Coping and Co-Occurrence of Gaming Disorder and Substance Use in Recovering Substance Users
Abstract
1. Introduction
1.1. Gaming Disorder and Comorbid Disorders
1.2. Coping
1.3. Substance Use and Gamers
1.4. Replacement, Co-Occurrence and the Cycle of Reciprocity
1.5. The Present Study
2. Materials and Methods
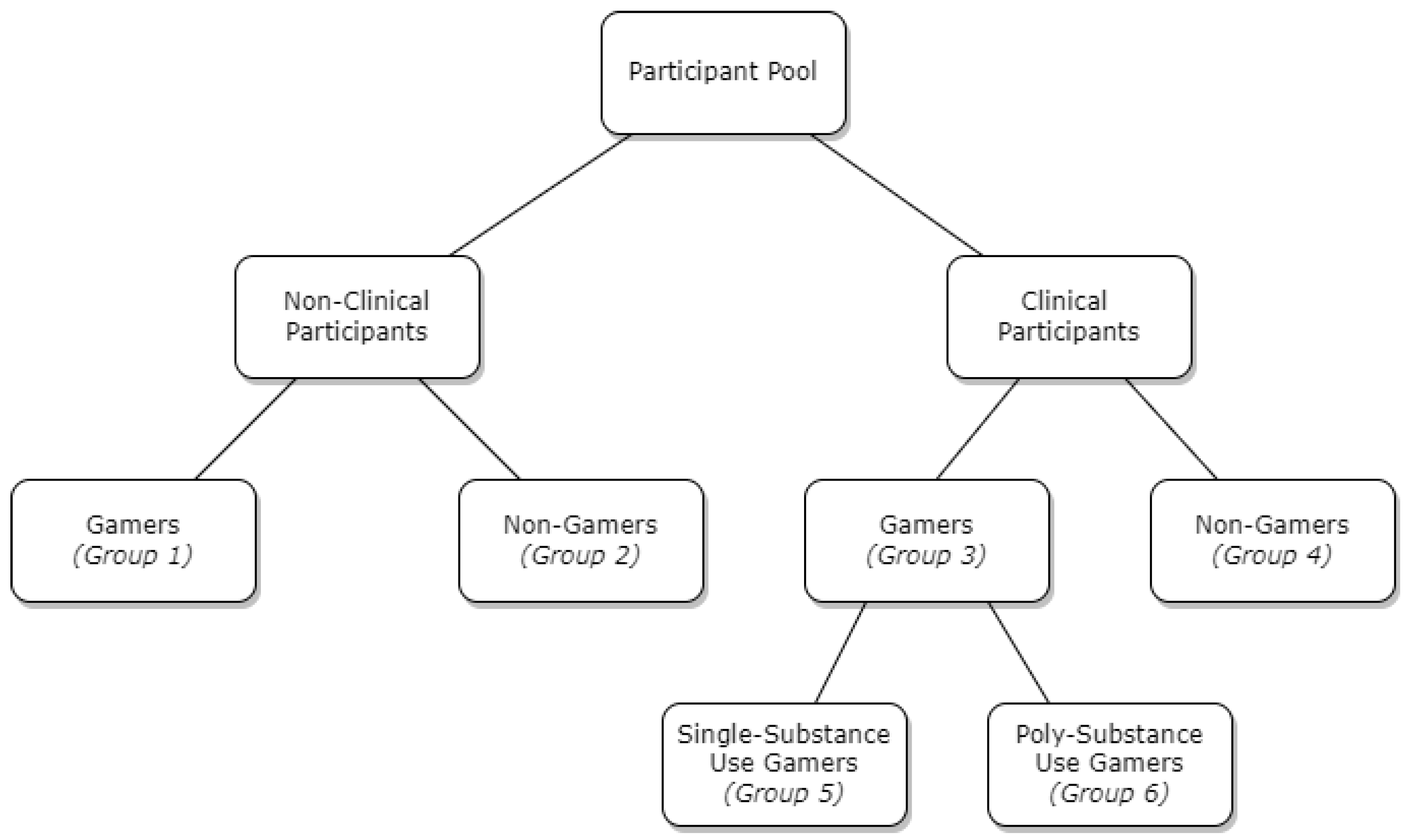
2.1. Participants and Procedure
2.2. Measures
2.2.1. Nine-Item Internet Gaming Disorder Scale—Short Form (IGDS9-SF)
2.2.2. Problem Gambling Severity Index (PGSI)
2.2.3. Nine-Item Internet Disorder Scale—Short Form (IDS9-SF)
2.2.4. The Bergen Social Media Addiction Scale (BSMAS)
2.2.5. Bergen-Yale Sex Addiction Scale (BYSAS)
2.2.6. Bergen Shopping Addiction Scale (BSAS)
2.2.7. Cigarette Dependency Scale-5 (CDS)
2.2.8. Alcohol Use Disorder Identification Test (AUDIT)
2.2.9. Drug Abuse Screen Test-10 (DAST)
2.2.10. Brief Coping Orientation to Problems Experienced (Brief-COPE)
2.3. Data Analyses
3. Results
3.1. Correlations between Problematic Behaviours and Substance Use among Gamers and Non-Gamers
3.2. Co-Occurring Substance Use and Gaming among Clinical Gamers
