The Prediction Accuracy of Digital Orthodontic Setups for the Orthodontic Phase before Orthognathic Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Image Acquisition
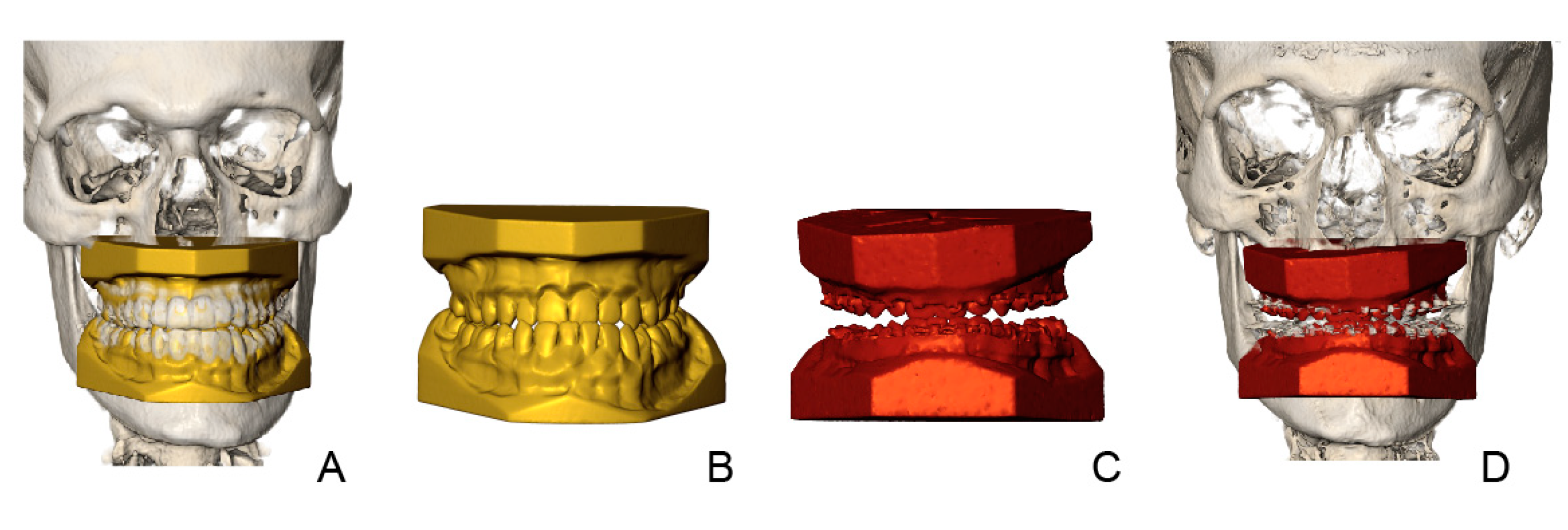
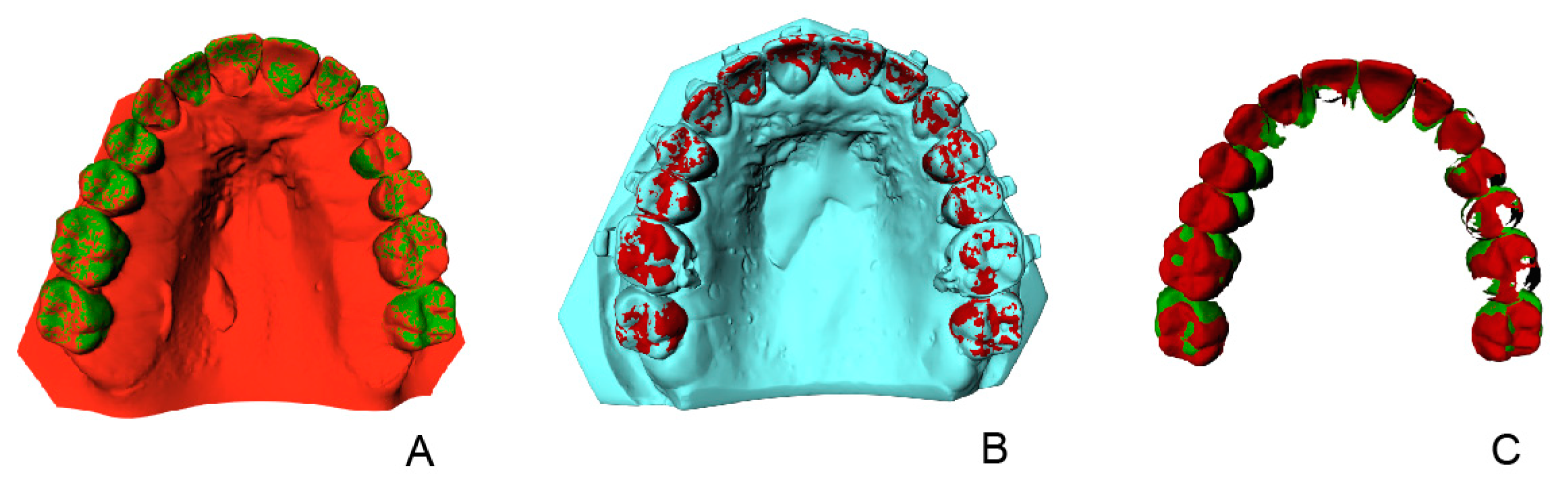
2.3. Creating the Orthodontic Virtual Setup
2.4. Treatment Evaluation
2.5. Statistical Analysis
3. Results
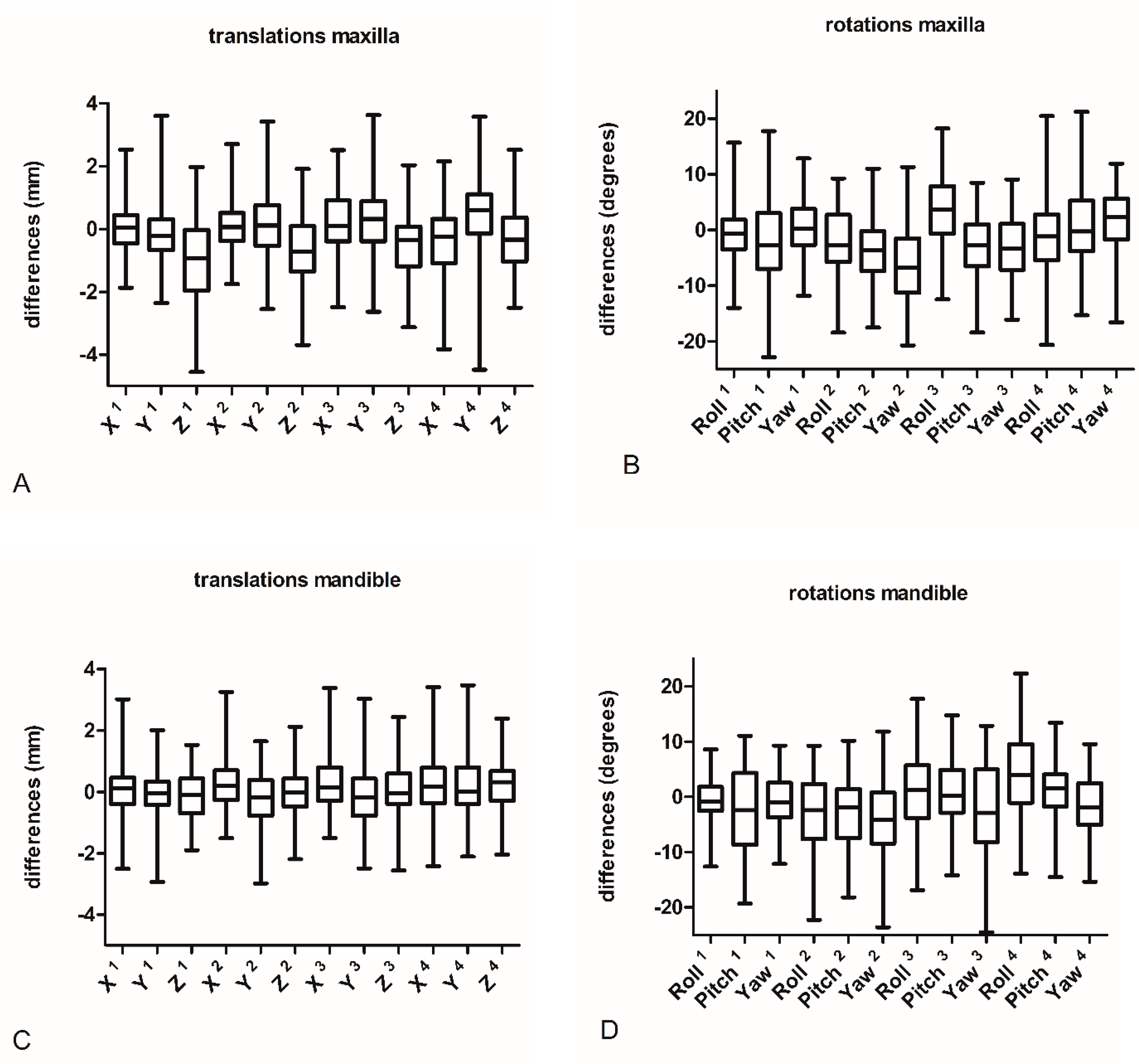
3.1. Setup Accuracy
3.2. Effect of SARME and Extractions on the Results
4. Discussion
4.1. Interpretation of Study Results
4.2. Limitations of the Study Design
4.3. Clinical Relevance
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kesling, H.D. The diagnostic setup with consideration of the third dimension. Am. J. Orthod. Dentofac. Orthop. 1956, 42, 740–748. [Google Scholar] [CrossRef]
- Camardella, L.T.; Vilella, O.V.; Breuning, K.H.; de Assis Ribeiro Carvalho, F.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. The influence of the model superimposition method on the assessment of accuracy and predictability of setup models. J. Orofac. Orthop. 2021, 82, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Hajeer, M.Y.; Millett, D.T.; Ayoub, A.F.; Siebert, J.P. Applications of 3D imaging in orthodontics: Part II. J. Orthod. 2004, 31, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Hou, D.; Capote, R.; Bayirli, B.; Chan, D.C.N.; Huang, G. The effect of digital diagnostic setups on orthodontic treatment planning. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 542–549. [Google Scholar] [CrossRef]
- Camardella, L.T.; Rothier, E.K.; Vilella, O.V.; Ongkosuwito, E.M.; Breuning, K.H. Virtual setup: Application in orthodontic practice. J. Orofac. Orthop. 2016, 77, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Kara-Boulad, J.M.; Burhan, A.S.; Hajeer, M.Y.; Khattab, T.Z.; Nawaya, F.R.; Al-Sabbagh, R. Treatment of Moderately Crowded Teeth Using Lingual Fixed Appliance Prepared by a Modified HIRO(R) Technique: A Case Report and Method Description. Cureus 2022, 14, e25077. [Google Scholar] [CrossRef] [PubMed]
