Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Functional Outcomes in Acute Ischemic Stroke Patients Who Received Endovascular Thrombectomy
Abstract
:1. Introduction
2. Methods
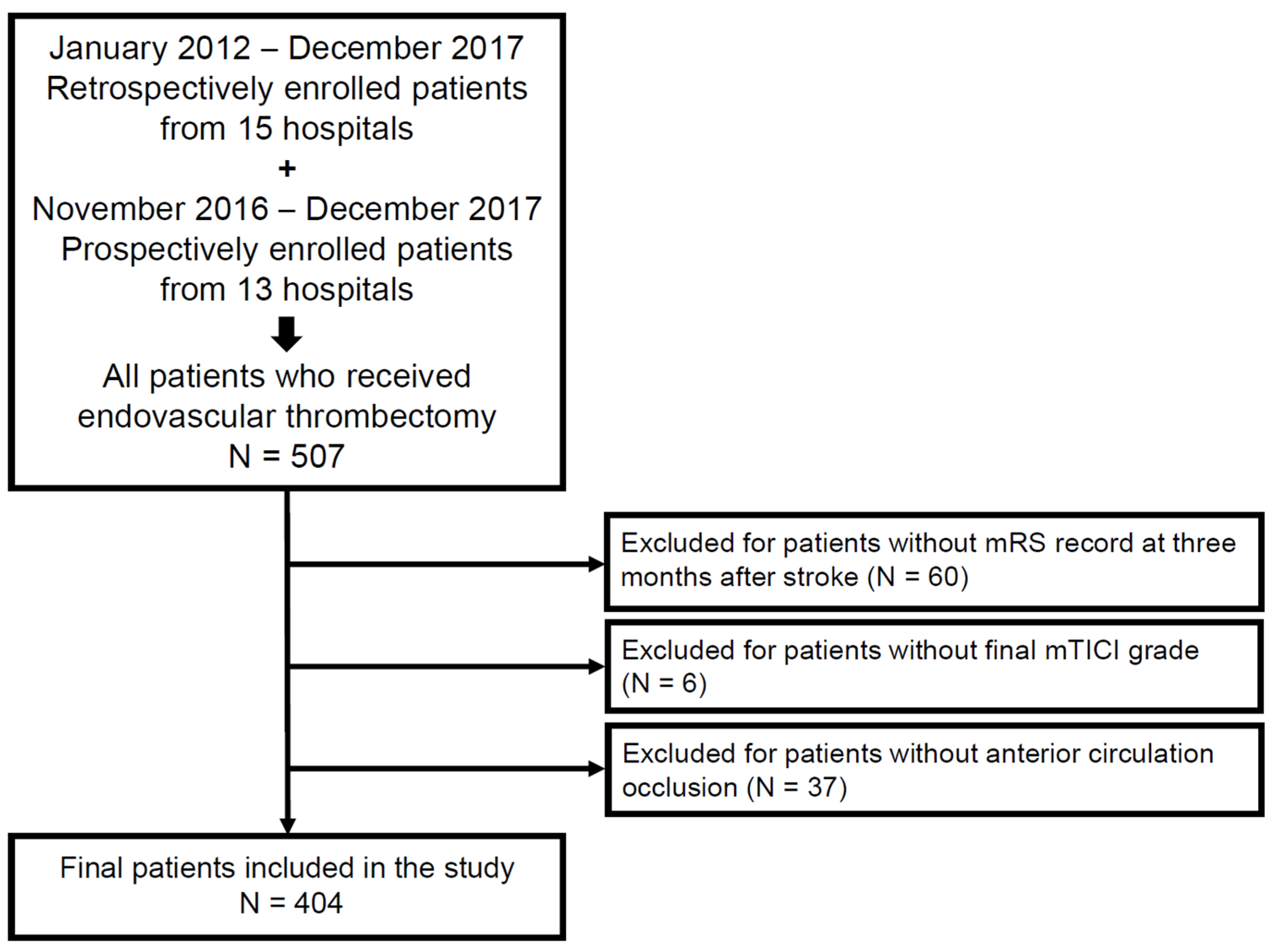
2.1. Study Popuslation
2.2. The Stroke Risk Scoring Systems
2.3. Statistical Analyses
3. Results
3.1. Study Population
3.2. Correlation between Stroke Risk Scores and Functional Outcomes
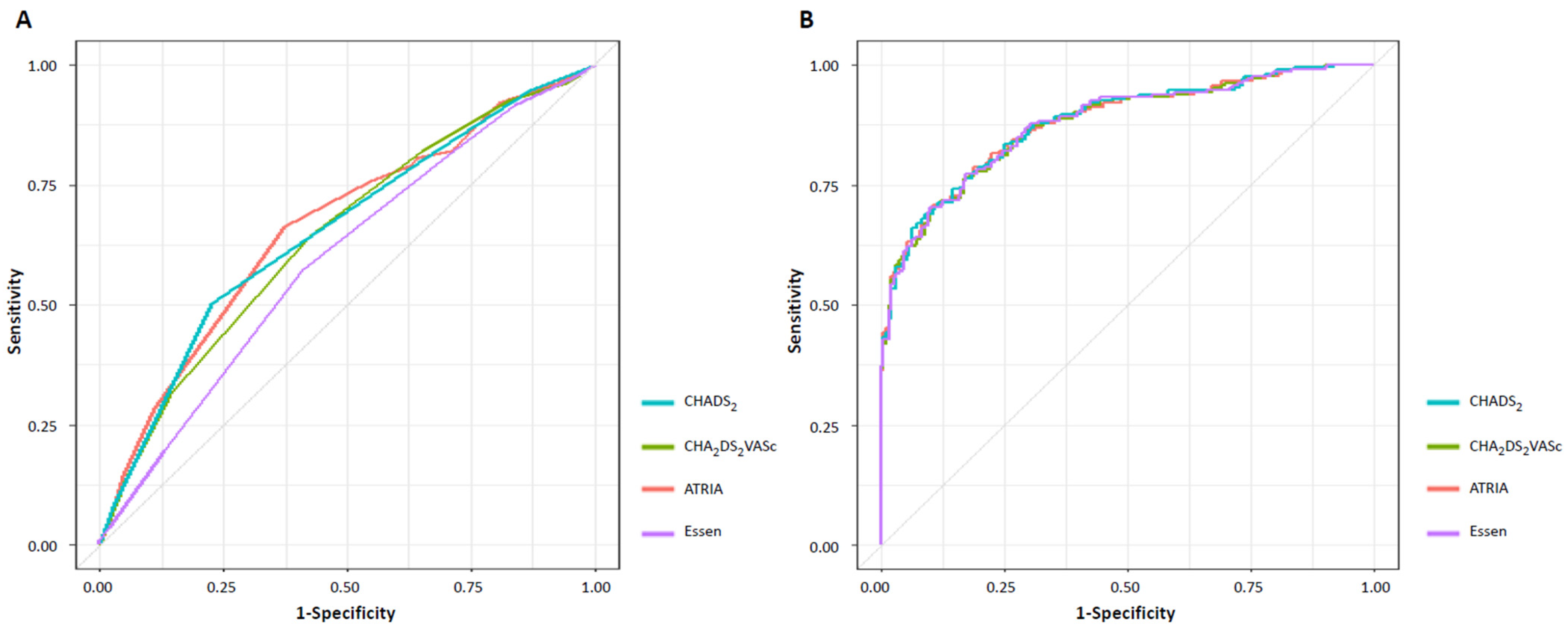
3.3. Comparison of Stroke Risk Scores for Unfavorable Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huttner, H.B.; Schwab, S. Malignant middle cerebral artery infarction: Clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol. 2009, 8, 949–958. [Google Scholar] [CrossRef]
- Ko, S.B.; Park, H.K.; Kim, B.M.; Heo, J.H.; Rha, J.H.; Kwon, S.U.; Kim, J.S.; Lee, B.C.; Suh, S.H.; Jung, C.; et al. 2019 Update of the Korean Clinical Practice Guidelines of Stroke for Endovascular Recanalization Therapy in Patients with Acute Ischemic Stroke. J. Stroke 2019, 21, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Berkhemer, O.A.; Fransen, P.S.; Beumer, D.; van den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.; et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.; Mitchell, P.J.; Kleinig, T.J.; Dewey, H.M.; Churilov, L.; Yassi, N.; Yan, B.; Dowling, R.J.; Parsons, M.W.; Oxley, T.J.; et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N. Engl. J. Med. 2015, 372, 1009–1018. [Google Scholar] [CrossRef]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Saver, J.L.; Goyal, M.; Bonafe, A.; Diener, H.C.; Levy, E.I.; Pereira, V.M.; Albers, G.W.; Cognard, C.; Cohen, D.J.; Hacke, W.; et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, M.; Hao, Y.; Zi, W.; Yang, D.; Zhou, Z.; Geng, Y.; Wang, Z.; Li, H.; Xu, G.; et al. Early Prediction of Poor Outcome Despite Successful Recanalization After Endovascular Treatment for Anterior Large Vessel Occlusion Stroke. World Neurosurg. 2018, 115, e312–e321. [Google Scholar] [CrossRef]
- Nie, X.; Pu, Y.; Zhang, Z.; Liu, X.; Duan, W.; Liu, L. Futile Recanalization after Endovascular Therapy in Acute Ischemic Stroke. Biomed Res. Int. 2018, 2018, 5879548. [Google Scholar] [CrossRef]