3.3. The Effect of Coping Style on Gaming among Clinical and Non-Clinical Gamers
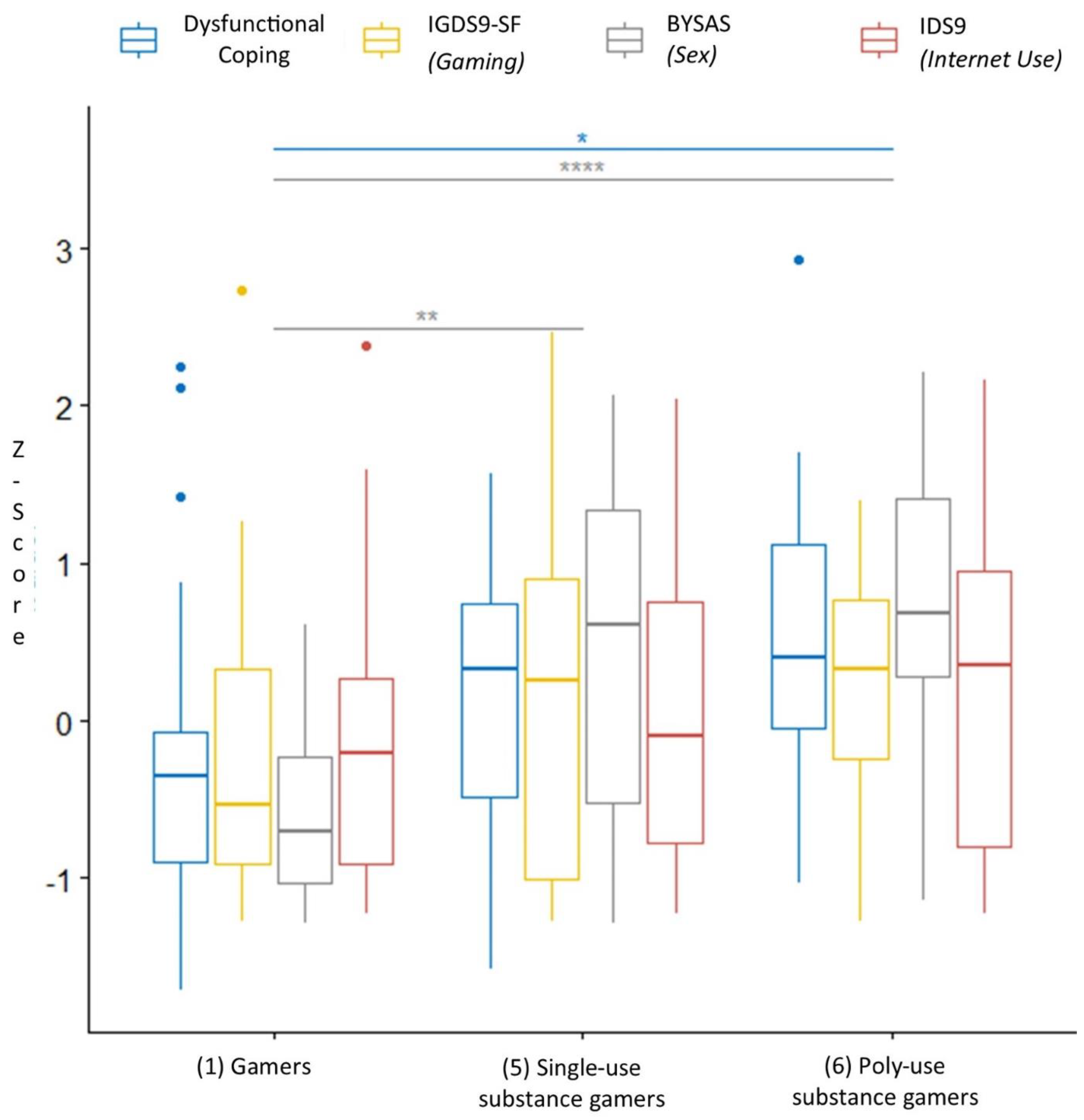
3.4. Exploratory Direct Comparisons of Clinical Gamers and Non-Clinical Gamers
4. Discussion
4.1. Gaming Disorder, Problematic Behaviours, and Substance Use
4.2. The Exacerbating Effect of Co-Occurrence
4.3. Coping Strategies among Gamers
4.4. Exploring Differences between Gamers and Abstinent Substance Use Gamers
4.5. Clinical Implications and Future Directions
4.6. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hughes, J.R.; Fingar, J.R.; Budney, A.J.; Naud, S.; Helzer, J.E.; Callas, P.W. Marijuana use and intoxication among daily users: An intensive longitudinal study. Addict. Behav. 2014, 39, 1464–1470. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Pontes, H.M.; Griffiths, M.D. Neurobiological correlates in internet gaming disorder: A systematic literature review. Front. Psychiatry 2018, 9, 166. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- World Health Organization. ICD-11 for Mortality and Morbidity Statistics. Available online: http://id.who.int/icd/entity/1448597234 (accessed on 15 July 2021).
