30-Day Postoperative Outcomes in Adults with Obstructive Sleep Apnea Undergoing Upper Airway Surgery
Abstract
1. Introduction
2. Methods
2.1. Data Source and Patient Selection
2.2. Variable Extraction
2.3. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Surgical Characteristics
3.3. Perioperative Outcomes
3.4. Postoperative Surgical and Medical Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Epstein, L.J.; Kristo, D.; Strollo, P.J., Jr.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar]
- Jordan, A.S.; White, D.P. Pharyngeal motor control and the pathogenesis of obstructive sleep apnea. Respir. Physiol. Neurobiol. 2008, 160, 1–7. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Mehra, R. Sleep apnea and the heart. Cleve Clin. J. Med. 2019, 86, 10–18. [Google Scholar] [CrossRef]
- Sabil, A.; Bignard, R.; Gerves-Pinquie, C.; Philip, P.; Le Vaillant, M.; Trzepizur, W.; Meslier, N.; Gagnadoux, F. Risk Factors for Sleepiness at the Wheel and Sleep-Related Car Accidents Among Patients with Obstructive Sleep Apnea: Data from the French Pays de la Loire Sleep Cohort. Nat. Sci. Sleep 2021, 13, 1737–1746. [Google Scholar] [CrossRef]
- Hirsch Allen, A.J.M.; Bansback, N.; Ayas, N.T. The effect of OSA on work disability and work-related injuries. Chest 2015, 147, 1422–1428. [Google Scholar] [CrossRef]
- Patil, S.P.; Ayappa, I.A.; Caples, S.M.; Kimoff, R.J.; Patel, S.R.; Harrod, C.G. Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J. Clin. Sleep Med. 2019, 15, 301–334. [Google Scholar] [CrossRef]
- Kezirian, E.J.; Maselli, J.; Vittinghoff, E.; Goldberg, A.N.; Auerbach, A.D. Obstructive sleep apnea surgery practice patterns in the United States: 2000 to 2006. Otolaryngol. Head Neck Surg. 2010, 143, 441–447. [Google Scholar] [CrossRef]
- Liao, P.; Yegneswaran, B.; Vairavanathan, S.; Zilberman, P.; Chung, F. Postoperative complications in patients with obstructive sleep apnea: A retrospective matched cohort study. Can. J. Anesth./J. Can. D’anesthésie 2009, 56, 819. [Google Scholar] [CrossRef]
- Kezirian, E.J.; Weaver, E.M.; Yueh, B.; Deyo, R.A.; Khuri, S.F.; Daley, J.; Henderson, W. Incidence of serious complications after uvulopalatopharyngoplasty. Laryngoscope 2004, 114, 450–453. [Google Scholar] [CrossRef]
- Practice guidelines for the perioperative management of patients with obstructive sleep apnea: An updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 2014, 120, 268–286. [CrossRef]
- Kaw, R.; Pasupuleti, V.; Walker, E.; Ramaswamy, A.; Foldvary-Schafer, N. Postoperative complications in patients with obstructive sleep apnea. Chest 2012, 141, 436–441. [Google Scholar] [CrossRef]
- Zaghi, S.; Holty, J.E.; Certal, V.; Abdullatif, J.; Guilleminault, C.; Powell, N.B.; Riley, R.W.; Camacho, M. Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea: A Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 58–66. [Google Scholar] [CrossRef]
- Du, A.L.; Tully, J.L.; Curran, B.P.; Gabriel, R.A. Obesity and outcomes in patients undergoing upper airway surgery for obstructive sleep apnea. PLoS ONE 2022, 17, e0272331. [Google Scholar] [CrossRef]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Lee, S.D.; Kang, S.H.; Ju, G.; Han, J.W.; Kim, T.H.; Lee, C.S.; Kim, T.; Kim, K.W.; Yoon, I.Y. The prevalence of and risk factors for sleep-disordered breathing in an elderly Korean population. Respiration 2014, 87, 372–378. [Google Scholar] [CrossRef]
- Bednarek, M.; Plywaczewski, R.; Jonczak, L.; Zielinski, J. There is no relationship between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome: A population study. Respiration 2005, 72, 142–149. [Google Scholar] [CrossRef]
- Choi, K.M.; Thomas, R.J.; Kim, J.; Lee, S.K.; Yoon, D.W.; Shin, C. Overlap syndrome of COPD and OSA in Koreans. Medicine 2017, 96, e7241. [Google Scholar] [CrossRef]
- Reitsma, M.B.; Kendrick, P.J.; Ababneh, E.; Abbafati, C.; Abbasi-Kangevari, M.; Abdoli, A.; Abedi, A.; Abhilash, E.S.; Abila, D.B.; Aboyans, V.; et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [Google Scholar] [CrossRef]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- Islami, F.; Torre, L.A.; Jemal, A. Global trends of lung cancer mortality and smoking prevalence. Transl. Lung Cancer Res. 2015, 4, 327–338. [Google Scholar] [CrossRef]