- Baan, F.; de Waard, O.; Bruggink, R.; Xi, T.; Ongkosuwito, E.M.; Maal, T.J.J. Virtual setup in orthodontics: Planning and evaluation. Clin. Oral Investig. 2020, 24, 2385–2393. [Google Scholar] [CrossRef] [PubMed]
- Larson, B.E. Orthodontic preparation for orthognathic surgery. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 441–458. [Google Scholar] [CrossRef]
- Brouns, V.; de Waal, A.M.L.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. Oral health-related quality of life before, during, and after orthodontic-orthognathic treatment: A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 2223–2235. [Google Scholar] [CrossRef]
- Pauls, A.; Nienkemper, M.; Schwestka-Polly, R.; Wiechmann, D. Therapeutic accuracy of the completely customized lingual appliance WIN: A retrospective cohort study. J. Orofac. Orthop. 2017, 78, 52–61. [Google Scholar] [CrossRef]
- Grauer, D.; Proffit, W.R. Accuracy in tooth positioning with a fully customized lingual orthodontic appliance. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 433–443. [Google Scholar] [CrossRef]
- Lombardo, L.; Arreghini, A.; Ramina, F.; Huanca Ghislanzoni, L.T.; Siciliani, G. Predictability of orthodontic movement with orthodontic aligners: A retrospective study. Prog. Orthod. 2017, 18, 35. [Google Scholar] [CrossRef] [PubMed]
- Tepedino, M.; Paoloni, V.; Cozza, P.; Chimenti, C. Movement of anterior teeth using clear aligners: A three-dimensional, retrospective evaluation. Prog. Orthod. 2018, 19, 9. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A. The Cervical Vertebral Maturation (CVM) Method for the Assessment of Optimal Treatment Timing in Dentofacial Orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar] [CrossRef]
- Pandis, N. Sample calculations for comparison of 2 means. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 519–521. [Google Scholar] [CrossRef] [PubMed]
