A Retrospective Taiwanese-Population-Based Clinical Study on Determining the Efficacy and Safety of Disposable Circumcision Anastomat
Abstract
1. Introduction
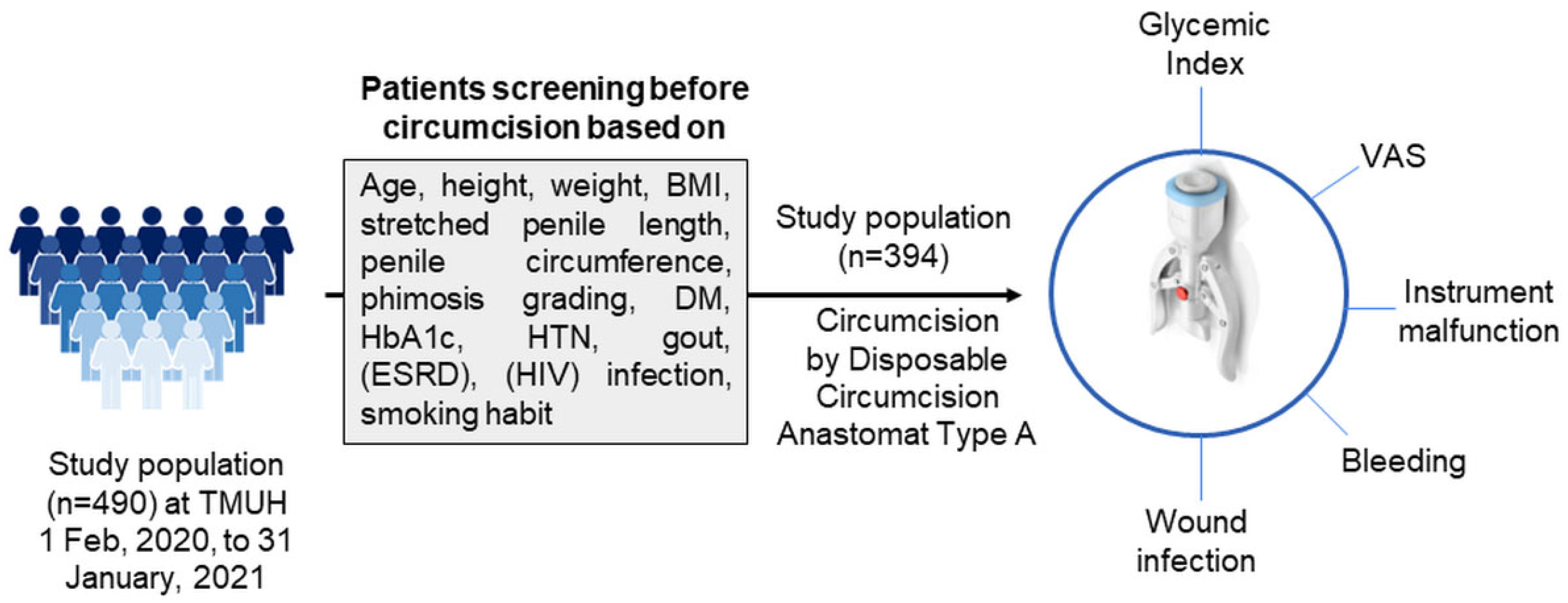
2. Materials and Methods
2.1. Patients Recruitment
2.2. Patient Demographics and Clinical Data
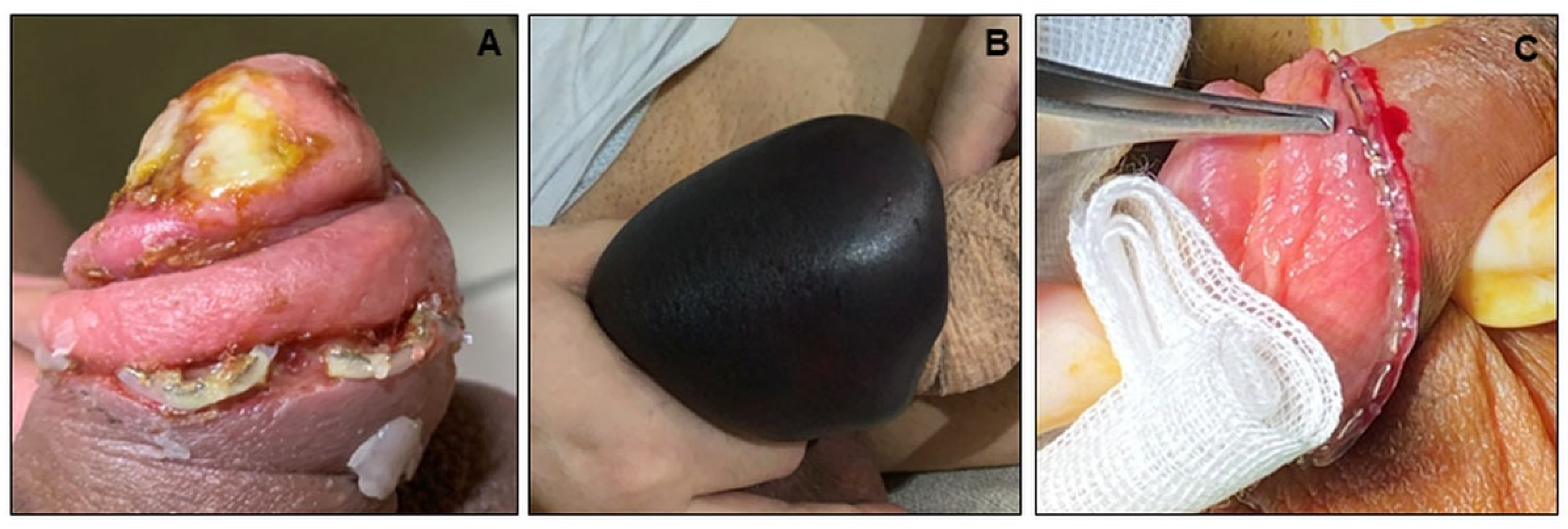
2.3. Surgical Instruments and Procedures
2.4. Statistical Analysis
3. Results
3.1. Demographics and Characteristics of Patients
3.2. Operation Time, Pain, Postoperative Bleeding, and the Adverse Events
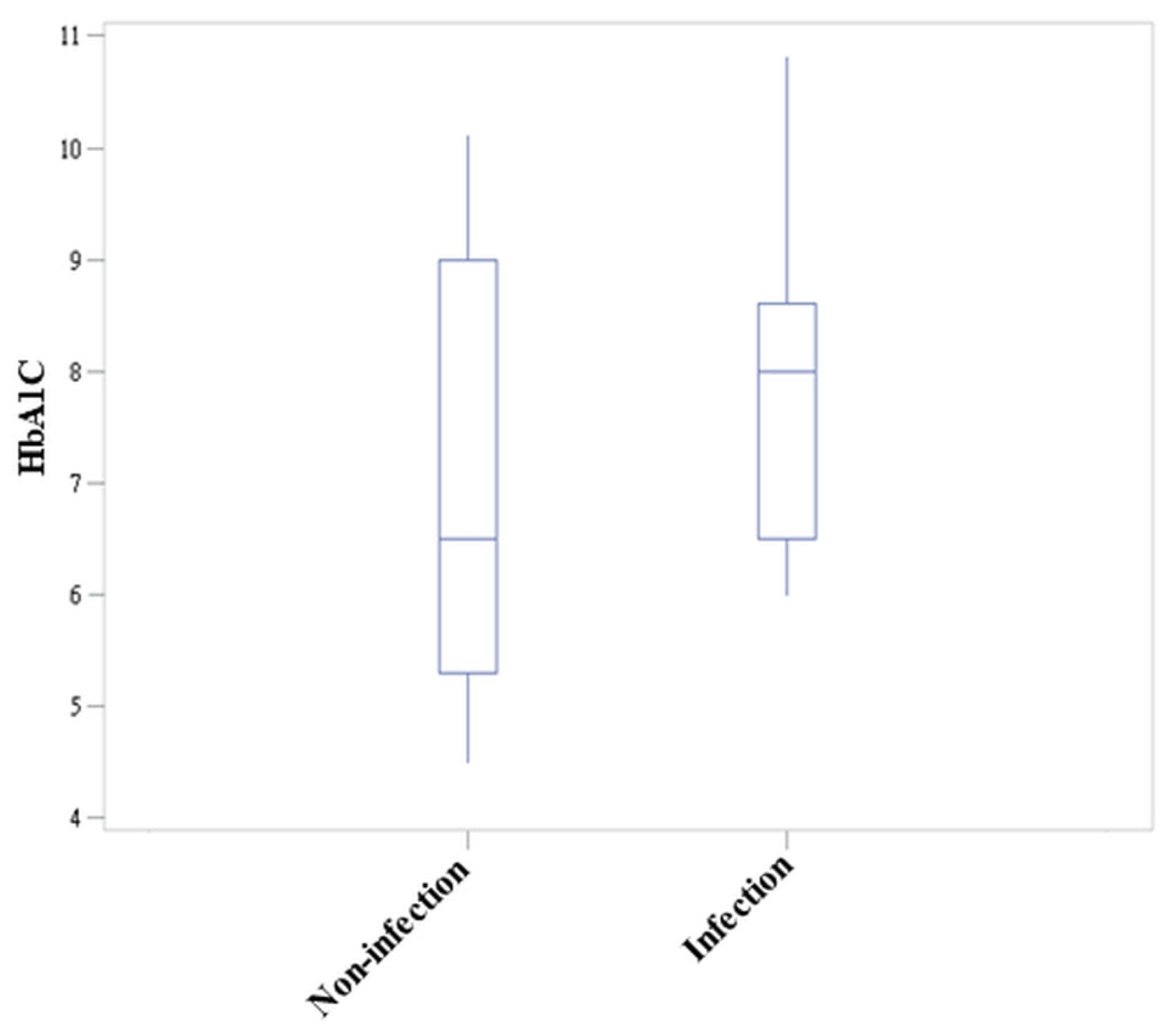
3.3. Association between Wound Infection and Clinical Parameters
3.4. Identifying the Risk Factor for Wound Infection
3.5. Impact of HbA1c on Wound Infection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Male Circumcision: Global Trends and Determinants of Prevalence, Safety and Acceptability; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Huo, Z.C.; Liu, G.; Li, X.Y.; Liu, F.; Fan, W.J.; Guan, R.H.; Li, P.F.; Mo, D.Y.; He, Y.Z. Use of a disposable circumcision suture device versus conventional circumcision: A systematic review and meta-analysis. Asian J. Androl. 2017, 19, 362–367. [Google Scholar] [CrossRef]
- Jacobs, A.J. Male circumcision. Assigning Responsibility for Children’s Health When Parents and Authorities Disagree: Whose Child? Springer: Berlin/Heidelberg, Germany, 2022; pp. 259–275. [Google Scholar]
- Kennedy, C.E.; Yeh, P.T.; Atkins, K.; Fonner, V.A.; Sweat, M.D.; O’Reilly, K.R.; Rutherford, G.W.; Baggaley, R.; Samuelson, J. Economic compensation interventions to increase uptake of voluntary medical male circumcision for HIV prevention: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0227623. [Google Scholar] [CrossRef]
- Morris, B.J.; Hankins, C.A.; Banerjee, J.; Lumbers, E.R.; Mindel, A.; Klausner, J.D.; Krieger, J.N. Does Male Circumcision Reduce Women’s Risk of Sexually Transmitted Infections, Cervical Cancer, and Associated Conditions? Front. Public Health 2019, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.; Necchi, A.; Muneer, A.; Tobias-Machado, M.; Tran, A.T.H.; Van Rompuy, A.