The Effect of Manual Therapy Plus Exercise in Patients with Lateral Ankle Sprains: A Critically Appraised Topic with a Meta-Analysis
Abstract
1. Introduction
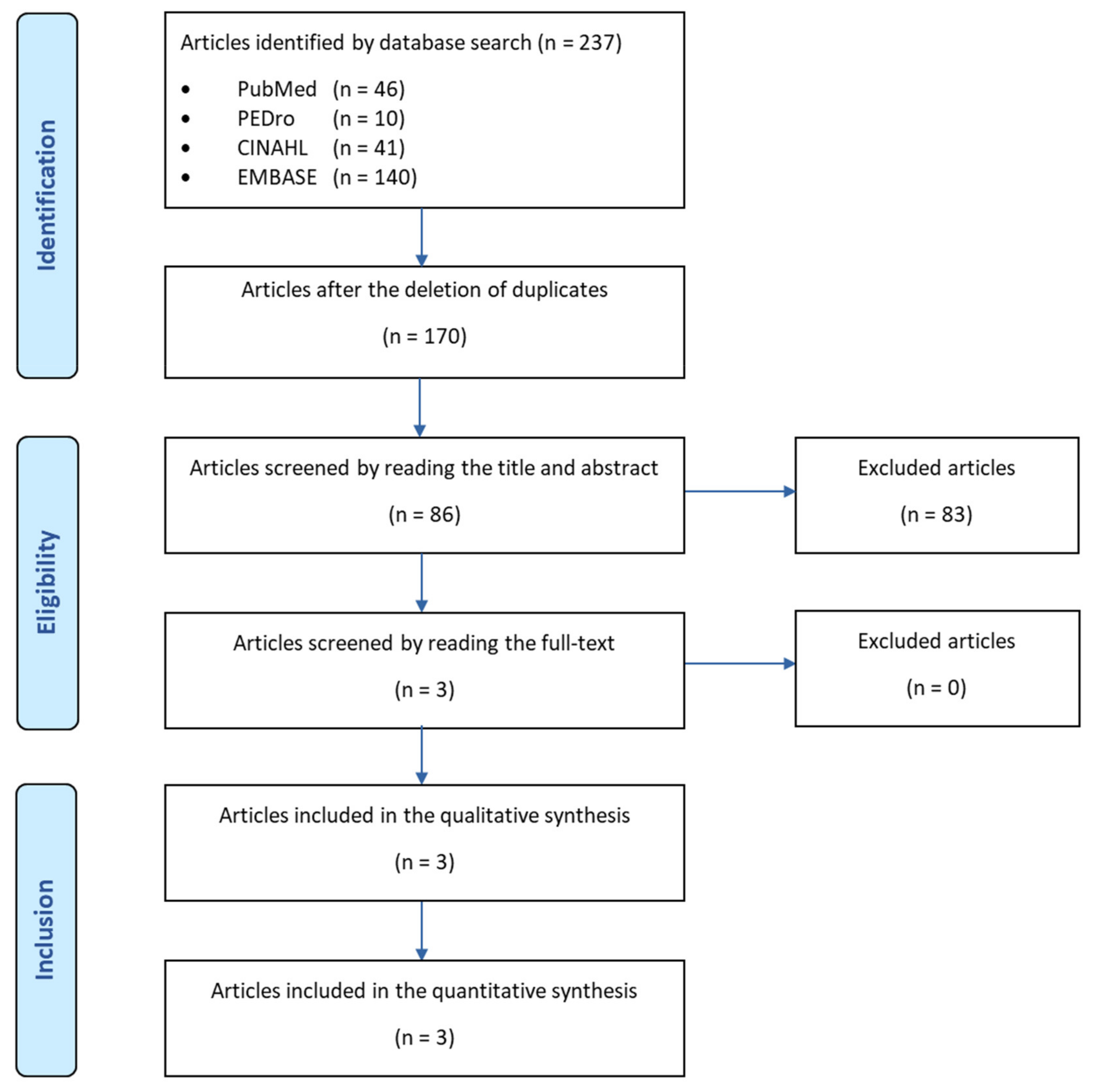
2. Materials and Methods
2.1. Focused Clinical Question
2.2. Search Strategy
- Population: patients with an LAS;
- Intervention: manual therapy plus therapeutic exercise;
- Comparison: therapeutic exercise;
- Outcome: clinical outcomes (i.e., pain, joint mobility and lower limb function);
- Type of study: randomized clinical trial (RCT).
2.3. Inclusion Criteria and Exclusion Criteria
- Patients with an LAS were enrolled;
- The effect of manual therapy plus therapeutic exercise, compared with therapeutic exercise alone, was investigated;
- The study design was as an RCT;
- The publication languages were English or Italian.
- Patients with ankle instability or chronic ankle instability (CAI) were enrolled;
- The effects of only manual therapy or only therapeutic exercise were investigated;
- The study design was a cohort, non-randomized clinical trial or not identified as an RCT.