- Gilberti, N.; Gamba, M.; Premi, E.; Costa, A.; Vergani, V.; Delrio, I.; Spezi, R.; Dikran, M.; Frigerio, M.; Gasparotti, R.; et al. Leukoaraiosis is a predictor of futile recanalization in acute ischemic stroke. J. Neurol. 2017, 264, 448–452. [Google Scholar] [CrossRef]
- Hussein, H.M.; Georgiadis, A.L.; Vazquez, G.; Miley, J.T.; Memon, M.Z.; Mohammad, Y.M.; Christoforidis, G.A.; Tariq, N.; Qureshi, A.I. Occurrence and predictors of futile recanalization following endovascular treatment among patients with acute ischemic stroke: A multicenter study. Am. J. Neuroradiol. 2010, 31, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, D.H.; Cha, M.J.; Song, T.J.; Park, J.H.; Lee, H.S.; Nam, C.M.; Nam, H.S.; Kim, Y.D.; Heo, J.H. Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction. Atherosclerosis 2012, 224, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.F.; Waterman, A.D.; Shannon, W.; Boechler, M.; Rich, M.W.; Radford, M.J. Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA 2001, 285, 2864–2870. [Google Scholar] [CrossRef]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef]
- Singer, D.E.; Chang, Y.; Borowsky, L.H.; Fang, M.C.; Pomernacki, N.K.; Udaltsova, N.; Reynolds, K.; Go, A.S. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: The ATRIA study stroke risk score. J. Am. Heart Assoc. 2013, 2, e000250. [Google Scholar] [CrossRef]
- Kim, Y.D.; Cha, M.J.; Kim, J.; Lee, D.H.; Lee, H.S.; Nam, C.M.; Nam, H.S.; Heo, J.H. Increases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke 2011, 42, 930–934. [Google Scholar] [CrossRef]
- Cha, M.-J.; Lee, H.S.; Kim, Y.D.; Nam, H.S.; Heo, J.H. The association between asymptomatic coronary artery disease and CHADS2and CHA2DS2-VASc scores in patients with stroke. Eur. J. Neurol. 2013, 20, 1256–1263. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, M.-S.; Yoo, J.; Kim, Y.D.; Park, H.; Kim, B.M.; Bang, O.Y.; Kim, H.C.; Han, E.; Kim, D.J.; et al. Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Unsuccessful Recanalization after Endovascular Thrombectomy in Acute Ischemic Stroke Patients. J. Clin. Med. 2022, 11, 274. [Google Scholar] [CrossRef]