- Estévez, A.; Jáuregui, P.; Sánchez-Marcos, I.; López-González, H.; Griffiths, M.D. Attachment and emotion regulation in substance addictions and behavioral addictions. J. Behav. Addict. 2017, 6, 534–544. [Google Scholar] [CrossRef] [PubMed]
- Brand, M.; Laier, C.; Young, K.S. Internet addiction: Coping styles, expectancies, and treatment implications. Front. Psychol. 2014, 5, 1256. [Google Scholar] [CrossRef]
- Adams, B.L.M.; Stavropoulos, V.; Burleigh, T.L.; Liew, L.W.L.; Beard, C.L.; Griffiths, M.D. Internet gaming disorder behaviors in emergent adulthood: A pilot study examining the interplay between anxiety and family cohesion. Int. J. Ment. Health Addict. 2019, 17, 828–844. [Google Scholar] [CrossRef]
- King, D.L.; Delfabbro, P.H.; Zwaans, T.; Kaptsis, D. Clinical features and Axis I comorbidity of Australian adolescent pathological internet and video game users. Aust. N. Z. J. Psychiatry 2013, 47, 1058–1067. [Google Scholar] [CrossRef]
- Schimmenti, A.; Infanti, A.; Badoud, D.; Laloyaux, J.; Billieux, J. Schizotypal personality traits and problematic use of massivelymultiplayer online role-playing games (MMORPGs). Comput. Hum. Behav. 2017, 74, 286–293. [Google Scholar] [CrossRef]
- Burleigh, T.L.; Griffiths, M.D.; Sumich, A.; Stavropoulos, V.; Kuss, D.J. A systematic review of the co-occurrence of gaming disorder and other potentially addictive behaviors. Curr. Addict. Rep. 2019, 6, 383–401. [Google Scholar] [CrossRef]
- van Rooij, A.J.; Ferguson, C.J.; Colder Carras, M.; Kardefelt-Winther, D.; Shi, J.; Aarseth, E.; Bean, A.M.; Bergmark, K.H.; Brus, A.; Coulson, M.; et al. A weak scientific basis for gaming disorder: Let us err on the side of caution. J. Behav. Addict. 2018, 7, 1–9. [Google Scholar] [CrossRef]
- Aarseth, E.; Bean, A.M.; Boonen, H.; Carras, M.C.; Coulson, M.; Das, D.; Deleuze, J.; Dunkels, E.; Edman, J.; Ferguson, C.J.; et al. Scholars’ open debate paper on the world health organization ICD-11 gaming disorder proposal. J. Behav. Addict. 2017, 6, 267–270. [Google Scholar] [CrossRef]
- Colder Carras, M.; Kardefelt-Winther, D. When addiction symptoms and life problems diverge: A latent class analysis of problematic gaming in a representative multinational sample of european adolescents. Eur. Child Adolesc. Psychiatry 2018, 27, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Griffiths, M.D. Internet gaming addiction: A systematic review of empirical research. Int. J. Ment. Health Addict. 2012, 10, 278–296. [Google Scholar] [CrossRef]
- Schneider, L.A.; King, D.L.; Delfabbro, P.H. Maladaptive coping styles in adolescents with internet gaming disorder symptoms. Int. J. Ment. Health Addict. 2018, 16, 905–916. [Google Scholar] [CrossRef]
- McMahon, E.M.; Corcoran, P.; McAuliffe, C.; Keeley, H.; Perry, I.J.; Arensman, E. Mediating effects of coping style on associations between mental health factors and self-harm among adolescents. Crisis 2013, 34, 242–250. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’ too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Carver, C.S.; Scheier, M.F. Attention and Self-Regulation: A Control Theory Approach; Springer: New York, NY, USA, 1981. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Kuss, D.; Dunn, T.J.; Wölfling, K.; Müller, K.W.; Hȩdzelek, M.; Marcinkowski, J.; Hędzelek, M.; Marcinkowski, J.; Hȩdzelek, M.; Marcinkowski, J. Excessive internet use and psychopathology: The role of coping. Clin. Neuropsychiatry 2017, 14, 73–81. [Google Scholar]
- Baker, J.P.; Berenbaum, H. Emotional approach and problem-focused coping: A comparison of potentially adaptive strategies. Cogn. Emot. 2007, 21, 95–118. [Google Scholar] [CrossRef]
