Direct Anterior versus Lateral Approach for Femoral Neck Fracture: Role in COVID-19 Disease
Abstract
:1. Introduction
2. Materials and Methods
- femoral neck fractures type 31.B according to the A.O. classification [27] and simultaneous COVID-19 infection at the time of the surgical procedure;
- age > 70 years;
- patients eligible for surgery.
- Exclusion criteria were:
- Parkinson’s disease;
- Hemoglobin < 8 g/dL;
- Patient underwent general anesthesia;
- ASA score 5.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graham Carlos, W.; dela Cruz, C.S.; Cao, B.; Pasnick, S.; Jamil, S. Novel Wuhan (2019-nCoV) Coronavirus. Am. J. Respir. Crit. Care Med. 2020, 201, P7–P8. [Google Scholar] [CrossRef]
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Ireland, N. ICNARC Report on COVID-19 in Criical Care. 2020. Available online: https://www.icnarc.org/our-audit/audits/cmp/reports (accessed on 3 January 2021).
- Archer, J.E.; Odeh, A.; Ereidge, S.; Salem, H.K.; Jones, G.P.; Gardner, A.; Tripathi, S.S.; Gregg, A.; Jeganathan, R.; Siddique, M.H.; et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet 2020, 396, 27–38. [Google Scholar] [CrossRef]
- Maccagnano, G.; Notarnicola, A.; Pesce, V.; Mudoni, S.; Tafuri, S.; Moretti, B. The Prevalence of Fragility Fractures in a Population of a Region of Southern Italy Affected by Thyroid Disorders. BioMed Res. Int. 2016, 2016, 6017165. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Maccagnano, G.; Moretti, L.; Tafuri, S.; Moretti, B. Cardiopathy and osteoporosis: The epidemiology in a region of Italy. J. Biol. Regul. Homeost. Agents 2017, 31, 251–255. [Google Scholar] [PubMed]
- Kayani, B.; Onochie, E.; Patil, V.; Begum, F.; Cuthbert, R.; Ferguson, D.; Bhamra, J.; Sharma, A.; Bates, P.; Haddad, F.S. Infographic: The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt. J. 2020, 102-B, 1279–1280. [Google Scholar] [CrossRef]
- Ciatti, C.; Maniscalco, P.; Quattrini, F.; Gattoni, S.; Magro, A.; Capelli, P.; Banchini, F.; Fiazza, C.; Pavone, V.; Pagliarello, C.P.; et al. The epidemiology of proximal femur fractures during COVID-19 emergency in italy: A multicentric study. Acta. Biomed. 2021, 92, e2021398. [Google Scholar] [CrossRef]
- Collaborative, C.; Collaborative, G. SARS-CoV-2 infection and venous thromboembolism after surgery: An international prospective cohort study. Anaesthesia 2022, 77, 3–6. [Google Scholar] [CrossRef]
- Harvin, J.A.; Harvin, W.H.; Camp, E.; Caga-Anan, Z.; Burgess, A.R.; Wade, C.E.; Holcomb, J.B.; Cotton, B.A. Early femur fracture fixation is associated with a reduction in pulmonary complications and hospital charges: A decade of experience with 1376 diaphyseal femur fractures. J. Trauma Acute Care Surg. 2012, 73, 1442–1448. [Google Scholar] [CrossRef]
- Simunovic, N.; Devereaux, P.J.; Sprague, S.; Guyatt, G.H.; Schemitsch, E.; DeBeer, J.; Bhandari, M. Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. Can. Med Assoc. J. 2010, 182, 1609–1616. [Google Scholar] [CrossRef]