2.4. Evidence of Quality Assessment
- A is assigned to consistent, high-quality patient-oriented evidence;
- B is assigned to evidence that is inconsistent or limited quality patient-oriented evidence;
- C is assigned to evidence that is considered an opinion, disease-oriented or a case series.
2.5. Data Synthesis
3. Results
3.1. Summary of Search and Key Findings
3.2. Results of Quality Assessment from the Best Available Evidence
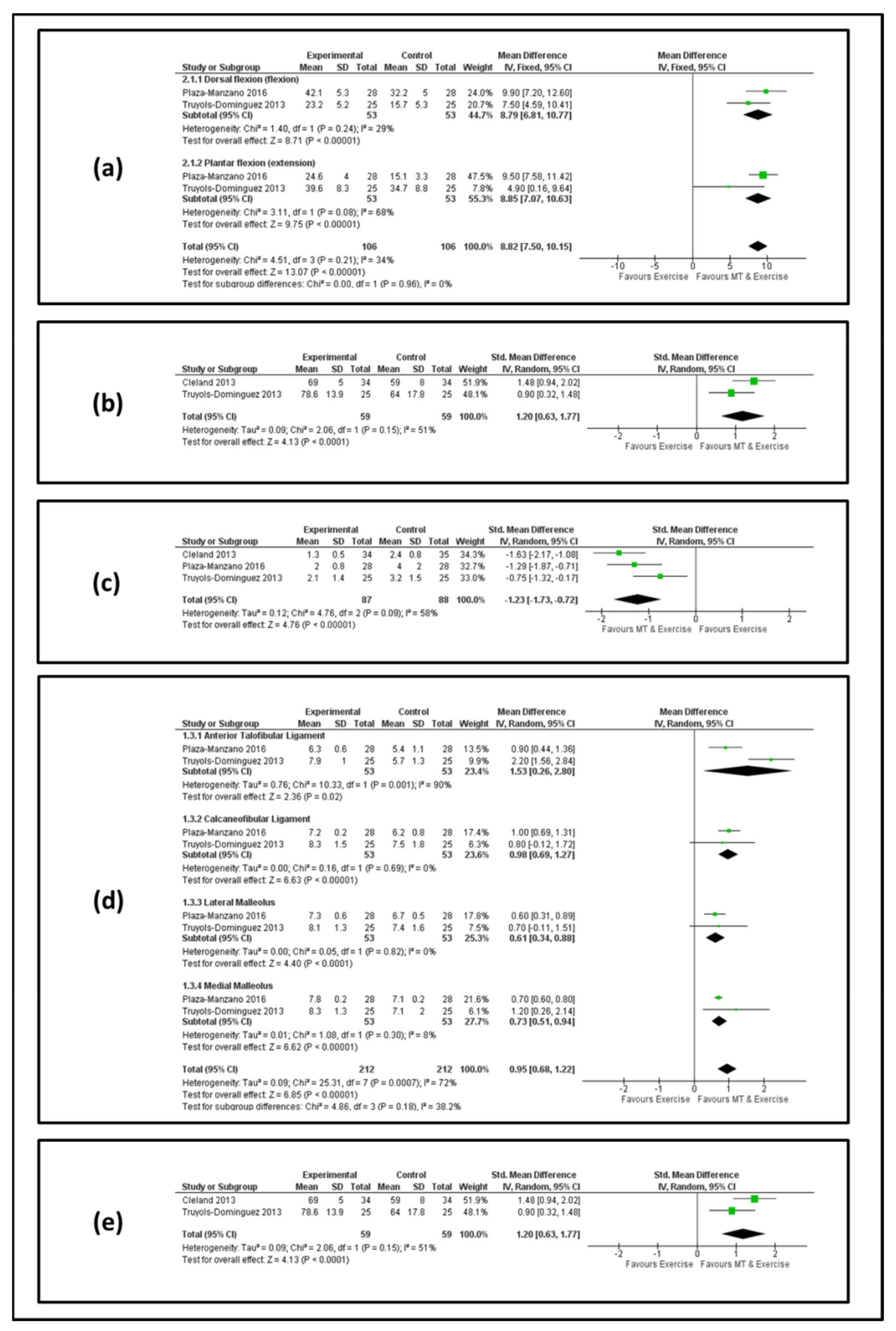
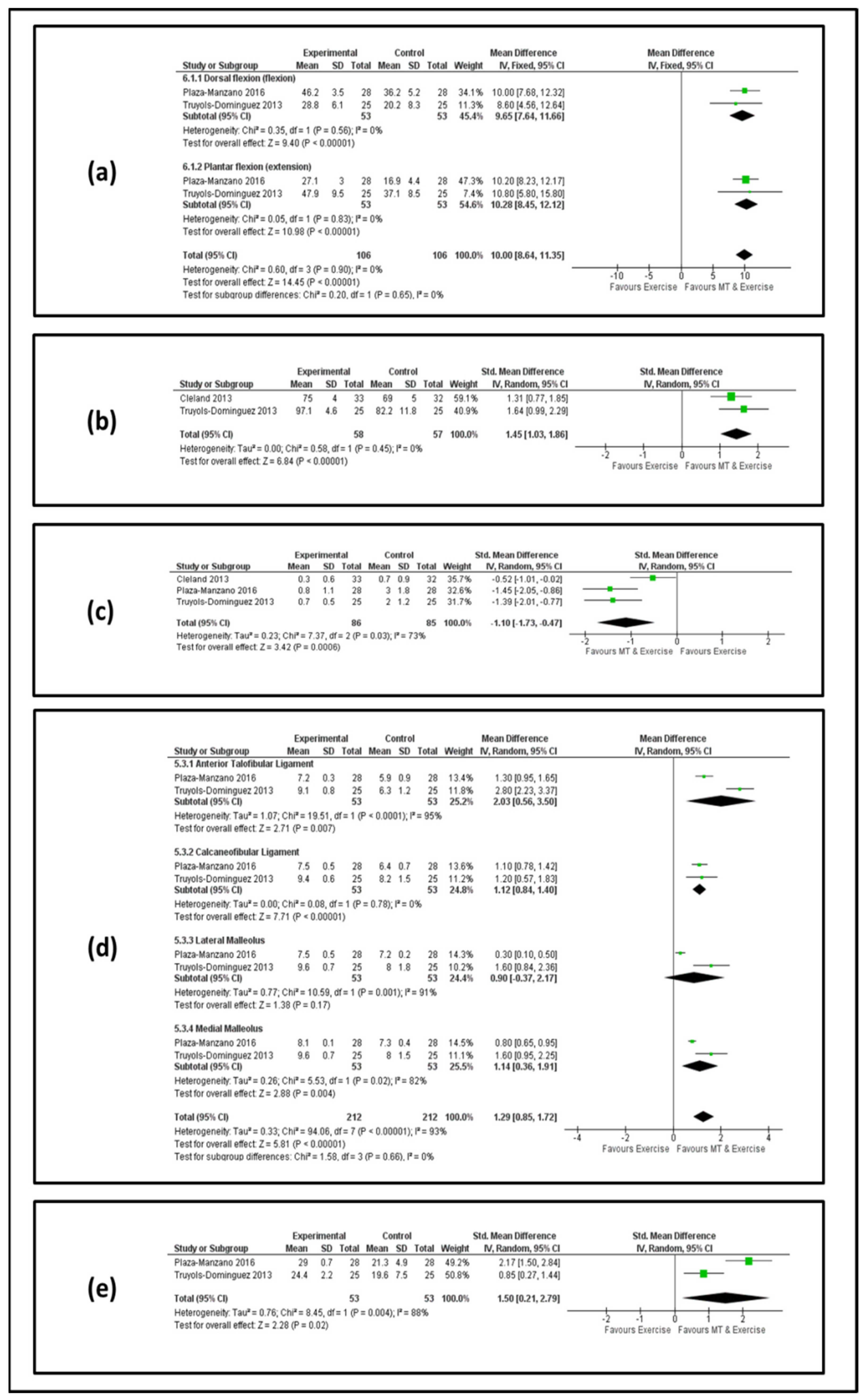
3.3. Results of the Meta-Analysis
3.4. Clinical Bottom Line
4. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hertel, J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar] [PubMed]
- Lynch, S.A.; Renstrom, P.A. Treatment of Acute Lateral Ankle Ligament Rupture in the Athlete. Sports Med. 1999, 27, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.; Hong, Y.; Chan, L.K.; Yung, P.S.; Chang, K.M. A Systematic Review on Ankle Injury and Ankle Sprain in Sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Delhaunt, E.; Coughlan, G.F.; Caulfield, B.; Nightingale, E.J.; Lin, C.W.C.; Hiller, C.E. Inclusion Criteria When Investigating Insufficiencies in Chronic Ankle Instability. Med. Sci. Sports Exerc. 2010, 42, 2106–2121. [Google Scholar] [CrossRef]
- Ferran, N.A.; Maffulli, N. Epidemiology of Sprains of the Lateral Ankle Ligament Complex. Foot Ankle Clin. 2006, 11, 659–662. [Google Scholar] [CrossRef]
- Terada, M.; Pietrosimone, B.; Gribble, P.A. Therapeutic Interventions for Increasing Ankle Dorsiflexion After Ankle Sprain: A Systematic Review. J. Athl. Train. 2013, 48, 696–709. [Google Scholar] [CrossRef]
- Terada, M.; Pietrosimone, B.; Gribble, P.A. Individuals with chronic ankle instability exhibit altered landing knee kinematics: Potential link with the mechanism of loading for the anterior cruciate ligament. Clin. Biomech. 2014, 29, 1125–1130. [Google Scholar] [CrossRef]
- Anandacoomarasamy, A.; Barnsley, L. Long term outcomes of inversion ankle injuries. Br. J. Sports Med. 2005, 39, 14. [Google Scholar] [CrossRef]
- Arnold, B.L.; de La Motte, S.; Linens, S.; Ross, E.S. Ankle Instability Is Associated with Balance Impairments: A Meta-Analysis. Med. Sci. Sports Exerc. 2009, 41, 1048–1062. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic Ankle Instability: Evolution of the Model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef]
- Konradsen, L. Factors Contributing to Chronic Ankle Instability: Kinesthesia and Joint Position Sense. J. Athl. Train. 2002, 37, 381–385. [Google Scholar] [PubMed]
- Romero-Morales, C.; López-López, S.; Bravo-Aguilar, M.; Cerezo-Téllez, E.; Benito-de Pedro, M.; López López, D.; Lobo, C.C. Ultrasonography Comparison of the Plantar Fascia and Tibialis Anterior in People with and Without Lateral Ankle Sprain: A Case-Control Study. J. Manip. Physiol. 2020, 43, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Lobo, C.C.; Morales, C.R.; Sanz, D.R.; Corbalán, I.S.; Marín, A.G.; López, D.L. Ultrasonography Comparison of Peroneus Muscle Cross-sectional Area in Subjects with or Without Lateral Ankle Sprains. J. Manipulative Physiol. Ther. 2016, 39, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, K.; Arab, A.M.; Abdollahi, I.; López-López, D.; Calvo-Lobo, C. Electromiography comparison of distal and proximal lower limb muscle activity patterns during external perturbation in subjects with and without functional ankle instability. Hum. Mov. Sci. 2017, 55, 211–220. [Google Scholar] [CrossRef]