-S.; Spiess, P.E.; Albersen, M. Penile cancer. Nat. Rev. Dis. Primers 2021, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Kohri, K. Circumcision related to urinary tract infections, sexually transmitted infections, human immunodeficiency virus infections, and penile and cervical cancer. Int. J. Urol. 2013, 20, 769–775. [Google Scholar] [CrossRef]
- Morris, B.J.; Wamai, R.G.; Henebeng, E.B.; Tobian, A.A.; Klausner, J.D.; Banerjee, J.; Hankins, C.A. Estimation of country-specific and global prevalence of male circumcision. Popul. Health Metr. 2016, 14, 4. [Google Scholar] [CrossRef]
- Simpson, E.; Carstensen, J.; Murphy, P. Neonatal circumcision: New recommendations & implications for practice. Mo. Med. 2014, 111, 222–230. [Google Scholar]
- Circumcision, T.F.O.; Blank, S.; Brady, M.; Buerk, E.; Carlo, W.; Diekema, D.; Freedman, A.; Maxwell, L.; Wegner, S. Circumcision Policy Statement. Pediatrics 2012, 130, 585–586. [Google Scholar] [CrossRef]
- World Health Organization. Male Circumcision for HIV Prevention: Manual for Male Circumcision under Local Anaesthesia and HIV Prevention Services for Adolescent Boys and Men; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- WHO; Jhpiego, U. Manual for Male Circumcision under Local Anaesthesia, Version; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Weiss, H.A.; Larke, N.; Halperin, D.; Schenker, I. Complications of circumcision in male neonates, infants and children: A systematic review. BMC Urol. 2010, 10, 2. [Google Scholar] [CrossRef]
- Shabanzadeh, D.M.; Clausen, S.; Maigaard, K.; Fode, M. Male Circumcision Complications—A Systematic Review, Meta-Analysis and Meta-Regression. Urology 2021, 152, 25–34. [Google Scholar] [CrossRef]
- Jiang, W.; Fu, J.L.; Guo, W.L.; Yan, Z.C.; Zheng, R.Q.; Lu, J.R.; Lai, X.D. A Modified Pressure Dressing to Avoid Severe Bleeding After Circumcision With a Disposable Circumcision Suture Device and a Discussion on the Mechanism of Bleeding with the Disposable Circumcision Suture Device. Sex. Med. 2021, 9, 100288. [Google Scholar] [CrossRef]