- Hemenover, S.H.; Bowman, N.D. Video games, emotion, and emotion regulation: Expanding the scope. Ann. Int. Commun. Assoc. 2018, 42, 125–143. [Google Scholar] [CrossRef]
- Kuss, D.J.; Louws, J.; Wiers, R.W. Online gaming addiction? Motives predict addictive play behavior in massively multiplayer online role-playing games. Cyberpsychology Behav. Soc. Netw. 2012, 15, 480–485. [Google Scholar] [CrossRef]
- Heggeness, L.F.; Bean, C.A.L.; Kalmbach, D.A.; Ciesla, J.A. Cognitive risk, coping-oriented substance use, and increased avoidance tendencies among depressed outpatients: A prospective investigation. J. Clin. Psychol. 2020, 76, 2249–2263. [Google Scholar] [CrossRef] [PubMed]
- Burleigh, T.L.; Stavropoulos, V.; Liew, L.W.L.; Adams, B.L.M.; Griffiths, M.D. Depression, internet gaming disorder, and the moderating effect of the gamer-avatar relationship: An exploratory longitudinal study. Int. J. Ment. Health Addict. 2018, 16, 102–124. [Google Scholar] [CrossRef]
- Ream, G.L.; Elliott, L.C.; Dunlap, E. Trends in video game play through childhood, adolescence, and emerging adulthood. Psychiatry J. 2013, 2013, 301460. [Google Scholar] [CrossRef] [PubMed]
- Khantzian, E.J. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. Am. J. Psychiatry 1985, 142, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- van Rooij, A.J.; Kuss, D.J.; Griffiths, M.D.; Shorter, G.W.; Schoenmakers, T.M.; van de Mheen, D. The (co-)occurrence of problematic video gaming, substance use, and psychosocial problems in adolescents. J. Behav. Addict. 2014, 3, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Gallimberti, L.; Buja, A.; Chindamo, S.; Rabensteiner, A.; Terraneo, A.; Marini, E.; Pérez, L.J.G.; Baldo, V. Problematic use of video games and substance abuse in early adolescence: A cross-sectional study. Am. J. Health Behav. 2016, 40, 594–603. [Google Scholar] [CrossRef]
- Sussman, S.; Pokhrel, P.; Sun, P.; Rohrbach, L.A.; Spruijt-Metz, D. Prevalence and co-occurrence of addictive behaviors among former alternative high school youth: A longitudinal follow-up study. J. Behav. Addict. 2015, 4, 189–194. [Google Scholar] [CrossRef]
- Tsai, J.; Huh, J.; Idrisov, B.; Galimov, A.; Espada, J.P.; Gonzálvez, M.T.; Sussman, S. Prevalence and co-occurrence of addictive behaviors among russian and spanish youth. J. Drug Educ. 2016, 46, 32–46. [Google Scholar] [CrossRef]
- Di Nicola, M.; Tedeschi, D.; De Risio, L.; Pettorruso, M.; Martinotti, G.; Ruggeri, F.; Swierkosz-Lenart, K.; Guglielmo, R.; Callea, A.; Ruggeri, G.; et al. Co-occurrence of alcohol use disorder and behavioral addictions: Relevance of impulsivity and craving. Drug Alcohol Depend. 2015, 148, 118–125. [Google Scholar] [CrossRef]
- Walther, B.; Morgenstern, M.; Hanewinkel, R. Co-occurrence of addictive behaviours: Personality factors related to substance use, gambling and computer gaming. Eur. Addict. Res. 2012, 18, 167–174. [Google Scholar] [CrossRef]
- Sussman, S.; Black, D.S. Substitute addiction: A concern for researchers and practitioners. J. Drug Educ. 2008, 38, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Sussman, S. The relations of cigarette smoking with risky sexual behavior among teens. Sex. Addict. Compulsivity 2005, 12, 181–199. [Google Scholar] [CrossRef]
- Kotyuk, E.; Magi, A.; Eisinger, A.; Király, O.; Vereczkei, A.; Barta, C.; Griffiths, M.D.; Székely, A.; Kökönyei, G.; Farkas, J.; et al. Co-occurrences of substance use and other potentially addictive behaviors: Epidemiological results from the psychological and genetic factors of the addictive behaviors (PGA) study. J. Behav. Addict. 2020, 9, 272–288. [Google Scholar] [CrossRef] [PubMed]