- Van Rijn, R.M.; van Os, A.J.; Bernsen, R.M.; Luijsterburg, P.A.; Koes, B.W.; Bierma-Zeinstra, S.M.A. What Is the Clinical Course of Acute Ankle Sprains? A Systematic Literature Review. Am. J. Med. 2008, 121, 324–331. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. Consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Mueller, C.; Cain, M.S. Lack of Consensus on Return to Sport Criteria Following Lateral Ankle Sprain: A Systematic Review of Expert Opinions. J. Sport Rehabil. 2019, 29, 231–237. [Google Scholar] [CrossRef]
- Cooke, M.W.; Lamb, S.E.; Marsh, J.; Dale, J. A survey of current consultant practice of treatment of severe ankle sprains in emergency departments in the United Kingdom. Emerg. Med. J. 2003, 20, 505–507. [Google Scholar] [CrossRef]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef]
- Petersen, W.; Rembitzki, I.V.; Koppenburg, A.G.; Ellermann, A.; Liebau, C.; Bruggemann, G.P.; Best, R. Treatment of acute ankle ligament injuries: A systematic review. Arch. Orthop. Trauma Surg. 2013, 133, 1129–1141. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Glasgow, P.; MacAuley, D.C. Price needs updating, should we call the police? Br. J. Sports Med. 2012, 46, 220–221. [Google Scholar] [CrossRef] [PubMed]
- Dubois, B.; Esculier, J.F. Soft-tissue injuries simply need PEACE and LOVE. Br. J. Sports Med. 2020, 54, 72–73. [Google Scholar] [CrossRef] [PubMed]
- Feger, M.A.; Goetschius, J.; Love, H.; Saliba, S.A.; Hertel, J. Electrical stimulation as a treatment intervention to improve function, edema or pain following acute lateral ankle sprains: A systematic review. Phys. Ther. Sport 2015, 16, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Van den Bekerom, M.P.J.; van der Windt, D.A.W.M.; ter Riet, G.; van der Heijden, G.J.; Bouter, L.M. 2011 Therapeutic ultrasound for acute ankle sprains. Cochrane Database Syst. Rev. 2011, 6, CD001250. [Google Scholar]
- Jahjah, A.; Seidenspinner, D.; Shuttler, K.; Klasan, A.; Heyse, T.J.; Malcherczyk, D.; El-Zayat, B.F. The Effect of Ankle Tape on Joint Position Sense After Local Muscle Fatigue: A Randomized Controlled Trial. BMC Musculoskelet. Disord. 2018, 19, 8. [Google Scholar] [CrossRef]
- Slevin, Z.M.; Arnold, G.P.; Wang, W.; Abboud, R.J. Immediate effect of kinesiology tape on ankle stability. BMJ Open Sport Exerc. Med. 2020, 6, e000604. [Google Scholar] [CrossRef]
- De Vasconcelos, G.S.; Cini, A.; Sbruzzi, G.; Lima, C.S. Effects of proprioceptive training on the incidence of ankle sprain in athletes: Systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 1581–1590. [Google Scholar] [CrossRef]
- Burger, M.; Dreyer, D.; Fisher, R.L.; Foot, D.; O’Connor, D.H.; Galante, M.; Zalgaonkir, S. The Effectiveness of Proprioceptive and Neuromuscular Training Compared to Bracing in Reducing the Recurrence Rate of Ankle Sprains in Athletes: A Systematic Review and Meta-analysis. J. Back Musculoskelet. Rehabil. 2018, 31, 221–229. [Google Scholar] [CrossRef]
- Weerasekara, I.; Deam, H.; Bamborough, N.; Brown, S.; Donnelly, J.; Thorp, N.; Rivett, D.A. Effect of Mobilisation with Movement (MWM) on clinical outcomes in lateral ankle sprains: A systematic review and meta-analysis. Foot 2020, 43, 101657. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Taylor, J.B.; Dischiavi, S.L.; Doherty, C.; Delahunt, E. Rehabilitation Exercises Reduce Reinjury Post Ankle Sprain, But the Content and Parameters of an Optimal Exercise Program Have Yet to Be Established: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1367–1375. [Google Scholar] [CrossRef]