- Barone, M.A.; Ndede, F.; Li, P.S.; Masson, P.; Awori, Q.; Okech, J.; Cherutich, P.; Muraguri, N.; Perchal, P.; Lee, R.; et al. The Shang Ring device for adult male circumcision: A proof of concept study in Kenya. J. Acquir. Immune Defic. Syndr. 2011, 57, e7–e12. [Google Scholar] [CrossRef] [PubMed]
- Millard, P.S. Circumcision-what’s wrong with plastic rings? S. Afr. Med. J. 2012, 102, 126–129. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bromage, S.J.; Crump, A.; Pearce, I. Phimosis as a presenting feature of diabetes. BJU Int. 2008, 101, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Ke, C.-C.; Chen, C.-H.; Chen, J.-J.; Wang, C.-C. Balanoposthitis with a volcano-like appearance may be the first clinical presentation of undiagnosed diabetes mellitus. Incont. Pelvic. Floor. Dysfunct. 2011, 5, 120–121. [Google Scholar]
- Carey, I.M.; Critchley, J.A.; DeWilde, S.; Harris, T.; Hosking, F.J.; Cook, D.G. Risk of Infection in Type 1 and Type 2 Diabetes Compared With the General Population: A Matched Cohort Study. Diabetes Care 2018, 41, 513–521. [Google Scholar] [CrossRef]
- Carilli, M.; Asimakopoulos, A.D.; Pastore, S.; Germani, S.; Orecchia, L.; Agrò, E.F.; Miano, R. Can circumcision be avoided in adult male with phimosis? Results of the PhimoStop(TM) prospective trial. Transl. Androl. Urol. 2021, 10, 4152–4160. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Gu, D. Glycated Hemoglobin as a Marker for Predicting Outcomes of Patients With Stroke (Ischemic and Hemorrhagic): A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 642899. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.W.; Park, G.H.; Yun, W.J.; Rho, N.K.; Jang, K.A.; Won, C.H.; Chang, S.E.; Chung, S.J.; Lee, M.W. Adverse events associated with botulinum toxin injection: A multidepartment, retrospective study of 5310 treatments administered to 1819 patients. J. Dermatol. Treat 2014, 25, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.-M.; Xu, Z.-Q. The Morphological Classification of the Penile Frenulum in Chinese’s People and its Clinical Application Value in the Frenulum Malposition of Circumcision with the Disposable Circumcision Suture Device (DCSD); Research Square: Durham, NC, USA, 2021. [Google Scholar]
