Prognostic Value of Systemic Immune-Inflammation Index (SII) in Patients with Glioblastoma: A Comprehensive Study Based on Meta-Analysis and Retrospective Single-Center Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedures of Meta-Analysis
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Study Selection and Data Extraction
2.5. Quality Evaluation
2.6. Inclusion and Exclusion Criteria for GBM Patients
2.7. Ethics Approval
2.8. Data Collection
2.9. Statistical Analysis
3. Results
3.1. A Meta-Analysis Evaluating the Prognosis of SII in Patients with GBM
3.2. Publication Bias
3.3. Clinical Characteristics of GBM Patients from the Single-Center
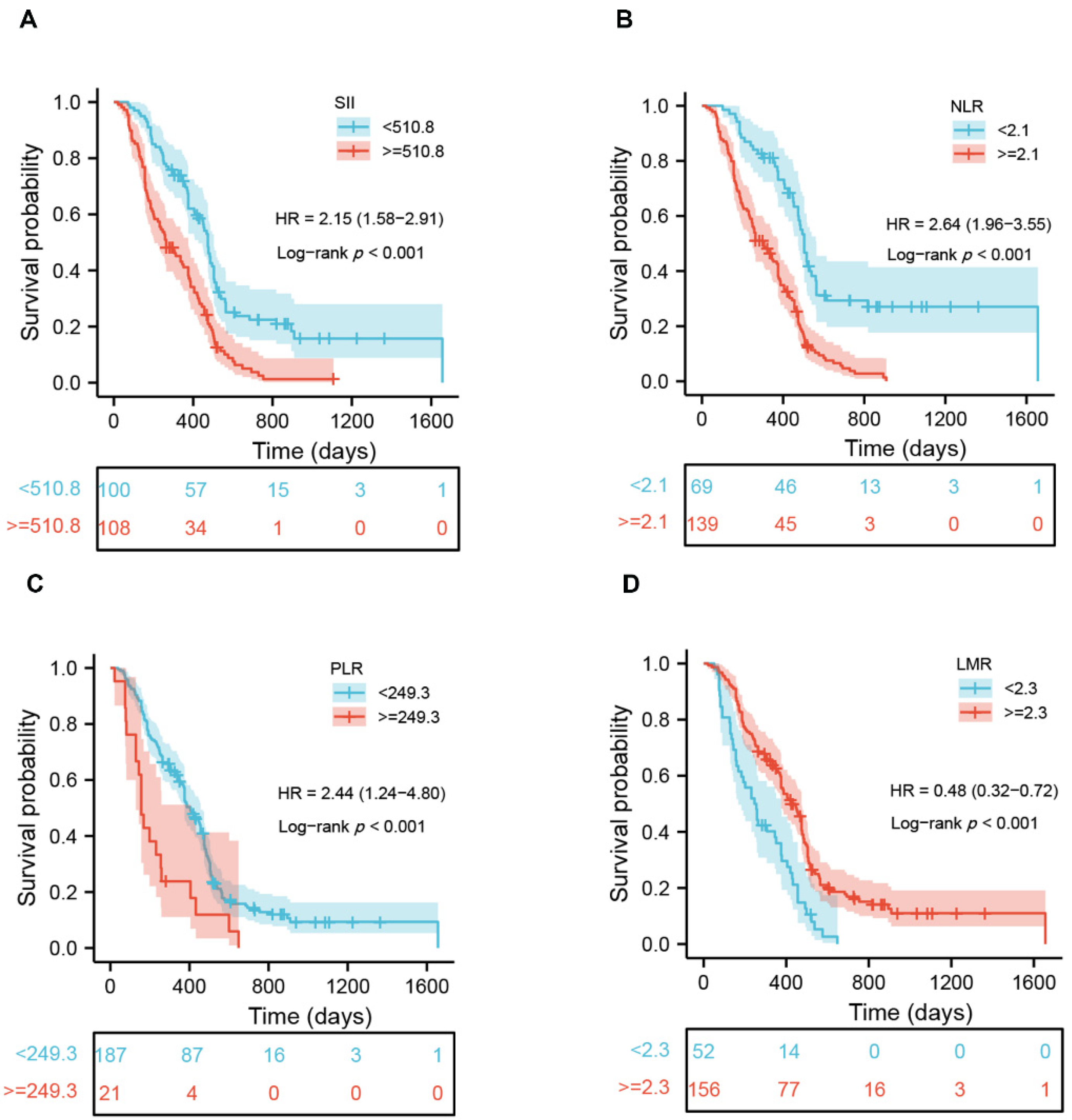
3.4. Prognostic Significance of Peripheral Inflammatory Markers in Patients with GBM
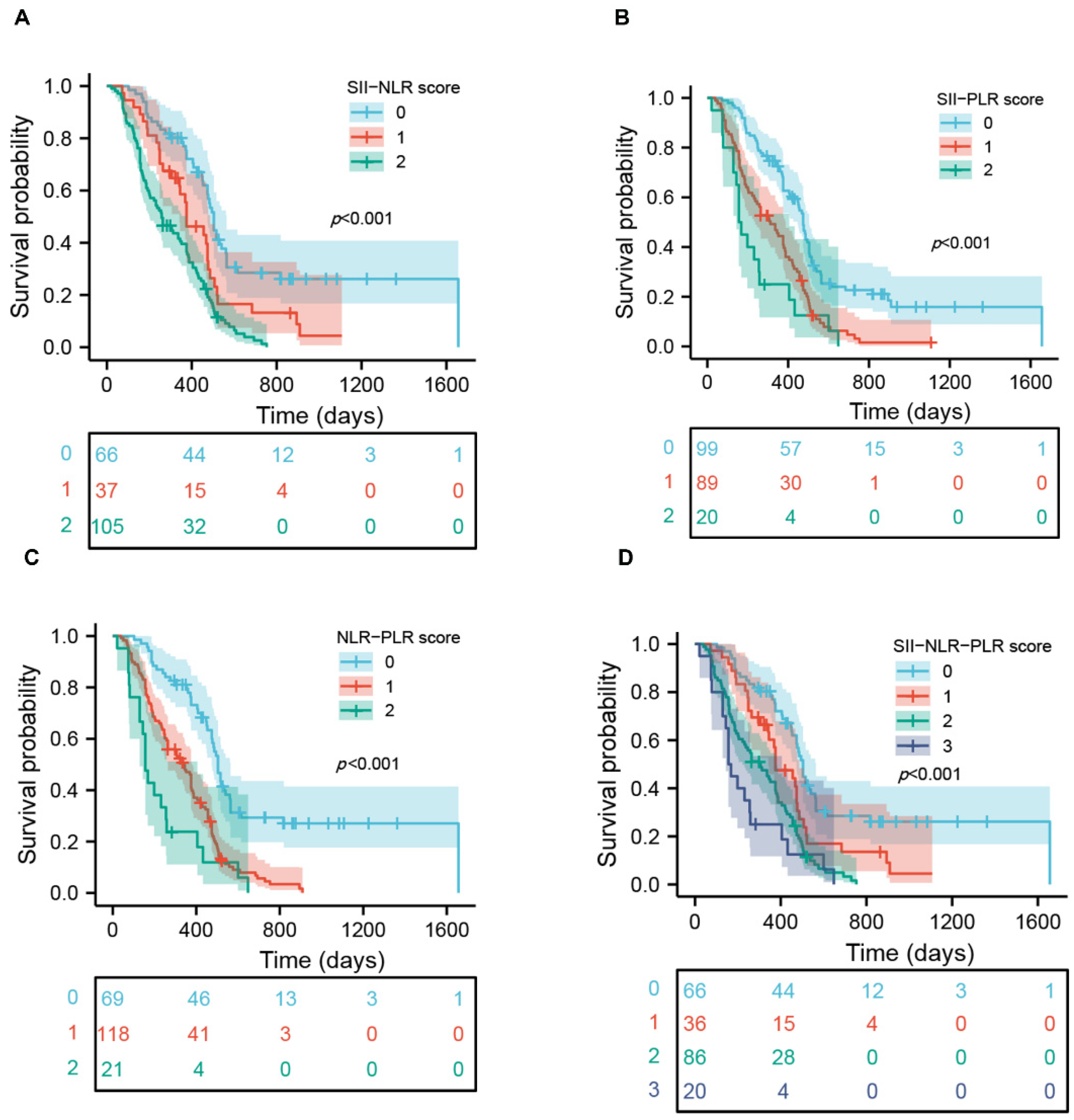
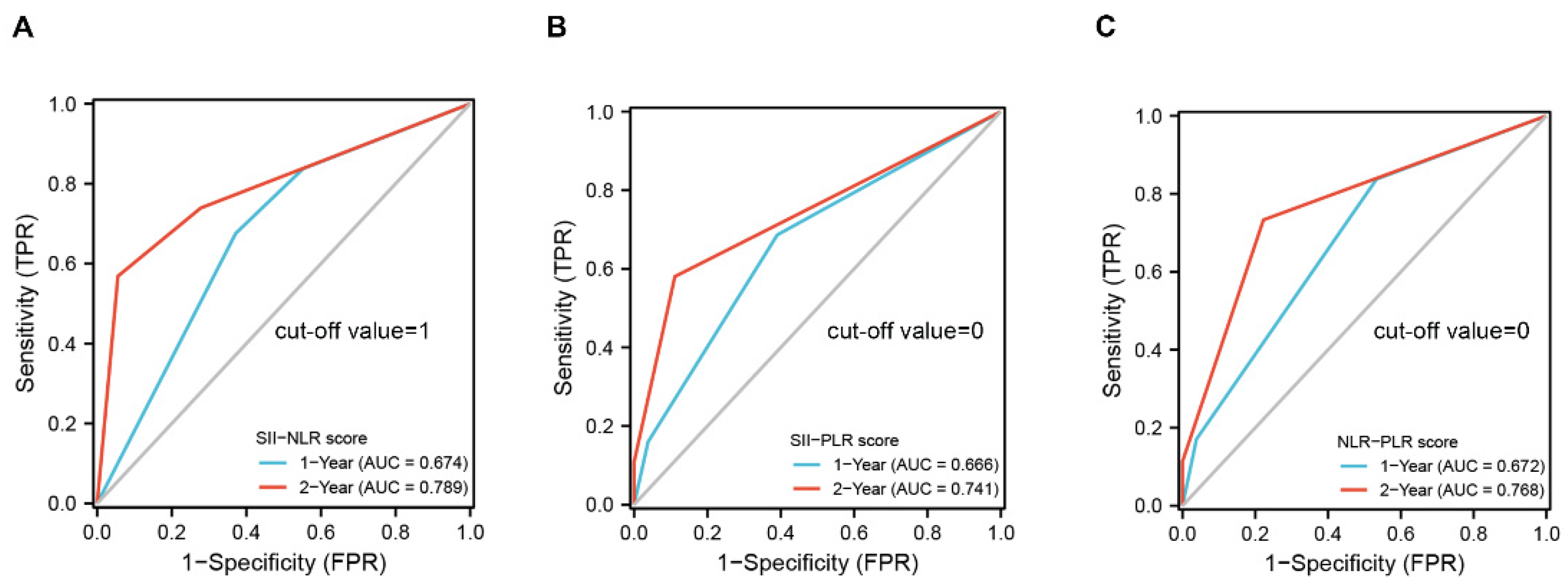
3.5. Prognostic Significance of Scoring Systems in Patients with GBM
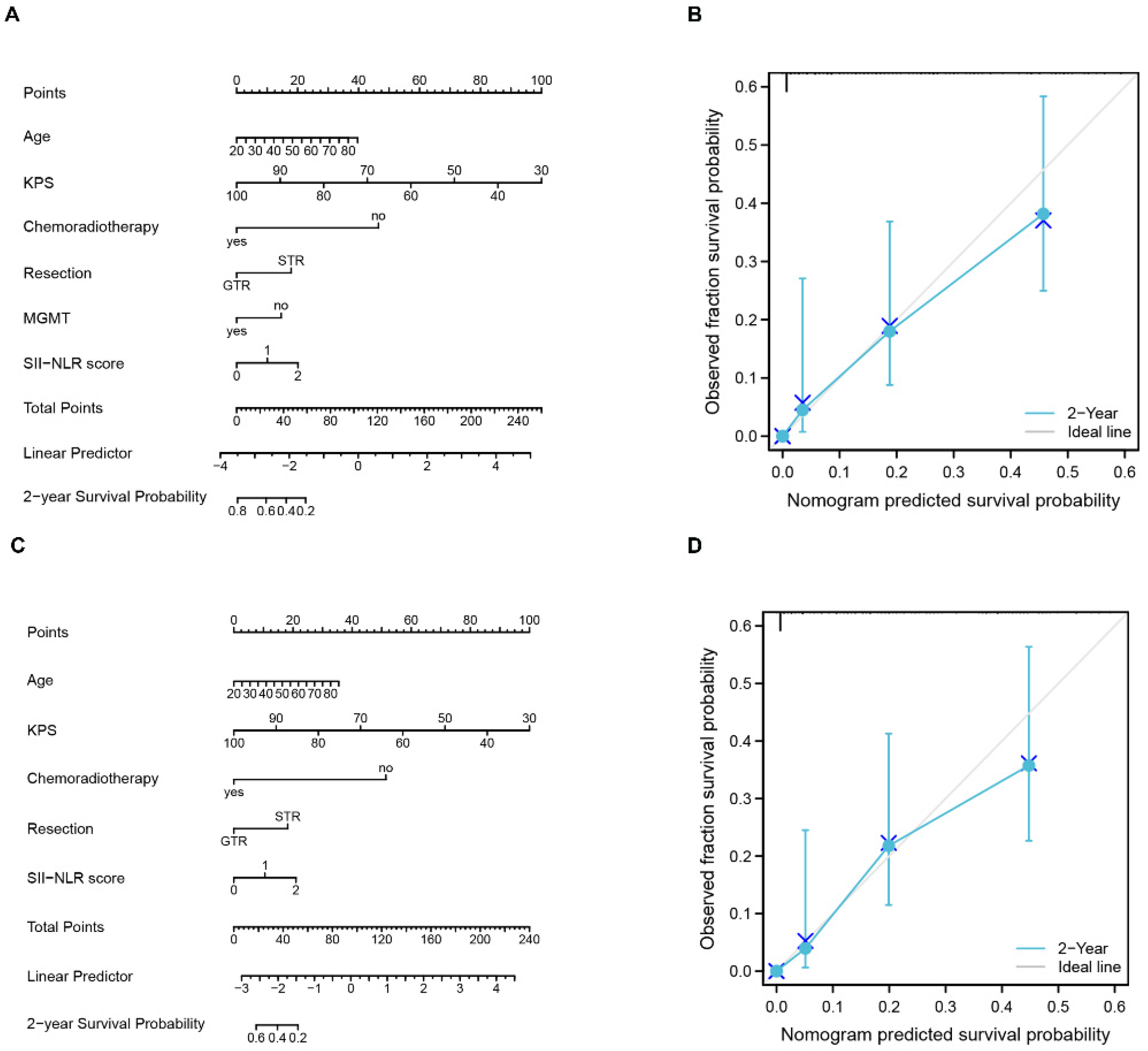
3.6. Nomograms for Predicting OS in Patients with GBM
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wesseling, P.; Capper, D. WHO 2016 Classification of gliomas. Neuropathol. Appl. Neurobiol. 2018, 44, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: A randomized clinical trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.-H.; Wang, X.; Cao, C.-J.; Weng, H.; Xu, C.-S.; Li, K.; Li, J.-L.; Lan, J.; Zeng, X.-T.; Li, Z.-Q. The Clinical Significance of O-Methylguanine-DNA Methyltransferase Promoter Methylation Status in Adult Patients With Glioblastoma: A Meta-analysis. Front. Neurol. 2018, 9, 127. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Weinberg. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444. [Google Scholar] [CrossRef]
- Albulescu, R.; Codrici, E.; Popescu, I.D.; Mihai, S.; Necula, L.G.; Petrescu, D.; Teodoru, M.; Tanase, C.P. Cytokine patterns in brain tumour progression. Mediat. Inflamm. 2013, 2013, 979748. [Google Scholar] [CrossRef]
- Yang, C.; Wen, H.-B.; Zhao, Y.-H.; Huang, W.-H.; Wang, Z.-F.; Li, Z.-Q. Systemic Inflammatory Indicators as Prognosticators in Glioblastoma Patients: A Comprehensive Meta-Analysis. Front. Neurol. 2020, 11, 580101. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Chen, P.; Xu, W.; Wu, Y.; Che, G. Prognostic value of the pretreatment systemic immune-inflammation index (SII) in patients with non-small cell lung cancer: A meta-analysis. Ann. Transl. Med. 2019, 7, 433. [Google Scholar] [CrossRef]