- Baan, F.; Bruggink, R.; Nijsink, J.; Maal, T.J.J.; Ongkosuwito, E.M. Fusion of intra-oral scans in cone-beam computed tomography scans. Clin. Oral Investig. 2021, 25, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Nada, R.M.; Maal, T.J.; Breuning, K.H.; Berge, S.J.; Mostafa, Y.A.; Kuijpers-Jagtman, A.M. Accuracy and reproducibility of voxel based superimposition of cone beam computed tomography models on the anterior cranial base and the zygomatic arches. PLoS ONE 2011, 6, e16520. [Google Scholar] [CrossRef] [PubMed]
- de Waard, O.; Bruggink, R.; Baan, F.; Reukers, H.A.J.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. Operator Performance of the Digital Setup Fabrication for Orthodontic-Orthognathic Treatment: An Explorative Study. J. Clin. Med. 2021, 11, 145. [Google Scholar] [CrossRef]
- Larson, B.E.; Vaubel, C.J.; Grunheid, T. Effectiveness of computer-assisted orthodontic treatment technology to achieve predicted outcomes. Angle Orthod. 2013, 83, 557–562. [Google Scholar] [CrossRef]
- Awad, M.G.; Ellouze, S.; Ashley, S.; Vaid, N.; Makki, L.; Ferguson, D.J. Accuracy of digital predictions with CAD/CAM labial and lingual appliances: A retrospective cohort study. Semin. Orthod. 2018, 24, 393–406. [Google Scholar] [CrossRef]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofac. Res. 2020, 23, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.; Julien, K.; Kesterke, M.; Buschang, P.H. Differences in finished case quality between Invisalign and traditional fixed appliances. Angle Orthod. 2022, 92, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Cassina, C.; Vandevska-Radunovic, V.; Eliades, T. Incisor and profile alterations in extraction cases treated with standard Edgewise and pre-adjusted appliances: A controlled before-and-after study. J. World Fed. Orthod. 2021, 10, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Xi, T.; Laskowska, M.; van de Voort, N.; Ghaeminia, H.; Pawlak, W.; Berge, S.; Maal, T. The effects of surgically assisted rapid maxillary expansion (SARME) on the dental show and chin projection. J. Craniomaxillofac. Surg. 2017, 45, 1835–1841. [Google Scholar] [CrossRef]