- Lin, H.C.; Weaver, E.M.; Lin, H.S.; Friedman, M. Multilevel Obstructive Sleep Apnea Surgery. Adv. Otorhinolaryngol. 2017, 80, 109–115. [Google Scholar] [CrossRef]
- Friedman, J.J.; Salapatas, A.M.; Bonzelaar, L.B.; Hwang, M.S.; Friedman, M. Changing Rates of Morbidity and Mortality in Obstructive Sleep Apnea Surgery. Otolaryngol. Head Neck Surg. 2017, 157, 123–127. [Google Scholar] [CrossRef]
- Barrera, J.E. Skeletal Surgery for Obstructive Sleep Apnea. Otolaryngol. Clin. N. Am. 2016, 49, 1433–1447. [Google Scholar] [CrossRef]
- Van Daele, D.J.; Cromwell, J.W.; Hsia, J.K.; Nord, R.S. Post-operative Complication Rate Comparison Between Airway Surgery and Upper Airway Stimulation Using NSQIP and ADHERE. OTO Open 2021, 5, 2473974X211051313. [Google Scholar] [CrossRef]
- Rosero, E.B.; Joshi, G.P. Outcomes of Sleep Apnea Surgery in Outpatient and Inpatient Settings. Anesth. Analg. 2021, 132, 1215–1222. [Google Scholar] [CrossRef]
- Saenwandee, P.; Neruntarat, C.; Saengthong, P.; Wiriyaamornchai, P.; Khuancharee, K.; Sirisomboonwech, S.; Chuoykwamdee, N. Barbed pharyngoplasty for obstructive sleep apnea: A meta-analysis. Am. J. Otolaryngol. 2022, 43, 103306. [Google Scholar] [CrossRef]
- Gafar, H.A.-L.; Abdulla, A.E.-D.A.; Ghanem, Y.Y.; Bahgat, A.Y. Comparative study between single-stage multilevel surgery and staged surgery for management of snoring and/or obstructive sleep apnea. Egypt. J. Otolaryngol. 2022, 38, 90. [Google Scholar] [CrossRef]
- Zhou, N.; Ho, J.T.F.; Huang, Z.; Spijker, R.; de Vries, N.; Aarab, G.; Lobbezoo, F.; Ravesloot, M.J.L.; de Lange, J. Maxillomandibular advancement versus multilevel surgery for treatment of obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 57, 101471. [Google Scholar] [CrossRef]
- MacKay, S.; Carney, A.S.; Catcheside, P.G.; Chai-Coetzer, C.L.; Chia, M.; Cistulli, P.A.; Hodge, J.-C.; Jones, A.; Kaambwa, B.; Lewis, R.; et al. Effect of Multilevel Upper Airway Surgery vs Medical Management on the Apnea-Hypopnea Index and Patient-Reported Daytime Sleepiness Among Patients With Moderate or Severe Obstructive Sleep Apnea: The SAMS Randomized Clinical Trial. JAMA 2020, 324, 1168–1179. [Google Scholar] [CrossRef]
- Bosco, G.; Morato, M.; Pérez-Martín, N.; Navarro, A.; Racionero, M.A.; O’Connor-Reina, C.; Baptista, P.; Plaza, G. One-Stage Multilevel Surgery for Treatment of Obstructive Sleep Apnea Syndrome. J. Clin. Med. 2021, 10, 4822. [Google Scholar] [CrossRef] [PubMed]
- Browaldh, N.; Markström, A.; Friberg, D. Elective tracheostomy is an alternative treatment in patients with severe obstructive sleep apnoea syndrome and CPAP failure. Acta Otolaryngol. 2009, 129, 1121–1126. [Google Scholar] [CrossRef][Green Version]
- Camacho, M.; Zaghi, S.; Chang, E.T.; Song, S.A.; Szelestey, B.; Certal, V. Mini Tracheostomy for Obstructive Sleep Apnea: An Evidence Based Proposal. Int. J. Otolaryngol. 2016, 2016, 7195349. [Google Scholar] [CrossRef]
- Rizzi, C.J.; Amin, J.D.; Isaiah, A.; Valdez, T.A.; Jeyakumar, A.; Smart, S.E.; Pereira, K.D. Tracheostomy for Severe Pediatric Obstructive Sleep Apnea: Indications and Outcomes. Otolaryngol. Head Neck Surg. 2017, 157, 309–313. [Google Scholar] [CrossRef]
- Camacho, M.; Certal, V.; Brietzke, S.E.; Holty, J.E.; Guilleminault, C.; Capasso, R. Tracheostomy as treatment for adult obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope 2014, 124, 803–811. [Google Scholar] [CrossRef]
- Thatcher, G.W.; Maisel, R.H. The long-term evaluation of tracheostomy in the management of severe obstructive sleep apnea. Laryngoscope 2003, 113, 201–204. [Google Scholar] [CrossRef]
- Fernandez-Bussy, S.; Mahajan, B.; Folch, E.; Caviedes, I.; Guerrero, J.; Majid, A. Tracheostomy Tube Placement: Early and Late Complications. J. Bronchol. Interv. Pulmonol. 2015, 22, 357–364. [Google Scholar] [CrossRef]
- Rosero, E.B.; Corbett, J.; Mau, T.; Joshi, G.P. Intraoperative Airway Management Considerations for Adult Patients Presenting With Tracheostomy: A Narrative Review. Anesth. Analg. 2021, 132, 1003–1011. [Google Scholar] [CrossRef]