- Hu, H.; Yao, X.; Xie, X.; Wu, X.; Zheng, C.; Xia, W.; Ma, S. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J. Urol. 2017, 35, 261–270. [Google Scholar] [CrossRef]
- Massara, M.; Persico, P.; Bonavita, O.; Poeta, V.M.; Locati, M.; Simonelli, M.; Bonecchi, R. Neutrophils in Gliomas. Front. Immunol. 2017, 8, 1349. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Kang, K.; Lin, Q.; Hai, J. Prognostic Significance of Preoperative Systemic Cellular Inflammatory Markers in Gliomas: A Systematic Review and Meta-Analysis. Clin. Transl. Sci. 2020, 13, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Li, M.; Bo, C.; Liu, X.; Zhang, J.; Li, Z.; Zhao, F.; Kong, L.; Yu, J. Prognostic significance of the lymphocyte-to-monocyte ratio and the tumor-infiltrating lymphocyte to tumor-associated macrophage ratio in patients with stage T3N0M0 esophageal squamous cell carcinoma. Cancer Immunol. Immunother. 2017, 66, 343–354. [Google Scholar] [CrossRef]
- Yang, C.; Lan, T.; Wang, Y.; Huang, W.-H.; Li, S.-M.; Li, J.; Li, F.-P.; Li, Y.-R.; Wang, Z.-F.; Li, Z.-Q. Cumulative scoring systems and nomograms for predicating survival in patients with glioblastomas: A study based on peripheral inflammatory markers. Front. Oncol. 2022, 12, 716295. [Google Scholar] [CrossRef]
- Haemmerle, M.; Stone, R.L.; Menter, D.G.; Afshar-Kharghan, V.; Sood, A.K. The platelet lifeline to cancer: Challenges and opportunities. Cancer Cell 2018, 33, 965–983. [Google Scholar] [CrossRef]
- Aziz, M.H.; Sideras, K.; Aziz, N.A.; Mauff, K.; Haen, R.; Roos, D.; Saida, L.; Suker, M.; van der Harst, E.; Mieog, J.S.; et al. The Systemic-immune-inflammation index independently predicts survival and recurrence in resectable pancreatic cancer and its prognostic value depends on bilirubin levels: A retrospective multicenter cohort study. Ann. Surg. 2019, 270, 139–146. [Google Scholar] [CrossRef]
- Li, W.; Ma, G.; Deng, Y.; Chen, W.; Liu, Z.; Chen, F.; Wu, Q. Systemic Immune-Inflammation Index Is a Prognostic Factor for Breast Cancer Patients After Curative Resection. Front. Oncol. 2021, 11, 570208. [Google Scholar] [CrossRef]
- Hu, B.; Yang, X.-R.; Xu, Y.; Sun, Y.-F.; Sun, C.; Guo, W.; Zhang, X.; Wang, W.-M.; Qiu, S.-J.; Zhou, J.; et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin. Cancer Res. 2014, 20, 6212–6222. [Google Scholar] [CrossRef]
- Topkan, E.; Besen, A.A.; Ozdemir, Y.; Küçük, A.; Mertsoylu, H.; Pehlivan, B.; Selek, U. Prognostic Value of Pretreatment Systemic Immune-Inflammation Index in Glioblastoma Multiforme Patients Undergoing Postneurosurgical Radiotherapy Plus Concurrent and Adjuvant Temozolomide. Mediat. Inflamm. 2020, 2020, 4392189. [Google Scholar] [CrossRef]