- Haylett, S.A.; Stephenson, G.M.; Lefever, R.M.H. Covariation in addictive behaviours: A study of addictive orientations using the shorter promis questionnaire. Addict. Behav. 2004, 29, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Gossop, M. A web of dependence. Addiction 2001, 96, 677–678. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.J.; Usdan, S.; Cremeens, J.; Vail-Smith, K. Disordered gambling and co-morbidity of psychiatric disorders among college students: An examination of problem drinking, anxiety and depression. J. Gambl. Stud. 2014, 30, 321–333. [Google Scholar] [CrossRef]
- Urbanoski, K.A.; Castel, S.; Rush, B.R.; Bassani, D.G.; Wild, T.C. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatr. Serv. 2007, 58, 962–969. [Google Scholar] [CrossRef]
- Najt, P.; Fusar-Poli, P.; Brambilla, P. Co-occurring mental and substance abuse disorders: A review on the potential predictors and clinical outcomes. Psychiatry Res. 2011, 186, 159–164. [Google Scholar] [CrossRef]
- Freimuth, M.; Waddell, M.; Stannard, J.; Kelley, S.; Kipper, A.; Richardson, A.; Szuromi, I. Expanding the scope of dual diagnosis and co-addictions: Behavioral addictions. J. Groups Addict. Recover. 2008, 3, 137–160. [Google Scholar] [CrossRef]
- Roncero, C.; Grau-López, L.; Casas, M. Dual disorders. Addict. Disord. Their Treat. 2017, 16, 175–179. [Google Scholar] [CrossRef]
- Carrà, G.; Bartoli, F.; Brambilla, G.; Crocamo, C.; Clerici, M. Comorbid addiction and major mental illness in Europe: A narrative review. Subst. Abus. 2015, 36, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.; Degenhardt, L.; Teesson, M. Reprint of “Understanding comorbidity between substance use, anxiety and affective disorders: Broadening the research base”. Addict. Behav. 2009, 34, 795–799. [Google Scholar] [CrossRef] [PubMed]
- Yakovenko, I.; Hodgins, D.C. A scoping review of co-morbidity in individuals with disordered gambling. Int. Gambl. Stud. 2018, 18, 143–172. [Google Scholar] [CrossRef]
- Kuss, D.J.; Griffiths, M.D.; Karila, L.; Billieux, J. Internet addiction: A systematic review of epidemiological research for the last decade. Curr. Pharm. Des. 2014, 20, 4026–4052. [Google Scholar] [CrossRef] [PubMed]
- Winkler, A.; Dörsing, B.; Rief, W.; Shen, Y.; Glombiewski, J.A. Treatment of internet addiction: A meta-analysis. Clin. Psychol. Rev. 2013, 33, 317–329. [Google Scholar] [CrossRef]
- Pontes, H.M.; Griffiths, M.D. Measuring DSM-5 internet gaming disorder: Development and validation of a short psychometric scale. Comput. Hum. Behav. 2015, 45, 137–143. [Google Scholar] [CrossRef]
- Ferris, J.A.; Wynne, H.J. The Canadian Problem Gambling Index; Canadian Centre on Substance Abuse: Ottawa, ON, USA, 2001. [Google Scholar]
- Pontes, H.M.; Griffiths, M.D. The development and psychometric properties of the Internet Disorder Scale–Short Form (IDS9-sf). Addicta Turkish J. Addict. 2017, 3, 303–318. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Billieux, J.; Griffiths, M.D.; Kuss, D.J.; Demetrovics, Z.; Mazzoni, E.; Pallesen, S. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychol. Addict. Behav. 2016, 30, 252–262. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Torsheim, T.; Brunborg, G.S.; Pallesen, S. Development of a Facebook addiction scale. Psychol. Rep. 2012, 110, 501–517. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Pallesen, S.; Griffiths, M.D.; Torsheim, T.; Sinha, R. The development and validation of the Bergen–Yale Sex Addiction Scale with a large national sample. Front. Psychol. 2018, 9, 144. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Griffiths, M.D.; Pallesen, S.; Bilder, R.M.; Torsheim, T.; Aboujaoude, E. The Bergen Shopping Addiction Scale: Reliability and validity of a brief screening test. Front. Psychol. 2015, 6, 1374. [Google Scholar] [CrossRef] [PubMed]