- Cipriano, A.; Mao, M.L.; Hon, H.H.; Vazquez, D.; Stawicki, S.P.; Sharpe, R.P.; Evans, D.C. An overview of complications associated with open and percutaneous tracheostomy procedures. Int. J. Crit. Illn. Inj. Sci. 2015, 5, 179–188. [Google Scholar] [CrossRef]
- Koitschev, A.; Simon, C.; Blumenstock, G.; Mach, H.; Graumueller, S. Surgical technique affects the risk for tracheostoma-related complications in post-ICU patients. Acta Otolaryngol. 2006, 126, 1303–1308. [Google Scholar] [CrossRef]
- Kaw, R.; Gali, B.; Collop, N.A. Perioperative care of patients with obstructive sleep apnea. Curr. Treat. Options Neurol. 2011, 13, 496–507. [Google Scholar] [CrossRef] [PubMed]
- Bamba, R.; Gupta, V.; Shack, R.B.; Grotting, J.C.; Higdon, K.K. Evaluation of Diabetes Mellitus as a Risk Factor for Major Complications in Patients Undergoing Aesthetic Surgery. Aesthet. Surg. J. 2016, 36, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Dulai, M.; Tawfick, W.; Hynes, N.; Sultan, S. Female Gender as a Risk Factor for Adverse Outcomes After Carotid Revascularization. Ann. Vasc. Surg. 2019, 60, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Fitz-Henry, J. The ASA classification and peri-operative risk. Ann. R. Coll. Surg. Engl. 2011, 93, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Negus, O.J.; Watts, D.; Loveday, D.T. Diabetes: A major risk factor in trauma and orthopaedic surgery. Br. J. Hosp. Med. 2021, 82, 1–5. [Google Scholar] [CrossRef]
- Hackett, N.J.; De Oliveira, G.S.; Jain, U.K.; Kim, J.Y. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int. J. Surg. 2015, 18, 184–190. [Google Scholar] [CrossRef]
- Davenport, D.L.; Bowe, E.A.; Henderson, W.G.; Khuri, S.F.; Mentzer, R.M., Jr. National Surgical Quality Improvement Program (NSQIP) risk factors can be used to validate American Society of Anesthesiologists Physical Status Classification (ASA PS) levels. Ann. Surg. 2006, 243, 636–641, discussion 641–634. [Google Scholar] [CrossRef]
- Kandasamy, T.; Wright, E.D.; Fuller, J.; Rotenberg, B.W. The incidence of early post-operative complications following uvulopalatopharyngoplasty: Identification of predictive risk factors. J. Otolaryngol. Head Neck Surg. 2013, 42, 15. [Google Scholar] [CrossRef]
- Maldonado, O.; Demasi, R.; Maldonado, Y.; Taylor, M.; Troncale, F.; Vender, R. Extremely high levels of alkaline phosphatase in hospitalized patients. J. Clin. Gastroenterol. 1998, 27, 342–345. [Google Scholar] [CrossRef]
- Moss, D.W. Alkaline phosphatase isoenzymes. Clin. Chem. 1982, 28, 2007–2016. [Google Scholar] [CrossRef]
- Karhade, A.V.; Thio, Q.; Ogink, P.T.; Schwab, J.H. Serum alkaline phosphatase and 30-day mortality after surgery for spinal metastatic disease. J. Neurooncol. 2018, 140, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Kudsk, K.A.; Tolley, E.A.; DeWitt, R.C.; Janu, P.G.; Blackwell, A.P.; Yeary, S.; King, B.K. Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J. Parenter. Enter. Nutr. 2003, 27, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Panayi, A.C.; Haug, V.; Kauke-Navarro, M.; Foroutanjazi, S.; Diehm, Y.F.; Pomahac, B. The modified 5-item frailty index is a predictor of perioperative risk in head and neck microvascular reconstruction: An analysis of 3795 cases. Am. J. Otolaryngol. 2021, 42, 103121. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, M.; Ehrenstein, V.; Vandenbroucke, J.P. Confounding in observational studies based on large health care databases: Problems and potential solutions—A primer for the clinician. Clin. Epidemiol. 2017, 9, 185–193. [Google Scholar] [CrossRef]
- American College of Surgeons. Quality Programs. Frequently Asked Questions. Available online: https://www.facs.org/quality-programs/data-and-registries/acs-nsqip/faq/ (accessed on 18 November 2022).
- American College of Surgeons. User Guide for the 2016 ACS NSQIP Participant Use Data File (PUF). Available online: https://www.facs.org/media/kthpmx3h/nsqip_puf_userguide_2016.pdf (accessed on 18 November 2022).
- Shiloach, M.; Frencher, S.K., Jr.; Steeger, J.E.; Rowell, K.S.; Bartzokis, K.; Tomeh, M.G.; Richards, K.E.; Ko, C.Y.; Hall, B.L. Toward robust information: Data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J. Am. Coll. Surg. 2010, 210, 6–16. [Google Scholar] [CrossRef]
