Global Impact of the COVID-19 Pandemic on Orthopedics and the Implications of Telemedicine: A Systematic Review of the Literature
Abstract
:1. Introduction
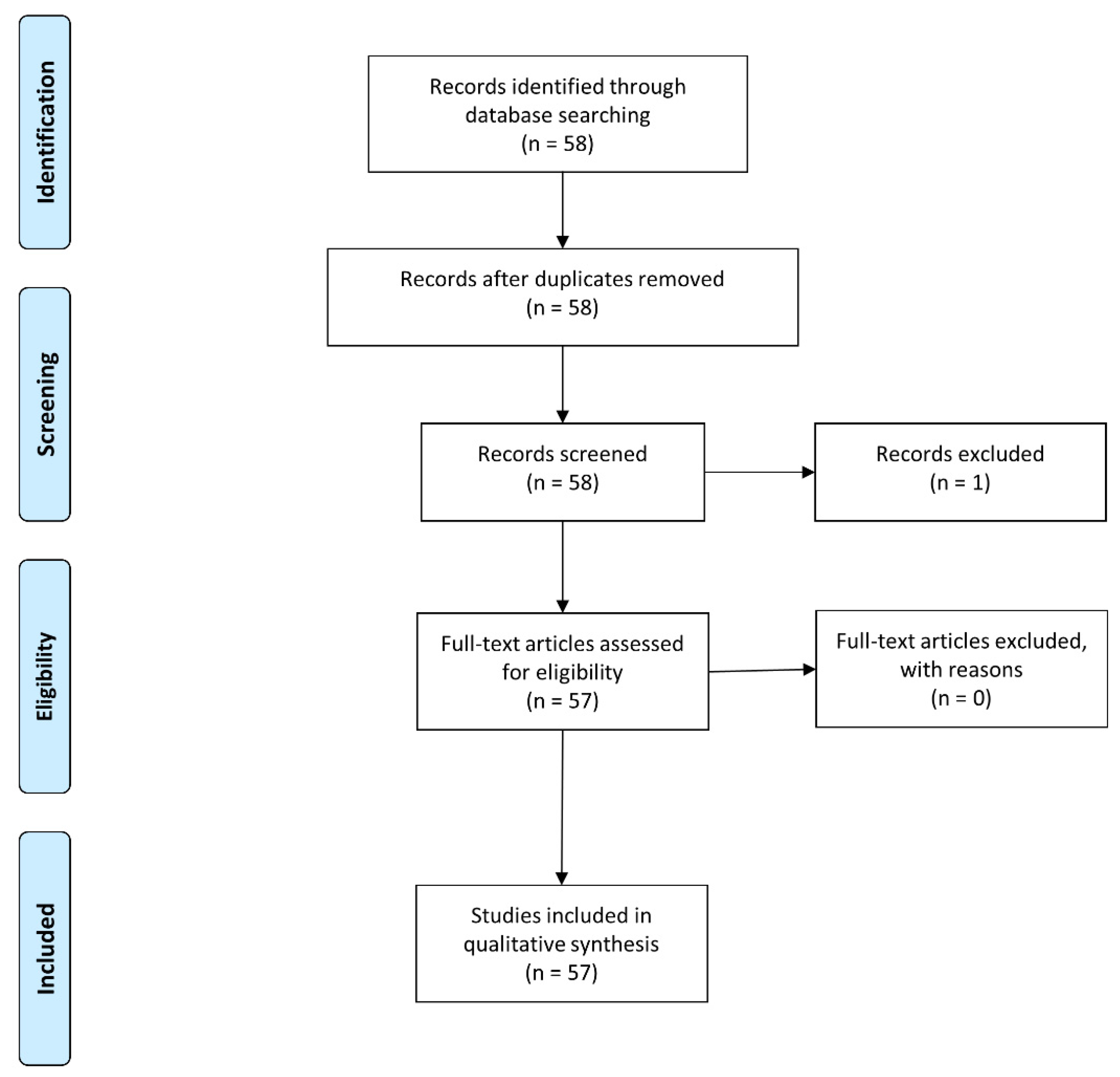
2. Materials and Methods
3. Results
3.1. Impact on Orthopedic Training and Application
3.1.1. Impact on Training
3.1.2. Impact on Application Process
3.2. Impact on Global Orthopedic Performance
3.2.1. Europe
3.2.2. Asia
3.2.3. America
3.2.4. Australia
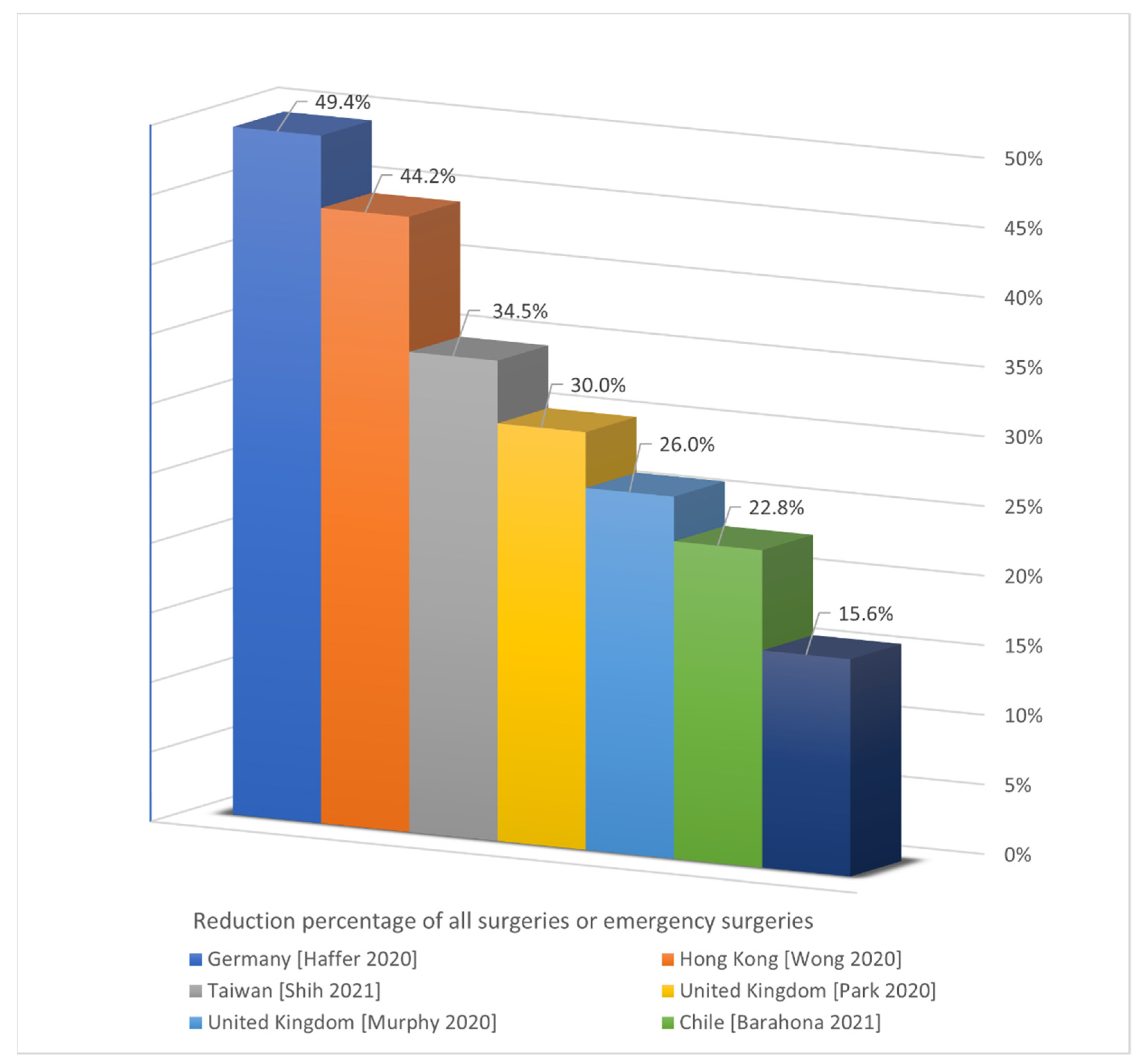
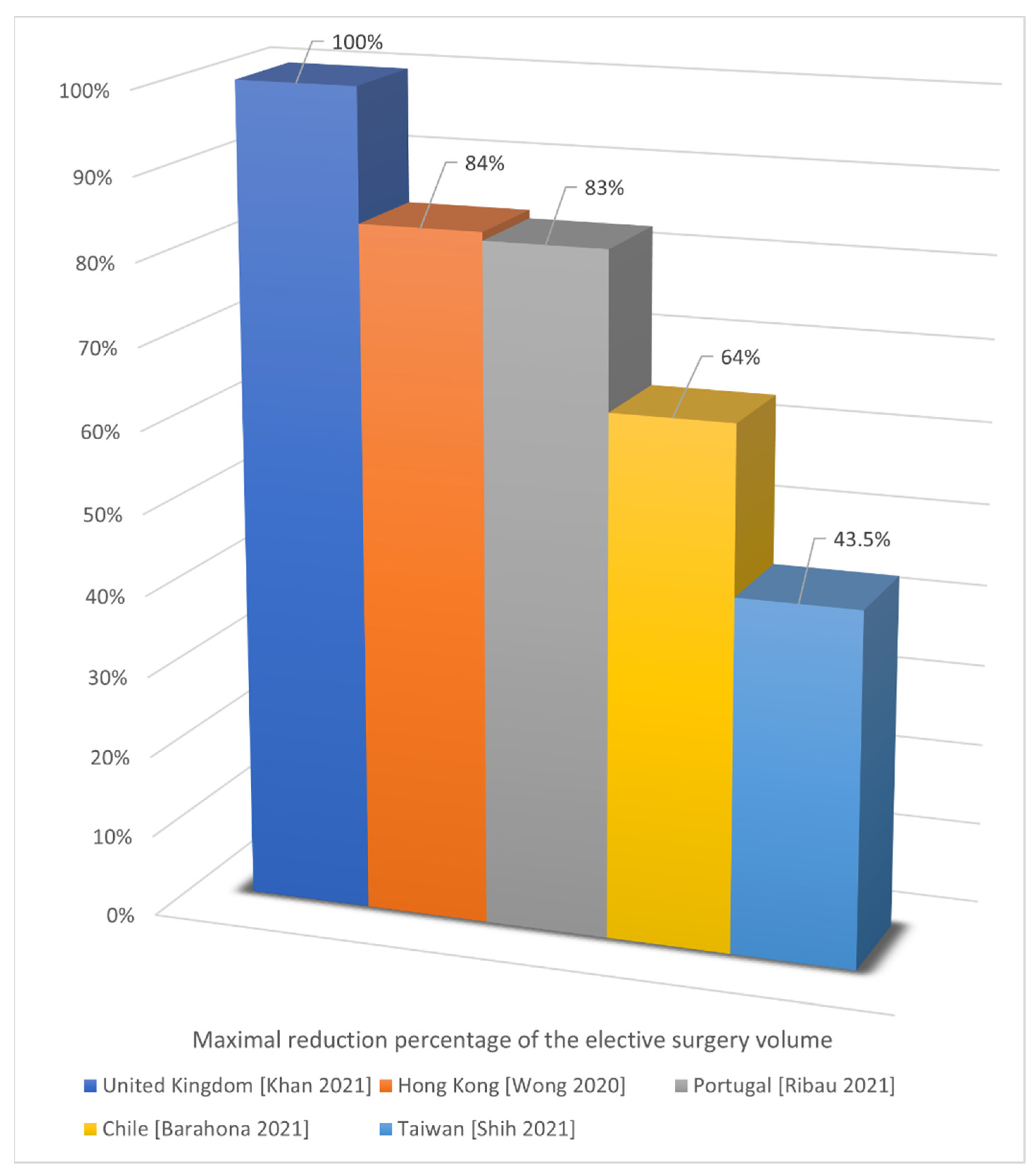
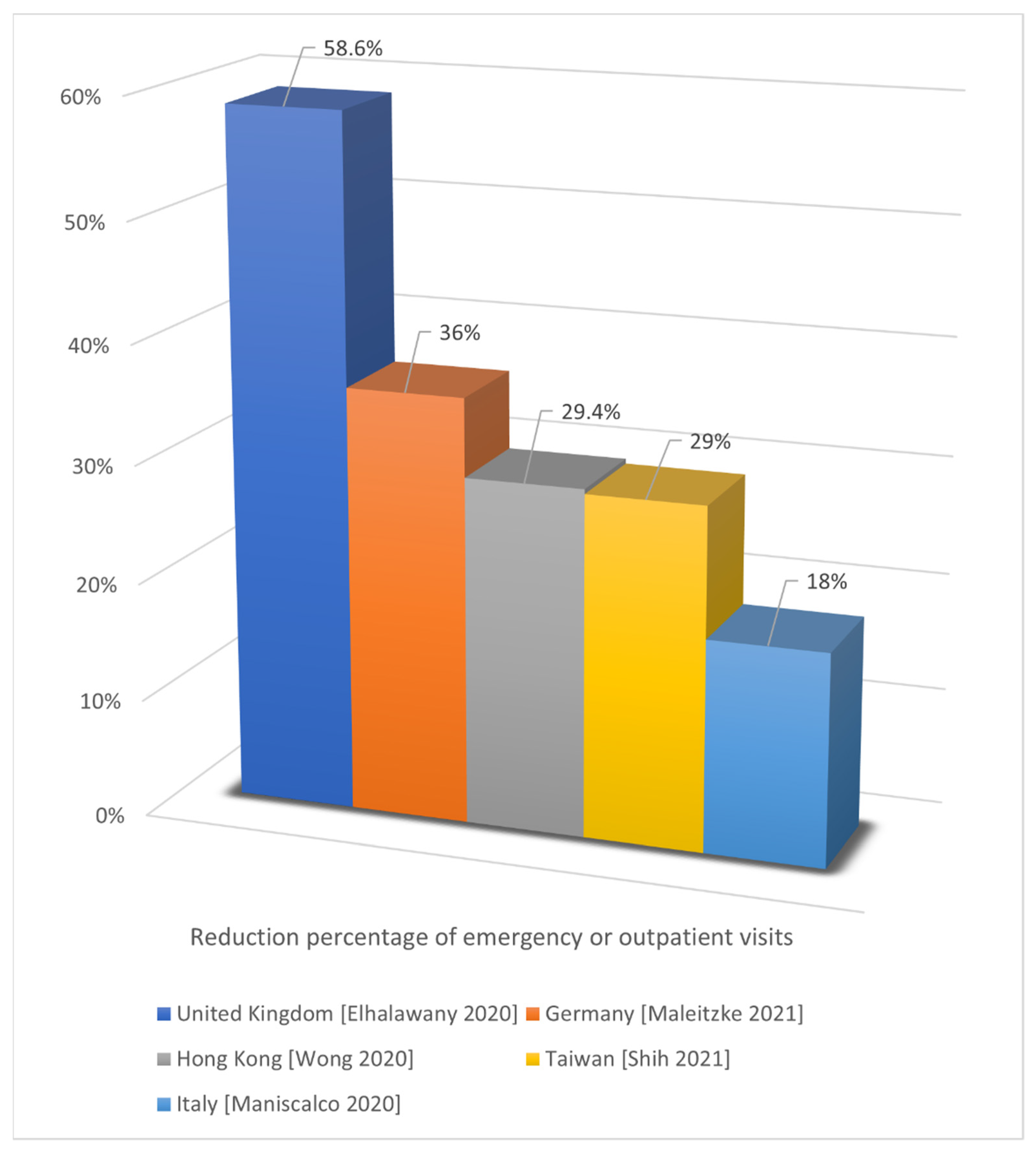
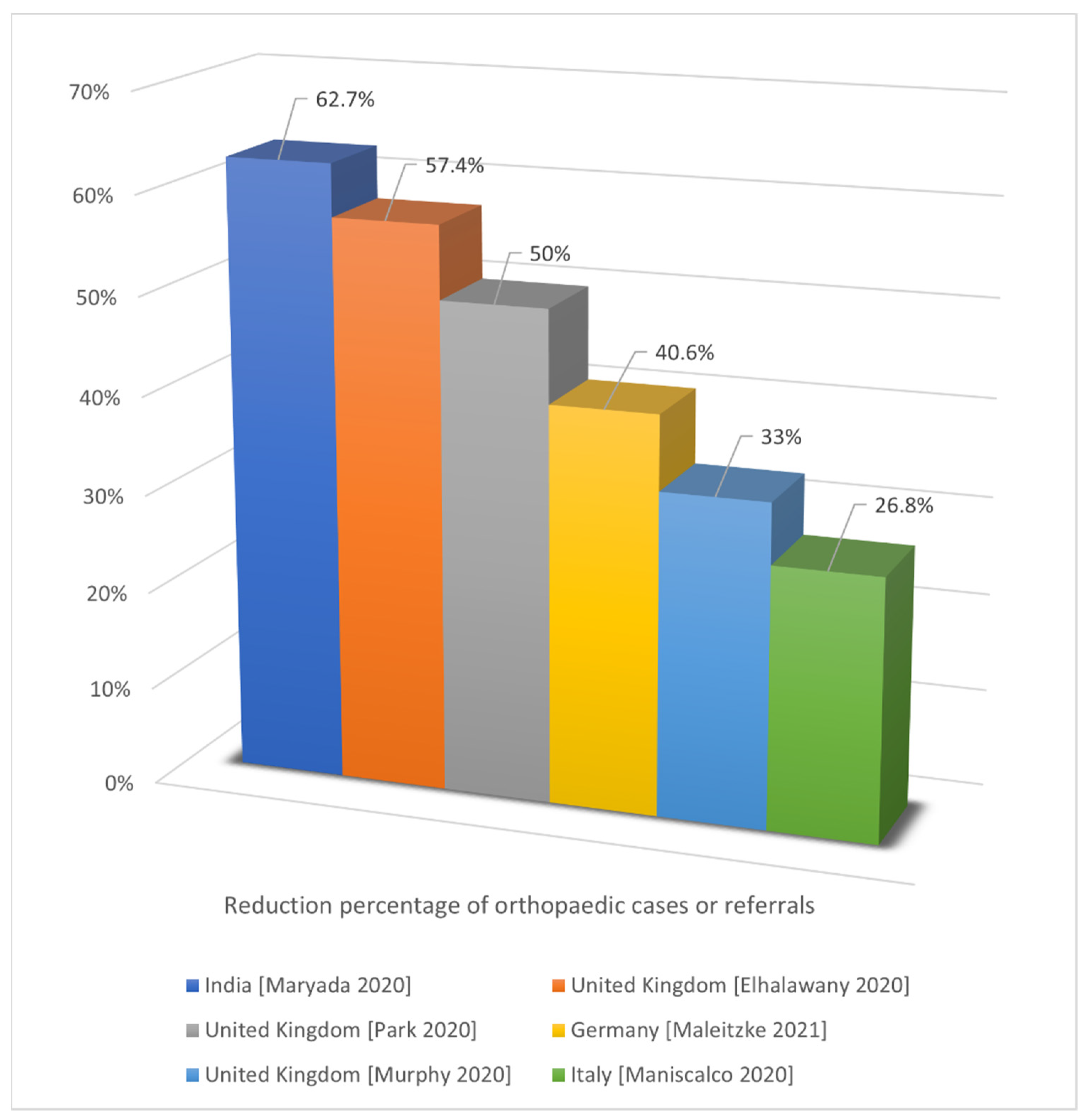
3.2.5. Comparison of the Reduction Percentage in Various Countries
3.3. Impact on Work Loading
3.4. Change of Practice
3.5. Psychological Impact
3.6. Impact on Orthopedic Research Work
3.7. Implications of Telemedicine
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aiyer, A.A.; Granger, C.J.; McCormick, K.L.; Cipriano, C.A.; Kaplan, J.R.; Varacallo, M.A.; Dodds, S.D.; Levine, W.N. The Impact of COVID-19 on the Orthopaedic Surgery Residency Application Process. J. Am. Acad. Orthop. Surg. 2020, 28, e633–e641. [Google Scholar] [CrossRef] [PubMed]
- Alyami, A.H.; Alyami, A.A.; AlMaeen, B.N. Impact of COVID-19 on orthopedic surgery: Experience from Saudi Arabia. Ann. Med. Surg. 2020, 56, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Andreozzi, V.; Marzilli, F.; Muselli, M.; Previ, L.; Cantagalli, M.R.; Princi, G.; Ferretti, A. The impact of COVID-19 on orthopaedic trauma: A retrospective comparative study from a single university hospital in Italy. Orthop. Rev. 2020, 12, 8941. [Google Scholar] [CrossRef]
- Bernstein, D.N.; Greene, N.; Ibrahim, I.O. The personal and professional impact of COVID-19 on orthopedic surgery trainees: Reflections from an incoming intern, current intern, and chief resident. Acta Orthop. 2020, 91, 547–550. [Google Scholar] [CrossRef]
- Chang, D.G.; Park, J.B.; Baek, G.H.; Kim, H.J.; Bosco, A.; Hey, H.W.D.; Lee, C.-K. The impact of COVID-19 pandemic on orthopaedic resident education: A nationwide survey study in South Korea. Int. Orthop. 2020, 44, 2203–2210. [Google Scholar] [CrossRef]
- Clement, N.D.; Hall, A.J.; Makaram, N.S.; Robinson, P.G.; Patton, R.F.L.; Moran, M.; Macpherson, G.J.; Duckworth, A.D.; Jenkins, P.J. IMPACT-Restart: The influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Jt. J. 2020, 102-B, 1774–1781. [Google Scholar] [CrossRef]
- Costa, G.G.; Fanzone, G.; Graceffa, A.; Lauria, M.; Zocco, G.; Cassara, A.; Campailla, A.; Saccà, A.; Santanna, E.; Caputo, G.; et al. The impact of COVID-19 prevention measures on epidemiology of orthopedic injuries: The outbreak ages fractures! Acta Biomed. 2020, 91, e2020158. [Google Scholar]
- Danford, N.C.; Crutchfield, C.; Aiyer, A.; Jobin, C.M.; Levine, W.N.; Lynch, T.S. The Impact of the COVID-19 Pandemic on Orthopaedic Surgery Residency Applicants during the 2021 Residency Match Cycle in the United States. JAAOS Glob. Res. Rev. 2020, 4, e20.00103. [Google Scholar] [CrossRef]
- Dattani, R.; Morgan, C.; Li, L.; Bennett-Brown, K.; Wharton, R.M.H. The impact of COVID-19 on the future of orthopaedic training in the UK. Acta Orthop. 2020, 91, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Elhalawany, A.S.; Beastall, J.; Cousins, G. The impact of the COVID-19 lockdown on orthopaedic emergency presentations in a remote and rural population. Bone Jt. Open 2020, 1, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Ghermandi, R.; Pipola, V.; Terzi, S.; Tedesco, G.; Cavallari, C.; Bandiera, S.; Barbanti Bròdano, G.; Evangelist, G.; Girolami, M.; Gasbarrini, A. The impact of SARS-CoV-2 pandemic on Oncologic and Degenerative Spine Surgery Department activity: The experience of Rizzoli Orthopaedic Institute under COVID-19 lockdown. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7519–7523. [Google Scholar] [PubMed]
- Gonzi, G.; Gwyn, R.; Rooney, K.; Boktor, J.; Roy, K.; Sciberras, N.C.; Pullen, H.; Mohanty, K. The role of orthopaedic trainees during the COVID-19 pandemic and impact on post-graduate orthopaedic education: A four-nation survey of over 100 orthopaedic trainees. Bone Jt. Open 2020, 1, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Haffer, H.; Schomig, F.; Rickert, M.; Randau, T.; Raschke, M.; Wirtz, D.; Pumberger, M.; Perka, C. Impact of the COVID-19 Pandemic on Orthopaedic and Trauma Surgery in University Hospitals in Germany: Results of a Nationwide Survey. J. Bone Jt. Surg. Am. 2020, 102, e78. [Google Scholar] [CrossRef] [PubMed]