- Shi, X.; Li, H.; Xu, Y.; Nyalali, A.M.K.; Li, F. The prognostic value of the preoperative inflammatory index on the survival of glioblastoma patients. Neurol. Sci. 2022, 43, 5523–5531. [Google Scholar] [CrossRef]
- Pasqualetti, F.; Giampietro, C.; Montemurro, N.; Giannini, N.; Gadducci, G.; Orlandi, P.; Natali, E.; Chiarugi, P.; Gonnelli, A.; Cantarella, M.; et al. Old and new systemic immune-inflammation indexes are associated with overall survival of glioblastoma patients treated with radio-chemotherapy. Genes 2022, 13, 1054. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, H.; Niğdelioğlu, B.; Oktay, E.; Meydan, N. Clinical significance of postoperatif controlling nutritional status (CONUT) score in glioblastoma multiforme. J. Clin. Neurosci. 2021, 86, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Lv, Y.; Zhang, S.; Liu, Z.; Tian, Y.; Liang, N.; Zhang, J. Prognostic value of preoperative neutrophil to lymphocyte ratio is superior to systemic immune inflammation index for survival in patients with Glioblastoma. Clin. Neurol. Neurosurg. 2019, 181, 24–27. [Google Scholar] [CrossRef]
- Wang, D.; Hu, X.; Xiao, L.; Long, G.; Yao, L.; Wang, Z.; Zhou, L. Prognostic Nutritional Index and Systemic Immune-Inflammation Index Predict the Prognosis of Patients with HCC. J. Gastrointest. Surg. 2021, 25, 421–427. [Google Scholar] [CrossRef]
- Zhou, Y.; Dai, M.; Zhang, Z. Prognostic significance of the systemic immune-inflammation index (SII) in patients with small cell lung cancer: A meta-analysis. Front. Oncol. 2022, 12, 814727. [Google Scholar] [CrossRef]
- Jin, M.; Yuan, S.; Yuan, Y.; Yi, L. Prognostic and clinicopathological significance of the systemic immune-inflammation index in patients with renal cell carcinoma: A meta-analysis. Front. Oncol. 2021, 11, 735803. [Google Scholar] [CrossRef]
- Lei, H.; Xu, S.; Mao, X.; Chen, X.; Chen, Y.; Sun, X.; Sun, P. Systemic immune-inflammatory index as a predictor of lymph node metastasis in endometrial cancer. J. Inflamm. Res. 2021, 14, 7131–7142. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kawada, K.; Obama, K. Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int. J. Mol. Sci. 2021, 22, 8002. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Deng, Q.; Pan, Y.; He, B.; Ying, H.; Sun, H.; Liu, X.; Wang, S. Prognostic value of neutrophil-to-lymphocyte ratio in breast cancer. FEBS. Open Bio. 2015, 5, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Geng, Y.; Shao, Y.; Zhu, D.; Zheng, X.; Zhou, Q.; Zhou, W.; Ni, X.; Wu, C.; Jiang, J. Systemic immune-inflammation index predicts prognosis of patients with esophageal squamous cell carcinoma: A propensity score-matched analysis. Sci. Rep. 2016, 6, 39482. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, J.R.; Lung, T.J.; Hirsch, Y.; Katz, E.A.; Cheng, T.; Saini, N.S.; Pandey, D.K.; Testai, F.D. Systemic immune-inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery 2021, 89, 1071–1079. [Google Scholar] [CrossRef]
- Ruta, V.M.; Man, A.M.; Alexescu, T.G.; Motoc, N.S.; Tarmure, S.; Ungur, R.A.; Todea, D.A.; Coste, S.C.; Valean, D.; Pop, M.C. Neutrophil-To-Lymphocyte ratio and systemic immune-inflammation index-biomarkers in interstitial lung disease. Medicina 2020, 56, 381. [Google Scholar] [CrossRef]
- McCourt, M.; Wang, J.H.; Sookhai, S.; Redmond, H.P. Proinflammatory mediators stimulate neutrophil-directed angiogenesis. Arch. Surg. 1999, 134, 1325–1331. [Google Scholar] [CrossRef]
- Jabłońska, E.; Kiluk, M.; Markiewicz, W.; Piotrowski, L.; Grabowska, Z.; Jabłoński, J. TNF-alpha, IL-6 and their soluble receptor serum levels and secretion by neutrophils in cancer patients. Arch. Immunol. Ther. Exp. 2001, 49, 63–69. [Google Scholar]
- Schaider, H.; Oka, M.; Bogenrieder, T.; Nesbit, M.; Satyamoorthy, K.; Berking, C.; Matsushima, K.; Herlyn, M. Differential response of primary and metastatic melanomas to neutrophils attracted by IL. Int. J. Cancer 2003, 103, 335–343. [Google Scholar] [CrossRef]
- Mizuno, R.; Kawada, K.; Sakai, Y. Prostaglandin E2/EP Signaling in the tumor microenvironment of colorectal cancer. Int. J. Mol. Sci. 2019, 20, 6254. [Google Scholar] [CrossRef]
- Shamamian, P.; Schwartz, J.D.; Pocock, B.J.; Monea, S.; Whiting, D.; Marcus, S.G.; Mignatti, P. Activation of progelatinase A (MMP-2) by neutrophil elastase, cathepsin G, and proteinase-3: A role for inflammatory cells in tumor invasion and angiogenesis. J. Cell Physiol. 2001, 189, 197–206. [Google Scholar] [CrossRef]
- Gregory, A.D.; Houghton, A.M. Tumor-associated neutrophils: New targets for cancer therapy. Cancer Res. 2011, 71, 2411–2416. [Google Scholar] [CrossRef] [PubMed]