- Young, J.L.; Rhon, D.I.; de Zoete, R.M.J.; Cleland, J.A.; Snodgrass, S.J. The influence of dosing on effect size of exercise therapy for musculoskeletal foot and ankle disorders: A systematic review. Braz. J. Phys. Ther. 2018, 22, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Núñez-Cabaleiro, P.; Leirós-Rodríguez, R. Effectiveness of manual therapy in the treatment of cervicogenic headache: A systematic review. Headache 2022, 62, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Steuri, R.; Sattelmayer, M.; Elsig, S.; Kolly, C.; Tal, A.; Taeymans, J.; Hilfiker, R. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: A systematic review and meta-analysis of RCTs. Br. J. Sports Med. 2017, 51, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- De Luca, K.E.; Fang, S.H.; Ong, J.; Shin, K.S.; Woods, S.; Tuchin, P.J. The Effectiveness and Safety of Manual Therapy on Pain and Disability in Older Persons with Chronic Low Back Pain: A Systematic Review. J. Manip. Physiol. 2017, 40, 527–534. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Hubbard, T.J. Talar positional fault in persons with chronic ankle instability. Arch. Phys. Med. Rehabil. 2010, 91, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Vicenzino, B.; Branjerdporn, M.; Teys, P.; Jordan, K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J. Orthop. Sports Phys. Ther. 2006, 36, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.A.; Mintken, P.E.; McDevitt, A.; Bieniek, M.L.; Carpenter, K.J.; Kulp, K.; Whitman, J.M. Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: A multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2013, 43, 443–455. [Google Scholar] [CrossRef]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sports Phys. Ther. 2018, 48, 8–18. [Google Scholar] [CrossRef]
- Bove, G.M.; Delany, S.P.; Hobson, L.; Cruz, G.E.; Harris, M.Y.; Amin, M.; Chapelle, S.L.; Barbe, M.F. Manual therapy prevents onset of nociceptor activity, sensorimotor dysfunction, and neural fibrosis induced by a volitional repetitive task. Pain 2019, 160, 632–644. [Google Scholar] [CrossRef]
- Bleakley, C.M.; McDonough, S.M.; MacAuley, D.C. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: A systematic review. Aust. J. Physiother. 2008, 54, 7–20. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Feger, M.A.; Herb, C.C.; Fraser, J.J.; Glaviano, N.; Hertel, J. Supervised rehabilitation versus home exercise in the treatment of acute ankle sprains: A systematic review. Clin. Sports Med. 2015, 34, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Kerkhoffs, G.; Rowe, B.H.; Assendelft, W.; Kelly, K.D.; Struijs, P.A.A.; van Dijk, C.N. WITHDRAWN: Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst. Rev. 2013, 3, CD003762. [Google Scholar]
- Postle, K.; Pak, D.; Smith, T.O. Effectiveness of proprioceptive exercises for ankle ligament injury in adults: A systematic literature and meta-analysis. Man. Ther. 2012, 17, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Van Ochten, J.M.; Middlekoop, M.V.; Meuffels, D.; Bierma-Zeinstra, S.M. Chronic Complaints After Ankle Sprains: A Systematic Review on Effectiveness of Treatments. J. Orthop. Sports Phys. Ther. 2014, 44, 862–871. [Google Scholar] [CrossRef] [PubMed]
