CBCT Analysis of Dento-Skeletal Changes after Rapid versus Slow Maxillary Expansion on Deciduous Teeth: A Randomized Clinical Trial
Abstract
1. Introduction
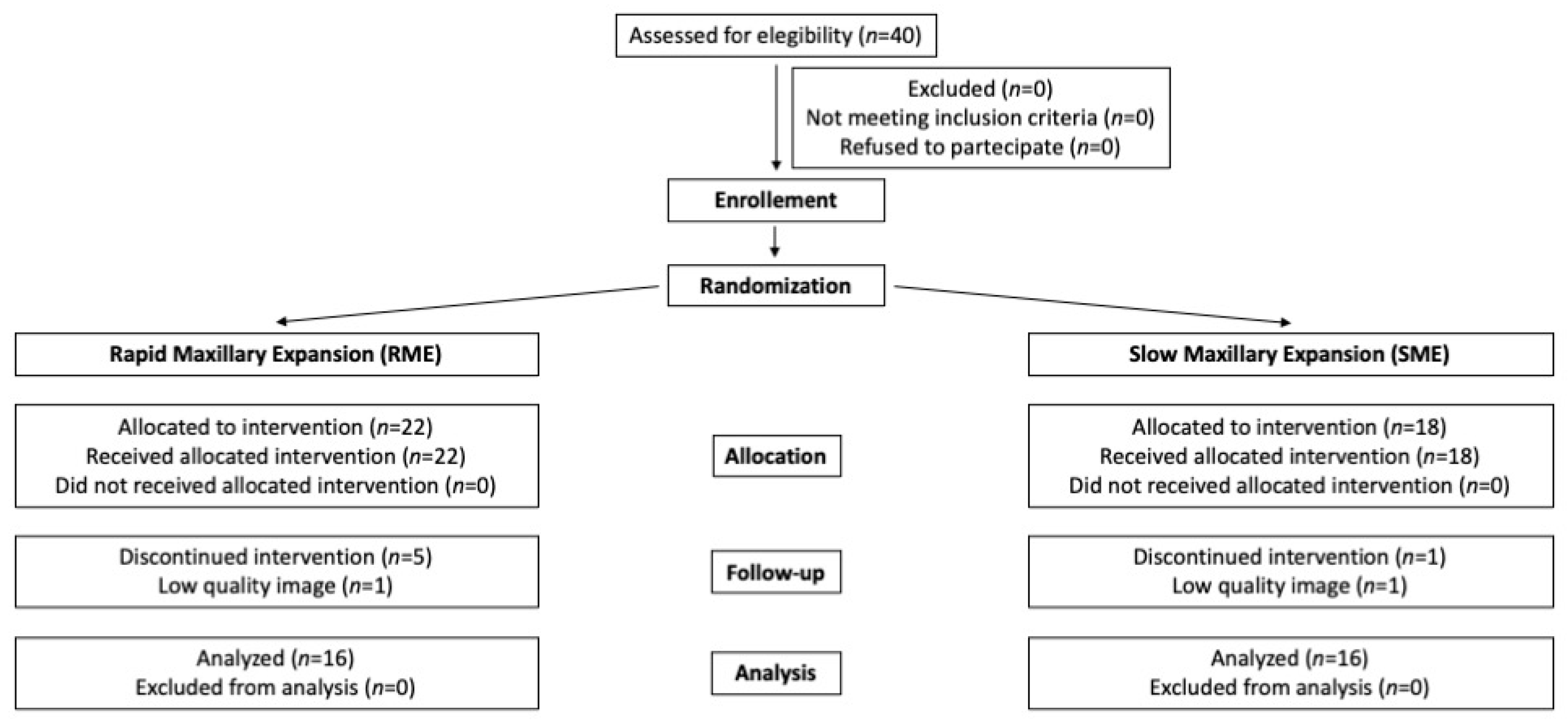
2. Materials and Methods
2.1. Population and Study Design
2.2. Sample Size Calculation
2.3. Randomization Procedure
2.4. Intervention and Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- RME and SME are equally capable of producing both skeletal and dentoalveolar transverse expansion; deciduous teeth anchorage provides clinically significant transverse expansion causing less damage to permanent teeth;
- RME produced more anterior expansion than SME, therefore it could be better suited for patients with respiratory dysfunctions and anterior dental crowding;
- Molar inclination control is more superior for SME than RME, making SME recommended in patients with severe buccal inclination of upper permanent molars without the need for a preparatory appliance to molar decompensation;
- SME provides a more controlled dental movement because of its constant release of forces, also eliminating the need for home activation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caprioglio, A.; Castiglioni, F.; Sambataro, S.; Giuntini, V.; Comaglio, I.; Lorvetti, F.; Fastuca, R. Changes in canine inclination after rapid and slow maxillary expansion compared to untreated controls. Orthod. Craniofac. Res. 2020, 23, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Serafin, M.; Esposito, L.; Conti, V.; Fastuca, R.; Lagravère, M.; Caprioglio, A. CBCT Comparison of Dentoskeletal Effects of Haas-Type and Hyrax-Type Expanders Using Deciduous Teeth as Anchorage: A Randomized Clinical Trial. Appl. Sci. 2021, 11, 7110. [Google Scholar] [CrossRef]
- Caprioglio, A.; Bergamini, C.; Franchi, L.; Vercellini, N.; Zecca, P.A.; Nucera, R.; Fastuca, R. Prediction of Class II improvement after rapid maxillary expansion in early mixed dentition. Prog. Orthod. 2017, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr.; Baccetti, T.; Franchi, L.; Herberger, T.A. Rapid maxillary expansion followed by fixed appliances: A long-term evaluation of changes in arch dimensions. Angle Orthod. 2003, 73, 344–353. [Google Scholar] [PubMed]
- Caprioglio, A.; Fastuca, R.; Zecca, P.A.; Beretta, M.; Mangano, C.; Piattelli, A.; Macchi, A.; Iezzi, G. Cellular Midpalatal Suture Changes after Rapid Maxillary Expansion in Growing Subjects: A Case Report. Int. J. Mol. Sci. 2017, 18, 615. [Google Scholar] [CrossRef]
- Ghoneima, A.; Abdel-Fattah, E.; Hartsfield, J.; El-Bedwehi, A.; Kamel, A.; Kula, K. Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 510–519. [Google Scholar] [CrossRef]
- Digregorio, M.V.; Fastuca, R.; Zecca, P.A.; Caprioglio, A.; Lagravere, M.O. Buccal bone plate thickness after rapid maxillary expansion in mixed and permanent dentitions. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 198–206. [Google Scholar] [CrossRef]
