Evaluation of Cardiovascular Activity and Emotional Experience in Healthcare Workers (HCWs) Operating in COVID-19 Wards
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Medical Examinations
2.4. Psychological Examinations
2.5. Statistical Analysis
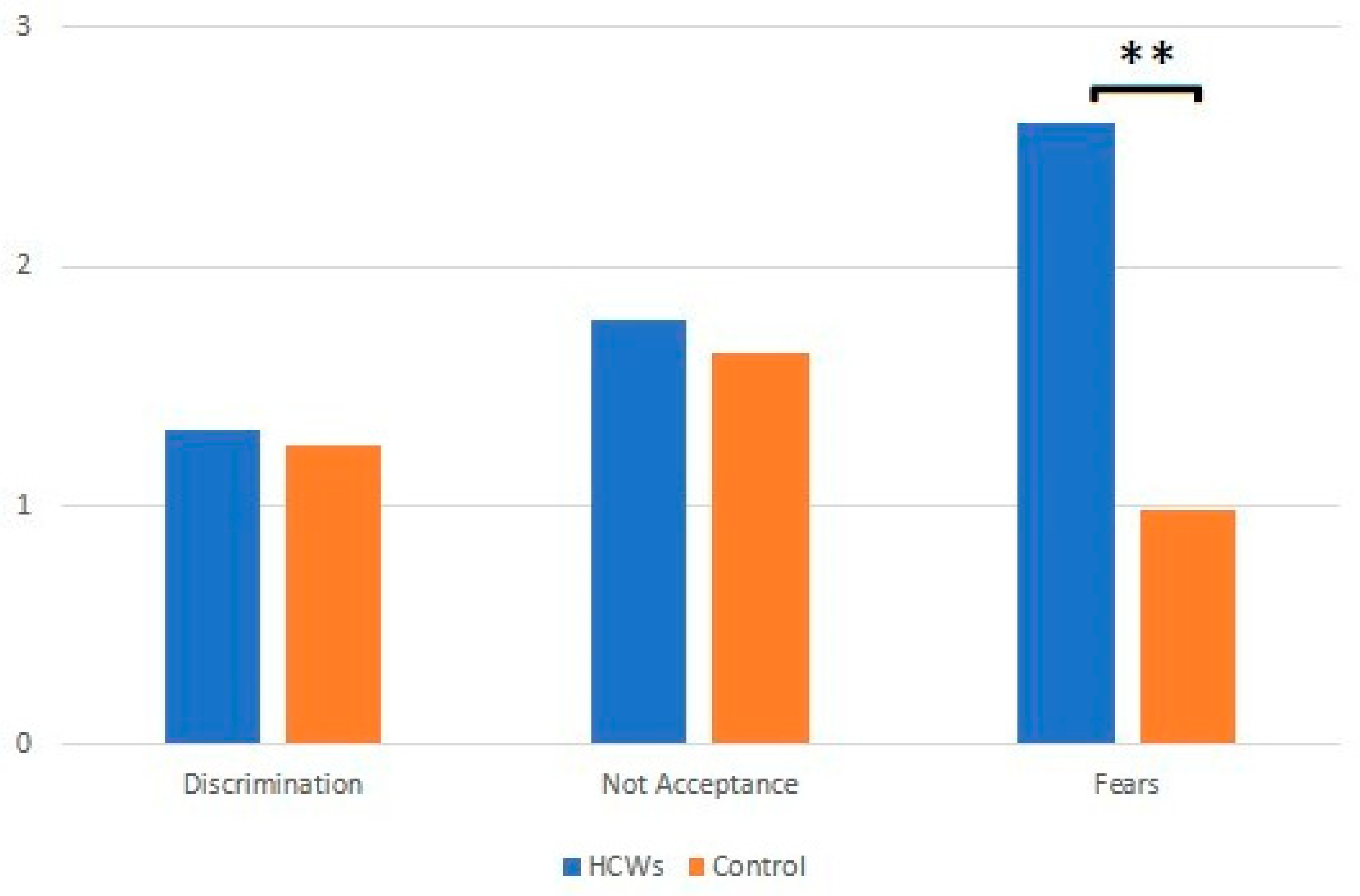
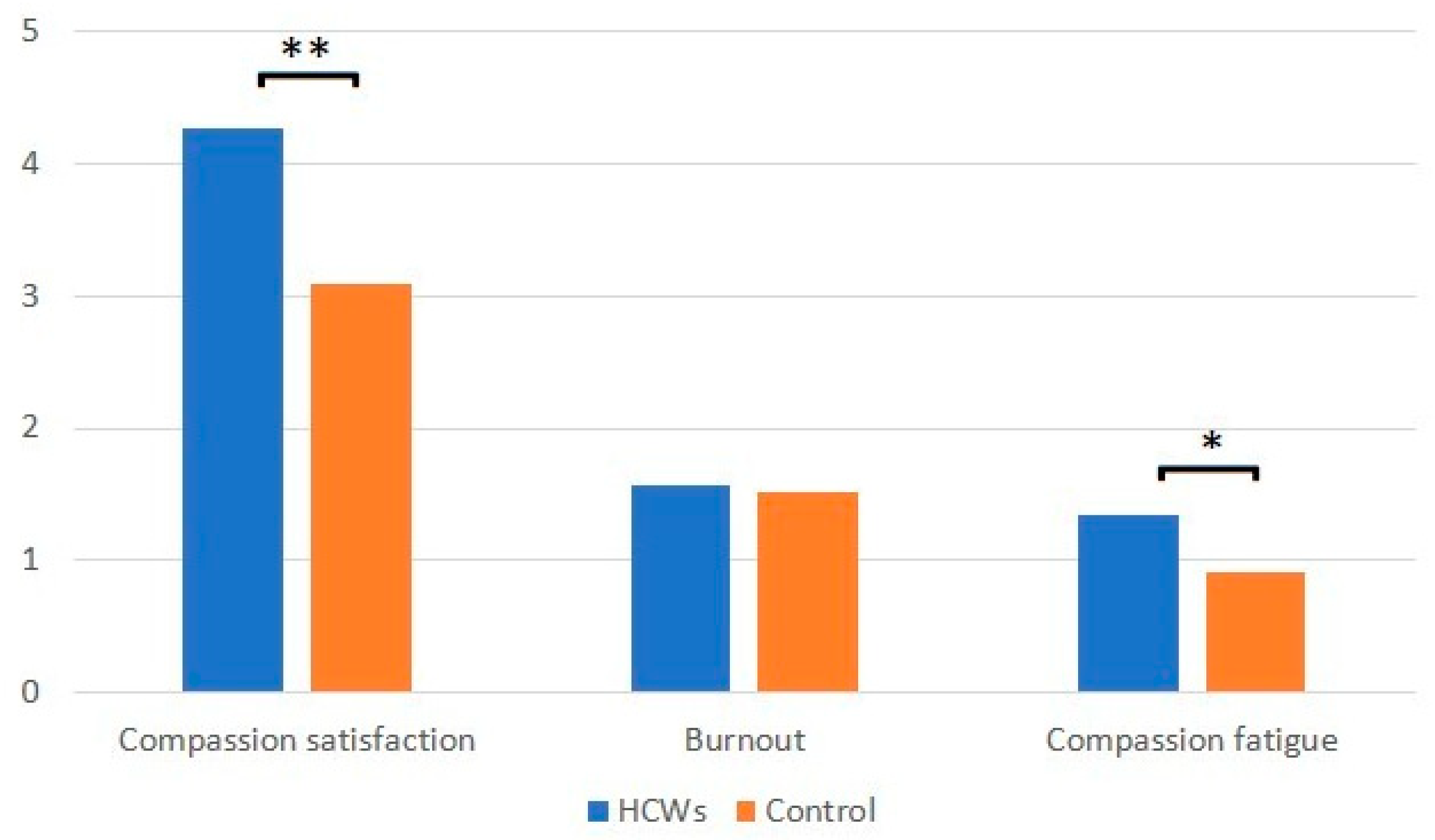
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chan, J.; Yuan, S.; Kok, K.H.; To, K.K.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.; Poon, R.W.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Yun, J.; Kim, T. Stress and work-related burnout in frontline health care professionals during the COVID-19 pandemic. Disaster Med. Public Health Prep. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Vella, F.; Senia, P.; Ceccarelli, M.; Vitale, E.; Maltezou, H.; Taibi, R.; Lleshi, A.; Venanzi, R.E.; Pellicanò, G.F.; Rapisarda, V.; et al. Transmission mode associated with coronavirus disease 2019: A review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7889–7904. [Google Scholar] [PubMed]
- Senia, P.; Vella, F.; Mucci, N.; Dounias, G.; Trovato, A.; Marconi, A.; Ledda, C.; Rapisarda, V.; Vitale, E. Survey on COVID-19-related mortality associated with occupational infection during the first phase of the pandemic: A systematic review. Exp. Ther. Med. 2022, 23, 10. [Google Scholar] [CrossRef]
