDDS) | 12 | 2 | 50 | Apparatus work and floor mat work | Group (5–10) | Certified Pilates instructor | No | No |
| Eftekhari and Etemadifar [39], 2018 | RRMS(13) | 2–6 | 8 | 3 | 40–50 | Floor mat work | NA | NA | NA | Yes |
| Kalron et al. [40], 2017 | RRMS (22) | 4.3 ± 1.3 (3–6) | 12 | 1 | 30 | NA | Individual | Certified Pilates physiotherapist | No | No |
| Bulguroglu et al. [41], 2017 | NA | <4.5 | 8 | 2 | 60–90 | Floor mat work or Reformer work | Individual | Certified Pilates physiotherapist | NA | No |
| Kara et al. [42], 2017 | RRMS (9) | 2.85 ± 1.57 (≤6) | 8 | 2 | 45–60 | Floor mat work | NA | Physiotherapist | Yes (4) | Yes |
| Fox et al. [43], 2016 | RRMS (13/PPMS (12)/SPMS (8) | 4–6.5 | 12 | 1 | 30 | Floor mat work | Individual | Certified Pilates physiotherapist | No | Yes (in a previous study) |
| Küçük et al. [44], 2016 | NA | 3.2 ± 2.2 (≤6) | 8 | 2 | 45–60 | Floor mat work | Group | Physiotherapist | NA | Yes |
| Hosseini Sisi et al. [45], 2014 | NA | 0–4 | 8 | 3 | 60 | NA | NA | NA | NA | No |
| Guclu-Cunduz et al. [46], 2014 | NA | 2 (0–4) | 8 | 2 | 60 | NA | Group | Certified Pilates physiotherapist | No | No |
| Marandi et al. [47], 2013 | NA | <4.5 | 12 | 3 | 60 | NA | NA | NA | NA | No |
| Study and Year | Sample Size Calculation | #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | #11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Güngör et al. [28], 2021 | Yes | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 6/10 |
| Fleming et al. [29], 2021 | Yes | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7/10 |
| Gheitasi et al. [30], 2021 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 |
| Arntzen et al. [31], 2020 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| Ozkul et al. [32], 2020 | Yes | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| Banitalebi et al. [33], 2020 | No | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 6/10 |
| Abasiyanik et al. [34], 2020 | Yes | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| Fleming et al. [35], 2019 | No | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 4/10 |
| Eftekhari and Etemadifar [36], 2018 | No | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 5/10 |
| Ozkul tel al. [37], 2018 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 6/10 |
| Duff et al. [38], 2018 | Yes | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7/10 |
| Eftekhari and Etemadifar [39], 2018 | No | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 |
| Kalron et al. [40], 2017 | No | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 |
| Bulguroglu et al. [41], 2017 | No | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 5/10 |
| Kara et al. [42], 2017 | No | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 3/10 |
| Fox et al. [43], 2016 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| Küçük et al. [44], 2016 | No | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Hosseini Sisi et al. [45], 2014 | No | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3/10 |
| Guclu-Cunduz et al. [46], 2014 | No | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 5/10 |
| Marandi et al. [47], 2013 | No | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3/10 |
| 17 | 16 | 9 | 15 | 1 | 0 | 10 | 10 | 6 | 15 | 17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Fuentes, G.; Silveira-Pereira, L.; Ferradáns-Rodríguez, P.; Campo-Prieto, P. Therapeutic Effects of the Pilates Method in Patients with Multiple Sclerosis: A Systematic Review. J. Clin. Med. 2022, 11, 683. https://doi.org/10.3390/jcm11030683
Rodríguez-Fuentes G, Silveira-Pereira L, Ferradáns-Rodríguez P, Campo-Prieto P. Therapeutic Effects of the Pilates Method in Patients with Multiple Sclerosis: A Systematic Review. Journal of Clinical Medicine. 2022; 11(3):683. https://doi.org/10.3390/jcm11030683
Chicago/Turabian StyleRodríguez-Fuentes, Gustavo, Lucía Silveira-Pereira, Pedro Ferradáns-Rodríguez, and Pablo Campo-Prieto. 2022. "Therapeutic Effects of the Pilates Method in Patients with Multiple Sclerosis: A Systematic Review" Journal of Clinical Medicine 11, no. 3: 683. https://doi.org/10.3390/jcm11030683
APA StyleRodríguez-Fuentes, G., Silveira-Pereira, L., Ferradáns-Rodríguez, P., & Campo-Prieto, P. (2022). Therapeutic Effects of the Pilates Method in Patients with Multiple Sclerosis: A Systematic Review. Journal of Clinical Medicine, 11(3), 683. https://doi.org/10.3390/jcm11030683