- Pawlaczyk-Kamieńska, T.; Kulczyk, T.; Pawlaczyk-Wróblewska, E.; Borysewicz-Lewicka, M.; Niedziela, M. Limited Mandibular Movements as a Consequence of Unilateral or Asymmetrical Temporomandibular Joint Involvement in Juvenile Idiopathic Arthritis Patients. J. Clin. Med. 2020, 9, 2576. [Google Scholar] [CrossRef]
- Mutinelli, S.; Manfredi, M.; Guiducci, A.; Denotti, G.; Cozzani, M. Anchorage onto deciduous teeth: Effectiveness of early rapid maxillary expansion in increasing dental arch dimension and improving anterior crowding. Prog. Orthod. 2015, 16, 22. [Google Scholar] [CrossRef]
- Rosa, M.; Lucchi, P.; Manti, G.; Caprioglio, A. Rapid Palatal Expansion in the absence of posterior cross-bite to intercept maxillary incisor crowding in the mixed dentition: A CBCT evaluation of spontaneous changes of untouched permanent molars. Eur. J. Paediatr. Dent. 2016, 17, 286–294. [Google Scholar]
- Fastuca, R.; Michelotti, A.; Nucera, R.; D’Antò, V.; Militi, A.; Logiudice, A.; Caprioglio, A.; Portelli, M. Midpalatal Suture Density Evaluation after Rapid and Slow Maxillary Expansion with a Low-Dose CT Protocol: A Retrospective Study. Medicina (Kaunas) 2020, 56, 112. [Google Scholar] [CrossRef] [PubMed]
- Paoloni, V.; Giuntini, V.; Lione, R.; Nieri, M.; Barone, V.; Merlo, M.M.; Mazza, F.; Passaleva, S.; Cozza, P.; Franchi, L. Comparison of the dento-skeletal effects produced by Leaf expander versus rapid maxillary expander in prepubertal patients: A two-center randomized controlled trial. Eur. J. Orthod. 2021, 44, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Tremont, T.J.; Posnick, J.C. Selected Orthodontic Principles for Management of Cranio-Maxillofacial Deformities. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 321–338. [Google Scholar] [CrossRef]
- Primozic, J.; Federici Canova, F.; Rizzo, F.A.; Marzo, G.; Quinzi, V. Diagnostic ability of the primary second molar crown-to-root length ratio and the corresponding underlying premolar position in estimating future expander anchoring teeth exfoliation. Orthod. Craniofac. Res. 2021, 24, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Lagravere, M.O.; Major, P.W.; Carey, J. Sensitivity analysis for plane orientation in three-dimensional cephalometric analysis based on superimposition of serial cone beam computed tomography images. Dentomaxillofac. Radiol. 2010, 39, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.D.S.; Jacob, H.B.; Locks, A.; Brunetto, M.; Ribeiro, G.L.U. Evaluation of the rapid and slow maxillary expansion using cone-beam computed tomography: A randomized clinical trial. Dent. Press J. Orthod. 2017, 22, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Brunetto, M.; Andriani Jda, S.; Ribeiro, G.L.; Locks, A.; Correa, M.; Correa, L.R. Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: A clinical trial study. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 633–644. [Google Scholar] [CrossRef]