- Van Os, A.G.; Bierma-Zeinstra, S.M.; Verhagen, A.P.; de Bie, R.A.; Luijsterburg, P.A.J.; Koes, B.W. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: A systematic review of the literature. J. Orthop. Sports Phys. Ther. 2005, 35, 95–105. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Rijn, R.M.; van Ochten, J.; Luijsterburg, P.A.J.; van Middelkoop, M.; Koes, B.W.; Bierma-Zeinstra, S.M.A. Effectiveness of additional supervised exercises compared with conventional treatment alone in patients with acute lateral ankle sprains: Systematic review. BMJ 2010, 341, c5688. [Google Scholar] [CrossRef]
- Loudon, J.K.; Reiman, M.P.; Sylvain, J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: A systematic review. Br. J. Sports Med. 2014, 48, 365–370. [Google Scholar] [CrossRef]
- Weerasekara, I.; Osmotherly, P.; Snodgrass, S.; Marquez, J.; de Zoete, R.; Rivett, D.A. Clinical Benefits of Joint Mobilization on Ankle Sprains: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1395–1412. [Google Scholar] [CrossRef]
- Brantingham, J.W.; Bonnefin, D.; Perle, S.M.; Cassa, T.K.; Globe, G.; Pribicevic, M.; Hicks, M.; Korporaal, C. Manipulative therapy for lower extremity conditions: Update of a literature review. J. Manip. Physiol. Ther. 2012, 35, 127–166. [Google Scholar] [CrossRef]
- Sadigh, G.; Parker, R.; Kelly, A.M.; Cronin, P. How to write a critically appraised topic (CAT). Acad. Radiol. 2012, 19, 872–888. [Google Scholar] [CrossRef] [PubMed]
- Callander, J.; Anstey, A.V.; Ingram, J.R.; Limpens, J.; Flohr, C.; Spuls, P.I. How to write a Critically Appraised Topic: Evidence to underpin routine clinical practice. Br. J. Derm. 2017, 177, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Ebell, M.H.; Siwek, J.; Weiss, B.D.; Woolf, S.H.; Susman, J.; Ewigman, B.; Bowman, M. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. Am. Fam. Physician 2004, 69, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Manzano, G.; Vergara-Vila, M.; Val-Otero, S.; Rivera-Prieto, C.; Pecos-Martin, D.; Gallego-Izquierdo, T.; Ferragut-Garcias, A.; Romero-Franco, N. Manual therapy in joint and nerve structures combined with exercises in the treatment of recurrent ankle sprains: A randomized, controlled trial. Man. Ther. 2016, 26, 141–149. [Google Scholar] [CrossRef]
- Truyols-Dominiguez, S.; Salom-Moreno, J.; Abian-Vicen, J.; Cleland, J.A.; Fernandez-de-la-Penas, J. Efficacy of Thrust and Nonthrust Manipulation and Exercise with or Without the Addition of Myofascial Therapy for the Management of Acute Inversion Ankle Sprain: A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2013, 43, 300–309. [Google Scholar] [CrossRef]
- Schiftan, G.S.; Ross, L.A.; Hahne, A.J. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: A systematic review and meta-analysis. J. Sci. Med. Sport 2015, 18, 238–244. [Google Scholar] [CrossRef]
- Ben Moussa Zouita, A.; Majdoub, O.; Ferchichi, H.; Grandy, K.; Dziri, C.; Ben Salah, F.Z. The effect of 8-weeks proprioceptive exercise program in postural sway and isokinetic strength of ankle sprains of Tunisian athletes. Ann. Phys. Rehabil. Med. 2013, 56, 634–643. [Google Scholar] [CrossRef][Green Version]
- Nurse, M. Proprioceptive Training to Prevent Ankle Injuries in Basketball. Clin. J. Sport Med. 2011, 21, 277–278. [Google Scholar] [CrossRef][Green Version]