- Yuan, Y.; Zhang, Z.; Cui, W.; Gao, B.; Peng, J.; Xin, Z.; Guo, Y. Clinical investigation of a novel surgical device for circumcision. J. Urol. 2014, 191, 1411–1415. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Song, P.; Xu, C.; Wang, R.; Wei, L.; Zhao, X. Comparative efficacy and safety of different circumcisions for patients with redundant prepuce or phimosis: A network meta-analysis. Int. J. Surg. 2017, 43, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Rao, J.M.; Huang, H.; Chen, T.; Yang, C.G.; Pan, C.Z.; Deng, G.C.; Shen, L.J.; Qian, X.H.; Peng, M.K.; Zhou, H.D.; et al. Modified Circumcision Using the Disposable Circumcision Suture Device in Children: A Randomized Controlled Trial. Urology 2020, 143, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Baskin, L.S.; Canning, D.A.; Snyder, H.M.; Duckett, J.W. Treating complications of circumcision. Pediatr. Emerg. Care 1996, 12, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Moutschen, M.P.; Scheen, A.J.; Lefebvre, P.J. Impaired immune responses in diabetes mellitus: Analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabete Metab. 1992, 18, 187–201. [Google Scholar] [PubMed]
- Okonkwo, U.A.; DiPietro, L.A. Diabetes and Wound Angiogenesis. Int. J. Mol. Sci. 2017, 18, 1419. [Google Scholar] [CrossRef]
- Martin, E.T.; Kaye, K.S.; Knott, C.; Nguyen, H.; Santarossa, M.; Evans, R.; Bertran, E.; Jaber, L. Diabetes and Risk of Surgical Site Infection: A Systematic Review and Meta-analysis. Infect. Control Hosp. Epidemiol. 2016, 37, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Lv, B.D.; Zhang, S.G.; Zhu, X.W.; Zhang, J.; Chen, G.; Chen, M.F.; Shen, H.L.; Pei, Z.J.; Chen, Z.D. Disposable circumcision suture device: Clinical effect and patient satisfaction. Asian J. Androl. 2014, 16, 453–456. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yang, B.; Yu, W.; Han, Y.; Xu, Z.; Chen, H.; Chen, Y.; Dai, Y. Application of a novel disposable suture device in circumcision: A prospective non-randomized controlled study. Int. Urol. Nephrol. 2016, 48, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.D.; Lu, J.J.; Liu, W.H.; Zhou, J.; Yu, R.K.; Yu, B.; Zhang, X.J.; Shen, B.H. Adult male circumcision with a circular stapler versus conventional circumcision: A prospective randomized clinical trial. Braz. J. Med. Biol. Res. 2015, 48, 577–582. [Google Scholar] [CrossRef]