- Gruppo di lavoro ISS Prevenzione e controllo delle Infezioni. Indicazioni ad Interim per un Utilizzo Razionale delle Protezioni per Infezione da SARS-COV-2 Nelle Attività Sanitarie e Sociosanitarie (Assistenza a Soggetti affetti da COVID-19) Nell’attuale Scenario Emergenziale SARS-COV-2; Versione del 28 marzo 2020; Istituto Superiore di Sanità: Roma, Italy, 2020; (Rapporto ISS COVID-19, n.2/2020 Rev.).
- Ledda, C.; Costantino, C.; Cuccia, M.; Maltezou, H.C.; Rapisarda, V. Attitudes of Healthcare Personnel towards Vaccinations before and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2703. [Google Scholar] [CrossRef]
- Cirrincione, L.; Rapisarda, V.; Ledda, C.; Vitale, E.; Provenzano, R.; Cannizzaro, E. Considerations on the update of the risk assessment document during the pandemic state by COVID-19 in Italy. Front. Public Health 2021, 9, 655927. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Cannizzaro, E.; Alba, D.; Conforto, A.; Cimino, L.; Mazzucco, W. SARS-CoV-2 pandemic in the mediterranean area: Epidemiology and perspectives. Eur. Mediterr. Biomed. J. 2020, 15, 102–106. [Google Scholar]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef]
- Elbay, R.Y.; Kurtulmuş, A.; Arpacıoğlu, S.; Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res. 2020, 290, 113130. [Google Scholar] [CrossRef]
- Yusra, H.K.; Tauqeer, H.M.; Nasser, H.A.; Abdulaziz, I.A. Work related stress factors among healthcare professionals during COVID-19 pandemic; a call for immediate action. Hosp. Pract. 2020, 48, 244–245. [Google Scholar]
- Rapisarda, V.; Vella, F.; Ledda, C.; Barattucci, M.; Ramaci, T. What Prompts Doctors to Recommend COVID-19 Vaccines: Is It a Question of Positive Emotion? Vaccines 2021, 9, 578. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.epicentro.iss.it/vaccini/covid-19-piano-vaccinazione (accessed on 18 January 2021).
- Task Force COVID-19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità. Epidemia COVID-19. Aggiornamento Nazionale: 27 ottobre 2021. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_27-ottobre-2021.pdf (accessed on 29 October 2021).
- Task Force COVID-19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità. Epidemia COVID-19. Aggiornamento Nazionale: 15 dicembre 2021. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_15-dicembre-2021.pdf (accessed on 17 December 2021).