- Guyen, O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop. Traumatol. Surg. Res. 2018, 105, S95–S101. [Google Scholar] [CrossRef]
- Pesce, V.; Maccagnano, G.; Vicenti, G.; Notarnicola, A.; Moretti, L.; Tafuri, S.; Vanni, D.; Salini, V.; Moretti, B. The effect of hydroxyapatite coated screw in the lateral fragility fractures of the femur. A prospective randomized clinical study. J. Biol. Regul. Homeost. Agents 2014, 28, 125–132. [Google Scholar]
- Petis, S.; Howard, J.L.; Lanting, B.L.; Vasarhelyi, E.M. Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes. Can. J. Surg. 2015, 58, 128–139. [Google Scholar] [CrossRef]
- Ramadanov, N.; Bueschges, S.; Lazaru, P.; Dimitrov, D. A meta-analysis on RCTs of direct anterior and conventional approaches in total hip arthroplasty. Sci. Rep. 2021, 11, 20991. [Google Scholar] [CrossRef]
- Putananon, C.; Tuchinda, H.; Arirachakaran, A.; Wongsak, S.; Narinsorasak, T.; Kongtharvonskul, J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: Network meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2017, 28, 255–267. [Google Scholar] [CrossRef]
- Zhong, H.; Poeran, J.; Liu, J.; Wilson, L.A.; Memtsoudis, S.G. Hip fracture characteristics and outcomes during COVID-19: A large retrospective national database review. Br. J. Anaesth. 2021, 127, 15–22. [Google Scholar] [CrossRef]
- Moppett, I.K.; Parker, M.; Griffiths, R.; Bowers, T.; White, S.M.; Moran, C.G. Nottingham Hip Fracture Score: Longitudinal and multi-centre assessment. Br. J. Anaesth. 2012, 109, 546–550. [Google Scholar] [CrossRef]
- Yue, C.; Kang, P.; Pei, F. Comparison of Direct Anterior and Lateral Approaches in Total Hip Arthroplasty: A systematic review and meta-analysis (PRISMA). Medicine 2015, 94, e2126. [Google Scholar] [CrossRef]
- Meermans, G.; Konan, S.; Das, R.; Volpin, A.; Haddad, F.S. The direct anterior approach in total hip arthroplasty: A systematic review of the literature. Bone Jt. J. 2017, 99-B, 732–740. [Google Scholar] [CrossRef]
- Huang, X.T.; Liu, D.G.; Jia, B.; Xu, Y.X.; Post-Graduate, X.-T.H.; Post-Graduate, D.-G.L.; Post-Graduate, B.J. Comparisons between Direct Anterior Approach and Lateral Approach for Primary Total Hip Arthroplasty in Postoperative Orthopaedic Complications: A Systematic Review and Meta-Analysis. Orthop. Surg. 2021, 13, 1707–1720. [Google Scholar] [CrossRef] [PubMed]
- Ryan, S.P.; Politzer, C.; Green, C.; Wellman, S.; Bolognesi, M.; Seyler, T. Albumin Versus American Society of Anesthesiologists Score: Which Is More Predictive of Complications Following Total Joint Arthroplasty? Orthopedics 2018, 41, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, A.; Consonni, D.; Carugno, M.; Bozzi, G.; Mangioni, D.; Muscatello, A.; Castelli, V.; Palomba, E.; Cantù, A.; Ceriotti, F.; et al. Characteristics of 1573 healthcare workers who underwent nasopharyngeal swab testing for SARS-CoV-2 in Milan, Lombardy, Italy. Clin. Microbiol. Infect. 2020, 26, 1413.e9–1413.e13. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Cai, Q.; Qu, Z.; Gao, Z. COVID-19 Screening in Chest X-Ray Images Using Lung Region Priors. IEEE J. Biomed. Health Informatics 2021, 25, 4119–4127. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef]