- Mackay, N.D.; Wilding, C.P.; Langley, C.R.; Young, J. The impact of COVID-19 on trauma and orthopaedic patients requiring surgery during the peak of the pandemic: A retrospective cohort study. Bone Jt. Open 2020, 1, 520–529. [Google Scholar] [CrossRef]
- Maniscalco, P.; Ciatti, C.; Gattoni, S.; Puma Pagliarello, C.; Moretti, G.; Cauteruccio, M.; Carpaneto, D.; Capelli, P.; Gurrieri, L.; Banchini, F.; et al. The impact of COVID-19 pandemic on the Emergency Room and Orthopedic Departments in Piacenza: A retrospective analysis. Acta Biomed. 2020, 91, e2020028. [Google Scholar]
- Maryada, V.R.; Mulpur, P.; Guravareddy, A.V.; Pedamallu, S.K.; Bhasker, B.V. Impact of COVID-19 Pandemic on Orthopaedic Trauma Volumes: A Multi-Centre Perspective from the State of Telangana. Indian J. Orthop. 2020, 54, 368–373. [Google Scholar] [CrossRef]
- Megaloikonomos, P.D.; Thaler, M.; Igoumenou, V.G.; Bonanzinga, T.; Ostojic, M.; Couto, A.F.; Diallo, J.; Khosravi, I. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery training in Europe. Int. Orthop. 2020, 44, 1611–1619. [Google Scholar] [CrossRef]
- Murphy, T.; Akehurst, H.; Mutimer, J. Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury 2020, 51, 2142–2147. [Google Scholar] [CrossRef]
- Ong, M.T.; Ling, S.K.; Wong, R.M.; Ho, K.K.; Chow, S.K.; Cheung, L.W.; Yung, P.S.-H. Impact of COVID-19 on orthopaedic clinical service, education and research in a university hospital. J. Orthop. Translat. 2020, 25, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Sugand, K.; Nathwani, D.; Bhattacharya, R.; Sarraf, K.M. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: The “golden month”. Acta Orthop. 2020, 91, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.R.; Chang, Y.; Zura, R.D.; Mehta, S.; Giannoudis, P.V.; Nolte, P.A.; Bhandari, M. Impact of COVID-19 on orthopaedic care: A call for nonoperative management. Ther. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20934276. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.A.; Islam, W.; Magruder, M. The Evolving Impact of COVID-19 on Medical Student Orthopedic Education: Perspectives from Medical Students in Different Phases of the Curriculum. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320951721. [Google Scholar] [CrossRef]
- Sahu, D.; Agrawal, T.; Rathod, V.; Bagaria, V. Impact of COVID 19 lockdown on orthopaedic surgeons in India: A survey. J. Clin. Orthop. Trauma 2020, 11, S283–S290. [Google Scholar] [CrossRef]
- Sheridan, G.A.; Hughes, A.J.; Quinlan, J.F.; Sheehan, E.; O’Byrne, J.M. Quantifying the impact of the COVID-19 pandemic on orthopaedic trainees: A national perspective. Bone Jt. Open 2020, 1, 645–652. [Google Scholar] [CrossRef]
- Sugand, K.; Park, C.; Morgan, C.; Dyke, R.; Aframian, A.; Hulme, A.; Evans, S.; Sarraf, K.M.; Baker, C.; Bennett-Brown, K.; et al. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: A multi-centre longitudinal observational study over the “golden weeks”. Acta Orthop. 2020, 91, 633–638. [Google Scholar] [CrossRef]
- Teo, S.H.; Abd Rahim, M.R.; Nizlan, N.M. The impact of COVID-19 pandemic on orthopaedic specialty in Malaysia: A cross-sectional survey. J. Orthop. Surg. 2020, 28, 2309499020938877. [Google Scholar] [CrossRef]
- Upadhyaya, G.K.; Jain, V.K.; Iyengar, K.P.; Patralekh, M.K.; Vaish, A. Impact of COVID-19 on post-graduate orthopaedic training in Delhi-NCR. J. Clin. Orthop. Trauma 2020, 11, S687–S695. [Google Scholar] [CrossRef]
- Wallace, C.N.; Kontoghiorghe, C.; Kayani, B.; Chang, J.S.; Haddad, F.S. The impact of COVID-19 on trauma and orthopaedic surgery in the United Kingdom. Bone Jt. Open 2020, 1, 420–423. [Google Scholar] [CrossRef]
- Wong, J.S.H.; Cheung, K.M.C. Impact of COVID-19 on Orthopaedic and Trauma Service: An Epidemiological Study. J. Bone Jt. Surg. Am. 2020, 102, e80. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.C.; Han, X.A.; Tay, K.S.; Koh, S.B.; Howe, T.S. The psychological impact on an orthopaedic outpatient setting in the early phase of the COVID-19 pandemic: A cross-sectional study. J. Orthop. Surg. Res. 2020, 15, 322. [Google Scholar] [CrossRef] [PubMed]
- Barahona, M.; Infante, C.A.; Palet, M.J.; Barahona, M.A.; Barrientos, C.; Martinez, A. Impact of the COVID-19 Outbreak on Orthopedic Surgery: A Nationwide Analysis of the First Pandemic Year. Cureus 2021, 13, e17252. [Google Scholar] [CrossRef] [PubMed]