- Fabels, L.N.; Nijkamp, P.G. Interexaminer and intraexaminer reliabilities of 3-dimensional orthodontic digital setups. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 806–811. [Google Scholar] [CrossRef]

| Tooth Type | Parameter | N | Mean | 95% CI | p | |
|---|---|---|---|---|---|---|
| Upper | Lower | |||||
| MAXILLA | ||||||
| incisors | Roll | 100 | −0.64 | −1.85 | 0.58 | 0.303 |
| Pitch | 100 | −1.98 | −5.06 | 1.11 | 0.208 | |
| Yaw | 100 | 0.34 | −0.67 | 1.38 | 0.500 | |
| X | 100 | 0.04 | −0.10 | 0.19 | 0.567 | |
| Y | 100 | −0.02 | −0.46 | 0.41 | 0.914 | |
| Z | 100 | −1.01 | −1.58 | −0.44 | 0.001 | |
| canines | Roll | 52 | −2.51 | −4.65 | −0.37 | 0.021 |
| Pitch | 52 | −4.18 | −6.10 | −2.26 | 0.000 | |
| Yaw | 52 | −5.69 | −8.16 | −3.22 | 0.000 | |
| X | 52 | 0.08 | −0.18 | 0.33 | 0.552 | |
| Y | 52 | 0.25 | −0.11 | 0.61 | 0.173 | |
| Z | 52 | −0.70 | −1.16 | −0.25 | 0.002 | |
| premolars | Roll | 84 | 3.42 | 1.51 | 5.30 | 0.000 |
| Pitch | 84 | −2.96 | −4.54 | −1.40 | 0.000 | |
| Yaw | 84 | −3.08 | −4.73 | −1.46 | 0.000 | |
| X | 84 | 0.20 | −0.15 | 0.54 | 0.271 | |
| Y | 84 | 0.38 | 0.01 | 0.74 | 0.043 | |
| Z | 84 | −0.47 | −0.83 | −0.10 | 0.011 | |
| molars | Roll | 99 | −0.76 | −3.16 | 1.65 | 0.537 |
| Pitch | 99 | 0.88 | −1.17 | 2.91 | 0.403 | |
| Yaw | 99 | 1.96 | 0.48 | 3.45 | 0.009 | |
| X | 99 | −0.38 | −0.76 | −0.01 | 0.048 | |
| Y | 99 | 0.54 | 0.21 | 0.86 | 0.001 | |
| Z | 99 | −0.31 | −0.64 | 0.02 | 0.062 | |
| MANDIBLE | ||||||
| incisors | Roll | 104 | −0.66 | −1.64 | 0.33 | 0.190 |
| Pitch | 104 | −2.82 | −5.59 | −0.05 | 0.046 | |
| Yaw | 104 | −0.71 | −1.67 | 0.25 | 0.148 | |
| X | 104 | 0.06 | −0.10 | 0.23 | 0.432 | |
| Y | 104 | −0.04 | −0.35 | 0.26 | 0.778 | |
| Z | 104 | −0.11 | −0.41 | 0.18 | 0.454 | |
| canines | Roll | 52 | −2.77 | −4.92 | −0.62 | 0.011 |