- Knutsson, S.B.; Wennergren, D.; Bojan, A.; Ekelund, J.; Möller, M. Femoral fracture classification in the Swedish Fracture Register—A validity study. BMC Musculoskelet. Disord. 2019, 20, 197. [Google Scholar] [CrossRef]
- Moretti, V.M.; Post, Z.D. Surgical Approaches for Total Hip Arthroplasty. Indian J. Orthop. 2017, 51, 368–376. [Google Scholar] [CrossRef]
- Auffarth, A.; Resch, H.; Lederer, S.; Karpik, S.; Hitzl, W.; Bogner, R.; Mayer, M.; Matis, N. Does the Choice of Approach for Hip Hemiarthroplasty in Geriatric Patients Significantly Influence Early Postoperative Outcomes? A Randomized-Controlled Trial Comparing the Modified Smith-Petersen and Hardinge Approaches. J. Trauma: Inj. Infect. Crit. Care 2011, 70, 1257–1262. [Google Scholar] [CrossRef]
- Trevisan, C.; Compagnoni, R.; Klumpp, R. Comparison of clinical results and patient’s satisfaction between direct anterior approach and Hardinge approach in primary total hip arthroplasty in a community hospital. Musculoskelet. Surg. 2017, 101, 261–267. [Google Scholar] [CrossRef]
- Prasad, N.; Rajamani, V.; Hullin, D.; Murray, J.M. Post-operative anaemia in femoral neck fracture patients: Does it need treatment? A single blinded prospective randomised controlled trial. Injury 2009, 40, 1073–1076. [Google Scholar] [CrossRef]
- Mears, S.C.; Kates, S.L. A Guide to Improving the Care of Patients with Fragility Fractures, Edition 2. Geriatr. Orthop. Surg. Rehabilitation 2015, 6, 58–120. [Google Scholar] [CrossRef]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 13933. [Google Scholar] [CrossRef]
- Andritsos, L.; Thomas, O.; Pallikadavath, S.; Kirmani, S.; Sambwhani, S. Neck of Femur Fractures in the First Eight Months of the COVID-19 Pandemic: A UK Systematic Review and Meta-Analysis. Cureus 2021, 13, e20262. [Google Scholar] [CrossRef]
- Zhu, Y.; Chen, W.; Xin, X.; Yin, Y.; Hu, J.; Lv, H.; Li, W.; Deng, X.; Zhu, C.; Zhu, J.; et al. Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China. Int. Orthop. 2020, 44, 1565–1570. [Google Scholar] [CrossRef]
- Kayani, B.; Onochie, E.; Patil, V.; Begum, F.; Cuthbert, R.; Ferguson, D.; Bhamra, J.S.; Sharma, A.; Bates, P.; Haddad, F.S. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures: A multicentre cohort study. Bone Jt. J. 2020, 102, 1136–1145. [Google Scholar] [CrossRef]
- Hall, A.J.; Clement, N.D.; Farrow, L.; MacLullich, A.M.J.; Dall, G.F.; Scott, C.E.H.; Jenkins, P.J.; White, T.O.; Duckworth, A.D. Impact-Scot Study Group IMPACT-Scot report on COVID-19 and hip fractures. Bone Jt. J. 2020, 102-B, 1219–1228. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. China medical treatment expert group for COVID-19 2020. Clinical Characteristics of coronavirus disease in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Grieco, D.L.; Menga, L.S.; Eleuteri, D.; Antonelli, M. Patient self-inflicted lung injury: Implications for acute hypoxemic respiratory failure and ARDS patients on non-invasive support. Minerva Anestesiol. 2019, 85, 1014–1023. [Google Scholar] [CrossRef]