- Weimar, C.; Diener, H.C.; Alberts, M.J.; Steg, P.G.; Bhatt, D.L.; Wilson, P.W.; Mas, J.L.; Röther, J. The Essen stroke risk score predicts recurrent cardiovascular events: A validation within the REduction of Atherothrombosis for Continued Health (REACH) registry. Stroke 2009, 40, 350–354. [Google Scholar] [CrossRef]
- Kim, Y.D.; Heo, J.H.; Yoo, J.; Park, H.; Kim, B.M.; Bang, O.Y.; Kim, H.C.; Han, E.; Kim, D.J.; Heo, J.; et al. Improving the Clinical Outcome in Stroke Patients Receiving Thrombolytic or Endovascular Treatment in Korea: From the SECRET Study. J. Clin. Med. 2020, 9, 717. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.D.; Nam, H.S.; Yoo, J.; Park, H.; Sohn, S.-I.; Hong, J.-H.; Kim, B.M.; Kim, D.J.; Bang, O.Y.; Seo, W.-K.; et al. Prediction of Early Recanalization after Intravenous Thrombolysis in Patients with Large-Vessel Occlusion. J. Stroke 2021, 23, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.; Kim, Y.D.; Park, H.; Kim, B.M.; Bang, O.Y.; Kim, H.C.; Han, E.; Kim, D.J.; Heo, J.; Kim, M.; et al. Immediate and Long-Term Outcomes of Reperfusion Therapy in Patients With Cancer. Stroke 2021, 52, 2026–2034. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, O.; Giray, S.; Arlier, Z.; Bas, D.F.; Inanç, Y.; Colak, E. Predictors of a Good Outcome after Endovascular Stroke Treatment with Stent Retrievers. Sci. World J. 2015, 2015, 403726. [Google Scholar] [CrossRef]
- Song, T.J.; Kim, J.; Kim, Y.D.; Nam, H.S.; Lee, H.S.; Nam, C.M.; Heo, J.H. The distribution of cerebral microbleeds determines their association with arterial stiffness in non-cardioembolic acute stroke patients. Eur. J. Neurol. 2014, 21, 463–469. [Google Scholar] [CrossRef]
- Song, T.J.; Kim, Y.D.; Yoo, J.; Kim, J.; Chang, H.J.; Hong, G.R.; Shim, C.Y.; Song, D.; Heo, J.H.; Nam, H.S. Association between Aortic Atheroma and Cerebral Small Vessel Disease in Patients with Ischemic Stroke. J. Stroke 2016, 18, 312–320. [Google Scholar] [CrossRef]
- Song, T.J.; Chang, Y.; Shin, M.J.; Heo, J.H.; Kim, Y.J. Low levels of plasma omega 3-polyunsaturated fatty acids are associated with cerebral small vessel diseases in acute ischemic stroke patients. Nutr. Res. 2015, 35, 368–374. [Google Scholar] [CrossRef]
- Song, T.J.; Kim, J.; Lee, H.S.; Nam, C.M.; Nam, H.S.; Kim, Y.D.; Heo, J.H. Distribution of cerebral microbleeds determines their association with impaired kidney function. J. Clin. Neurol. 2014, 10, 222–228. [Google Scholar] [CrossRef]