- Luiz Ulema Ribeiro, G.; Jacob, H.B.; Brunetto, M.; da Silva Pereira, J.; Motohiro Tanaka, O.; Buschang, P.H. A preliminary 3-D comparison of rapid and slow maxillary expansion in children: A randomized clinical trial. Int. J. Paediatr. Dent. 2020, 30, 349–359. [Google Scholar] [CrossRef]
- Bucci, R.; D’Anto, V.; Rongo, R.; Valletta, R.; Martina, R.; Michelotti, A. Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and meta-analyses. J. Oral Rehabil. 2016, 43, 543–564. [Google Scholar] [CrossRef]
- Lanteri, V.; Cossellu, G.; Gianolio, A.; Beretta, M.; Lanteri, C.; Cherchi, C.; Farronato, G. Comparison between RME, SME and Leaf Expander in growing patients: A retrospective postero-anterior cephalometric study. Eur. J. Paediatr. Dent. 2018, 19, 199–204. [Google Scholar]
- Lo Giudice, A.; Fastuca, R.; Portelli, M.; Militi, A.; Bellocchio, M.; Spinuzza, P.; Briguglio, F.; Caprioglio, A.; Nucera, R. Effects of rapid vs. slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur. J. Paediatr. Dent. 2017, 18, 299–304. [Google Scholar] [PubMed]
- Lanteri, V.; Gianolio, A.; Gualandi, G.; Beretta, M. Maxillary tridimensional changes after slow expansion with leaf expander in a sample of growing patients: A pilot study. Eur. J. Paediatr. Dent. 2018, 19, 29–34. [Google Scholar] [PubMed]
- Pinheiro, F.H.; Garib, D.G.; Janson, G.; Bombonatti, R.; de Freitas, M.R. Longitudinal stability of rapid and slow maxillary expansion. Dent. Press J. Orthod. 2014, 19, 70–77. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Srivastava, S.C.; Mahida, K.; Agarwal, C.; Chavda, R.M.; Patel, H.A. Longitudinal Stability of Rapid and Slow Maxillary Expansion: A Systematic Review. J. Contemp. Dent. Pract. 2020, 21, 1068–1072. [Google Scholar] [CrossRef]
- Rutili, V.; Mrakic, G.; Nieri, M.; Franceschi, D.; Pierleoni, F.; Giuntini, V.; Franchi, L. Dento-skeletal effects produced by rapid versus slow maxillary expansion using fixed jackscrew expanders: A systematic review and meta-analysis. Eur. J. Orthod. 2021, 43, 301–312. [Google Scholar] [CrossRef]
- Bastos, R.; Blagitz, M.N.; Aragón, M.; Maia, L.C.; Normando, D. Periodontal side effects of rapid and slow maxillary expansion: A systematic review. Angle Orthod. 2019, 89, 651–660. [Google Scholar] [CrossRef]
- Lowe, R.; Makowka, S.; Manzella, K.; Warunek, S.; Al-Jewair, T. Mechanical properties of the NiTi Memoria Leaf Spring Activated Expander (NiTi MLSAE) for maxillary transverse discrepancy correction: An in-vitro study. J. Clin. Exp. Dent. 2020, 12, e154–e160. [Google Scholar] [CrossRef]
- Huynh, T.; Kennedy, D.B.; Joondeph, D.R.; Bollen, A.M. Treatment response and stability of slow maxillary expansion using Haas, hyrax, and quad-helix appliances: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 331–339. [Google Scholar] [CrossRef]
- Ugolini, A.; Cerruto, C.; Di Vece, L.; Ghislanzoni, L.H.; Sforza, C.; Doldo, T.; Silvestrini-Biavati, A.; Caprioglio, A. Dental arch response to Haas-type rapid maxillary expansion anchored to deciduous vs. permanent molars: A multicentric randomized controlled trial. Angle Orthod. 2015, 85, 570–576. [Google Scholar] [CrossRef]