- Del Prete, A.; Allavena, P.; Santoro, G.; Fumarulo, R.; Corsi, M.M.; Mantovani, A. Molecular pathways in cancer-related inflammation. Biochem. Med. 2011, 21, 264–275. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.; Liebertz, D.J.; Epstein, A.L. Characterization of cytokine-induced myeloid-derived suppressor cells from normal human peripheral blood mononuclear cells. J. Immunol. 2010, 185, 2273–2284. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Liu, Y.; Li, Q.; Li, Z.; Hou, H.; Wu, A. Pre-treatment neutrophil-to-lymphocyte ratio is associated with neutrophil and T-cell infiltration and predicts clinical outcome in patients with glioblastoma. BMC Cancer 2015, 15, 617. [Google Scholar] [CrossRef]
- Di Vito, C.; Navone, S.E.; Marfia, G.; Hadi, L.A.; Mancuso, M.E.; Pecci, A.; Crisà, F.M.; Berno, V.; Rampini, P.; Campanella, R.; et al. Platelets from glioblastoma patients promote angiogenesis of tumor endothelial cells and exhibit increased VEGF content and release. Platelets 2017, 28, 585–594. [Google Scholar] [CrossRef]
- Westermark, B.; Heldin, C.; Nistér, M. Platelet-derived growth factor in human glioma. Glia 1995, 15, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Wojtukiewicz, M.Z.; Sierko, E.; Hempel, D.; Tucker, S.C.; Honn, K.V. Platelets and cancer angiogenesis nexus. Cancer Metastasis Rev. 2017, 36, 249–262. [Google Scholar] [CrossRef]
- Labelle, M.; Begum, S.; Hynes, R.O. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell 2011, 20, 576–590. [Google Scholar] [CrossRef]
- Gooden, M.J.M.; de Bock, G.H.; Leffers, N.; Daemen, T.; Nijman, H.W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: A systematic review with meta-analysis. Br. J. Cancer 2011, 105, 93–103. [Google Scholar] [CrossRef]
- Liang, R.; Chen, N.; Li, M.; Wang, X.; Mao, Q.; Liu, Y. Significance of systemic immune-inflammation index in the differential diagnosis of high. and low-grade gliomas. Clin. Neurol. Neurosurg. 2018, 164, 50–52. [Google Scholar] [CrossRef]
- De Giorgi, U.; Procopio, G.; Giannarelli, D.; Sabbatini, R.; Bearz, A.; Buti, S.; Basso, U.; Mitterer, M.; Ortega, C.; Bidoli, P.; et al. Association of systemic inflammation index and body mass index with survival in patients with renal cell cancer treated with nivolumab. Clin. Cancer Res. 2019, 25, 3839–3846. [Google Scholar] [CrossRef]
- Diem, S.; Schmid, S.; Krapf, M.; Flatz, L.; Born, D.; Jochum, W.; Templeton, A.J.; Früh, M. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer 2017, 111, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Valero, C.; Lee, M.; Hoen, D.; Weiss, K.; Kelly, D.W.; Adusumilli, P.S.; Paik, P.K.; Plitas, G.; Ladanyi, M.; Postow, M.A.; et al. Pretreatment neutrophil-to-lymphocyte ratio and mutational burden as biomarkers of tumor response to immune checkpoint inhibitors. Nat. Commun. 