- MacKay, S.G.; Lewis, R.; McEvoy, D.; Joosten, S.; Holt, N.R. Surgical management of obstructive sleep apnoea: A position statement of the Australasian Sleep Association. Respirology 2020, 25, 1292–1308. [Google Scholar] [CrossRef]
- Tan, J.W.C.; Leow, L.C.; Wong, S.; Khoo, S.M.; Kasai, T.; Kojodjojo, P.; Sy, D.Q.; Lee, C.P.; Chirakalwasan, N.; Li, H.Y.; et al. Asian Pacific Society of Cardiology Consensus Statements on the Diagnosis and Management of Obstructive Sleep Apnoea in Patients with Cardiovascular Disease. Eur. Cardiol. 2022, 17, e16. [Google Scholar] [CrossRef]
- Rösslein, M.; Bürkle, H.; Walther, A.; Stuck, B.A.; Verse, T. Positionspapier zum perioperativen Management von erwachsenen Patienten mit obstruktiver Schlafapnoe bei HNO-ärztlichen Eingriffen. [Position Paper: Perioperative Management of Adult Patients with Obstructive Sleep Apnea in ENT Surgery]. Laryngorhinootologie 2015, 94, 516–523. [Google Scholar] [CrossRef]
- Chang, J.L.; Goldberg, A.N.; Alt, J.A.; Ashbrook, L.; Auckley, D.; Ayappa, I.; Bakhtiar, H.; Barrera, J.E.; Bartley, B.L.; Billings, M.E.; et al. International consensus statement on obstructive sleep apnea. Int. Forum Allergy Rhinol. 2022. [Google Scholar] [CrossRef]
- Haug, V.; Kadakia, N.; Wang, A.T.; Dorante, M.I.; Panayi, A.C.; Kauke-Navarro, M.; Hundeshagen, G.; Diehm, Y.F.; Fischer, S.; Hirche, C.; et al. Racial disparities in short-term outcomes after breast reduction surgery-A National Surgical Quality Improvement Project Analysis with 23,268 patients using Propensity Score Matching. J. Plast Reconstr. Aesthet. Surg. 2022, 75, 1849–1857. [Google Scholar] [CrossRef]

| Characteristic | Patients (n = 4662) |
|---|---|
| Demographics | |
| Sex | |
| Female (n) | 1273 (27) |
| Male (n) | 3388 (73) |
| Age, mean ± SD | 42 ± 13 |
| BMI, mean ± SD | 33 ± 7.3 |
| Race | |
| American Indian or Alaskan Native | 28 (0.6) |
| Asian | 244 (5.2) |
| Native Hawaiian or Pacific Islander | 51 (1.1) |
| Black or African American | 544 (12) |
| White | 2979 (64) |
| Other or unknown | 804 (17) |
| Preoperative health and comorbidities | |
| Diabetes | 469 (10) |
| Insulin-treated diabetes | 137 (2.9) |
| COPD | 60 (1.3) |
| CHF | 5 (0.1) |
| Obesity | 2909 (62) |
| Hypertension | 1435 (31) |
| Dyspnea | 229 (4.9) |
| Current smoker | 742 (16) |
| Corticosteroid use | 80 (1.7) |
| Wound infection | 13 (0.3) |
| ASA physical status classification score | |
| 1—No disturbance | 217 (4.7) |
| 2—Mild disturbance | 2650 (57) |
| 3—Severe disturbance | 1744 (37) |
| 4—Life-threatening | 45 (1.0) |
| Wound class | |
| 1—Clean | 179 (3.8) |
| 2—Clean/contaminated | 4396 (94) |
| 3—Contaminated | 63 (1.4) |
| 4—Dirty/infected | 24 (0.5) |
| Functional Status | |
| Independent | 4606 (99) |
| Partially or totally dependent | 56 (1.2) |
| Characteristic | Patients (n = 4662) |
|---|---|
| Surgical specialty | |
| General | 39 (0.8) |
| ENT | 4587 (98) |
| Other | 36 (0.8) |
| Type of anesthesia | |
| General | 4642 (100) |
| Local | 3 (0.06) |
| Monitored anesthesia care | 8 (0.2) |
| Epidural or spinal | 6 (0.1) |
| Other or unknown | 3 (0.06) |
| Setting | |
| Inpatient | 1382 (30) |
| Outpatient | 3280 (70) |
| Year of surgery | |
| 2008 | 173 (3.7) |
| 2009 | 202 (4.3) |
| 2010 | 306 (6.6) |
| 2011 | 120 (2.6) |
| 2012 | 441 (9.5) |
| 2013 | 429 (9.2) |
| 2014 | 440 (9.4) |
| 2015 | 455 (9.8) |
| 2016 | 457 (9.8) |
| 2017 | 516 (11) |
| 2018 | 445 (9.5) |
| 2019 | 376 (8.1) |
| 2020 | 302 (6.5) |
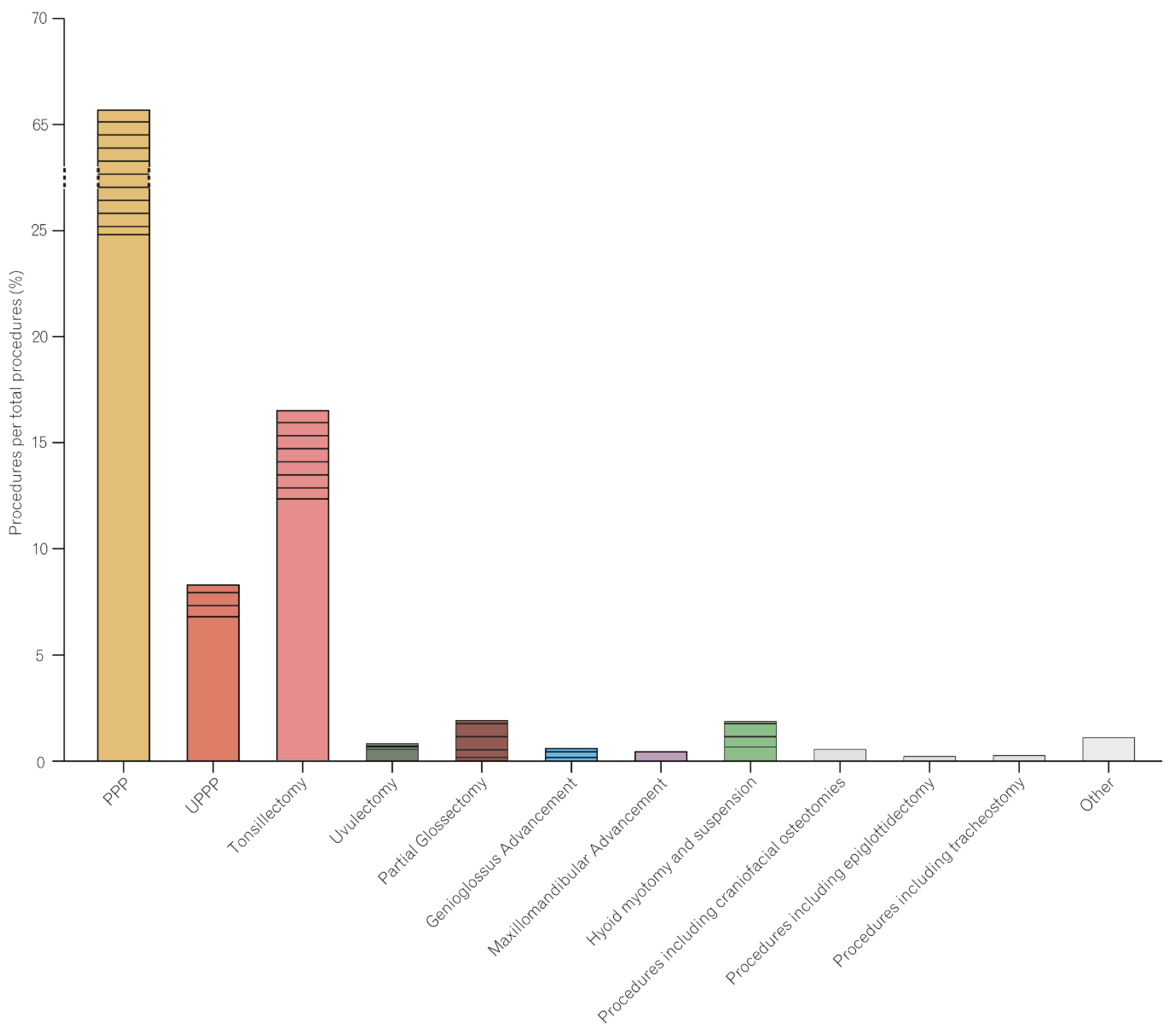
| Type of Surgery | N of Patients (%) |
|---|---|
| Isolated Uvulopalatopharyngoplasty (UPPP) | 321 (6.9) |
| + tonsillectomy | 46 (1.0) |
| + turbinate reduction | 14 (0.3) |
| + tongue radiofrequency ablation (RFA) + tonsillectomy | 1 (0.02) |
| + turbinate reduction + tongue RFA | 3 (0.06) |
| + tongue RFA | 2 (0.04) |
| + turbinate reduction + tonsillectomy | 7 (0.2) |
| Isolated Palatopharyngoplasty (PPP) | 1161 (25) |
| + tonsillectomy | 887 (19) |
| + tonsillectomy + turbinate reduction | 306 (6.6) |
| + tonsillectomy + tongue RFA | 70 (1.5) |
| + tonsillectomy + turbinate reduction + tongue RFA | 43 (0.9) |
| + tonsillectomy + hyoid myotomy and suspension + turbinate reduction | 5 (0.1) |
| + turbinate reduction + sinus surgery | 27 (0.6) |