| Pitch | 52 | −2.48 | −4.50 | −0.45 | 0.016 | |
| Yaw | 52 | −3.94 | −5.92 | −1.96 | 0.000 | |
| X | 52 | 0.26 | 0.02 | 0.50 | 0.035 | |
| Y | 52 | −0.16 | −0.48 | 0.16 | 0.326 | |
| Z | 52 | 0.03 | −0.25 | 0.31 | 0.819 | |
| premolars | Roll | 73 | 1.34 | −1.26 | 3.87 | 0.318 |
| Pitch | 73 | 0.72 | −1.05 | 2.48 | 0.426 | |
| Yaw | 73 | −2.29 | −4.15 | −0.47 | 0.014 | |
| X | 73 | 0.27 | 0.03 | 0.49 | 0.024 | |
| Y | 73 | −0.08 | −0.43 | 0.27 | 0.661 | |
| Z | 73 | 0.04 | −0.28 | 0.36 | 0.819 | |
| molars | Roll | 93 | 4.73 | 1.53 | 7.90 | 0.004 |
| Pitch | 93 | 1.15 | −0.07 | 2.38 | 0.063 | |
| Yaw | 93 | −1.83 | −3.48 | −0.20 | 0.028 | |
| X | 93 | 0.21 | −0.07 | 0.49 | 0.146 | |
| Y | 93 | 0.15 | −0.18 | 0.49 | 0.366 | |
| Z | 93 | 0.29 | 0.02 | 0.56 | 0.036 | |
| Tooth Type | Parameter | Estimate | 95% CI | p | Estimate | 95% CI | p | ||
|---|---|---|---|---|---|---|---|---|---|
| Upper | Lower | Upper | Lower | ||||||
| MAXILLA | MANDIBLE | ||||||||
| incisors | Roll | 1.13 | −1.66 | 3.92 | 0.428 | −1.15 | −3.92 | 1.63 | 0.418 |
| Pitch | −8.58 | −11.10 | −6.06 | <0.001 | −7.27 | −9.78 | −4.77 | <0.001 | |
| Yaw | −0.70 | −2.69 | 1.29 | 0.491 | −0.51 | −2.49 | 1.46 | 0.611 | |
| X | 0.18 | −0.25 | 0.61 | 0.403 | 0.11 | −0.32 | 0.54 | 0.610 | |
| Y | 0.41 | −0.08 | 0.91 | 0.103 | 0.17 | −0.33 | 0.66 | 0.509 | |
| Z | 0.22 | −0.28 | 0.71 | 0.386 | −0.33 | −0.83 | 0.16 | 0.186 | |
| canines | Roll | −0.24 | −3.58 | 3.09 | 0.886 | −2.52 | −5.85 | 0.82 | 0.139 |
| Pitch | −3.87 | −6.85 | −0.89 | 0.011 | −2.57 | −5.54 | 0.41 | 0.091 | |
| Yaw | 1.47 | −1.07 | 4.00 | 0.256 | 1.65 | −0.88 | 4.19 | 0.201 | |
| X | 0.26 | −0.23 | 0.75 | 0.303 | 0.18 | −0.40 | 0.67 | 0.459 | |
| Y | 0.57 | 0.02 | 1.12 | 0.042 | 0.32 | −0.23 | 0.87 | 0.248 | |
| Z | 0.09 | −0.46 | 0.64 | 0.747 | −0.46 | −1.01 | 0.09 | 0.102 | |
| premolars | Roll | 0.07 | −2.88 | 3.025 | 0.961 | −2.20 | −5.19 | 0.79 | 0.149 |