2021, 12, 728. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Feng, Y.; Zhang, Y.; Liu, H. Evaluation of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio on predicting responsiveness to neoadjuvant chemoradiotherapy in locally advanced rectal cancer patients. Biomed. Res. Int. 2022, 2022, 3839670. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | SII < 510.8 | SII ≥ 510.8 | p |
|---|---|---|---|
| n | 100 | 108 | |
| Sex, n (%) | 0.244 | ||
| female | 45 (21.6%) | 39 (18.8%) | |
| male | 55 (26.4%) | 69 (33.2%) | |
| Location, n (%) | 0.667 | ||
| frontal | 32 (15.4%) | 31 (14.9%) | |
| temporal | 27 (13%) | 26 (12.5%) | |
| parietal | 12 (5.8%) | 10 (4.8%) | |
| multiple | 15 (7.2%) | 18 (8.7%) | |
| other | 14 (6.7%) | 23 (11.1%) | |
| KPS, n (%) | <0.001 | ||
| ≤50 | 11 (11.0%) | 37 (34.2%) | |
| >50 | 89 (89.0%) | 71 (65.8%) | |
| Chemoradiotherapy, n (%) | <0.001 | ||
| no | 18 (8.7%) | 45 (21.6%) | |
| yes | 82 (39.4%) | 63 (30.3%) | |
| Resection, n (%) | <0.001 | ||
| STR | 26 (12.5%) | 57 (27.4%) | |
| GTR | 74 (35.6%) | 51 (24.5%) | |
| MGMT, n (%) | 1.000 | ||
| no | 57 (27.4%) | 62 (29.8%) | |
| yes | 43 (20.7%) | 46 (22.1%) | |
| Age, median (IQR) | 58 (51.75, 65) | 59 (51, 65) | 0.956 |
| WBC, median (IQR) | 5.42 (4.62, 6.39) | 7.05 (5.77, 9.17) | <0.001 |
| Neu, median (IQR) | 3.28 (2.56, 4) | 5.43 (4.11, 7.49) | <0.001 |
| Lym, median (IQR) | 1.8 (1.38, 2.13) | 1.3 (0.92, 1.62) | <0.001 |
| PLT, median (IQR) | 178.5 (143.75, 203.5) | 219 (177.5, 273.5) | <0.001 |
| OS, median (IQR) | 14.95 (9.95, 18.18) | 8.8 (5.2, 14.9) | <0.001 |
| Characteristics | Total (N) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | ||
| Sex | 208 | ||||
| male | 124 | Reference | |||
| female | 84 | 1.032 (0.761–1.400) | 0.839 | ||
| Age | 208 | 1.025 (1.011–1.040) | <0.001 | 1.025 (1.010–1.039) | <0.001 |
| Location | 208 | 1.110 (1.004–1.228) | 0.042 | 1.047 (0.944–1.162) | 0.385 |
| KPS | 208 | ||||
| ≤50 | 23 | Reference | |||
| >50 | 185 | 0.150 (0.095–0.237) | <0.001 | 0.253 (0.148–0.431) | <0.001 |
| Chemoradiotherapy | 208 | ||||
| no | 63 | Reference | |||
| yes | 145 | 0.066 (0.043–0.103) | <0.001 | 0.136 (0.075–0.245) | <0.001 |
| Resection | 208 | ||||
| STR | 83 | Reference | |||
| GTR | 125 | 0.199 (0.145–0.275) | <0.001 | 0.433 (0.276–0.680) | <0.001 |
| MGMT | 208 | ||||
| no | 121 | Reference | |||
| yes | 87 | 0.419 (0.306–0.573) | <0.001 | 0.654 (0.452–0.945) | 0.024 |
| WBC | 208 | ||||
| ≤6.7 | 127 | Reference | |||