- Blum, P.; Putzer, D.; Liebensteiner, M.C.; Dammerer, D. Impact of the COVID-19 Pandemic on Orthopaedic and Trauma Surgery—A Systematic Review of the Current Literature. In Vivo 2021, 35, 1337–1343. [Google Scholar] [CrossRef]
- Chatterji, G.; Patel, Y.; Jain, V.; Geevarughese, N.M.; Haq, R.U. Impact of COVID-19 on Orthopaedic Care and Practice: A Rapid Review. Indian J. Orthop. 2021, 55, 839–852. [Google Scholar] [CrossRef]
- Garcia de Cortazar, A.U.; Arrieta-Salinas, M.; Escobar-Sanchez, D.; Caba-Doussoux, P. Survey about the impact of COVID-19 on the traumatology and orthopedic surgery departments in Spain. J. Healthc. Qual. Res. 2021, 36, 253–262. [Google Scholar]
- Gibbard, M.; Ponton, E.; Sidhu, B.V.; Farrell, S.; Bone, J.N.; Wu, L.A.; Schaeffer, E.; Cooper, A.; Aroojis, A.; Mulpuri, K.; et al. Survey of the Impact of COVID-19 on Pediatric Orthopaedic Surgeons Globally. J. Pediatr. Orthop. 2021, 41, e692–e697. [Google Scholar] [CrossRef]
- Giordano, V.; Belangero, W.; Godoy-Santos, A.L.; Pires, R.E.; Xicara, J.A.; Labronici, P.; Clinical Decision Rules (CDR) Study Group. The hidden impact of rapid spread of the COVID-19 pandemic in professional, financial, and psychosocial health of Latin American orthopedic trauma surgeons. Injury 2021, 52, 673–678. [Google Scholar] [CrossRef]
- Green, G.; Abbott, S.; Vyrides, Y.; Afzal, I.; Kader, D.; Radha, S. The impact of the COVID-19 pandemic on the length of stay following total hip and knee arthroplasty in a high volume elective orthopaedic unit. Bone Jt. Open 2021, 2, 655–660. [Google Scholar] [CrossRef]
- Heaps, B.M.; Ladnier, K.; Haselman, W.T.; Limpisvasti, O.; Banffy, M.B. Epidemiologic impact of COVID-19 on a multi-subspecialty orthopaedic practice. J. Orthop. 2021, 25, 151–154. [Google Scholar] [CrossRef]
- Howles, S.M.; Mahmood, T.; Lala, S.; Pearse, A.; Docker, C. Impact of an Orthopedic-Delivered ‘One-Stop’ Clinic for Ambulatory Trauma on Emergency Department and Fracture Clinic Pressures During the COVID-19 Pandemic. Cureus 2021, 13, e15207. [Google Scholar] [CrossRef] [PubMed]
- Jain, V.K.; Upadhyaya, G.K.; Iyengar, K.P.; Patralekh, M.K.; Lal, H.; Vaishya, R. Impact of COVID-19 on Clinical Practices during Lockdown: A pan India Survey of Orthopaedic Surgeons. Malays. Orthop. J. 2021, 15, 55–62. [Google Scholar] [PubMed]
- Khan, H.; Williamson, M.; Trompeter, A. The impact of the COVID-19 pandemic on orthopaedic services and training in the UK. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.H.; Tsai, S.W.; Chen, C.F.; Wu, P.K.; Chen, C.M.; Chiang, C.C.; Chen, W.-M. Impact of screening COVID-19 on orthopedic trauma patients at the emergency department: A consecutive series from a level I trauma center. J. Chin. Med. Assoc. 2021, 84, 423–427. [Google Scholar] [CrossRef]
- Maleitzke, T.; Pumberger, M.; Gerlach, U.A.; Herrmann, C.; Slagman, A.; Henriksen, L.S.; von Mauchenheim, F.; Hüttermann, N.; Santos, A.N.; Fleckenstein, F.N.; et al. Impact of the COVID-19 shutdown on orthopedic trauma numbers and patterns in an academic Level I Trauma Center in Berlin, Germany. PLoS ONE 2021, 16, e0246956. [Google Scholar] [CrossRef]
- Moretti, L.; Vitale, E.; Bettinsoli, M.; Bizzoca, D.; Delmedico, M.; Papalia, R.; Solarino, G.; Moretti, B. The psychological and clinical impact of the COVID-19 pandemic on orthopaedic patients: An Italian gender-specific analysis. Orthop. Rev. 2021, 13, 9005. [Google Scholar] [CrossRef]
- Oguzkaya, S.; Misir, A.; Ozcamdalli, M.; Eken, G.; Kizkapan, T.B.; Kurk, M.B.; Uzun, E. Impact of the COVID-19 pandemic on orthopedic fracture characteristics in three hospitals in Turkey: A multi-center epidemiological study. Jt. Dis. Relat. Surg. 2021, 32, 323–332. [Google Scholar] [CrossRef]
- Paul, K.D.; Levitt, E.; McGwin, G.; Brabston, E.W., 3rd; Gilbert, S.R.; Ponce, B.A.; Momaya, A.M. COVID-19 Impact on Orthopedic Surgeons: Elective Procedures, Telehealth, and Income. South. Med. J. 2021, 114, 311–316. [Google Scholar] [CrossRef]
- Peebles, L.A.; Kraeutler, M.J.; Waterman, B.R.; Sherman, S.L.; Mulcahey, M.K. The Impact of COVID-19 on the Orthopaedic Sports Medicine Fellowship Application Process. Arthrosc. Sports Med. Rehabil. 2021, 3, e1237–e1241. [Google Scholar] [CrossRef]