- Nam, H.S.; Kim, Y.D.; Yoo, J.; Park, H.; Kim, B.M.; Bang, O.Y.; Kim, H.C.; Han, E.; Kim, D.J.; Heo, J.; et al. Comorbidity index for predicting mortality at 6 months after reperfusion therapy. Sci. Rep. 2021, 11, 5963. [Google Scholar] [CrossRef]
- Desilles, J.P.; Meseguer, E.; Labreuche, J.; Lapergue, B.; Sirimarco, G.; Gonzalez-Valcarcel, J.; Lavallée, P.; Cabrejo, L.; Guidoux, C.; Klein, I.; et al. Diabetes mellitus, admission glucose, and outcomes after stroke thrombolysis: A registry and systematic review. Stroke 2013, 44, 1915–1923. [Google Scholar] [CrossRef]
- Huang, X.; Guo, H.; Yuan, L.; Cai, Q.; Zhang, M.; Zhang, Y.; Zhu, W.; Li, Z.; Yang, Q.; Zhou, Z.; et al. Blood pressure variability and outcomes after mechanical thrombectomy based on the recanalization and collateral status. Ther. Adv. Neurol. Disord. 2021, 14, 1756286421997383. [Google Scholar] [CrossRef] [PubMed]
- Noh, Y.; Jung, C.K.; Hong, J.H.; Jeong, J.H.; Chang, J.Y.; Kim, B.J.; Bae, H.J.; Kwon, O.K.; Oh, C.W.; Han, M.K. Recanalization Rate and Clinical Outcome in Acute Carotid-T Occlusion. Eur. Neurol. 2015, 74, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; De Miquel, M.A.; Molina, C.A.; Rovira, A.; Román, L.S.; Serena, J.; Abilleira, S.; Ribo, M.; et al. Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Lane, D.A.; Lip, G.Y. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation 2012, 126, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Aspberg, S.; Chang, Y.; Atterman, A.; Bottai, M.; Go, A.S.; Singer, D.E. Comparison of the ATRIA, CHADS2, and CHA2DS2-VASc stroke risk scores in predicting ischaemic stroke in a large Swedish cohort of patients with atrial fibrillation. Eur. Heart J. 2016, 37, 3203–3210. [Google Scholar] [CrossRef] [PubMed]
- Katki, H.A. Quantifying risk stratification provided by diagnostic tests and risk predictions: Comparison to AUC and decision curve analysis. Stat. Med. 2019, 38, 2943–2955. [Google Scholar] [CrossRef]
| EVT— Followed Up to 3 Months (N = 404) | p-Value | Successful Recanalization— Followed Up to 3 Months (N = 332) | p-Value | |||
|---|---|---|---|---|---|---|