| + tongue RFA | 76 (1.6) |
| + turbinate reduction | 409 (8.8) |
| + sinus surgery | 22 (0.5) |
| + tonsillectomy + sinus surgery | 9 (0.2) |
| + turbinate reduction + tongue RFA | 41 (0.9) |
| + tonsillectomy + sinus surgery + turbinate reduction | 9 (0.2) |
| + tonsillectomy + turbinate reduction + sinus surgery + tongue RFA | 2 (0.04) |
| + turbinate reduction + sinus surgery + tongue RFA | 1 (0.02) |
| + sinus surgery + turbinate reduction + tonsillectomy | 2 (0.04) |
| + sinus surgery + tongue RFA | 1 (0.02) |
| + sinus surgery + tonsillectomy + tongue RFA | 1 (0.02) |
| Isolated Tonsillectomy | 578 (12) |
| + turbinate reduction | 85 (1.8) |
| + turbinate reduction + sinus surgery | 7 (0.2) |
| + uvulectomy | 76 (1.6) |
| + uvulectomy + sinus surgery | 2 (0.04) |
| + turbinate reduction + uvulectomy | 18 (0.4) |
| + uvulectomy + tongue RFA | 3 (0.06) |
| + turbinate reduction + tongue RFA | 1 (0.02) |
| + tongue RFA | 3 (0.06) |
| + sinus surgery | 2 (0.04) |
| Isolated Uvulectomy | 31 (0.7) |
| + turbinate reduction | 14 (0.3) |
| + sinus surgery + turbinate reduction | 2 (0.04) |
| + sinus surgery | 1 (0.02) |
| Isolated Partial Glossectomy | 13 (0.3) |
| + PPP | 35 (0.8) |
| + PPP + turbinate reduction | 6 (0.1) |
| + turbinate reduction | 4 (0.09) |
| + PPP + tonsillectomy | 28 (0.6) |
| + tonsillectomy + PPP + turbinate reduction | 7 (0.2) |
| + tonsillectomy + turbinate reduction | 3 (0.06) |
| + tonsillectomy | 2 (0.04) |
| + hyoid myotomy and suspension | 1 (0.02) |
| Isolated Genioglossus Advancement | 0 (0.0) |
| + maxillomandibular advancement | 15 (0.3) |
| + PPP + turbinate reduction | 1 (0.02) |
| + PPP + tonsillectomy | 3 (0.06) |
| + maxillomandibular advancement + sinus surgery + turbinate reduction | 1 (0.02) |
| + maxillomandibular advancement + PPP | 4 (0.09) |
| + maxillomandibular advancement + PPP + tonsillectomy | 2 (0.04) |
| + maxillomandibular advancement + PPP + turbinate reduction | 2 (0.04) |
| + maxillomandibular advancement + turbinate reduction | 1 (0.02) |
| + turbinate reduction | 1 (0.02) |
| + PPP | 1 (0.02) |
| Isolated Maxillomandibular Advancement | 25 (0.5) |
| Isolated Hyoid Myotomy and Suspension | 35 (0.8) |
| + tonsillectomy | 6 (0.1) |
| + PPP | 26 (0.6) |
| + tongue RFA | 3 (0.06) |
| + PPP + turbinate reduction | 10 (0.2) |
| + PPP + partial glossectomy | 1 (0.02) |
| + tongue RFA + turbinate reduction | 4 (0.09) |
| + PPP + tonsillectomy | 7 (0.2) |
| + PPP + tongue RFA | 2 (0.04) |
| + turbinate reduction | 1 (0.02) |
| Procedures Including Craniofacial Osteotomies | 32 (0.7) |
| Procedures Including Epiglottidectomy | 16 (0.3) |
| Procedures Including Tracheostomy | 18 (0.4) |
| Other | 57 (1.2) |
| Outcome | Patients (n = 4662) |
|---|---|
| Length of Hospital Stay, mean days ± SD | 0.9 ± 2.0 |
| Operative Time, mean minutes ± SD | 66 ± 54 |
| Any Complication | 292 (6.3) |
| Mortality within 30 days | 2 (0.04) |
| Reoperation | 163 (3.5) |
| Readmission | 100 (2.1) |
| Unplanned Readmission | 99 (2.1) |
| Surgical Complication | 48 (1.0) |
| Superficial Incisional Infection | 26 (0.6) |
| Deep Incisional Infection | 4 (0.09) |
| Organ-Space Infection | 8 (0.2) |
| Dehiscence | 10 (0.2) |
| Medical Complication | 55 (1.2) |
| Pneumonia | 21 (0.5) |
| Reintubation | 17 (0.4) |
| Pulmonary Embolism | 4 (0.09) |
| Ventilator > 48 h | 10 (0.2) |
| Myocardial Infarction | 1 (0.02) |
| Cardiac Arrest Requiring CPR | 1 (0.02) |
| DVT or Thrombophlebitis | 5 (0.1) |
| Urinary Tract Infection | 11 (0.2) |
| Septic Shock | 1 (0.02) |
| Sepsis | 8 (0.2) |
| Discharge destination | |
| Home | 3956 (85) |
| Not Home | 16 (0.3) |
| Other or Unknown | 8 (0.2) |
| Type of Surgery | Total | Any Complication | Any Complication (Total %) |
|---|---|---|---|
| Uvulopalatopharyngoplasty (UPPP), of which: | |||
| Isolated | 321 | 13 | 4.0 |
| + tonsillectomy | 46 | 3 | 6.5 |
| + turbinate reduction | 14 | 1 | 7.1 |
| + tongue radiofrequency ablation (RFA) | 2 | 0 | 0.0 |
| + turbinate reduction + tonsillectomy | 7 | 0 | 0.0 |
| + turbinate reduction + tongue RFA | 3 | 0 | 0.0 |
| + tongue RFA + tonsillectomy | 1 | 0 | 0.0 |
| Palatopharyngoplasty (PPP), of which: | |||