- Etter, J.-F.; Le Houezec, J.; Perneger, T.V. A self-administered questionnaire to measure dependence on cigarettes: The Cigarette Dependence scale. Neuropsychopharmacology 2003, 28, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De La Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-ii. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- de Meneses-Gaya, C.; Zuardi, A.W.; Loureiro, S.R.; Crippa, J.A.S. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychol. Neurosci. 2009, 2, 83–97. [Google Scholar] [CrossRef]
- Skinner, H.A. The drug abuse screening test. Addict. Behav. 1982, 7, 363–371. [Google Scholar] [CrossRef]
- Yudko, E.; Lozhkina, O.; Fouts, A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. J. Subst. Abuse Treat. 2007, 32, 189–198. [Google Scholar] [CrossRef]
- Ho, D.E.; Imai, K.; King, G.; Stuart, E.A. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit. Anal. 2007, 15, 199–236. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turkish J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Coëffec, A.; Romo, L.; Cheze, N.; Riazuelo, H.; Plantey, S.; Kotbagi, G.; Kern, L. Early substance consumption and problematic use of video games in adolescence. Front. Psychol. 2015, 6, 501. [Google Scholar] [CrossRef][Green Version]
- Turel, O.; Bechara, A. Little video-gaming in adolescents can be protective, but too much is associated with increased substance use. Subst. Use Misuse 2019, 54, 384–395. [Google Scholar] [CrossRef]
- Strizek, J.; Atzendorf, J.; Kraus, L.; Monshouwer, K.; Puhm, A.; Uhl, A. Perceived problems with adolescent online gaming: National differences and correlations with substance use. J. Behav. Addict. 2020, 9, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Aresi, G.; Cleveland, M.J.; Beccaria, F.; Marta, E. Variations in acceptability of heavy alcohol use and gender double standards across drinking cultures. A U.S.A.–Italy study. J. Ethn. Subst. Abuse 2021, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Cavalieri, D.; McGovern, P.E.; Hartl, D.L.; Mortimer, R.; Polsinelli, M. Evidence for s. cerevisiae fermentation in ancient wine. J. Mol. Evol. 2003, 57, S226–S232. [Google Scholar] [CrossRef] [PubMed]
- Hellman, M.; Rolando, S. Collectivist and individualist values traits in Finnish and Italian adolescents’ alcohol norms. Drugs Alcohol Today 2013, 13, 51–59. [Google Scholar] [CrossRef]
- Gossop, M.; Marsden, J.; Stewart, D. Dual dependence: Assessment of dependence upon alcohol and illicit drugs, and the relationship of alcohol dependence among drug misusers to patterns of drinking, illicit drug use and health problems. Addiction 2002, 97, 169–178. [Google Scholar] [CrossRef]
- Wölfling, K.; Thalemann, R.; Grüsser-Sinopoli, S. Computerspielsucht: Ein psychopathologischer symptomkomplex im jugendalter. Psychiatr. Prax. 2008, 35, 226–232. [Google Scholar] [CrossRef]
- Dreier, M.; Wölfling, K.; Duven, E.; Giralt, S.; Beutel, M.E.; Müller, K.W. Free-to-play: About addicted whales, at risk dolphins and healthy minnows. Monetarization design and internet gaming disorder. Addict. Behav. 2017, 64, 328–333. [Google Scholar] [CrossRef]
- Loton, D.; Borkoles, E.; Lubman, D.; Polman, R. Video game addiction, engagement and symptoms of stress, depression and anxiety: The mediating role of coping. Int. J. Ment. Health Addict. 2016, 14, 565–578. [Google Scholar] [CrossRef]