| Favorable Outcome (mRS 0–2) (N = 191) | Unfavorable Outcome (mRS 3–6) (N = 213) | Favorable Outcome (mRS 0–2) (N = 181) | Unfavorable Outcome (mRS 3–6) (N = 151) | |||
| Age, years, mean (SD) | 72.6 ± 13.2 | 79.7 ± 12.4 | <0.001 | 73.0 ± 12.7 | 79.0 ± 12.3 | <0.001 |
| Female, (%) | 86 (45.0%) | 99 (46.5%) | 0.847 | 83 (45.9%) | 68 (45.0%) | 0.969 |
| BMI (kg/m2) | 21.4 ± 4.0 | 20.2 ± 4.2 | 0.003 | 21.3 ± 3.9 | 20.1 ± 4.0 | 0.005 |
| Vascular risk factors | ||||||
| Hypertension, (%) | 142 (74.4%) | 161 (75.6%) | 0.863 | 134 (74.0%) | 107 (70.9%) | 0.602 |
| Diabetes mellitus, (%) | 82 (42.9%) | 148 (69.5%) | <0.001 | 78 (43.1%) | 100 (66.2%) | <0.001 |
| Hypercholesterolemia, (%) | 85 (44.5%) | 96 (45.1%) | 0.989 | 81 (44.8%) | 68 (45.0%) | >0.999 |
| Current smoking, (%) | 41 (21.5%) | 29 (13.6%) | 0.051 | 36 (19.9%) | 19 (12.6%) | 0.102 |
| eGFR < 60 mL/min, (%) | 72 (37.7%) | 131 (61.5%) | <0.001 | 67 (37.0%) | 93 (61.6%) | <0.001 |
| Comorbidities | ||||||
| Atrial fibrillation (%) | 95 (49.7%) | 126 (59.2%) | 0.072 | 90 (49.7%) | 90 (59.6%) | 0.091 |
| Heart failure, (%) | 11 (5.8%) | 26 (12.2%) | 0.038 | 11 (6.1%) | 17 (11.3%) | 0.135 |
| Coronary disease, (%) | 67 (35.1%) | 53 (24.9%) | 0.033 | 66 (36.5%) | 40 (26.5%) | 0.068 |
| Peripheral artery disease, (%) | 5 (2.6%) | 10 (4.7%) | 0.402 | 4 (2.2%) | 6 (4.0%) | 0.539 |
| Previous infarction, (%) | 34 (17.8%) | 57 (26.8%) | 0.042 | 32 (17.7%) | 39 (25.8%) | 0.095 |
| Previous hemorrhage | 7 (3.7%) | 13 (6.1%) | 0.369 | 7 (3.9%) | 8 (5.3%) | 0.719 |
| Medication before admission | ||||||
| Prior antiplatelet therapy, (%) | 57 (29.8%) | 74 (34.7%) | 0.345 | 55 (30.4%) | 52 (34.4%) | 0.504 |
| Prior anticoagulation therapy, (%) | 38 (19.9%) | 29 (13.6%) | 0.119 | 37 (20.4%) | 21 (13.9%) | 0.157 |
| Prior statin therapy, (%) | 58 (30.4%) | 68 (31.9%) | 0.818 | 56 (30.9%) | 51 (33.8%) | 0.665 |
| Initial NIHSS score, median ((IQR) | 12 (7–16) | 18 (13–21) | <0.001 | 12 (7–16) | 17 (13–20.5) | <0.001 |
| Treatment | ||||||
| IA thrombectomy alone, (%) | 100 (52.4%) | 145 (68.1%) | 0.002 | 95 (52.5%) | 99 (65.6%) | 0.022 |
| Combined IV/IA thrombolysis *, (%) | 91 (47.6%) | 68 (31.9%) | 0.002 | 86 (47.5%) | 52 (34.4%) | 0.022 |