- Fletcher, J.W.A.; Sommer, C.; Eckardt, H.; Knobe, M.; Gueorguiev, B.; Stoffel, K. Intracapsular Femoral Neck Fractures—A Surgical Management Algorithm. Medicina 2021, 57, 791. [Google Scholar] [CrossRef]
- Muñoz Vives, J.M.; Jornet-Gibert, M.; Cámara-Cabrera, J.; Esteban, P.L.; Brunet, L.; Delgado-Flores, L.; Camacho-Carrasco, P.; Torner, P.; Marcano-Fernández, F. Spanish HIP-COVID Investigation Group Mortality Rates of Patients with Proximal Femoral Fracture in a Worldwide Pandemic: Preliminary Results of the Spanish HIP-COVID Observational Study. J. Bone Jt. Surg. Am. 2020, 102, e69. [Google Scholar] [CrossRef]
- Pincus, D.; Jenkinson, R.; Paterson, M.; Leroux, T.; Ravi, B. Association between Surgical Approach and Major Surgical Complications in Patients Undergoing Total Hip Arthroplasty. J. Am. Med. Assoc. 2020, 323, 1070–1076. [Google Scholar] [CrossRef]
- Spina, M.; Luppi, V.; Chiappi, J.; Bagnis, F.; Balsano, M. Direct anterior approach versus direct lateral approach in total hip arthroplasty and bipolar hemiarthroplasty for femoral neck fractures: A retrospective comparative study. Aging Clin. Exp. Res. 2020, 33, 1635–1644. [Google Scholar] [CrossRef]
- Moskal, J.T.; Capps, S.G.; Scanelli, J.A. Anterior muscle sparing approach for total hip arthroplasty. World J. Orthop. 2013, 4, 12–18. [Google Scholar] [CrossRef]
- Pujol, O.; Soza, D.; Lara, Y.; Castellanos, S.; Hernández, A.; Barro, V. Restoring hip biomechanics during the learning curve of a novice surgeon: Direct anterior approach vs. posterior approach. J. Orthop. 2021, 26, 72–78. [Google Scholar] [CrossRef]
- Wang, Z.; Hou, J.-Z.; Wu, C.-H.; Zhou, Y.-J.; Gu, X.-M.; Wang, H.-H.; Feng, W.; Cheng, Y.-X.; Sheng, X.; Bao, H.-W. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J. Orthop. Surg. Res. 2018, 13, 229. [Google Scholar] [CrossRef]
- Higgins, B.T.; Barlow, D.R.; Heagerty, N.E.; Lin, T.J. Anterior vs. Posterior Approach for Total Hip Arthroplasty, a Systematic Review and Meta-analysis. J. Arthroplast. 2015, 30, 419–434. [Google Scholar] [CrossRef]
- Kunkel, S.T.; Sabatino, M.J.; Kang, R.; Jevsevar, D.S.; Moschetti, W.E. A systematic review and meta-analysis of the direct anterior approach for hemiarthroplasty for femoral neck fracture. Eur. J. Orthop. Surg. Traumatol. 2017, 28, 217–232. [Google Scholar] [CrossRef]
- Notarnicola, A.; Pesce, V.; Scaraggi, A.; Maccagnano, G.; Vicenti, G.; Moretti, B. Total hip replacement in a patient with acquired haemophilia a: A case report and literature review. Blood Coagul. Fibrinolysis 2011, 22, 436–439. [Google Scholar] [CrossRef]