- Plante, C.N.; Gentile, D.A.; Groves, C.L.; Modlin, A.; Blanco-Herrera, J. Video games as coping mechanisms in the etiology of video game addiction. Psychol. Pop. Media Cult. 2019, 8, 385–394. [Google Scholar] [CrossRef]
- Ekhtiari, H.; Rezapour, T.; Aupperle, R.L.; Paulus, M.P. Neuroscience-informed psychoeducation for addiction medicine: A neurocognitive perspective. In Brain Research in Addiction; Calvey, T., Daniels, W., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; Volume 235, pp. 239–264. [Google Scholar] [CrossRef]
| Sociodemographic Variables | Total (n = 64) | |
|---|---|---|
| Gender | Male | 49 (76.5%) |
| Female | 15 (23.4%) | |
| Marital status | Same-sex civil partnership/married/Separated, but still legally in a same-sex civil partnership/married | 6 (9.3%) |
| Civil partnership has been dissolved/divorced | 9 (14%) | |
| Never registered a same-sex civil partnership/married | 32 (50%) | |
| Prefer not to say | 17 (26.5%) | |
| Qualification | Postgraduate degree (e.g., MA, PhD)/Degree (e.g., BA, BSc) | 8 (12.4%) |
| Professional qualification (e.g., teaching, nursing, accountancy)/Other vocational/work related qualifications | 4 (6.4%) | |
| Foundation degree/Progression diploma/Advanced diploma/Certificate or equivalent | 4 (6.4%) | |
| A levels/AS levels/VCEs/Higher diploma or equivalent/GCSEs/CSEs/O levels or equivalent | 24 (37.4%) | |
| No qualifications or education/Prefer not to say | 24 (37.4%) | |
| Videogame use * | Yes | 35 (54.7%) |
| No | 39 (45.3%) | |
| Years using playing videogames (M ± SD) | 19.96 ± 6.76 | |
| Hours spent playing videogames during a weekday (M ± SD) | 4 ± 5.37 | |
| Hours spent playing videogames during weekend day (M ± SD) | 3.61 ± 3.53 | |
| Videogame platform * | Online PC games | 3 (8.5%) |
| Offline PC games | 2 (5.7%) | |
| Online console games | 7 (20%) | |
| Offline console games | 8 (22.9%) | |
| Games for smartphones and tablets | 15 (42.9%) |
| Substance | How Many Times in the Last 30 Days? (in Days; Mean ± SD) * | Lifetime Use (in Years; Mean ± SD) | Route of Use ** | Major Problem (Currently Abstaining) *** | ||||
|---|---|---|---|---|---|---|---|---|
| Oral | Nasal | Smoking | Non-IV Injections | IV Injections | ||||
| Alcohol—any use | 3.4 ± 2.79 (n = 5) | 16.04 ± 10.11 (n = 58) | 92.7% | - | 7.3% | - | - | 46.9% |
| Alcohol—to intoxication | 1 ± 0 (n = 2) | 16.04 ± 10.11 (n = 47) | 93% | 2.3% | 4.7% | - | - | N/A |
| Heroin | 1 ± N/A (n = 1) | 13.10 ± 13.81 (n = 10) | - | 20% | 30% | - | 50% | 3.1% |
| Methadone | - | 8.16 ± 11.63 (n = 12) | 36.4% | 9.1% | - | - | 54.5% | 6.3% |
| Other (opiates/analgesics) | 15 ± N/A (n = 1) | 14.90 ± 12.43 (n = 11) | 63.6% | 9.1% | 9.1% | - | 18.2% | 7.8% |
| Barbiturates | 15 ± N/A (n = 1) | 19.66 ± 12.57 (n = 9) | 87.5% | 12.5% | - | - | - | - |
| Other (sedative/tranquilizer) | 5 ± 4.24 (n = 2) | 17.11 ± 14.64 (n = 9) | 66.7% | 33.3% | - | - | - | 3.1% |
| Cocaine | - | 6.26 ± 9.53 (n = 19) | 11.8% | 58.8% | - | - | 29.4% | 1.6% |
| Amphetamines | 3.21 ± 1.70 (n = 4) | 12.8 ± 9.10 (n = 50) | 15.2% | 2.2% | 58.7% | 2.2% | 21.7% | 68.7% |
| Ecstasy | - | 8.11 ± 8.08 (n = 36) | 58.1% | 19.3% | 9.7% | 3.2% | 9.7% | 4.7% |
| Cannabis | 7 ± 12 (n = 4) | 17.02 ± 10.79 (n = 46) | 18.2% | 81.8% | - | - | - | 28.1% |
| Hallucinogens | - | 12.76 ± 12.02 (n = 21) | 82.6% | 4.4% | 13% | - | - | 4.7% |
| Inhalants | 4.5 ± 4.94 (n = 2) | 7.90 ± 9.46 (n = 11) | 54.5% | 27.3% | 18.2% | - | - | - |
| Nicotine | 27.52 ± 5.77 (n = 17) | 18.56 ± 11.22 (n = 50) | 24.4% | 75.6% | - | - | - | 21.9% |
| More than one substance per day | 9.6 ± 10.16 (n = 5) | 16.62 ± 11.65 (n = 24) | 28.6% | 47.6% | - | - | 23.8% | N/A |