| Pitch | −3.56 | −6.21 | −0.90 | 0.008 | −2.25 | −4.94 | 0.43 | 0.100 | |
| Yaw | 0.79 | −1.36 | 2.94 | 0.471 | 0.98 | −1.21 | 2.49 | 0.382 | |
| X | 0.04 | −0.40 | 0.49 | 0.845 | −0.03 | −0.48 | 0.42 | 0.905 | |
| Y | 0.61 | 0.10 | 1.12 | 0.019 | 0.36 | −0.15 | 0.88 | 0.166 | |
| Z | −0.11 | −0.62 | 0.40 | 0.678 | −0.66 | −1.18 | −0.14 | 0.112 | |
| molars | Roll | 2.46 | −0.35 | 5.26 | 0.086 | 0.18 | −2.65 | 3.01 | 0.900 |
| Pitch | −2.93 | −5.46 | −0.40 | 0.023 | −1.62 | −4.17 | 0.93 | 0.213 | |
| Yaw | 0.49 | −1.51 | 2.49 | 0.632 | 0.68 | −1.35 | 2.70 | 0.514 | |
| X | −0.10 | −0.53 | 0.33 | 0.661 | −0.17 | −0.60 | 0.27 | 0.446 | |
| Y | 0.53 | 0.03 | 1.03 | 0.036 | 0.29 | −0.21 | 0.79 | 0.261 | |
| Z | 0.54 | 0.05 | 1.04 | 0.032 | −0.01 | −0.51 | 0.49 | 0.974 | |
| Tooth Type | Parameter | Estimate | 95% CI | p | Estimate | 95% CI | p | ||
|---|---|---|---|---|---|---|---|---|---|
| Upper | Lower | Upper | Lower | ||||||
| MAXILLA | MANDIBLE | ||||||||
| incisors | Roll | 1.15 | −1.62 | 3.91 | 0.417 | 0.38 | −2.36 | 3.12 | 0.785 |
| Pitch | −5.80 | −8.76 | −2.83 | <0.001 | −5.13 | −8.09 | −2.19 | <0.001 | |
| Yaw | −0.29 | −2.44 | 1.87 | 0.794 | −1.10 | −3.23 | 1.04 | 0.313 | |
| X | −0.07 | −0.51 | 0.37 | 0.754 | 0.16 | −0.29 | 0.60 | 0.489 | |
| Y | −0.23 | −0.81 | 0.34 | 0.421 | 0.01 | −0.56 | 0.58 | 0.981 | |
| Z | −0.41 | −0.91 | 0.09 | 0.110 | −0.42 | −0.92 | 0.08 | 0.102 | |
| canines | Roll | −1.16 | −4.55 | 2.23 | 0.503 | −1.92 | −5.32 | 1.47 | 0.266 |
| Pitch | −4.52 | −7.95 | −1.08 | 0.010 | −3.86 | −7.29 | −0.42 | 0.028 | |
| Yaw | 0.59 | −2.14 | 3.34 | 0.670 | −0.21 | −2.96 | 2.52 | −0.877 | |
| X | −0.21 | −0.72 | 0.29 | 0.408 | 0.01 | −0.50 | 0.52 | 0.963 | |
| Y | −0.13 | −0.75 | 0.50 | 0.691 | 0.12 | −0.51 | 0.74 | 0.717 | |
| Z | −0.47 | −1.05 | 0.10 | 0.102 | −0.48 | −1.05 | 0.09 | 0.099 | |
| premolars | Roll | −2.95 | −5.85 | −0.05 | 0.046 | −3.71 | −6.74 | −0.69 | 0.016 |
| Pitch | −2.37 | −5.44 | 0.69 | 0.128 | −1.71 | −4.87 | 1.44 | 0.287 | |