| Stent-retriever alone, (%) | 154 (80.6%) | 144 (67.6%) | 0.004 | 176 (97.2%) | 141 (93.4%) | 0.155 |
| Aspiration alone, (%) | 5 (2.6%) | 18 (8.5%) | 0.021 | 5 (2.76%) | 10 (6.62%) | 0.1553 |
| Combined stent-retriever/aspiration **, (%) | 32 (16.8%) | 51 (23.9%) | 0.096 | 31 (17.1%) | 28 (18.5%) | 0.848 |
| Number of stent-retrieval passes (SD) | 1.8 ± 1.3 | 2.4 ± 2.3 | <0.001 | 1.7 ± 1.2 | 2.3 ± 2.0 | 0.004 |
| Onset to puncture, min, mean (SD) | 343.1 ± 447.6 | 335.4 ± 301.0 | 0.842 | 344.1 ± 457.3 | 324.9 ± 299.1 | 0.646 |
| Onset to recanalization, min, mean (SD) | N/A | N/A | 418.5 ± 482.8 | 408.7 ± 303.9 | 0.825 | |
| LNT-to-puncture time (within 6 h) | 142 (74.4%) | 150 (70.4%) | 0.442 | 134 (74.0%) | 106 (70.2%) | 0.513 |
| Stroke etiology | 0.418 | 0.258 | ||||
| Cardioembolic | 103 (53.9%) | 124 (58.2%) | 98 (54.1%) | 89 (58.9%) | ||
| Large artery atherosclerosis | 35 (18.3%) | 29 (13.6%) | 32 (17.7%) | 17 (11.3%) | ||
| Undetermined or others | 53 (27.8%) | 60 (28.2%) | 51 (28.2%) | 45 (29.8%) | ||
| Image finding after EVT | ||||||
| mTICI 2b-3 | 181 (94.8%) | 151 (70.9%) | <0.001 | N/A | N/A | N/A |
| Hemorrhagic transformation | 9 (4.7%) | 65 (30.6%) | <0.001 | 54 (29.8%) | 87 (57.6%) | <0.001 |
| Pre-admission stroke risk score, median (IQR) | ||||||
| CHADS2 score | 2 (1–2) | 3 (2–3) | <0.001 | 2 (1–2) | 2 (2–3) | <0.001 |
| CHA2DS2VASc score | 3 (2–4) | 4 (3–5) | <0.001 | 3 (2–4) | 4 (3–5) | <0.001 |
| ATRIA score | 7 (2–8.5) | 8 (7–10) | <0.001 | 7 (2–8) | 8 (6–10) | <0.001 |
| Essen score | 3 (2–4) | 4 (3–4) | <0.001 | 3 (2–4) | 4 (3–4) | 0.026 |
| CHADS2 | p-Value | CHA2DS2VASc | p-Value | ATRIA | p-Value | Essen | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Variables | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| BMI, per-1-kg/m2 increase | 0.940 (0.878–1.006) | 0.075 | 0.966 (0.899–1.038) | 0.075 | 0.966 (0.899–1.038) | 0.341 | 0.962 (0.985–1.034) | 0.297 |
| Current smoking | 0.545 (0.253–1.173) | 0.121 | 0.533 (0.248–1.147) | 0.108 | 0.533 (0.247–1.148) | 0.108 | 0.466 (0.220–0.989) | 0.047 |
| eGFR < 60 mL/min | 1.484 (0.812–2.714) | 0.200 | 1.691 (0.961–2.973) | 0.068 | 1.542 (0.802–2.967) | 0.194 | 1.897 (1.108–3.246) | 0.020 |