| >6.7 | 81 | 1.622 (1.198–2.197) | 0.002 | 0.979 (0.597–1.606) | 0.934 |
| Neu | 208 | ||||
| ≤4.9 | 134 | Reference | |||
| >4.9 | 74 | 2.540 (1.863–3.461) | <0.001 | 1.040 (0.588–1.839) | 0.892 |
| Lym | 208 | ||||
| ≤1.9 | 151 | Reference | |||
| >1.9 | 57 | 0.546 (0.382–0.782) | <0.001 | 0.830 (0.550–1.251) | 0.373 |
| PLT | 208 | ||||
| ≤255 | 168 | Reference | |||
| >255 | 40 | 1.546 (1.070–2.234) | 0.020 | 0.710 (0.461–1.096) | 0.122 |
| Monocyte | 208 | ||||
| ≤0.4 | 77 | Reference | |||
| >0.4 | 131 | 1.358 (0.990–1.862) | 0.058 | 1.390 (0.945–2.047) | 0.095 |
| NLR | 208 | ||||
| ≤2.1 | 69 | Reference | |||
| >2.1 | 139 | 2.820 (1.992–3.993) | <0.001 | 1.769 (1.106–2.829) | 0.017 |
| PLR | 208 | ||||
| ≤249.3 | 187 | Reference | |||
| >249.3 | 21 | 2.478 (1.547–3.969) | <0.001 | 2.598 (1.473–4.581) | <0.001 |
| LMR | 208 | ||||
| ≤2.3 | 52 | Reference | |||
| >2.3 | 156 | 0.461 (0.328–0.646) | <0.001 | 0.899 (0.590–1.371) | 0.621 |
| SII | 208 | ||||
| ≤510.8 | 100 | Reference | |||
| >510.8 | 108 | 2.226 (1.638–3.025) | <0.001 | 1.782 (1.168–2.719) | 0.007 |
| Score | N (%) | OS (Mean ± SD) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Variables | Definition | (Months) | |||||
| SII-NLR | 208 (100) | ||||||
| Score 0 | SII < 510.8 and NLR < 2.1 | 66 (31.7) | 17.5 ± 9.9 | reference | |||
| Score 1 | SII > 510.8 or NLR > 2.1 | 37 (17.8) | 13.4 ± 7.9 | 0.012 | |||
| Score 2 | SII > 510.8 and NLR > 2.1 | 105 (50.5) | 9.8 ± 5.8 | 0.013 | |||
| SII-PLR | 208 (100) | ||||||
| Score 0 | SII < 510.8 and PLR < 249.3 | 99 (47.6) | 16.0 ± 9.2 | reference | |||
| Score 1 | SII > 510.8 or PLR > 249.3 | 89 (42.8) | 10.6 ± 6.4 | <0.001 | |||
| Score 2 | SII > 510.8 and PLR > 249.3 | 20 (9.6) | 7.7 ± 5.7 | <0.001 | |||
| NLR-PLR | 208 (100) | ||||||
| Score 0 | NLR < 2.1 and PLR < 249.3 | 69 (33.2) | 17.6 ± 10.0 | reference | |||
| Score 1 | NLR > 2.1 or PLR > 249.3 | 118 (56.7) | 11.0 ± 6.2 | <0.001 | |||
| Score 2 | NLR > 2.1 and PLR > 249.3 | 21 (10.1) | 7.4 ± 5.6 | <0.001 | |||
| SII-NLR-PLR | 208 (100) | ||||||
| Score 0 | SII < 510.8 and NLR < 2.1 and PLR < 249.3 | 66 (31.7) | 17.5 ± 9.9 | reference | |||
| Score 1 | SII > 510.8 or NLR > 2.1 or PLR > 249.3 | 36 (17.3) | 13.8 ± 7.8 | 0.022 | |||
| Score 2 | SII > 510.8 and NLR > 2.1, or SII > 510.8 and PLR > 249.3, or NLR > 2.1 and PLR > 249.3 | 86 (41.3) | 10.2 ± 5.8 | <0.001 | |||
| Score 3 | SII > 510.8 and NLR > 2.1 and PLR > 249.3 | 20 (9.6) | 7.6 ± 5.7 | <0.001 | |||