| Isolated | 1161 | 65 | 5.6 |
| + tonsillectomy | 887 | 57 | 6.4 |
| + tonsillectomy + turbinate reduction | 306 | 18 | 5.9 |
| + tonsillectomy + tongue RFA | 70 | 9 | 13 |
| + tonsillectomy + turbinate reduction + tongue RFA | 43 | 0 | 0.0 |
| + tonsillectomy + hyoid myotomy and suspension + turbinate reduction | 5 | 1 | 20 |
| + turbinate reduction + sinus surgery | 27 | 2 | 7.4 |
| + tongue RFA | 76 | 5 | 6.6 |
| + turbinate reduction | 409 | 18 | 4.4 |
| + sinus surgery | 22 | 0 | 0.0 |
| + tonsillectomy + sinus surgery | 9 | 2 | 22 |
| + turbinate reduction + tongue RFA | 41 | 4 | 9.8 |
| + tonsillectomy + sinus surgery + turbinate reduction | 9 | 1 | 11 |
| + tonsillectomy + turbinate reduction + sinus surgery + tongue RFA | 2 | 0 | 0.0 |
| + turbinate reduction + sinus surgery + tongue RFA | 1 | 0 | 0.0 |
| + sinus surgery + turbinate reduction + tonsillectomy | 2 | 0 | 0.0 |
| + sinus surgery + tongue RFA | 1 | 0 | 0.0 |
| + sinus surgery + tonsillectomy + tongue RFA | 1 | 0 | 0.0 |
| Tonsillectomy, of which: | |||
| Isolated | 578 | 50 | 8.7 |
| + turbinate reduction | 85 | 4 | 4.7 |
| + turbinate reduction + sinus surgery | 7 | 0 | 0.0 |
| + uvulectomy | 76 | 4 | 5.4 |
| + uvulectomy + sinus surgery | 2 | 0 | 0.0 |
| + turbinate reduction + uvulectomy | 18 | 2 | 11 |
| + uvulectomy + tongue RFA | 3 | 0 | 0.0 |
| + turbinate reduction + tongue RFA | 1 | 0 | 0.0 |
| + tongue RFA | 3 | 0 | 0.0 |
| + sinus surgery | 2 | 0 | 0.0 |
| Uvulectomy, of which: | |||
| Isolated | 31 | 0 | 0.0 |
| + turbinate reduction | 14 | 2 | 14 |
| + sinus surgery + turbinate reduction | 2 | 0 | 0.0 |
| + sinus surgery | 1 | 0 | 0.0 |
| Partial Glossectomy, of which: | |||
| Isolated | 13 | 0 | 0.0 |
| + PPP | 35 | 2 | 5.7 |
| + PPP + turbinate reduction | 6 | 1 | 17 |
| + turbinate reduction | 4 | 0 | 0.0 |
| + PPP + tonsillectomy | 28 | 3 | 11 |
| + tonsillectomy + PPP + turbinate reduction | 7 | 0 | 0.0 |
| + tonsillectomy + turbinate reduction | 3 | 0 | 0.0 |
| + tonsillectomy | 2 | 0 | 0.0 |
| + hyoid myotomy and suspension | 1 | 0 | 0.0 |
| Genioglossus Advancement, of which: | |||
| Isolated | 0 | 0 | 0.0 |
| + maxillomandibular advancement | 15 | 2 | 13 |
| + PPP + turbinate reduction | 1 | 0 | 0.0 |
| + PPP + tonsillectomy | 3 | 0 | 0.0 |
| + maxillomandibular advancement + sinus surgery + turbinate reduction | 1 | 0 | 0.0 |
| + maxillomandibular advancement + PPP | 4 | 0 | 0.0 |
| + maxillomandibular advancement + PPP + tonsillectomy | 2 | 1 | 50 |
| + maxillomandibular advancement + PPP + turbinate reduction | 2 | 1 | 50 |
| + maxillomandibular advancement + turbinate reduction | 1 | 0 | 0.0 |
| + turbinate reduction | 1 | 0 | 0.0 |
| + PPP | 1 | 0 | 0.0 |
| Isolated Maxillomandibular Advancement | 25 | 2 | 8.0 |
| Hyoid Myotomy and Suspension, of which: | |||
| Isolated | 35 | 3 | 8.6 |
| + tonsillectomy | 6 | 0 | 0.0 |
| + PPP | 26 | 3 | 12 |
| + tongue RFA | 3 | 0 | 0.0 |
| + PPP + turbinate reduction | 10 | 1 | 10 |
| + PPP + partial glossectomy | 1 | 0 | 0.0 |
| + tongue RFA + turbinate reduction | 4 | 1 | 25 |
| + PPP + tonsillectomy | 7 | 0 | 0.0 |
| + PPP + tongue RFA | 2 | 0 | 0.0 |
| + turbinate reduction | 1 | 0 | 0.0 |
| Procedures Including Craniofacial Osteotomies | 32 | 2 | 6.3 |
| Procedures Including Epiglottidectomy | 16 | 0 | 0.0 |
| Procedures Including Tracheostomy | 18 | 4 | 22 |
| Other | 57 | 5 | 8.8 |
| Any Complication | Surgical Complication | Medical Complication | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Yes (n = 292) | No (n = 4370) | p-Value | Yes (n = 48) | No (n = 4614) | p-Value | Yes (n = 55) | No (n = 4607) | p-Value |
| Demographics | |||||||||
| Sex | 0.03 | 0.20 | 0.36 | ||||||
| Female (n) | 64 (22) | 1209 (28) | 9 (19) | 1264 (27) | 18 (33) | 1255 (27) | |||
| Male (n) | 228 (78) | 3160 (72) | 39 (81) | 3349 (73) | 37 (67) | 3351 (73) | |||
| Age, mean ± SD | 41 ± 13 | 42 ± 13 | 0.44 | 46 ± 13 | 42 ± 13 | 0.04 | 45 ± 13 | 42 ± 13 | 0.05 |
| BMI, mean ± SD | 34 ± 8 | 33 ± 7 | 0.01 | 32 ± 6 | 33 ± 7 | 0.46 | 38 ± 9 | 33 ± 7 | <0.0001 |
| Race | 0.30 | 0.02 | 0.66 | ||||||
| American Indian or Alaskan Native | 2 (0.7) | 26 (0.6) | 0 (0) | 28 (0.1) | 0 (0) | 28 (0.6) | |||