| Yaw | 1.23 | −1.04 | 3.51 | 0.288 | 0.42 | −1.97 | 2.82 | 0.729 | |
| X | −0.52 | −0.98 | −0.06 | 0.026 | −0.29 | −0.76 | 0.18 | 0.223 | |
| Y | −0.05 | −0.63 | 0.53 | 0.870 | 0.19 | −0.40 | 0.79 | 0.522 | |
| Z | −0.69 | −1.21 | −0.18 | 0.009 | −0.70 | −1.12 | −0.17 | 0.010 | |
| molars | Roll | −3.17 | −5.97 | −0.38 | 0.026 | −3.94 | −6.76 | −1.12 | 0.006 |
| Pitch | −2.65 | −5.64 | 0.33 | 0.082 | −1.99 | −4.99 | 1.01 | 0.194 | |
| Yaw | −0.97 | −3.16 | 1.21 | 0.381 | −1.78 | −4.00 | −0.42 | 0.113 | |
| X | −0.68 | −1.13 | −0.23 | 0.003 | −0.46 | −0.91 | −0.01 | 0.047 | |
| Y | 0.27 | −0.30 | 0.85 | 0.350 | 0.51 | −0.06 | 1.09 | 0.079 | |
| Z | −0.39 | −0.90 | 0.12 | 0.132 | −0.40 | −0.91 | 0.11 | 0.127 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Waard, O.; Baan, F.; Bruggink, R.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. The Prediction Accuracy of Digital Orthodontic Setups for the Orthodontic Phase before Orthognathic Surgery. J. Clin. Med. 2022, 11, 6141. https://doi.org/10.3390/jcm11206141
de Waard O, Baan F, Bruggink R, Bronkhorst EM, Kuijpers-Jagtman AM, Ongkosuwito EM. The Prediction Accuracy of Digital Orthodontic Setups for the Orthodontic Phase before Orthognathic Surgery. Journal of Clinical Medicine. 2022; 11(20):6141. https://doi.org/10.3390/jcm11206141
Chicago/Turabian Stylede Waard, Olivier, Frank Baan, Robin Bruggink, Ewald M. Bronkhorst, Anne Marie Kuijpers-Jagtman, and Edwin M. Ongkosuwito. 2022. "The Prediction Accuracy of Digital Orthodontic Setups for the Orthodontic Phase before Orthognathic Surgery" Journal of Clinical Medicine 11, no. 20: 6141. https://doi.org/10.3390/jcm11206141
APA Stylede Waard, O., Baan, F., Bruggink, R., Bronkhorst, E. M., Kuijpers-Jagtman, A. M., & Ongkosuwito, E. M. (2022). The Prediction Accuracy of Digital Orthodontic Setups for the Orthodontic Phase before Orthognathic Surgery. Journal of Clinical Medicine, 11(20), 6141. https://doi.org/10.3390/jcm11206141