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Barattucci, M.; Padovan, A.M.; Vitale, E.; Rapisarda, V.; Ramaci, T.; De Giorgio, A. Mindfulness-Based IARA Model® Proves Effective to Reduce Stress and Anxiety in Health Care Professionals. A Six-Month Follow-Up Study. Int. J. Environ. Res. Public Health 2019, 16, 4421. [Google Scholar] [CrossRef] [PubMed]
- Ramaci, T.; Barattucci, M.; Vella, F.; Senia, P.; Cannizzaro, E.; Scorciapino, A.; Ledda, C.; De Giorgio, A.; Rapisarda, V. Straining at Work and Its Relationship with Personality Profiles and Individual Consequences in Healthcare Workers (HCWs). Int. J. Environ. Res. Public Health 2020, 17, 610. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Khalid, I.; Khalid, T.; Qabajah, M.; Barnard, A.; Qushmaq, I. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies during a MERS-CoV Outbreak. Clin. Med. Res. 2016, 14, 7–14. [Google Scholar] [CrossRef]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—A review. Asian J. Psychiatr. 2020, 51, 102119. [Google Scholar] [CrossRef]
- Yesudhas, D.; Srivastava, A.; Gromiha, M.M. COVID-19 outbreak: History, mechanism, transmission, structural studies and therapeutics. Infection 2021, 49, 199–213. [Google Scholar] [CrossRef]
- Steptoe, A.; Kivimäki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef]
- Szarpak, L.; Filipiak, K.J.; Gasecka, A.; Pruc, M.; Drozd, A.; Jaguszewski, M.J. Correlation between takotsubo cardiomyopathy and SARS-CoV-2 infection. Med. Hypotheses 2021, 146, 110454. [Google Scholar] [CrossRef]
- Kivimäki, M.; Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat. Rev. Cardiol. 2018, 15, 215–229. [Google Scholar] [CrossRef] [PubMed]
- Cohen, B.E.; Edmondson, D.; Kronish, I.M. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. Am. J. Hypertens. 2015, 28, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Carroll, D.; Phillips, A.C.; Der, G.; Hunt, K.; Benzeval, M. Blood pressure reactions to acute mental stress and future blood pressure status: Data from the 12-year follow-up of the West of Scotland Study. Psychosom. Med. 2011, 73, 737–742. [Google Scholar] [CrossRef] [PubMed]
- al’Absi, M.; Devereux, R.B.; Rao, D.C.; Kitzman, D.; Oberman, A.; Hopkins, P.; Arnett, D.K. Blood pressure stress reactivity and left ventricular mass in a random community sample of African American and Caucasian men and women. Am. J. Cardiol. 2006, 97, 240–244. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Gerin, W.; Davidson, K.W.; Pickering, T.G.; Brosschot, J.F.; Thayer, J.F.; Christenfeld, N.; Linden, W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom. Med. 2003, 65, 22–35. [Google Scholar] [CrossRef]
- Pozzi, F.; Frajese, G. Regolazione neuroendocrina dello stress, recenti acquisizioni. Noos 2004, 3, 143–154. [Google Scholar]
- Sara, J.D.; Prasad, M.; Eleid, M.F.; Zhang, M.; Widmer, R.J.; Lerman, A. Association Between Work-Related Stress and Coronary Heart Disease: A Review of Prospective Studies Through the Job Strain, Effort-Reward Balance, and Organizational Justice Models. J. Am. Heart Assoc. 2018, 7, e008073. [Google Scholar] [CrossRef]
- Putri, T.; Priyono, D. It’s Demographic Associated with Social Stigma of the Person with COVID-19. J. Aisyah J. Ilmu Kesehat. 2021, 6, 253–258. [Google Scholar] [CrossRef]
- Stamm, B.H. The Professional Quality of Life Scale: Compassion Satisfaction, Burnout, and Compassion Fatigue/Secondary Trauma Scales; Sidran Press: Latherville, MD, USA, 2005. [Google Scholar]
- Palestini, L.; Prati, G.; Pietrantoni, L.; Cicognani, E. La qualità della vita professionale nel lavoro di soccorso: Un contributo alla validazione italiana della Professional Quality of Life Scale (ProQOL). Psicoter. Cogn. E Comport. 2009, 15, 205–227. [Google Scholar]