- Probert, A.C.; Sivakumar, B.S.; An, V.; Nicholls, S.L.; Shatrov, J.G.; Symes, M.J.; Ellis, A.M. Impact of COVID-19-related social restrictions on orthopaedic trauma in a level 1 trauma centre in Sydney: The first wave. ANZ J. Surg. 2021, 91, 68–72. [Google Scholar] [CrossRef]
- Qian, C.; Zheng, Y.; Meng, J.; Li, H.; Wang, D. A cross-sectional study on the impact of the prevention and control response of the COVID-19 pandemic on minor’s orthopedic trauma in Shanghai. Arch. Public Health 2021, 79, 145. [Google Scholar] [CrossRef] [PubMed]
- Rachuene, P.A.; Masipa, R.R.; Dey, R.; Msingapantsi, M.; Khanyile, S.M.; Phala, M.P.; Murila, J.K.; Mariba, M.T. The impact of COVID-19 national lockdown on orthopaedic trauma admissions in the northern part of South Africa: A multicentre review of tertiary- and secondary-level hospital admissions. S. Afr. Med. J. 2021, 111, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Ribau, A.; Vale, J.; Xara-Leite, F.; Rodrigues-Pinto, R. Impact of COVID-19 pandemic and national lockdown in an orthopaedic and traumatology department-a comparison with the homologous period of 2019. Porto Biomed. J. 2021, 6, e109. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Champagne, A.A.; Del Papa, J.; Toor, J.; Larouche, J.; Nousiainen, M.T. The unique impact of COVID-19 on orthopedic surgery residency applicants and program directors in Canada. Can. J. Surg. 2021, 64, E249–E252. [Google Scholar] [CrossRef]
- Sharma, V.; Kumar, N.; Gupta, B.; Mahajan, A. Impact of COVID-19 pandemic on orthopaedic surgeons in terms of anxiety, sleep outcomes and change in management practices: A cross-sectional study from India. J. Orthop. Surg. 2021, 29, 23094990211001621. [Google Scholar] [CrossRef]
- Shih, C.L.; Huang, P.J.; Huang, H.T.; Chen, C.H.; Lee, T.C.; Hsu, C.H. Impact of the COVID-19 pandemic and its related psychological effect on orthopedic surgeries conducted in different types of hospitals in Taiwan. J. Orthop. Surg. 2021, 29, 2309499021996072. [Google Scholar] [CrossRef]
- Unterfrauner, I.; Hruby, L.A.; Jans, P.; Steinwender, L.; Farshad, M.; Uckay, I. Impact of a total lockdown for pandemic SARS-CoV-2 (COVID-19) on deep surgical site infections and other complications after orthopedic surgery: A retrospective analysis. Antimicrob. Resist. Infect. Control 2021, 10, 112. [Google Scholar] [CrossRef]
- Van Heest, A.; Brandt, A.M.; Dyer, G.; Homer, C.J.; Murray, P.M. COVID-19: Impact on Orthopaedic Graduate Medical Education in the U.S.: AOA Critical Issues Symposium. J. Bone Jt. Surg. Am. 2021, 103, e65. [Google Scholar] [CrossRef]
- Vasiliadis, E.; Vlachos, C.; Papagrigorakis, E.; Evangelopoulos, D.S.; Lelekis, M.; Pneumaticos, S.G. One Year Later: What Was the Impact of the COVID-19 Pandemic on Orthopedic Practice? Cureus 2021, 13, e16013. [Google Scholar] [CrossRef]
- Hsu, C.H.; Hsu, N.C. Impact and Strategies on Joint Surgery Centers without Lockdowns during the Peak of the COVID-19 Pandemic: A Multicenter Cross-Sectional Study. J. Clin. Med. 2021, 10, 5392. [Google Scholar] [CrossRef]
- Hsu, C.H.; Chen, C.H.; Huang, H.T.; Yang, C.J.; Chen, Y.H. To safely reopen after a lockdown, masks are crucial: Lessons from Taiwan. Public Health 2021, 190, 99–100. [Google Scholar] [CrossRef] [PubMed]
- COVID Surg Collaborative; GlobalSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: An international prospective cohort study. Anaesthesia 2021, 76, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Magan, A.A.; Plastow, R.; Haddad, F.S. Impact of COVID-19 on research. Bone Jt. Res. 2020, 9, 531–533. [Google Scholar] [CrossRef]
- Taha, A.; Saad, B.; Enodien, B.; Bachmann, M.; Frey, D.M.; Taha-Mehlitz, S. The Development of Telemedicine and eHealth in Surgery during the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11969. [Google Scholar] [CrossRef] [PubMed]
- Kettlewell, J.; Lindley, R.; Radford, K.; Patel, P.; Bridger, K.; Kellezi, B.; Timmons, S.; Andrews, I.; Fallon, S.; Lannin, N.; et al. Factors Affecting the Delivery and Acceptability of the ROWTATE Telehealth Vocational Rehabilitation Intervention for Traumatic Injury Survivors: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 9744. [Google Scholar] [CrossRef] [PubMed]
- Dionisi, S.; Giannetta, N.; Di Simone, E.; Ricciardi, F.; Liquori, G.; De Leo, A.; Moretti, L.; Napoli, C.; Di Muzio, M.; Orsi, G.B. The Use of mHealth in Orthopedic Surgery: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 12549. [Google Scholar] [CrossRef] [PubMed]