- Juraj, M.; Jaroslav, V.; Gažová, A.; Žufková, V.; Kyselovič, J.; Šteňo, B. Evaluation of efficacy and safety of systemic and topical intra-articular administration of tranexamic acid in primary unilateral total hip arthroplasty. Medicine 2021, 100, e26565. [Google Scholar] [CrossRef]
- Ors, C.; Caylak, R. The efficacy, safety, and cost-effectives of combined administration of Intravenous and Local Tranexamic Acid in the management of Patients Undergoing Primary Total Hip Arthroplasty: A prospective, blinded and randomized clinical study. Acta Orthop. et Traumatol. Turc. 2021, 55, 422–427. [Google Scholar] [CrossRef]
- Parvizi, J.; Rasouli, M.R.; Jaberi, M.; Chevrollier, G.; Vizzi, S.; Sharkey, P.F.; Hozack, W.J. Does the surgical approach in one stage bilateral total hip arthroplasty affect blood loss? Int. Orthop. 2013, 37, 2357–2362. [Google Scholar] [CrossRef] [PubMed]
- Egol, K.A.; Konda, S.R.; Bird, M.L.; Dedhia, N.; Landes, E.K.; Ranson, R.A.; Solasz, S.J.; Aggarwal, V.K.; Bosco, J.A.; Furgiuele, D.L.; et al. Increased Mortality and Major Complications in Hip Fracture Care During the COVID-19 Pandemic: A New York City Perspective. J. Orthop. Trauma 2020, 34, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Fell, A.; Malik-Tabassum, K.; Rickman, S.; Arealis, G. Thirty-day mortality and reliability of Nottingham Hip Fracture Score in patients with COVID19 infection. J. Orthop. 2021, 26, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Kucukdurmaz, F.; Sukeik, M.; Parvizi, J. A meta-analysis comparing the direct anterior with other approaches in primary total hip arthroplasty. Surgeon 2018, 17, 291–299. [Google Scholar] [CrossRef]
- Miller, L.E.; Gondusky, J.S.; Bhattacharyya, S.; Kamath, A.F.; Boettner, F.; Wright, J. Does Surgical Approach Affect Outcomes in Total Hip Arthroplasty Through 90 Days of Follow-Up? A Systematic Review with Meta-Analysis. J. Arthroplast. 2018, 33, 1296–1302. [Google Scholar] [CrossRef]
- Chong, Y.; Nan, C.; Mu, W.; Wang, C.; Zhao, M.; Yu, K. Effects of prone and lateral positioning alternate in high-flow nasal cannula patients with severe COVID-19. Crit. Care 2022, 26, 28. [Google Scholar] [CrossRef]
- Schifino, G.; de Grauw, A.J.; Daniele, F.; Comellini, V.; Fasano, L.; Pisani, L. Effects of prone and lateral position in non-intubated patients with 2019 Novel Coronavirus (COVID-19) pneumonia. Pulmonology 2020, 27, 167–171. [Google Scholar] [CrossRef]
- Retucci, M.; Aliberti, S.; Ceruti, C.; Santambrogio, M.; Tammaro, S.; Cuccarini, F.; Carai, C.; Grasselli, G.; Oneta, A.M.; Saderi, L.; et al. Prone and Lateral Positioning in Spontaneously Breathing Patients with COVID-19 Pneumonia Undergoing Noninvasive Helmet CPAP Treatment. Chest 2020, 158, 2431–2435. [Google Scholar] [CrossRef]
- Rauseo, M.; Mirabella, L.; Caporusso, R.R.; Cantatore, L.P.; Perrini, M.P.; Vetuschi, P.; La Bella, D.; Tullo, L.; Cinnella, G. SARS-CoV-2 pneumonia succesfully treated with cpap and cycles of tripod position: A case report. BMC Anesthesiol. 2021, 21, 9. [Google Scholar] [CrossRef]