| Characteristics | Total (N) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | ||
| SII-NLR | 208 | <0.001 | |||
| Score 0 | 66 | Reference | |||
| Score 1 | 37 | 1.806 (1.139–2.865) | 0.012 | 1.679 (1.053–2.678) | 0.030 |
| Score 2 | 105 | 3.043 (2.111–4.385) | <0.001 | 2.460 (1.694–3.572) | <0.001 |
| NLR-PLR | 208 | <0.001 | |||
| Score 0 | 69 | Reference | |||
| Score 1 | 118 | 2.642 (1.852–3.769) | <0.001 | 1.844 (1.269–2.680) | 0.001 |
| Score 2 | 21 | 4.557 (2.665–7.792) | <0.001 | 3.687 (2.080–6.535) | <0.001 |
| SII-PLR | 208 | <0.001 | |||
| Score 0 | 99 | Reference | |||
| Score 1 | 89 | 2.126 (1.542–2.931) | <0.001 | 1.623 (1.161–2.267) | 0.005 |
| Score 2 | 20 | 3.332 (1.997–5.561) | <0.001 | 2.992 (1.740–5.144) | <0.001 |
| SII-NLR-PLR | 208 | <0.001 | |||
| Score 0 | 66 | Reference | |||
| Score 1 | 36 | 1.751 (1.099–2.790) | 0.018 | 1.513 (0.939–2.440) | 0.089 |
| Score 2 | 86 | 2.892 (1.983–4.216) | <0.001 | 1.961 (1.321–2.910) | <0.001 |
| Score 3 | 20 | 4.219 (2.441–7.293) | <0.001 | 3.543 (1.987–6.317) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, C.; Hu, B.-W.; Tang, F.; Zhang, Q.; Quan, W.; Wang, J.; Wang, Z.-F.; Li, Y.-R.; Li, Z.-Q. Prognostic Value of Systemic Immune-Inflammation Index (SII) in Patients with Glioblastoma: A Comprehensive Study Based on Meta-Analysis and Retrospective Single-Center Analysis. J. Clin. Med. 2022, 11, 7514. https://doi.org/10.3390/jcm11247514
Yang C, Hu B-W, Tang F, Zhang Q, Quan W, Wang J, Wang Z-F, Li Y-R, Li Z-Q. Prognostic Value of Systemic Immune-Inflammation Index (SII) in Patients with Glioblastoma: A Comprehensive Study Based on Meta-Analysis and Retrospective Single-Center Analysis. Journal of Clinical Medicine. 2022; 11(24):7514. https://doi.org/10.3390/jcm11247514
Chicago/Turabian StyleYang, Chao, Bo-Wen Hu, Feng Tang, Qing Zhang, Wei Quan, Jie Wang, Ze-Fen Wang, Yi-Rong Li, and Zhi-Qiang Li. 2022. "Prognostic Value of Systemic Immune-Inflammation Index (SII) in Patients with Glioblastoma: A Comprehensive Study Based on Meta-Analysis and Retrospective Single-Center Analysis" Journal of Clinical Medicine 11, no. 24: 7514. https://doi.org/10.3390/jcm11247514
APA StyleYang, C., Hu, B.-W., Tang, F., Zhang, Q., Quan, W., Wang, J., Wang, Z.-F., Li, Y.-R., & Li, Z.-Q. (2022). Prognostic Value of Systemic Immune-Inflammation Index (SII) in Patients with Glioblastoma: A Comprehensive Study Based on Meta-Analysis and Retrospective Single-Center Analysis. Journal of Clinical Medicine, 11(24), 7514. https://doi.org/10.3390/jcm11247514