- Wertz, R.A. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am. J. Orthod. 1970, 58, 41–66. [Google Scholar] [CrossRef]
- Alves, A.C.M.; Maranhão, O.B.V.; Janson, G.; Garib, D.G. Mandibular dental arch short and long-term spontaneous dentoalveolar changes after slow or rapid maxillary expansion: A systematic review. Dent. Press J. Orthod. 2017, 22, 55–63. [Google Scholar] [CrossRef] [PubMed]
| Skeletal Landmarks | ||
| Foramen spinosum (RFs, LFs) | 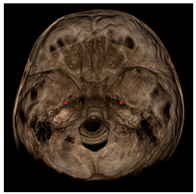 | Geometric center of the upper and smallest circumference with defined borders viewed axially on the foramen spinosum. |
| ELSA | 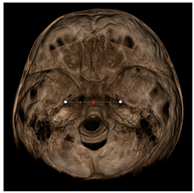 | Midpoint on a line connecting left and right foramen spinosum. |
| Foramen ovale (RFo, LFo) | 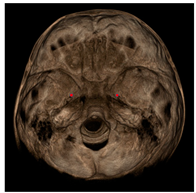 | Most posterior, upper and lateral point on the posterior cortical bone with defined borders viewed axially on the foramen ovale. |
| Medial foramen magnum (MFM) |  | Most anterior point of the foramen magnum. |
| Lateral pterygoid plate (RLpt, LLpt) | 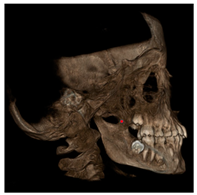 | Most posterior border of the pterygoid lateral plate at the vertical level of the palatal shelves by using an axial slice showing as much of the palate surface as possible. |
| Dental Landmarks | ||
| Pulp chamber (PC) |  | Center of the pulp chamber floor in upper first permanent molars (in all 3 planes of space). Center of pulp chamber floor in upper second deciduous molars (in all 3 planes of space). Tip of upper central incisor pulp chamber viewed sagittally. |
| Pulp horn (PH) | 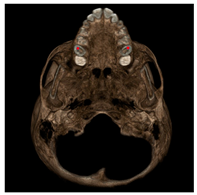 | Tip of the mesio-buccal pulp horn of upper first permanent molars. |
| Furcation (FURCA) | 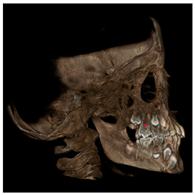 | Furcation of upper first permanent molars. |
| Nasal Landmarks | ||
| Nasal floor (RNF, LNF) |  | Junction of palatal cortical alveolar bone and cortical bone surrounding nasal cavity located in the coronal scan passing through PC16 point |
| Nasal wall (RNW, LNW) |  | Most external point of the cortex bone separating the maxillary sinus and the nasal cavity located in the coronal scan passing through PC16 point |
| Measurement | Variable |
|---|---|
| PC16_PC26 (mm) | Permanent Molars Expansion |
| PC55_PC65 (mm) | Deciduous Molars Expansion |
| PC11_PC21 (mm) | Central Incisors Expansion |
| LLPt_RLPt (mm) | Lateral Pterygoid Expansion |
| RNW_LNW (mm) | Nasal Wall Expansion |
| RNF_LNF (mm) | Nasal Floor Expansion |
| FURCA16_PC16_PC26 (°) | Right Upper Molar Tip |
| FURCA26_PC26_PC16 (°) | Left Upper Molar Tip |
| Measurement | RME Group | SME Group | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |
| PC16_PC26 (mm) | 40.9 | 3.7 | 41.1 | 2.5 | 0.621 |
| PC55_PC65 (mm) | 37.7 | 3.1 | 38.7 | 2.5 | 0.254 |
| PC11_PC21 (mm) | 7.9 | 0.6 | 9.0 | 3.5 | 0.518 |