- Rauseo, M.; Mirabella, L.; Laforgia, D.; Lamanna, A.; Vetuschi, P.; Soriano, E.; Ugliola, D.; Casiello, E.; Tullo, L.; Cinnella, G. A Pilot Study on Electrical Impedance Tomography During CPAP Trial in Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Pneumonia: The Bright Side of Non-invasive Ventilation. Front. Physiol. 2021, 12, 728243. [Google Scholar] [CrossRef]
- Cinnella, G.; Rauseo, M. Proning Responder or Not? This Is the Question. Crit. Care Med. 2022, 50, 708–711. [Google Scholar] [CrossRef]
- Goligher, E.C.; Jonkman, A.H.; Dianti, J.; Vaporidi, K.; Beitler, J.R.; Patel, B.K.; Yoshida, T.; Jaber, S.; Dres, M.; Mauri, T.; et al. Clinical strategies for implementing lung and diaphragm-protective ventilation: Avoiding insufficient and excessive effort. Intensiv. Care Med. 2020, 46, 2314–2326. [Google Scholar] [CrossRef]


| Age | Study Group | Control Group | p-Value |
|---|---|---|---|
| Mean ± SD | 77.02 ± 6.03 | 82.70 ± 4.89 | 0.01 |
| Gender | |||
| Female. n (%) | 20 (40%) | 33 (66%) | 0.01 |
| BMI (kg/cm2) | |||
| Mean ± SD | 26.59 ± 4.11 | 24.92 ± 2.32 | 0.02 |
| Surgical Approach | |||
| Lateral. n (%) | 25 (50%) | 25 (50%) | |
| Anterior. n (%) | 25 (50%) | 25 (50%) | |
| Surgical Time (min) | |||
| Mean ± SD | 53.74 ± 9.98 | 53.28 ± 0.09 | 0.84 |
| Nottingham Hip Fracture Score | |||
| Mean ± SD | 5.02 ± 1.02 | 5.04 ± 1.01 | 0.87 |
| ASA score | |||
| 2. n (%) | 15 (30%) | 13 (26%) | 0.84 |
| 3. n (%) | 28 (56%) | 31 (62%) | |
| 4. n (%) | 7 (14%) | 6 (12%) |
| Mean ± SD or n (%) | Group A | Group B | p-Value |
|---|---|---|---|
| Age (year) | 75.64 ± 5.13 | 78.40 ± 6.63 | 1.37 |
| Sex (female) | 10 (40%) | 10 (40%) | 0.61 |
| BMI (Kg/cm2) | 27.38 ± 3.97 | 25.82 ± 4.18 | 0.16 |
| Surgical Time (min) | 61 ± 8.47 | 46.48 ± 4.72 | 0.01 |
| Nottingham Hip fracture Score | 4.85 ± 0.99 | 5.20 ± 1.04 | 0.16 |
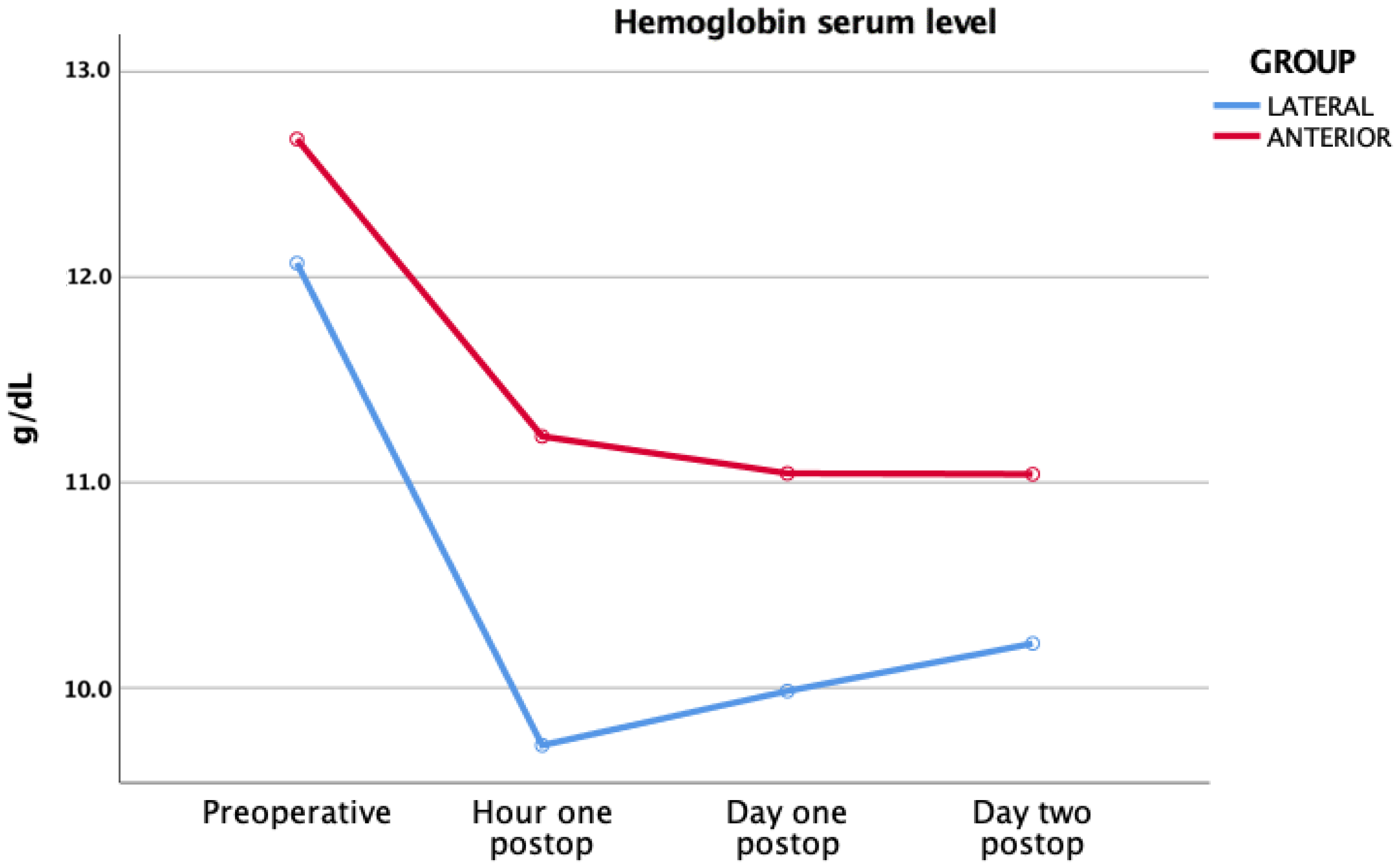
| Pre-operative hemoglobin (g/dL) | 12.07 ± 1.74 | 12.67 ± 1.82 | 0.27 |
| Pre-operative pH | 7.44 ± 0.08 | 7.42 ± 0.08 | 0.71 |
| Pre-operative pO2 (mmHg) | 88.4 ± 30.98 | 80.48 ± 25.65 | 0.21 |
| Pre-operative pCO2 (mmHg) | 40 ± 8.66 | 40.20 ± 9.17 | 0.92 |
| Pre-operative HHb | 2.50 ± 2.19 | 4.15 ± 3.29 | 0.08 |
| Pre-operative P/F | 273.16 ± 120.09 | 301.56 ± 147.33 | 0.76 |
| Pre-operative Alhazzani score | 2.20 ± 0.87 | 2.32 ± 0.85 | 0.60 |
| Different Times | Pre-Operative | One Hour Post-Operative | Day One Post-Operative | Day Two Post-Operative | |||||
|---|---|---|---|---|---|---|---|---|---|
| Ventilation Type | Group A/Group B | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| No oxygen support | 10 (40%) | 15 (60%) | 8 (32%) | 7 (28%) | 6 (24%) | 5 (20%) | 6 (24%) | 5 (20%) | |
| Conventional oxygen therapy | 0 (0%) | 0 (0%) | 2 (8%) | 0 (0%) | 3 (12%) | 0 (0%) | 3 (12%) | 0 (0%) | |
| Venturi | 8 (32%) | 5 (20%) | 8 (32%) | 9 (36%) | 9 (36%) | 7 (28%) | 10 (40%) | 6 (24%) | |