- Kamecka, K.; Rybarczyk-Szwajkowska, A.; Staszewska, A.; Engelseth, P.; Kozlowski, R. Process of Posthospital Care Involving Telemedicine Solutions for Patients after Total Hip Arthroplasty. Int. J. Environ. Res. Public Health 2021, 18, 10135. [Google Scholar] [CrossRef]
- Alsobayel, H.; Alodaibi, F.; Albarrati, A.; Alsalamah, N.; Alhawas, F.; Alhowimel, A. Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study. Int. J. Environ. Res. Public Health 2022, 19, 72. [Google Scholar] [CrossRef]
- Lieneck, C.; Ramamonjiarivelo, Z.; Cox, J.; Dominguez, J.; Gersbach, K.; Heredia, E.; Khan, A. Patient Throughput Initiatives in Ambulatory Care Organizations during the COVID-19 Pandemic: A Systematic Review. Healthcare 2021, 9, 1474. [Google Scholar] [CrossRef]
- Alonazi, A. Effectiveness and Acceptability of Telerehabilitation in Physical Therapy during COVID-19 in Children: Findings of a Systematic Review. Children 2021, 8, 1101. [Google Scholar] [CrossRef]
- Hertling, S.; Loos, F.M.; Graul, I. Telemedicine as a Therapeutic Option in Sports Medicine: Results of a Nationwide Cross-Sectional Study among Physicians and Patients in Germany. Int. J. Environ. Res. Public Health 2021, 18, 7110. [Google Scholar] [CrossRef] [PubMed]
- Lieneck, C.; Weaver, E.; Maryon, T. Outpatient Telehealth Implementation in the United States during the COVID-19 Global Pandemic: A Systematic Review. Medicina 2021, 57, 462. [Google Scholar] [CrossRef] [PubMed]
- Mayer, N.; Portnoy, S.; Palti, R.; Levanon, Y. The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study. Appl. Sci. 2021, 11, 1708. [Google Scholar] [CrossRef]
- Ortiz-Piña, M.; Molina-Garcia, P.; Femia, P.; Ashe, M.C.; Martín-Martín, L.; Salazar-Graván, S.; Salas-Fariña, Z.; Prieto-Moreno, R.; Castellote-Caballero, Y.; Estevez-Lopez, F.; et al. Effects of Tele-Rehabilitation Compared with Home-Based in-Person Rehabilitation for Older Adult’s Function after Hip Fracture. Int. J. Environ. Res. Public Health 2021, 18, 5493. [Google Scholar] [CrossRef]
- Mouli, V.H.; Carrera, C.X.; Schudrowitz, N.; Flanagan Jay, J.; Shah, V.; Fitz, W. Post-Operative Remote Monitoring for Same-Day Discharge Elective Orthopedic Surgery: A Pilot Study. Sensors 2021, 21, 5754. [Google Scholar] [CrossRef]
- Ulivi, M.; Orlandini, L.; Meroni, V.; D’Errico, M.; Fontana, A.; Viganò, M.; Mangiavini, L.; D’Anchise, R.; Parente, F.; Pozzoni, R.; et al. Remote Management of Patients after Total Joint Arthroplasty via a Web-Based Registry during the COVID-19 Pandemic. Healthcare 2021, 9, 1296. [Google Scholar] [CrossRef]
- Dierick, F.; Pierre, A.; Profeta, L.; Telliez, F.; Buisseret, F. Perceived Usefulness of Telerehabilitation of Musculoskeletal Disorders: A Belgium–France Pilot Study during Second Wave of COVID-19 Pandemic. Healthcare 2021, 9, 1605. [Google Scholar] [CrossRef]
- Dell’Isola, A.; Kiadaliri, A.; Turkiewicz, A.; Hughes, V.; Magnusson, K.; Runhaar, J.; Bierma-Zeinstra, S.; Englund, M. The impact of first and second wave of COVID-19 on knee and hip surgeries in Sweden. J. Exp. Orthop. 2021, 8, 60. [Google Scholar] [CrossRef]
- Mason, B.; Stott, S.; Beamish, R. Reduced presentations with fractures or orthopaedic infections to a major children’s hospital during a national COVID-19 elimination strategy. ANZ J. Surg. 2022, 92, 206–211. [Google Scholar] [CrossRef]
- Immel, L.; Neumeier, F.; Peichl, A. The Unequal Consequences of the COVID-19 Pandemic: Evidence from a Large Representative German Population Survey. Rev. Income Wealth 2022. [Google Scholar] [CrossRef]
| No | Study | Year | Country | Region | Restriction * (Lockdown) | Study Method | Focus |
|---|---|---|---|---|---|---|---|
| 1 | Aiyer et al. [3] | 2020 | USA | North America | Partial | Narrative/Perspective | Resident Application |
| 2 | Alyami et al. [4] | 2020 | Saudi Arabia | Middle East | Complete | Narrative/Perspective | Performance/Training |
| 3 | Andreozzi et al. [5] | 2020 | Italy | Europe | Complete | Retrospective | Performance/Orthopedic Trauma |
| 4 | Bernstein et al. [6] | 2020 | USA | North America | Partial | Perspective/Reflection | Resident and intern training |
| 5 | Chang et al. [7] | 2020 | South Korea | Asia | Partial | Survey/Questionnaire | Training/Residency |
| 6 | Clement et al. [8] | 2020 | UK | Europe | Partial | Multicenter, retrospective | Surgical Risk Assessment |
| 7 | Costa et al. [9] | 2020 | Italy | Europe | Partial | Retrospective | Prevention measures |