- Eisenhart, A.W.; Gaeta, T.J.; Yens, D.P. Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. J. Am. Osteopath. Assoc. 2003, 103, 417–421. [Google Scholar]
- Green, T.; Refshauge, K.; Crosbie, J.; Adams, R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys. Ther. 2001, 81, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.; Teys, P.; Vicenzino, B. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man. Ther. 2004, 9, 77–82. [Google Scholar] [CrossRef]
- Yeo, H.K.; Wright, A. Hypoalgesic effect of a passive accessory mobilisation technique in patients with lateral ankle pain. Man. Ther. 2011, 16, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Beazell, J.R.; Grindstaff, T.L.; Sauer, L.D.; Magrum, E.M.; Ingersoll, C.D.; Hertel, J. Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J. Orthop. Sports Phys. 2012, 42, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.E.; Kulig, K.; Fisher, B.E. Ankle manual therapy for individuals with post-acute ankle sprains: Description of a randomized, placebo-controlled clinical trial. BMC Complement. Altern. Med. 2010, 19, 59. [Google Scholar] [CrossRef]
- Rivera, M.J.; Winkelmann, Z.K.; Powden, C.J.; Games, K.E. Proprioceptive Training for the Prevention of Ankle Sprains: An Evidence-Based Review. J. Athl. Train. 2017, 52, 1065–1067. [Google Scholar] [CrossRef]
- Riva, D.; Bianchi, R.; Rocca, F.; Mamo, C. Proprioceptive Training and Injury Prevention in a Professional Men’s Basketball Team: A Six-Year Prospective Study. J. Strength Cond. Res. 2016, 30, 461–475. [Google Scholar] [CrossRef]
- Mosca, M.; Caravelli, S.; Massimi, S.; Fuiano, M.; Catanese, G.; Barone, G.; Bragonzoni, L.; Benedetti, M.G. Evaluation of proprioception and postural control at a minimum 1 year follow-up after ankle capsuloligamentous lateralplasty with Brostrom technique: A cohort study. Medicine 2020, 99, e19862. [Google Scholar] [CrossRef]
- Szczerbik, E.; Kalinowska, M.; Syczewska, M. Kinematic and Electromyography Responses to Increasing Proprioception Demand and a Lack of Visual Feedback in Healthy, Middle-Aged Women Tested on an Unstable Platform. Mot. Control 2022, 25, 1–19. [Google Scholar] [CrossRef]
- Moseley, A.M.; Sherrington, C.; Elkins, M.R.; Herbert, R.D.; Maher, C.G. Indexing of randomised controlled trials of physiotherapy interventions: A comparison of AMED, CENTRAL, CINAHL, EMBASE, hooked on evidence, PEDro, PsycINFO and PubMed. Physiotherapy 2009, 95, 151–156. [Google Scholar] [CrossRef]
- Martin, R.L.; Davenport, T.E.; Fraser, J.J.; Sawdon-Bea, J.; Carcia, C.R.; Carroll, L.A.; Kivlan, B.R.; Carreira, D. Ankle Stability and Movement Coordination Impairments: Lateral Ankle Ligament Sprains Revision. J Orthop. Sports Phys. 2021, 51, CPG1–CPG80. [Google Scholar] [CrossRef] [PubMed]
| Database | Search String |
|---|---|
| MEDLINE | (“Ankle Injuries”[Mesh] or (ankle injur*) OR (ankle sprain*) or (ankle strain*)) AND (“Exercise Therapy”[Mesh] OR “Exercise”[Mesh] or exercis*) AND (“Musculoskeletal Manipulations”[Mesh] or (musculoskeletal manipulation*) or (manual therap*) or (manipulative therap*)) |
| PEDro | ankle sprain* manual therap* exercis* |
| EMBASE | (‘ankle injuries’/exp OR (ankle AND injur*) OR ‘ankle sprain’/exp OR (ankle AND sprain*) OR (ankle strain*)) AND (‘exercise’/exp OR exercis*) AND (‘manual therapy’/exp OR (manual AND therap*)) |
| CINAHL | (ankle AND (sprain* OR injur*)) AND (exercis*) AND (manual therap*) |
| Plaza-Manzano et al. 2016 [55] | Truyols-Dominiguez et al. 2013 [56] | Cleland-Minkten et al. 2013 [37] | |