| HFNC | 1 (4%) | 0 (0%) | 1 (4%) | 0 (0%) | 1 (4%) | 0 (0%) | 4 (16%) | 0 (0%) | |
| CPAP | 0 (0%) | 2 (8%) | 0 (0%) | 1 (4%) | 0 (0%) | 2 (8%) | 0 (0%) | 2 (8%) | |
| NIV | 6 (24%) | 3 (12%) | 6 (24%) | 8 (32%) | 4 (16%) | 11 (44%) | 4 (16%) | 12 (48%) | |
| Mechanical ventilation | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (8%) | 0 (0%) | 2 (8%) | 0 (0%) | |
| Alhazzani scores | |||||||||
| Critical | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (8%) | 10 (40%) | 2 (8%) | 2 (8%) | |
| Severe | 12 (48%) | 14 (56%) | 12 (48%) | 20 (80%) | 11 (44%) | 20 (80%) | 11 (44%) | 18 (72%) | |
| Moderate | 6 (24%) | 5 (20%) | 7 (28%) | 0 (0%) | 7 (28%) | 0 (0%) | 7 (28%) | 0 (0%) | |
| Mild | 7 (28%) | 6 (24%) | 6 (24%) | 5 (20%) | 5 (20%) | 5 (20%) | 5 (20%) | 5 (20%) | |
| Surgical Time | p-Value | Spearman’s Rank Correlation Coefficient |
|---|---|---|
| Pre-operative hemoglobin (g/dL) | 0.39 | −0.12 |
| Hour One Post-operative hemoglobin (g/dL) | 0.02 | −0.33 |
| Day One Post-operative hemoglobin (g/dL) | 0.04 | −0.29 |
| Day Two Post-operative hemoglobin (g/dL) | 0.08 | −0.25 |
| Different p-Value | |||
|---|---|---|---|
| Pre-Operative vs. | One Hour Post-Operative | Day One Post-Operative | Day Two Post-Operative |
| Group A | 0.56 | 0.06 | 0.06 |
| Group B | 0.18 | 0.05 | 0.02 |
| p-Value | Spearman’s Rank Correlation Coefficient | |
|---|---|---|
| Pre-operative vs. | 0.78 | 0.041 |
| One hour Post-operative | 0.34 | 0.136 |
| Day One Post-operative | 0.03 | 0.315 |
| Day Two Post-operative | 0.02 | 0.333 |
| Different Time p-Value | |||||
|---|---|---|---|---|---|
| Pre-operative vs. Hour One | Hour One vs. Day One | Day One vs. Day Two | Related-Samples | ||
| Group A | |||||
| Hb (g/dL) | <0.01 | 0.35 | 0.01 | <0.01 | |
| pH | 0.70 | 0.81 | 0.57 | 0.95 | |
| pO2 (mmHg) | 0.22 | 0.08 | 0.47 | 0.05 | |
| pCO2 (mmHg) | 0.38 | 0.55 | 0.87 | 0.82 | |
| HHb | 0.69 | 0.08 | 0.05 | 0.09 | |
| P/F | 0.10 | 0.03 | 0.84 | 0.38 | |
| Group B | |||||
| Hb (g/dL) | <0.01 | <0.01 | 0.63 | <0.01 | |
| pH | 0.80 | 0.50 | 0.71 | 0.90 | |
| pO2 (mmHg) | 0.05 | 0.04 | 0.06 | 0.17 | |
| pCO2 (mmHg) | 0.55 | 0.95 | 0.57 | 0.65 | |
| HHb | <0.01 | 0.12 | <0.01 | <0.01 | |
| P/F | <0.01 | <0.01 | 0.14 | <0.01 | |
| pH | pO2 | pCO2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | p-Value | B | 95% CI | p-Value | B | 95% CI | p-Value | ||||
| Intercept | 7.51 | <0.01 | 82.28 | <0.01 | 47.13 | <0.01 | ||||||
| Non-COVID-19 | −0.03 | −0.04 | −0.02 | <0.01 | −3.77 | −7.28 | −0.26 | 0.04 | −3.40 | −4.51 | −1.57 | <0.01 |
| Anterior approach | −0.01 | −0.02 | 0.01 | 0.65 | −0.98 | −4.64 | 2.67 | 0.60 | −0.81 | −2.34 | 0.72 | 0.30 |
| Sex (female) | 0.01 | −0.01 | 0.02 | 0.35 | −1.96 | −5.33 | 1.43 | 0.26 | −1.18 | −2.60 | 0.23 | 0.10 |
| Age | <0.01 | −0.01 | 0.01 | 0.27 | −0.37 | −0.66 | −0.08 | 0.01 | −0.01 | −0.13 | 0.12 | 0.95 |
| BMI | −0.01 | −0.01 | 0.01 | 0.08 | 1.19 | 0.67 | 1.71 | <0.01 | 0.09 | −0.13 | 0.31 | 0.42 |