| 8 | Danford, et al. [10] | 2020 | USA | North America | Partial | Survey/Questionnaire | Resident Application |
| 9 | Dattani et al. [11] | 2020 | UK | Europe | Partial | Perspective/Narrative | Training/Trainees |
| 10 | Elhalawany et al. [12] | 2020 | UK | Europe | Complete | Retrospective | Performance/Orthopedic emergency |
| 11 | Ghermandi et al. [13] | 2020 | Italy | Europe | Partial | Retrospective | Performance/Orthopedic oncology and spine |
| 12 | Gonzi et al. [14] | 2020 | UK | Europe | Partial | Survey/Four-nation questionnaire | Training/Trainees |
| 13 | Haffer et al. [15] | 2020 | Germany | Europe | Partial | Nationwide questionnaire survey | Performance/Orthopedic and Trauma Surgery |
| 14 | Mackay et al. [16] | 2020 | UK | Europe | Partial | Retrospective cohort | Surgical Risk Assessment |
| 15 | Maniscalco et al. [17] | 2020 | Italy | Europe | Complete | Retrospective | Performance/Orthopedics and Emergency Room |
| 16 | Maryada et al. [18] | 2020 | India | Asia | Complete | Multi-center retrospective | Performance/Orthopedic Trauma |
| 17 | Megaloikonomos et al. [19] | 2020 | Europe | Europe | Partial | 23 European countries questionnaire | Training/Trainees |
| 18 | Murphy et al. [20] | 2020 | UK | Europe | Partial | Retrospective | Work loading/Orthopedic |
| 19 | Ong et al. [21] | 2020 | Hong Kong | Asia | Partial | Narrative/Perspective | Performance/Education/Research |
| 20 | Park et al. [22] | 2020 | UK | Europe | Complete | Retrospective | Work loading/Orthopedic trauma |
| 21 | Phillips et al. [23] | 2020 | N/A | N/A | Complete | Review | Orthopedic care |
| 22 | Richardson et al. [24] | 2020 | USA | North America | Partial | Perspectives | Training/medical student |
| 23 | Sahu et al. [25] | 2020 | India | Asia | Complete | Questionnaire survey | Psychological/orthopedic surgeon |
| 24 | Sheridan et al. [26] | 2020 | Ireland | Europe | Partial | Questionnaire | Training/Trainees |
| 25 | Sugand et al. [27] | 2020 | UK | Europe | Complete | Multi-center retrospective | Work loading/Pediatric orthopedic trauma |
| 26 | Teo et al. [28] | 2020 | Malaysia | Asia | Partial | Nationwide questionnaire survey | Practice Change/Surgeon |
| 27 | Upadhyaya et al. [29] | 2020 | India | Asia | Partial | Questionnaire survey | Training/Trainees |
| 28 | Wallace et al. [30] | 2020 | UK | Europe | Complete | Perspectives | Orthopedic surgery and trauma |
| 29 | Wong et al. [31] | 2020 | Hong Kong | Asia | Partial | Retrospective cohort | Performance/Orthopedic and Trauma |
| 30 | Wong et al. [32] | 2020 | Singapore | Asia | Partial | Questionnaire survey | Psychological/orthopedic outpatient setting |
| 31 | Barahona et al. [33] | 2021 | Chile | South America | Partial | Retrospective | Performance/Orthopedic surgery |
| 32 | Blum et al. [34] | 2021 | N/A | N/A | N/A | Review | Performance/Orthopedic and Trauma Surgery |
| 33 | Chatterji et al. [35] | 2021 | N/A | N/A | N/A | Rapid Review | Miscellaneous |
| 34 | Garcia et al. [36] | 2021 | Spain | Europe | Partial | Questionnaire survey | Change of practice/Orthopedic Surgeon |
| 35 | Gibbard et al. [37] | 2021 | N/A | N/A | Partial | Global (45 countries) questionnaire survey | Change of practice/Pediatric Orthopedic Surgeon |
| 36 | Giordano et al. [38] | 2021 | N/A | N/A | Partial | 14 Latin American countries questionnaire survey | Financial, Psychosocial/Orthopedic Trauma surgeon |
| 37 | Green et al. [39] | 2021 | UK | Europe | Partial | Retrospective cohort | Length of stay/total joint arthroplasty |
| 38 | Heaps et al. [40] | 2021 | USA | North America | Partial | Retrospective cohort | Performance/multi-subspecialty |
| 39 | Howles et al. [41] | 2021 | UK | Europe | Partial | Retrospective cohort | Performance/Minor injury one-stop unit |
| 40 | Jain et al. [42] | 2021 | India | Asia | Complete | Nationwide questionnaire | Change of practice/Orthopedic Surgeon |
| 41 | Khan et al. [43] | 2021 | UK | Europe | Partial | Nationwide questionnaire | Change of practice/Orthopedic Surgeon |
| 42 | Ma et al. [44] | 2021 | Taiwan | Asia | No | Retrospective cohort | Screening/Emergency room/Trauma |
| 43 | Maleitzke et al. [45] | 2021 | Germany | Europe | Complete | Retrospective cohort | Performance/Orthopedic trauma |
| 44 | Moretti et al. [46] | 2021 | Italy | Europe | Complete | Nationwide Questionnaire | Psychological/Gender-specific |