- See, L.C.; Shen, Y.M.; Chen, C.L.; Huang, T.M.; Huang, Y.H.; Huang, H.C.; Lin, S.R. Professional attitude of health care workers toward serving HIV/AIDS patients and drug users: Questionnaire design and evaluation of reliability and validity. AIDS Care 2011, 23, 1448–1455. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [PubMed]
- Tan, W.; Hao, F.; McIntyre, R.S.; Jiang, L.; Jiang, X.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020, 87, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Vitale, E.; Vella, F.; Filetti, V.; Cirrincione, L.; Indelicato, G.; Cannizzaro, E.; Rapisarda, V. How to prevent SARS-CoV-2 transmission in the agri-food industry during the first pandemic wave: Effects of seroprevalence. Appl. Sci. 2021, 11, 10051. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Canalella, A.; Vitale, E.; Vella, F.; Senia, P.; Cannizzaro, E.; Ledda, C.; Rapisarda, V. How the Heart Was Involved in COVID-19 during the First Pandemic Phase: A Review. Epidemiologia 2021, 2, 124–139. [Google Scholar] [CrossRef] [PubMed]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2021, 19, 2369–2382. [Google Scholar] [CrossRef]
- Wu, K.; Wei, X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med. Sci. Monit. Basic Res. 2020, 26, e924085. [Google Scholar] [CrossRef]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.I.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef]
- Shreffler, J.; Petrey, J.; Huecker, M. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West. J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar] [CrossRef]
- Shah, K.; Chaudhari, G.; Kamrai, D.; Lail, A.; Patel, R.S. How Essential Is to Focus on Physician’s Health and Burnout in Coronavirus (COVID-19) Pandemic? Cureus 2020, 12, e7538. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Kivimaki, M. Stress and cardiovascular disease: An up- date on current knowledge. Annu Rev. Public Health 2013, 34, 337–354. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, M.; Nyberg, S.T.; Batty, G.D.; Jokela, M.; Heikkilä, K.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; et al. Perceived job insecurity as a risk factor for incident coronary heart disease: Systematic review and meta-analysis. BMJ 2013, 347, f4746. [Google Scholar] [CrossRef] [PubMed]
- Fransson, E.I.; Heikkila, K.; Nyberg, S.T.; Zins, M.; Westerlund, H.; Westerholm, P.; Väänänen, A.; Virtanen, M.; Vahtera, J.; Theorell, T.; et al. Job strain as a risk factor for leisure-time physical inactivity: An individual-participant meta-analysis of up to 170,000 men and women—The IPD-Work consortium. Am. J. Epidemiol. 2012, 176, 1078–1089. [Google Scholar] [CrossRef] [PubMed]
- Heikkilä, K.; Fransson, E.I.; Nyberg, S.T.; Zins, M.; Westerlund, H.; Westerholm, P.; Virtanen, M.; Vahtera, J.; Suominen, S.; Steptoe, A.; et al. Job strain and health- related lifestyle: Findings from an individual participant meta-analysis of over 118,000 working adults. Am. J. Public Health 2013, 103, 2090–2097. [Google Scholar] [CrossRef]
- Rueda-Garrido, J.C.; Vicente-Herrero, M.T.; del Campo, T.M.; Reinoso-Barbero, L.; de la Hoz, R.E.; Delclos, G.L.; Kales, S.N.; Fernandez-Montero, A. Return to work guidelines for the COVID-19 pandemic. Occup. Med. 2020, 70, 300–305. [Google Scholar] [CrossRef]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Cmaj 2003, 168, 1245–1251. [Google Scholar]
- Huang, J.Z.; Han, M.F.; Luo, T.D.; Ren, A.K.; Zhou, X.P. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020, 38, 192–195. [Google Scholar]