| Surgical Time | <0.01 | 0.01 | 0.01 | 0.10 | 0.12 | −0.09 | 0.32 | 0.27 | −0.07 | −0.16 | 0.01 | 0.10 |
| Fu time | <0.01 | −0.01 | 0.01 | 0.70 | −0.09 | −1.41 | 1.24 | 0.90 | 0.57 | 0.22 | 1.13 | 0.05 |
| HHb | P/F | |||||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI | p-Value | B | 95% CI | p-Value | |||
| Intercept | 3.88 | <0.01 | 505.29 | <0.01 | ||||
| Non-Covid-19 | −0.71 | −1.28 | −0.15 | 0.01 | 109.37 | 87.32 | 131.43 | <0.01 |
| Anterior approach | −0.21 | −0.80 | 0.37 | 0.48 | −13.57 | −36.51 | 9.38 | 0.25 |
| Sex (female) | 0.48 | −0.06 | 1.02 | 0.08 | 7.02 | −14.19 | 28.24 | 0.56 |
| Age | 0.05 | 0.01 | 0.10 | 0.03 | −4.92 | −6.74 | −3.10 | <0.01 |
| BMI | −0.20 | −0.29 | −0.12 | <0.01 | 3.87 | 0.60 | 7.14 | 0.02 |
| Surgical Time | 0.02 | −0.01 | 0.05 | 0.23 | −0.77 | −2.05 | 0.51 | 0.24 |
| Fu time | −0.23 | −0.44 | −0.02 | 0.03 | −7.56 | −15.88 | 0.72 | 0.08 |
| Hb | PBC | |||||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI | p-Value | B | 95% CI | p-Value | |||
| Intercept | 12.36 | <0.01 | −1.54 | 0.04 | ||||
| Non-COVID-19 | −0.47 | −0.73 | −0.15 | 0.01 | 0.14 | −0.01 | 0.30 | 0.08 |
| Anterior approach | 1.01 | 0.68 | 1.35 | <0.01 | −0.17 | −0.33 | −0.02 | 0.03 |
| Sex (female) | −0.18 | −0.49 | 0.13 | 0.26 | −0.19 | −0.34 | −0.04 | 0.02 |
| Age | −0.01 | −0.04 | 0.02 | 0.54 | 0.01 | −0.01 | 0.02 | 0.08 |
| BMI | −0.04 | −0.09 | 0.01 | 0.12 | 0.03 | 0.01 | 0.05 | 0.02 |
| Surgical Time | −0.02 | −0.03 | 0.01 | 0.13 | 0.01 | 0.01 | 0.02 | 0.01 |
| Fu time | −0.14 | −0.26 | −0.02 | 0.02 | −0.01 | −0.06 | 0.06 | 0.98 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maccagnano, G.; Maruccia, F.; Rauseo, M.; Noia, G.; Coviello, M.; Laneve, A.; Quitadamo, A.P.; Trivellin, G.; Malavolta, M.; Pesce, V. Direct Anterior versus Lateral Approach for Femoral Neck Fracture: Role in COVID-19 Disease. J. Clin. Med. 2022, 11, 4785. https://doi.org/10.3390/jcm11164785
Maccagnano G, Maruccia F, Rauseo M, Noia G, Coviello M, Laneve A, Quitadamo AP, Trivellin G, Malavolta M, Pesce V. Direct Anterior versus Lateral Approach for Femoral Neck Fracture: Role in COVID-19 Disease. Journal of Clinical Medicine. 2022; 11(16):4785. https://doi.org/10.3390/jcm11164785
Chicago/Turabian StyleMaccagnano, Giuseppe, Francesco Maruccia, Michela Rauseo, Giovanni Noia, Michele Coviello, Andrea Laneve, Alessandro Pio Quitadamo, Giacomo Trivellin, Michele Malavolta, and Vito Pesce. 2022. "Direct Anterior versus Lateral Approach for Femoral Neck Fracture: Role in COVID-19 Disease" Journal of Clinical Medicine 11, no. 16: 4785. https://doi.org/10.3390/jcm11164785
APA StyleMaccagnano, G., Maruccia, F., Rauseo, M., Noia, G., Coviello, M., Laneve, A., Quitadamo, A. P., Trivellin, G., Malavolta, M., & Pesce, V. (2022). Direct Anterior versus Lateral Approach for Femoral Neck Fracture: Role in COVID-19 Disease. Journal of Clinical Medicine, 11(16), 4785. https://doi.org/10.3390/jcm11164785