| LLPt_RLPt (mm) | 50.5 | 4.2 | 49.5 | 28 | 0.649 |
| RNW_LNW (mm) | 28.9 | 2.3 | 28.1 | 2.0 | 0.197 |
| RNF_LNF (mm) | 17.3 | 5.2 | 16.7 | 3.1 | 0.447 |
| FURCA16_PC16_PC26 (°) | 116.9 | 25.6 | 135.8 | 9.4 | 0.019 * |
| FURCA26_PC26_PC16 (°) | 112.7 | 31.1 | 136.2 | 9.6 | 0.043 * |
| Measurement | T1 | T2 | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |
| PC16_PC26 (mm) | 40.9 | 3.7 | 44.8 | 3.4 | 0.001 * |
| PC55_PC65 (mm) | 37.7 | 3.1 | 41.9 | 8.4 | 0.023 * |
| PC11_PC21 (mm) | 7.9 | 0.6 | 8.7 | 1.0 | 0.001 * |
| LLPt_RLPt (mm) | 50.5 | 4.3 | 51.8 | 4.0 | 0.006 * |
| RNW_LNW (mm) | 29.0 | 2.3 | 31.2 | 2.4 | 0.001 * |
| RNF_LNF (mm) | 17.3 | 5.5 | 19.0 | 6.0 | 0.157 |
| FURCA16_PC16_PC26 (°) | 116.9 | 25.6 | 116.3 | 32.4 | 0.647 |
| FURCA26_PC26_PC16 (°) | 112.7 | 31.2 | 113.5 | 40.6 | 0.913 |
| Measurement | T1 | T2 | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |
| PC16_PC26 (mm) | 41.1 | 2.5 | 43.3 | 2.9 | 0.003 * |
| PC55_PC65 (mm) | 38.7 | 2.5 | 43.2 | 2.6 | 0.002 * |
| PC11_PC21 (mm) | 9.0 | 3.5 | 9.0 | 2.5 | 0.777 |
| LLPt_RLPt (mm) | 49.6 | 2.8 | 50.9 | 3.2 | 0.004 * |
| RNW_LNW (mm) | 28.1 | 2.0 | 28.7 | 2.4 | 0.041 * |
| RNF_LNF (mm) | 16.7 | 3.1 | 17.6 | 3.2 | 0.272 |
| FURCA16_PC16_PC26 (°) | 135.8 | 9.4 | 132.9 | 11.4 | 0.397 |
| FURCA26_PC26_PC16 (°) | 136.2 | 9.7 | 137.4 | 10.5 | 0.683 |
| Measurement | RME T2-T1 | SME T2-T1 | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |
| PC16_PC26 (mm) | 3.9 | 1.9 | 2.2 | 1.7 | 0.025 * |
| PC55_PC65 (mm) | 6.3 | 2.7 | 4.5 | 2.4 | 0.790 |
| PC11_PC21 (mm) | 0.8 | 0.7 | 0.0 | 1.4 | 0.058 |
| LLPt_RLPt (mm) | 1.3 | 1.8 | 1.3 | 1.3 | 0.849 |
| RNW_LNW (mm) | 2.2 | 1.6 | 0.6 | 1.7 | 0.004 * |
| RNF_LNF (mm) | 1.7 | 4.8 | 0.9 | 2.3 | 0.184 |
| FURCA16_PC16_PC26 (°) | −0.6 | 18.7 | −2.9 | 11.9 | 0.323 |
| FURCA26_PC26_PC16 (°) | 0.8 | 25.8 | 1.3 | 8.4 | 0.879 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serafin, M.; Fastuca, R.; Caprioglio, A. CBCT Analysis of Dento-Skeletal Changes after Rapid versus Slow Maxillary Expansion on Deciduous Teeth: A Randomized Clinical Trial. J. Clin. Med. 2022, 11, 4887. https://doi.org/10.3390/jcm11164887
Serafin M, Fastuca R, Caprioglio A. CBCT Analysis of Dento-Skeletal Changes after Rapid versus Slow Maxillary Expansion on Deciduous Teeth: A Randomized Clinical Trial. Journal of Clinical Medicine. 2022; 11(16):4887. https://doi.org/10.3390/jcm11164887
Chicago/Turabian StyleSerafin, Marco, Rosamaria Fastuca, and Alberto Caprioglio. 2022. "CBCT Analysis of Dento-Skeletal Changes after Rapid versus Slow Maxillary Expansion on Deciduous Teeth: A Randomized Clinical Trial" Journal of Clinical Medicine 11, no. 16: 4887. https://doi.org/10.3390/jcm11164887
APA StyleSerafin, M., Fastuca, R., & Caprioglio, A. (2022). CBCT Analysis of Dento-Skeletal Changes after Rapid versus Slow Maxillary Expansion on Deciduous Teeth: A Randomized Clinical Trial. Journal of Clinical Medicine, 11(16), 4887. https://doi.org/10.3390/jcm11164887