| Atrial fibrillation | 0.913 (0.515–1.619) | 0.755 | 0.949 (0.536–1.678) | 0.856 | 0.955 (0.542–1.684) | 0.874 | 0.931 (0.526–1.649) | 0.806 |
| Heart failure | 1.418 (0.484–4.158) | 0.525 | 1.671 (0.550–5.073) | 0.365 | 1.918 (0.706–5.210) | 0.202 | 2.265 (0.895–5.733) | 0.845 |
| Coronary disease | 0.479 (0.267–0.858) | 0.013 | 0.498 (0.278–0.889) | 0.018 | 0.506 (0.285–0.897) | 0.020 | 0.511 (0.287–0.910) | 0.022 |
| Previous infarction | 1.675 (0.868–3.233) | 0.124 | 1.649 (0.874–3.111) | 0.123 | 1.427 (0.655–3.108) | 0.371 | 1.801 (0.954–3.426) | 0.070 |
| Initial NIHSS score, per 1-score increase | 1.183 (1.126–1.243) | <0.001 | 1.176 (1.120–1.236) | <0.001 | 1.178 (1.121–1.238) | <0.001 | 1.180 (1.123–1.239) | <0.001 |
| IV thrombolysis | ||||||||
| IA thrombolysis alone | Reference | Reference | Reference | Reference | ||||
| Combined IA/IV thrombolysis * | 0.420 (0.243–0.727) | 0.002 | 0.429 (0.248–0.744) | 0.003 | 0.428 (0.248–0.738) | 0.002 | 0.448 (0.257–0.781 | 0.005 |
| IA thrombolysis | ||||||||
| Stent-retriever alone | 0.961 (0.465–1.984) | 0.914 | 0.922 (0.447–1.904) | 0.827 | 0.915 (0.446–1.877) | 0.808 | 0.938 (0.455–1.935) | 0.863 |
| Aspiration alone | 7.361 (1.978–27.386) | 0.003 | 7.700 (2.033–29.158) | 0.003 | 7.796 (2.068–29.390) | 0.002 | 8.128 (2.112–31.285) | 0.002 |
| Number of stent-retriever passes, per-1-passes increase | 1.169 (0.986–1.384) | 0.072 | 1.178 (0.996–1.393) | 0.056 | 1.179 (0.998–1.393) | 0.053 | 1.180 (0.999–1.393) | 0.052 |
| Imaging finding after EVT | ||||||||
| mTICI 2b-3 | 0.142 (0.059–0.340) | <0.001 | 0.138 (0.058–0.330) | <0.001 | 0.140 (0.059–0.334) | <0.001 | 0.131 (0.055–0.312) | <0.001 |
| Hemorrhagic transformation | 11.314 (4.836–26.468) | <0.001 | 12.450 (5.274–29.391) | <0.001 | 13.394 (5.681–31.589) | <0.001 | 13.304 (5.635–31.413) | <0.001 |
| Risk scoring score | ||||||||
| Per-1-point increase | 1.484 (1.290–1.950) | 0.005 | 1.177 (0.978–1.416) | 0.085 | 1.128 (1.041–1.223) | 0.004 | 1.173 (0.903–1.524) | 0.231 |
| AUC | Optimal Cutoff | Diagnostic Sensitivity | Diagnostic Specificity | PPV | NPV | |
|---|---|---|---|---|---|---|
| Unfavorable outcome: EVT patients | ||||||
| Pre-admission CHA2DS2VASc | 0.644 | 3.5 | 0.643 | 0.576 | 0.628 | 0.591 |