| Asian | 23 (7.9) | 221 (5.1) | 2 (4.2) | 242 (5.2) | 3 (5.5) | 241 (5.2) | |||
| Native Hawaiian or Pacific Islander | 4 (1.4) | 47 (1.1) | 1 (2.1) | 50 (1.1) | 0 (0) | 51 (1.1) | |||
| Black or African American | 32 (11) | 512 (12) | 3 (6.3) | 541 (12) | 10 (18) | 534 (12) | |||
| White | 173 (59) | 2806 (64) | 23 (48) | 2956 (64) | 32 (58) | 2947 (64) | |||
| Other or unknown | 55 (19) | 749 (17) | 17 (35) | 787 (17) | 10 (18) | 794 (17) | |||
| Setting | <0.0001 | 0.0002 | <0.0001 | ||||||
| Outpatient | 167 (57) | 3113 (71) | 22 (46) | 3258 (71) | 24 (44) | 3256 (71) | |||
| Inpatient | 125 (43) | 1257 (29) | 26 (54) | 1356 (29) | 31 (56) | 1351 (29) | |||
| Preop health and comorbidities | |||||||||
| Diabetes | 45 (15) | 424 (9.7) | 0.002 | 6 (13) | 463 (10) | 0.48 | 15 (27) | 454 (9.9) | <0.0001 |
| Insulin-treated diabetes | 15 (5.1) | 122 (2.8) | 0.02 | 2 (4.2) | 135 (2.9) | 0.65 | 5 (9.1) | 132 (2.9) | 0.02 |
| COPD | 8 (2.7) | 52 (1.2) | 0.05 | 4 (8.3) | 56 (1.2) | 0.003 | 2 (3.6) | 58 (1.3) | 0.16 |
| CHF | 1 (0.3) | 4 (0.09) | 0.28 | 0 (0) | 5 (0.1) | >0.99 | 1 (1.8) | 4 (0.09) | 0.06 |
| Obesity | 195 (67) | 2714 (62) | 0.11 | 29 (60) | 2880 (62) | 0.78 | 45 (82) | 2864 (62) | 0.003 |
| Hypertension | 106 (36) | 1329 (30) | 0.03 | 18 (38) | 1417 (31) | 0.31 | 21 (38) | 1414 (31) | 0.23 |
| Dyspnea | 21 (7.2) | 208 (4.8) | 0.06 | 6 (13) | 223 (4.8) | 0.03 | 6 (11) | 223 (4.8) | 0.05 |
| Current smoker | 52 (18) | 690 (16) | 0.36 | 7 (15) | 735 (16) | >0.99 | 10 (18) | 732 (16) | 0.64 |
| Corticosteroid use | 7 (2.4) | 73 (1.7) | 0.35 | 2 (4.2) | 78 (1.7) | 0.20 | 4 (7.3) | 76 (1.6) | 0.01 |
| Wound infection | 2 (0.7) | 11 (0.3) | 1.19 | 0 (0) | 13 (0.3) | >0.99 | 1 (1.8) | 12 (0.3) | 0.14 |
| ASA physical status classification score | <0.0001 | 0.48 | 0.0006 | ||||||
| 1—No disturbance | 13 (4.5) | 204 (4.7) | 4 (8.3) | 213 (4.6) | 1 (1.8) | 216 (4.7) | |||
| 2—Mild disturbance | 149 (51) | 2501 (57) | 24 (50) | 2626 (57) | 19 (35) | 2631 (57) | |||
| 3—Severe disturbance | 119 (41) | 1625 (37) | 19 (40) | 1725 (37) | 33 (60) | 1711 (37) | |||
| 4—Life-threatening | 10 (3.4) | 35 (0.8) | 1 (2.1) | 44 (1.0) | 2 (3.6) | 43 (0.9) | |||
| Wound class | 0.81 | 0.82 | 0.22 | ||||||
| 1—Clean | 14 (4.8) | 165 (3.8) | 2 (4.2) | 177 (3.8) | 4 (7.3) | 175 (3.8) | |||
| 2—Clean/Contaminated | 272 (93) | 4124 (94) | 46 (96) | 4350 (94) | 50 (91) | 4346 (94) | |||
| 3—Contaminated | 4 (1.4) | 59 (1.4) | 0 (0) | 63 (1.4) | 0 (0) | 63 (1.4) | |||
| 4—Dirty/Infected | 2 (0.7) | 22 (0.5) | 0 (0) | 24 (0.5) | 1 (1.8) | 23 (0.5) | |||
| Functional Status | 0.08 | 0.44 | 0.03 | ||||||
| Independent | 285 (98) | 4321 (99) | 47 (98) | 4559 (99) | 52 (95) | 4554 (99) | |||
| Partially or totally dependent | 7 (2.4) | 49 (1.1) | 1 (2.1) | 55 (1.2) | 3 (5.5) | 53 (1.2) | |||
| Risk-Associated Factors | OR | 95% CI | p-Value |
|---|---|---|---|
| Any complications | |||
| Sex (female) | −0.02 | −0.04–−0.01 | 0.003 |
| Diabetes | 0.03 | 0.00–0.05 | 0.03 |
| ASA physical status classification score (≥4) | 0.12 | 0.05–0.20 | 0.001 |
| Surgical complications | |||
| Race (White) | −0.02 | −0.02–−0.01 | <0.0001 |
| Race (Black or African American) | −0.02 | −0.03–−0.01 | 0.004 |
| COPD | 0.05 | 0.02–0.07 | 0.0006 |
| Medical complications | |||
| Diabetes | 0.02 | 0.01–0.03 | 0.003 |
| History of CHF | 0.15 | 0.05–0.24 | 0.004 |
| Corticosteroid use | 0.03 | 0.01–0.06 | 0.006 |
| Underweight; BMI < 18.5 | 0.08 | 0.01–0.14 | 0.02 |
| Extreme Obesity Class 3; BMI > 40 | 0.01 | 0.00–0.02 | 0.02 |
| Risk-Associated Factors | OR | 95% CI | p-Value |
|---|---|---|---|
| Any complications | |||
| Isolated tonsillectomy | 0.05 | 0.02–0.09 | 0.003 |
| Procedures including tracheostomy | 0.12 | 0.00–0.25 | 0.04 |
| PPP + tonsillectomy + tongue RFA | 0.09 | 0.02–0.15 | 0.007 |
| PPP + tonsillectomy + sinus surgery | 0.17 | 0.01–0.33 | 0.03 |
| Genioglossus advancement + maxillomandibular advancement + PPP + tonsillectomy | 0.45 | 0.11–0.78 | 0.009 |
| Genioglossus advancement + maxillomandibular advancement + turbinate reduction | 0.96 | 0.48–1.43 | <0.0001 |
| Surgical complications | |||
| Genioglossus advancement + maxillomandibular advancement | 0.06 | 0.01–0.11 | 0.03 |