- Shen, J.; Shi, J.; Gao, J.; Wang, N.; Tang, J.; Yu, B.; Wang, W.; Wang, R. A Comparative Study on the Clinical Efficacy of Two Different Disposable Circumcision Suture Devices in Adult Males. Urol. J. 2017, 14, 5013–5017. [Google Scholar]
- Han, H.; Xie, D.W.; Zhou, X.G.; Zhang, X.D. Novel penile circumcision suturing devices versus the shang ring for adult male circumcision: A prospective study. Int. Braz. J. Urol. 2017, 43, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, Y.; Xia, S.; Zhu, Z.; Jia, L.; Liu, Y.; Jiang, M. Safety and efficacy of a novel disposable circumcision device: A pilot randomized controlled clinical trial at 2 centers. Med. Sci. Monit. 2014, 20, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.J.; Zhan, P.C.; Chen, Q.; Cheng, W.; Ye, F.Z.; Wang, Y.S.; Wang, J.J.; Li, J.H.; Tang, Z.M. A novel disposable circumcision device versus conventional surgery in the treatment of redundant prepuce and phimosis. Natl. J. Androl. 2017, 23, 1007–1013. [Google Scholar]
- Kline, K.A.; Bowdish, D.M. Infection in an aging population. Curr. Opin. Microbiol. 2016, 29, 63–67. [Google Scholar] [CrossRef]
- Verschoor, C.P.; Johnstone, J.; Loeb, M.; Bramson, J.L.; Bowdish, D.M. Anti-pneumococcal deficits of monocyte-derived macrophages from the advanced-age, frail elderly and related impairments in PI3K-AKT signaling. Hum. Immunol. 2014, 75, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Dorner, T.E.; Schwarz, F.; Kranz, A.; Freidl, W.; Rieder, A.; Gisinger, C. Body mass index and the risk of infections in institutionalised geriatric patients. Br. J. Nutr. 2010, 103, 1830–1835. [Google Scholar] [CrossRef]
- Nave, H.; Beutel, G.; Kielstein, J.T. Obesity-related immunodeficiency in patients with pandemic influenza H1N1. Lancet Infect. Dis. 2011, 11, 14–15. [Google Scholar] [CrossRef]
- Francken, A.B.; van de Wiel, H.B.; van Driel, M.F.; Weijmar Schultz, W.C. What importance do women attribute to the size of the penis? Eur. Urol. 2002, 42, 426–431. [Google Scholar] [CrossRef]