| Pre-admission CHADS2 | 0.654 | 2.5 | 0.502 | 0.775 | 0.713 | 0.583 |
| Pre-admission ATRIA | 0.663 | 7.5 | 0.662 | 0.628 | 0.665 | 0.625 |
| Pre-admission Essen | 0.596 | 3.5 | 0.573 | 0.592 | 0.61 | 0.554 |
| Unfavorable outcome: successful recanalization patients | ||||||
| Pre-admission CHA2DS2VASc | 0.613 | 3.5 | 0.603 | 0.564 | 0.535 | 0.63 |
| Pre-admission CHADS2 | 0.621 | 2.5 | 0.431 | 0.774 | 0.613 | 0.62 |
| Pre-admission ATRIA | 0.642 | 7.5 | 0.636 | 0.63 | 0.589 | 0.675 |
| Pre-admission Essen | 0.57 | 3.5 | 0.523 | 0.586 | 0.513 | 0.596 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Park, M.-S.; Yoo, J.; Kim, Y.D.; Park, H.; Kim, B.M.; Bang, O.Y.; Kim, H.C.; Han, E.; Kim, D.J.; et al. Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Functional Outcomes in Acute Ischemic Stroke Patients Who Received Endovascular Thrombectomy. J. Clin. Med. 2022, 11, 5599. https://doi.org/10.3390/jcm11195599
Kim HJ, Park M-S, Yoo J, Kim YD, Park H, Kim BM, Bang OY, Kim HC, Han E, Kim DJ, et al. Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Functional Outcomes in Acute Ischemic Stroke Patients Who Received Endovascular Thrombectomy. Journal of Clinical Medicine. 2022; 11(19):5599. https://doi.org/10.3390/jcm11195599
Chicago/Turabian StyleKim, Hyung Jun, Moo-Seok Park, Joonsang Yoo, Young Dae Kim, Hyungjong Park, Byung Moon Kim, Oh Young Bang, Hyeon Chang Kim, Euna Han, Dong Joon Kim, and et al. 2022. "Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Functional Outcomes in Acute Ischemic Stroke Patients Who Received Endovascular Thrombectomy" Journal of Clinical Medicine 11, no. 19: 5599. https://doi.org/10.3390/jcm11195599
APA StyleKim, H. J., Park, M.-S., Yoo, J., Kim, Y. D., Park, H., Kim, B. M., Bang, O. Y., Kim, H. C., Han, E., Kim, D. J., Heo, J., Choi, J. K., Lee, K.-Y., Lee, H. S., Shin, D. H., Choi, H.-Y., Sohn, S.-I., Hong, J.-H., Lee, J. Y., ... Song, T.-J., on behalf of the SECRET Study Investigators. (2022). Association between CHADS2, CHA2DS2-VASc, ATRIA, and Essen Stroke Risk Scores and Functional Outcomes in Acute Ischemic Stroke Patients Who Received Endovascular Thrombectomy. Journal of Clinical Medicine, 11(19), 5599. https://doi.org/10.3390/jcm11195599