|---|---|---|---|
| Study design | Randomized controlled trial | Randomized controlled trial | Randomized controlled trial |
| Partecipants | N = 56 Age = 24 ± 2.5 Gender = 39 M–17 F Patients were randomly recruited from the University Hospital of Madrid | N = 50 Age = 33 ± 10 Gender = 37 M–13 F Patients were randomly recruited from a physical therapy clinic in Madrid | N = 74 Age = 35.1 ± 11 Gender = 38 M–36 F Patients were randomly recruited from 4 physical therapy clinics in the USA |
| Inclusion criteria |
|
| Patients with an inversion ankle sprain grade I or II, with an NPRS score greater than 3 and a negative result from the Ottawa ankle rules |
| Exclusion criteria |
|
|
|
| Intervention investigated | The experimental group performed 4 weeks of exercises combined with manual therapy (mobilization to influence joint and nerve structures). The control group performed 4 weeks of proprioceptive and strengthening exercises. The proprioceptive and strengthening exercise protocol consisted of four sessions of six exercises that were repeated twice a week and progressed every week, supervised by two physiotherapists with at least 6 years of experience in Sports Physiotherapy; The manual therapy protocol consisted of mobilization applied at grade III, including large amplitude passive movements repeated 10 times (the duration of techniques was 20–30 s with 2 min of resting) by two physiotherapists who were experts in manual therapy. | The experimental group received the thrust and non-thrust manipulation and exercise protocol in addition with myofascial manual therapy techniques for four sessions, once per week, for 4 weeks. The control group received the same thrust and non-thrust manipulation and exercise protocol for four sessions, once per week, for 4 weeks. Both groups received the same manual therapy protocol (performed for four sessions, once per week, for 4 weeks), which included ankle and foot mobilization (non thrust) applied at grade 3–4 and delivered for 20–30 s for thrust manipulation and exercise. Only the experimental group received myofascial therapy (pressure-release techniques, static strokes and cross-hand interventions) applied three times over the gastrocnemius and tibialis anterior muscles. | Patients in the MTEX group (manual therapy and exercise) were treated twice a week for 4 weeks, and each treatment session included thrust and non-thrust manipulation and mobilizing and strengthening exercises. Patients in the HEP group (home exercise program) attended physical therapy for four sessions for the instruction and progression of strengthening and proprioceptive exercises. The MTEX group was treated by two physical therapists twice weekly for 4 weeks, and each session lasted 30 min. Manual therapy techniques consisted of thrust and non-thrust manipulation performed for 5–30 s bouts at grades I, II, III and IV. Patients were also instructed to perform two self-mobilization techniques at home and strengthening exercises. For 4 weeks daily, the HEP group performed mobilizing exercises for the foot and ankle, gentle stretching exercises, resistive band exercises, one-leg standing activities, standing on a balance board and weight-bearing functional activities. |