- Grov, C.; Parsons, J.T.; Bimbi, D.S. The association between penis size and sexual health among men who have sex with men. Arch. Sex. Behav. 2010, 39, 788–797. [Google Scholar] [CrossRef]
- Taylor, J.R.; Lockwood, A.P.; Taylor, A.J. The prepuce: Specialized mucosa of the penis and its loss to circumcision. Br. J. Urol. 1996, 77, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Czajkowski, M.; Czajkowska, K.; Zarańska, K.; Giemza, A.; Kłącz, J.; Sokołowska-Wojdyło, M.; Matuszewski, M. Male Circumcision Due to Phimosis as the Procedure That Is Not Only Relieving Clinical Symptoms of Phimosis But Also Improves the Quality of Sexual Life. Sex. Med. 2021, 9, 100315. [Google Scholar] [CrossRef]
| n = 394 | |
|---|---|
| Age, years (Mean ± SD) | 30.1 ± 7.05 |
| Height, cm (Mean ± SD) | 172.26 ± 6.75 |
| Weight, Kg (Mean ± SD) | 75.76 ± 15.47 |
| BMI, Kg/m2 (Mean ± SD) | 25.47 ± 4.73 |
| SPL, cm (Mean ± SD) | 10.12 ± 1.61 |
| HbA1C * (Mean ± SD) | 7.23 ± 1.71 |
| Penile circumference (Mean ± SD) | 7.00 ± 0.73 |
| DM [n, (%)] | 24, (6.09%) |
| HTN [n, (%)] | 8, (2.03%) |
| Gout [n, (%)] | 4, (1.02%) |
| ESRD [n, (%)] | 1, (0.25%) |
| HIV [n, (%)] | 1, (0.25%) |
| Phimosis grading | |
| Grade 0–1 [n, (%)] | 338, (85.79%) |
| Grade 2–3 [n, (%)] | 14, (3.55%) |
| Grade 4–5 [n, (%)] | 42, (10.66%) |
| Smoking [n, (%)] | 24, (6.09%) |
| n = 394 | |
|---|---|
| # Bleeding [n, (%)] | 10, (2.54%) |
| Infection [n, (%)] | 37, (9.39%) |
| Instrument malfunction [n, (%)] | 8, (2.03%) |
| Reoperation [n, (%)] | 5, (1.27%) |
| POD0, VAS (Mean ± SD) | 4.4 ± 2.4 |
| POD1, VAS (Mean ± SD) | 1.9 ± 1.6 |
| OP time, minute (Mean ± SD) | 31.4 ± 9.96 |
| Infection | p-Value * | ||
|---|---|---|---|
| No (n = 357) | Yes (n = 37) | ||
| Hypertension | 6, (1.68%) | 2, (5.40%) | 0.1677 |
| DM | 12, (3.36%) | 12, (32.43%) | <0.001 |
| Gout | 4, (1.12%) | 0, (0.00%) | 1.00 |
| Phimosis grading | 0.0534 | ||
| Grade 0–1 | 311, (87.11%) | 27, (72.97%) | - |
| Grade 2–3 | 12, (3.36%) | 2, (5.40%) | - |
| Grade 4–5 | 34, (9.52) | 8, (21.62%) | - |
| Reoperation | 0, (0.00%) | 5, (13.51%) | <0.001 |