- Murat, M.; Köse, S.; Savaşer, S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int. J. Ment. Health Nurs. 2021, 30, 533–543. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID- 19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Ni, M.Y.; Yang, L.; Leung, C.M.C.; Li, N.; Yao, X.I.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: Cross-sectional survey. JMIR Ment. Health 2020, 7, e19009. [Google Scholar] [CrossRef]
- De los Santos, J.A.A.; Labrague, L.J. Impact of COVID-19 on the Psychological Well-Being and Turnover Intentions of Frontline Nurses in the Community: A Cross-Sectional Study in the Philippines. medRxiv 2020. [Google Scholar] [CrossRef]
- Cirrincione, L.; Plescia, F.; Ledda, C.; Rapisarda, V.; Martorana, D.; Lacca, G.; Argo, A.; Zerbo, S.; Vitale, E.; Vinnikov, D.; et al. COVID-19 pandemic: New prevention and protection measures. Sustainability 2022, 14, 4766. [Google Scholar] [CrossRef]
| COVID-19 OU 30 (100%) | No COVID-19 OU 30 (100%) | p-Value | |
|---|---|---|---|
| Gender (men) | 18 (60%) | 18 (60%) | n.s. |
| Gender (women) | 12 (40%) | 12 (40%) | n.s. |
| Mean age (yrs) | 41.1 ± 7.7 | 40.3 ± 8.1 | n.s. |
| Working seniority (yrs) | 10.5 ± 6.4 | 10.1 ± 5.6 | n.s. |
| BMI | 24.7 ± 2.8 | 24.4 ± 6.7 | n.s. |
| Non-smoker | 30 (100%) | 30 (100%) | n.s. |
| Family history of cardiovascular diseases | 5 (17%) | 6 (20%) | n.s. |
| Anti-COVID-19 Vaccination | 30 (100%) | 30 (100%) | n.s. |
| Physicians | 9 (30%) | 10 (33%) | n.s. |
| Nurses | 15 (50%) | 15 (50%) | n.s. |
| Healthcare assistants | 6 (20%) | 5 (17%) | n.s. |
| Shift work | 30 (100%) | 30 (100%) | n.s. |
| Full-time worker | 30 (100%) | 30 (100%) | n.s. |
| Permanent contract | 18 (60%) | 17 (57%) | n.s. |
| Fixed-term contract | 12 (40%) | 13 (43%) | n.s. |
| T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|
| HCWs | Control | HCWs | Control | HCWs | Control | |
| SAP (mmHg) | 120.2 ± 8.7 *# | 119.3 ± 9.8 | 149.1 ± 11.8 *°ç# | 122.4 ± 9.7 ç | 128.4 ± 15.7 °# | 121.9 ± 10.4 ç |
| DAP (mmHg) | 80.6 ± 114 *# | 80.5 ± 7.2 | 103.7 ± 32,7 *°ç# | 82.6 ± 8.4 ç | 86.6 ± 7.3 °# | 82.3 ± 6.1 ç |
| CF (bpm) | 79.8 ± 6.0 *# | 78.6 ± 4.7 | 104.6 ± 13.7 *°ç# | 79.8 ± 7.2 ç | 90.7 ± 16.5 °# | 80.7 ± 6.6 ç |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vitale, E.; Filetti, V.; Vella, F.; Senia, P.; Rapisarda, L.; Matera, S.; Lombardo, C.; Vinnikov, D.; Rapisarda, V.; Ledda, C. Evaluation of Cardiovascular Activity and Emotional Experience in Healthcare Workers (HCWs) Operating in COVID-19 Wards. J. Clin. Med. 2022, 11, 7372. https://doi.org/10.3390/jcm11247372
Vitale E, Filetti V, Vella F, Senia P, Rapisarda L, Matera S, Lombardo C, Vinnikov D, Rapisarda V, Ledda C. Evaluation of Cardiovascular Activity and Emotional Experience in Healthcare Workers (HCWs) Operating in COVID-19 Wards. Journal of Clinical Medicine. 2022; 11(24):7372. https://doi.org/10.3390/jcm11247372
Chicago/Turabian StyleVitale, Ermanno, Veronica Filetti, Francesca Vella, Paola Senia, Lucia Rapisarda, Serena Matera, Claudia Lombardo, Denis Vinnikov, Venerando Rapisarda, and Caterina Ledda. 2022. "Evaluation of Cardiovascular Activity and Emotional Experience in Healthcare Workers (HCWs) Operating in COVID-19 Wards" Journal of Clinical Medicine 11, no. 24: 7372. https://doi.org/10.3390/jcm11247372
APA StyleVitale, E., Filetti, V., Vella, F., Senia, P., Rapisarda, L., Matera, S., Lombardo, C., Vinnikov, D., Rapisarda, V., & Ledda, C. (2022). Evaluation of Cardiovascular Activity and Emotional Experience in Healthcare Workers (HCWs) Operating in COVID-19 Wards. Journal of Clinical Medicine, 11(24), 7372. https://doi.org/10.3390/jcm11247372