| Outcome measure | Assessors measured the outcomes (VAS, CAIT, PPT, Active range of motion measured with goniometer, Strength in ankle flexion and extension with dynamic dynamometry) before and after the 4 weeks of treatment. | Assessors measured the outcomes (NPRS, Functional score for the assessment of acute lateral ankle sprains, Active range of motion measured with goniometer, PPT) at the baseline after the last treatment session and at 1 month follow-up. | Assessors measured the outcomes (FAAM, LEFS, NPRS, GRC scale) at the final physical therapy session (4 weeks) and after 6 months. |
| Results | The addition of manual therapy to the proprioceptive and strengthening exercise elicited lower pain levels, reduced self-reported ankle instability, greater ankle strength, lower PPT and greater AROM in patients with an LAS. The effect size was large to moderate in the following domains:
| The addition of myofascial techniques to a protocol of thrust/non-thrust manipulation and exercise resulted in statistically significant improvements in pain and function. The effect size between groups was large to moderate in all domains (pain, instability, weight bearing, swelling, walking pattern). | The addition of manual therapy to therapeutic exercise resulted in significant improvements in pain and function in both the short- and long-term follow-up. The effect size between groups was large to moderate (NPRS, FAAM, LEFS, GRC). |
| Level of evidence | 1b | 1b | 1b |
| Quality assessment score | ROB-2: Low risk of Bias | ROB-2: Low risk of Bias | ROB-2: Low risk of Bias |
| Contribution to CAT question | Conclusive contribution | Conclusive contribution | Conclusive contribution |
| Study | Bias Arising from the Randomization Process | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Outcome Data | Bias in the Measurement of the Outcome | Bias in the Selection of the Reported Result | Overall Bias |
|---|---|---|---|---|---|---|
| Plaza-Manzano et al., 2016 [55] | LOW | LOW | LOW | LOW | LOW | LOW |
| Truyols-Dominiguez et al., 2013 [56] | LOW | LOW | LOW | LOW | LOW | LOW |
| Cleland et al., 2013 [37] | LOW | LOW | LOW | LOW | LOW | LOW |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Ruvo, R.; Russo, G.; Lena, F.; Giovannico, G.; Neville, C.; Turolla, A.; Torre, M.; Pellicciari, L. The Effect of Manual Therapy Plus Exercise in Patients with Lateral Ankle Sprains: A Critically Appraised Topic with a Meta-Analysis. J. Clin. Med. 2022, 11, 4925. https://doi.org/10.3390/jcm11164925
de Ruvo R, Russo G, Lena F, Giovannico G, Neville C, Turolla A, Torre M, Pellicciari L. The Effect of Manual Therapy Plus Exercise in Patients with Lateral Ankle Sprains: A Critically Appraised Topic with a Meta-Analysis. Journal of Clinical Medicine. 2022; 11(16):4925. https://doi.org/10.3390/jcm11164925
Chicago/Turabian Stylede Ruvo, Rocco, Giuseppe Russo, Francesco Lena, Giuseppe Giovannico, Christoper Neville, Andrea Turolla, Monica Torre, and Leonardo Pellicciari. 2022. "The Effect of Manual Therapy Plus Exercise in Patients with Lateral Ankle Sprains: A Critically Appraised Topic with a Meta-Analysis" Journal of Clinical Medicine 11, no. 16: 4925. https://doi.org/10.3390/jcm11164925
APA Stylede Ruvo, R., Russo, G., Lena, F., Giovannico, G., Neville, C., Turolla, A., Torre, M., & Pellicciari, L. (2022). The Effect of Manual Therapy Plus Exercise in Patients with Lateral Ankle Sprains: A Critically Appraised Topic with a Meta-Analysis. Journal of Clinical Medicine, 11(16), 4925. https://doi.org/10.3390/jcm11164925