| Genioglossus advancement + maxillomandibular advancement + turbinate reduction | 0.99 | 0.79–1.18 | <0.0001 |
| Hyoid myotomy and suspension | 0.07 | 0.04–0.11 | <0.0001 |
| Hyoid myotomy and suspension + PPP | 0.06 | 0.02–0.10 | 0.001 |
| Hyoid myotomy and suspension + tongue RFA + turbinate reduction | 0.24 | 0.15–0.34 | <0.0001 |
| Medical complications | |||
| Procedures including tracheostomy | 0.06 | 0.00–0.11 | 0.04 |
| Genioglossus advancement + maxillomandibular advancement | 0.06 | 0.00–0.11 | 0.04 |
| PPP + tonsillectomy + tongue RFA | 0.03 | 0.00–0.06 | 0.04 |
| PPP + tonsillectomy + sinus surgery | 0.09 | 0.02–0.17 | 0.01 |
| PPP + tonsillectomy + sinus surgery + turbinate reduction | 0.11 | 0.03–0.18 | 0.004 |
| Hyoid myotomy and suspension + PPP + turbinate reduction | 0.09 | 0.02–0.16 | 0.01 |
| UPPP + turbinate reduction | 0.07 | 0.01–0.13 | 0.02 |
| Any Complication | Surgical Complication | Medical Complication | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Yes (n = 292) | No (n = 4370) | p-Value | Yes (n = 48) | No (n = 4614) | p-Value | Yes (n = 55) | No (n = 4607) | p-Value | Reference Range |
| Serum sodium (mmol/L) | 139.5 (2.7) | 139.4 (2.5) | 0.45 | 139.0 (3.2) | 139.4 (2.5) | 0.51 | 139.6 (2.3) | 139.4 (2.5) | 0.57 | 135–145 mmol/L |
| BUN (mg/dL) | 15.3 (8.3) | 15.1 (5.4) | 0.64 | 16.2 (4.8) | 15.1 (5.6) | 0.43 | 16.5 (12.0) | 15.1 (5.4) | 0.14 | 8–25 mg/dL |
| Creatinine (g/D) | 0.9 (0.5) | 1.0 (0.5) | 0.65 | 1.0 (0.3) | 1.0 (0.5) | 0.79 | 1.0 (0.5) | 1.0 (0.5) | 0.61 | F 0.6–1.8, M 0.8–2.4 g/D |
| Serum albumin (g/dL) | 4.2 (0.5) | 4.3 (0.4) | 0.38 | 4.3 (0.5) | 4.2 (0.4) | 0.78 | 4.1 (0.4) | 4.3 (0.4) | 0.16 | 3.1–4.3 g/dL |
| Total bilirubin (mg/dL) | 0.7 (0.9) | 0.6 (0.5) | 0.07 | 0.6 (0.3) | 0.6 (0.6) | 0.91 | 0.7 (0.5) | 0.6 (0.6) | 0.40 | 0–1 mg/dL |
| SGOT (U/L) | 28.4 (15.4) | 27.1 (25.5) | 0.68 | 20.0 (4.7) | 27.3 (25.0) | 0.35 | 25.3 (10.2) | 27.3 (25.1) | 0.74 | F 9–25, M 10–40 U/L |
| Alkaline phosphatase (U/L) | 81.5 (32.8) | 74.4 (23.5) | 0.02 | 70.3 (18.9) | 75.0 (24.3) | 0.57 | 94.1 (43.5) | 74.6 (23.7) | 0.001 | F 30–100 U/L |
| WBC × 103/mm3 | 7.8 (2.6) | 7.4 (2.8) | 0.09 | 7.2 (2.1) | 7.5 (2.8) | 0.66 | 8.1 (2.2) | 7.4 (2.8) | 0.15 | 4.5–11 × 103/mm3 |
| Hematocrit (% of RBCs) | 43.0 (4.9) | 42.8 (4.2) | 0.64 | 43.8 (3.9) | 42.8 (4.2) | 0.26 | 42.4 (4.5) | 42.8 (4.2) | 0.58 | F 36.0–46.0%, M 37.0–49.0% of RBCs |
| Platelet count × 103/µL | 248.2 (62.9) | 250.4 (64.3) | 0.68 | 240.7 (46.1) | 250.4 (64.4) | 0.48 | 242.3 (55.3) | 250.4 (64.4) | 0.47 | 130–400 × 103/µL |
| PTT (s) | 30.2 (3.7) | 29.3 (5.2) | 0.20 | 31.7 (4.7) | 29.4 (5.1) | 0.19 | 29.8 (4.7) | 29.4 (5.1) | 0.77 | 25–35 s |
| INR of PT values | 1.0 (0.1) | 1.0 (0.3) | 0.86 | 1.0 (0.1) | 1.0 (0.3) | 0.89 | 1.0 (0.1) | 1.0 (0.3) | 0.95 | <1.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knoedler, S.; Knoedler, L.; Baecher, H.; Kauke-Navarro, M.; Obed, D.; Hoch, C.C.; Diehm, Y.F.; Vosler, P.S.; Harréus, U.; Kneser, U.; et al. 30-Day Postoperative Outcomes in Adults with Obstructive Sleep Apnea Undergoing Upper Airway Surgery. J. Clin. Med. 2022, 11, 7371. https://doi.org/10.3390/jcm11247371
Knoedler S, Knoedler L, Baecher H, Kauke-Navarro M, Obed D, Hoch CC, Diehm YF, Vosler PS, Harréus U, Kneser U, et al. 30-Day Postoperative Outcomes in Adults with Obstructive Sleep Apnea Undergoing Upper Airway Surgery. Journal of Clinical Medicine. 2022; 11(24):7371. https://doi.org/10.3390/jcm11247371
Chicago/Turabian StyleKnoedler, Samuel, Leonard Knoedler, Helena Baecher, Martin Kauke-Navarro, Doha Obed, Cosima C. Hoch, Yannick F. Diehm, Peter S. Vosler, Ulrich Harréus, Ulrich Kneser, and et al. 2022. "30-Day Postoperative Outcomes in Adults with Obstructive Sleep Apnea Undergoing Upper Airway Surgery" Journal of Clinical Medicine 11, no. 24: 7371. https://doi.org/10.3390/jcm11247371
APA StyleKnoedler, S., Knoedler, L., Baecher, H., Kauke-Navarro, M., Obed, D., Hoch, C. C., Diehm, Y. F., Vosler, P. S., Harréus, U., Kneser, U., & Panayi, A. C. (2022). 30-Day Postoperative Outcomes in Adults with Obstructive Sleep Apnea Undergoing Upper Airway Surgery. Journal of Clinical Medicine, 11(24), 7371. https://doi.org/10.3390/jcm11247371