| 45 | Oguzkaya et al. [47] | 2021 | Turkey | Asia and Europe | Partial | Multi-center retrospective | Orthopedic fracture characteristics |
| 46 | Paul et al. [48] | 2021 | USA | North America | Partial | Nationwide Questionnaire | Change of practice/Elective procedures/Telehealth and income |
| 47 | Peebles et al. [49] | 2021 | USA | North America | Partial | Narrative Review/Perspective | Sports Fellowship Application |
| 48 | Probert et al. [50] | 2021 | Australia | Australia | Complete | Retrospective | Performance/Orthopedic trauma |
| 49 | Qian et al. [51] | 2021 | China | Asia | Partial | Retrospective | Performance/orthopedic trauma |
| 50 | Rachuene et al. [52] | 2021 | South Africa | Africa | Complete | Multicenter retrospective | Performance/orthopedic trauma |
| 51 | Ribau et al. [53] | 2021 | Portugal | Europe | Complete | Retrospective | Performance/orthopedic trauma |
| 52 | Shah et al. [54] | 2021 | Canada | North America | partial | Narrative Review/Perspectives | Residency application |
| 53 | Sharma et al. [55] | 2021 | India | Asia | Complete | Questionnaire | Psychological/Change of practice |
| 54 | Shih et al. [56] | 2021 | Taiwan | Asia | No | Retrospective | Psychological/Performance |
| 55 | Unterfrauner et al. [57] | 2021 | Switzerland | Europe | Complete | Retrospective | Surgical site infections/Complications |
| 56 | Van Heest et al. [58] | 2021 | USA | North America | Partial | Symposium summary/Review | Training/Orthopedic Graduate Medical Education |
| 57 | Vasiliadis et al. [59] | 2021 | Greece | Europe | Partial | Retrospective cohort | Performance |
| Orthopedic Training | ||||
|---|---|---|---|---|
| Study | Country | Method of Questioning | Subject | Number of Respondents |
| Bernstein et al. [6] | USA | Perspective/Reflection | Resident and intern | N/A |
| Chang et al. [7] | South Korea | Web-based survey questionnaire | Resident | 229 |
| Dattani et al. [11] | UK | Perspective/Narrative | Trainees | N/A |
| Gonzi et al. [14] | UK | Survey/Four-nation questionnaire | Trainees | 101 |
| Megaloikonomos et al. [19] | Europe | 23 European countries questionnaire | Trainees | 327 |
| Richardson et al. [24] | USA | Perspectives | medical student | N/A |
| Sheridan et al. [26] | Ireland | Questionnaire | Trainees | 40 |
| Upadhyaya et al. [29] | India | Questionnaire survey | Post-graduate trainees | 138 |
| Orthopedic Application | ||||
|---|---|---|---|---|
| Study | Country | Method of Questioning | Subject | Number of Respondents |
| Aiyer et al. [3] | USA | Narrative/Perspective | Residency | N/A |
| Danford, et al. [10] | USA | Survey/Questionnaire | Residency | 462 |
| Peebles et al. [49] | USA | Narrative Review/Perspective | Sports Fellowship | N/A |
| Shah et al. [54] | Canada | Narrative Review/Perspectives | Residency | N/A |
| Study | Country | Study Method | Focus | Settings Investigated | Number of Patients (% Change) |
|---|---|---|---|---|---|
| Andreozzi et al. [5] | Italy | Retrospective | Orthopedic trauma | trauma admissions | 995/204 (−79%) [Age 41.4 ± 25.7/51.9 ± 24.8, p < 0.0001] |
| Elhalawany et al. [12] | UK | Retrospective | Orthopedic emergency | lockdown on orthopedic emergency presentations | 4777/1978 (−58.6% emergency visits) 1729/736 (−57.4% orthopedic presentations) |
| Ghermandi et al. [13] | Italy | Retrospective | Orthopedic oncology and spine | Daily surgical activity | 69/102 (+48%) |
| Haffer et al. [15] | Germany | Nationwide questionnaire survey | Orthopedic and trauma surgery | 52 surgeons participated | Mean of estimation from 43 respondents (−49.4% operating room capacity) |
| Maniscalco et al. [17] | Italy | Retrospective | Orthopedics and emergency room | trend of emergency room accesses and events | 32,980/27,042 (−18% emergency room accesses) 4007/2934 (−26.8% orthopedic pathways) |
| Howles et al. [41] | UK | Retrospective cohort | Minor injury one-stop unit | service provided to patients | 700 |
| Maleitzke et al. [45] | Germany | Retrospective cohort | Orthopedic trauma | trauma care in emergency departments | 167.54/106.94 (−36% daily total cases) 52.06/30.91 (−40.6% daily orthopedic trauma cases) |
| Ribau et al. [53] | Portugal | Retrospective | Orthopedic trauma | lockdown period on the surgical activity | 587/100 (−83% elective surgery) |
| Vasiliadis et al. [59] | Greece | Retrospective cohort | Orthopedic practice | everyday orthopedic practice | 1042/550 (−47.2% emergency) |