| Age (Mean ± SD) | 29.9 ± 7.10 | 32.5 ± 6.14 | 0.0313 |
| Height (Mean ± SD) | 172.3 ± 6.91 | 171.9 ± 4.96 | 0.6434 |
| Weight (Mean ± SD) | 74.91 ± 14.82 | 83.94 ± 19.12 | 0.0081 |
| BMI (Mean ± SD) | 25.17 ± 4.52 | 28.31 ± 5.78 | 0.0026 |
| Penile stretch length (Mean ± SD) | 10.11 ± 1.63 | 10.20 ± 1.46 | 0.7601 |
| Penile circumference (Mean ± SD) | 6.97 ± 0.73 | 7.24 ± 0.72 | 0.0343 |
| POD0VAS (Mean ± SD) | 4.41 ± 2.44 | 4.30 ± 2.44 | 0.7959 |
| POD1VAS (Mean ± SD) | 1.87 ± 1.61 | 1.97 ± 1.80 | 0.7099 |
| OP time (Mean ± SD) | 31.21 ± 9.85 | 33.35 ± 10.98 | 0.2132 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | |
| DM | 13.800 | <0.0001 | 10.685 | 3.32–34.3 | <0.0001 | |
| HTN | 3.343 | 0.1486 | 0.415 | 0.056–3.053 | 0.3878 | |
| Phimosis grading | ||||||
| Grade 0–1 | Ref. | - | Ref. | - | ||
| Grade 2–3 | 1.920 | 0.4089 | 0.600 | 0.092–3.905 | 0.5933 | |
| Grade 4–5 | 2.711 | 0.0238 | 1.677 | 0.615–4.573 | 0.3127 | |
| Age | 1.052 | 0.0327 | 1.007 | 0.953–1.065 | 0.7915 | |
| BMI | 1.123 | 0.0002 | 1.061 | 0.984–1.143 | 0.1234 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, A.-C.; Laih, C.-Y.; Ku, F.-Y. A Retrospective Taiwanese-Population-Based Clinical Study on Determining the Efficacy and Safety of Disposable Circumcision Anastomat. J. Clin. Med. 2022, 11, 6206. https://doi.org/10.3390/jcm11206206
Chou A-C, Laih C-Y, Ku F-Y. A Retrospective Taiwanese-Population-Based Clinical Study on Determining the Efficacy and Safety of Disposable Circumcision Anastomat. Journal of Clinical Medicine. 2022; 11(20):6206. https://doi.org/10.3390/jcm11206206
Chicago/Turabian StyleChou, An-Chi, Chun-Yo Laih, and Fang-Yu Ku. 2022. "A Retrospective Taiwanese-Population-Based Clinical Study on Determining the Efficacy and Safety of Disposable Circumcision Anastomat" Journal of Clinical Medicine 11, no. 20: 6206. https://doi.org/10.3390/jcm11206206
APA StyleChou, A.-C., Laih, C.-Y., & Ku, F.-Y. (2022). A Retrospective Taiwanese-Population-Based Clinical Study on Determining the Efficacy and Safety of Disposable Circumcision Anastomat. Journal of Clinical Medicine, 11(20), 6206. https://doi.org/10.3390/jcm11206206