| Sociodemographic Variables | Total (n = 138) | |
|---|---|---|
| Gender | Male | 72 (54.5%) |
| Female Other | 59 (44.7%) 1 (0.8%) | |
| Marital status | Same-sex civil partnership/married/Separated, but still legally in a same-sex civil partnership/married | 29 (22%) |
| Civil partnership has been dissolved/divorced | 5 (3.8%) | |
| Widowed | 1 (0.7%) | |
| Never registered a same-sex civil partnership/married | 88 (66.7%) | |
| Prefer not to say | 9 (6.8%) | |
| Qualification | Postgraduate degree (e.g., MA, PhD)/Degree (e.g., BA, BSc) | 55 (41.7%) |
| Professional qualification (e.g., teaching, nursing, accountancy)/Other vocational/work related qualifications | 5 (3.8%) | |
| Foundation degree/Progression diploma/Advanced diploma/Certificate or equivalent | 8 (6.1%) | |
| A levels/AS levels/VCEs/Higher diploma or equivalent/GCSEs/CSEs/O levels or equivalent | 54 (40.9%) | |
| No qualifications or education/Prefer not to say | 10 (7.5 %) | |
| Videogame use * | Yes | 108 (81.8%) |
| No | 24 (18.2%) | |
| Years using playing videogames (M ± SD) | 13.10 ± 7.51 | |
| Hours spent playing videogames during a weekday (M ± SD) | 4.24 ± 7.23 | |
| Hours spent playing videogames during weekend day (M ± SD) | 3.92 ± 3.73 | |
| Videogame platform * | Online PC games | 18 (16.7%) |
| Offline PC games | 8 (7.4%) | |
| Online console games | 26 (24.1%) | |
| Offline console games | 21 (19.4%) | |
| Games for smartphones and tablets | 35 (32.4%) |
| DA-Z | BYSAS | CDS | BSMAS | BSAS | IDS9-SF | PGSI | |
|---|---|---|---|---|---|---|---|
| DA-Z | 0.12 | - | 0.26 | −0.04 | 0.01 | −0.14 | |
| BYSAS | 0.41 ** | - | 0.27 | 0.30 | 0.61 * | −0.40 | |
| CDS | 0.52 | 0.18 | - | - | - | - | |
| BSMAS | 0.03 | 0.19 | −0.40 | 0.44 | 0.38 | 0.10 | |
| BSAS | 0.16 | 0.26 | 0.07 | 0.47 ** | 0.29 | 0.29 | |
| IDS9-SF | 0.10 | 0.46 ** | 0.08 | 0.53 ** | 0.41 ** | −0.45 | |
| PGSI | 0.30 * | 0.13 | - | 0.17 | 0.26 | 0.14 | |
| IGDS9-SF | 0.04 | 0.39 ** | 0.21 | 0.21 | 0.16 | 0.59 ** | 0.14 |
| DA-Z | BYSAS | CDS | BSMAS | BSAS | IDS9 | PGSI | |
|---|---|---|---|---|---|---|---|
| DA-Z | 0.13 | 0.17 | 0.25 | 0.03 | 0.16 | −0.14 | |
| BYSAS | 0.19 | −0.16 | 0.20 | 0.69 ** | 0.36 | 0.24 | |
| CDS | −0.12 | 0.00 | −0.01 | 0.25 | 0.69 | −0.09 | |
| BSMAS | 0.39 | 0.45 | −0.07 | 0.25 | 0.67 ** | −0.03 | |
| BSAS | −0.01 | 0.08 | 0.22 | 0.38 | 0.35 | 0.15 | |
| IDS9-SF | 0.21 | 0.38 ** | −0.04 | 0.70 ** | 0.46 | −0.01 | |
| PGSI | 0.57 ** | 0.34 | 0.23 | 0.52 * | 0.17 | 0.27 | |
| IGD9-SF | 0.50 | 0.39 ** | −0.07 | 0.62 ** | 0.16 | 0.71 ** | 0.37 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burleigh, T.L.; Griffiths, M.D.; Sumich, A.; Wang, G.Y.; Kuss, D.J. Coping and Co-Occurrence of Gaming Disorder and Substance Use in Recovering Substance Users. J. Clin. Med. 2022, 11, 7370. https://doi.org/10.3390/jcm11247370
Burleigh TL, Griffiths MD, Sumich A, Wang GY, Kuss DJ. Coping and Co-Occurrence of Gaming Disorder and Substance Use in Recovering Substance Users. Journal of Clinical Medicine. 2022; 11(24):7370. https://doi.org/10.3390/jcm11247370
Chicago/Turabian StyleBurleigh, Tyrone L., Mark D. Griffiths, Alexander Sumich, Grace Y. Wang, and Daria J. Kuss. 2022. "Coping and Co-Occurrence of Gaming Disorder and Substance Use in Recovering Substance Users" Journal of Clinical Medicine 11, no. 24: 7370. https://doi.org/10.3390/jcm11247370
APA StyleBurleigh, T. L., Griffiths, M. D., Sumich, A., Wang, G. Y., & Kuss, D. J. (2022). Coping and Co-Occurrence of Gaming Disorder and Substance Use in Recovering Substance Users. Journal of Clinical Medicine, 11(24), 7370. https://doi.org/10.3390/jcm11247370