| Study | Country | Study Method | Focus | Settings Investigated | Number of Patients (% Change) |
|---|---|---|---|---|---|
| Maryada et al. [18] | India | Multi-center retrospective | Orthopedic Trauma | lockdown on the trauma case load | 2020/754 (−62.7% trauma) 1343/298 (−77.9% road traffic accidents) |
| Wong et al. [31] | Hong Kong | Retrospective cohort | Orthopedic and Trauma | All orthopedic practice | 795 ± 115.1/443.6 ± 25.8 (−44.2% weekly operations) 14.9 ± 4.6/2.4 ± 2.2 (−84% weekly elective anterior cruciate ligament reconstruction) 11,693 ± 2240/8261 ± 1104 (−29.4% weekly outpatient visits) |
| Shih et al. [56] | Taiwan | Retrospective | Orthopedic practice | All orthopedic practice | 47.0 ± 8.4/30.8 ± 5.4 (−34.5% weekly surgery) 41.3 ± 8.1/22.8 ± 3.3 (maximal −43.5% weekly elective surgery |
| Study | Country | Study Method | Focus | Settings Investigated | Number of Patients (% Change) |
|---|---|---|---|---|---|
| Barahona et al. [33] | Chile | Retrospective | Orthopedic surgery | Orthopedic surgery in a single country | 128,735/99,333 (−22.8% surgery) 28.23/10.13 per 100,000 inhabitants (−64% maximum in total knee arthroplasty) |
| Heaps et al. [40] | USA | Retrospective cohort | multi-subspecialty | multi-subspecialty surgery percentages analysis | 1917/913 (pre-COVID-19 vs. post-COVID-19) |
| Study | Country | Study Method | Focus | Settings Investigated | Number of Patients (% Change) |
|---|---|---|---|---|---|
| Probert et al. [50] | Australia | Retrospective | Orthopedic trauma | Lockdown on emergency orthopedic surgery | 173/146 (−15.6% emergency operations) |
| Study | Country | Study Method | Focus | Settings Investigated | Number of Patients (% Change) |
|---|---|---|---|---|---|
| Murphy et al. [20] | UK | Retrospective | Orthopedic trauma | trauma referrals | 112/75 (−33% weekly referrals) 53/39 (−26% weekly operations) |
| Park et al. [22] | UK | Retrospective | Orthopedic trauma | trauma referrals and surgery for the first “golden” month | 90/63 (−30% total operations in first month 162/87 (−46.3% acute trauma referrals) |
| Sugand et al. [27] | UK | Multi-center retrospective | Pediatric orthopedic trauma | Lockdown on acute pediatric orthopedic trauma referral caseload | 302/97 (−68% acute pediatric trauma referrals) |
| Study | Country | Study Method | Respondent | Major Change of Practice |
|---|---|---|---|---|
| Teo et al. [28] | Malaysia | Nationwide questionnaire survey | Orthopedic Surgeon | 84.8% (189/223) make decision to manage more conservatively |
| Garcia et al. [36] | Spain | Questionnaire survey | Orthopedic Surgeon | 52% modified the treatment indications |
| Gibbard et al. [37] | N/A | Global (45 countries) questionnaire survey | Pediatric Orthopedic Surgeon | 79% (358/460) of respondents reported a lockdown, resulting in a change of practice |
| Jain et al. [42] | India | Nationwide questionnaire | Orthopedic Surgeon | 91.7% (539/588) had significant changes made in individual hospital protocols |
| Khan et al. [43] | UK | Nationwide questionnaire | Orthopedic Surgeon | All 202 participants reported disruption to their daily practice 91% reported all elective operating had been cancelled |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-H.; Huang, H.-T.; Chen, C.-H.; Fu, Y.-C.; Chou, P.-H.; Hsu, N.-C. Global Impact of the COVID-19 Pandemic on Orthopedics and the Implications of Telemedicine: A Systematic Review of the Literature. J. Clin. Med. 2022, 11, 2983. https://doi.org/10.3390/jcm11112983
Hsu C-H, Huang H-T, Chen C-H, Fu Y-C, Chou P-H, Hsu N-C. Global Impact of the COVID-19 Pandemic on Orthopedics and the Implications of Telemedicine: A Systematic Review of the Literature. Journal of Clinical Medicine. 2022; 11(11):2983. https://doi.org/10.3390/jcm11112983
Chicago/Turabian StyleHsu, Chia-Hao, Hsuan-Ti Huang, Chung-Hwan Chen, Yin-Chih Fu, Pei-Hsi Chou, and Nin-Chieh Hsu. 2022. "Global Impact of the COVID-19 Pandemic on Orthopedics and the Implications of Telemedicine: A Systematic Review of the Literature" Journal of Clinical Medicine 11, no. 11: 2983. https://doi.org/10.3390/jcm11112983
APA StyleHsu, C.-H., Huang, H.-T., Chen, C.-H., Fu, Y.-C., Chou, P.-H., & Hsu, N.-C. (2022). Global Impact of the COVID-19 Pandemic on Orthopedics and the Implications of Telemedicine: A Systematic Review of the Literature. Journal of Clinical Medicine, 11(11), 2983. https://doi.org/10.3390/jcm11112983