Who Benefits Most? Interactions between Personality Traits and Outcomes of Four Incremental Meditation and Yoga Treatments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Transparency and Openness
2.3. Participants
2.4. Treatment
2.5. Measures
2.6. Data Analysis
3. Results
3.1. Moderators of Outcome Variables
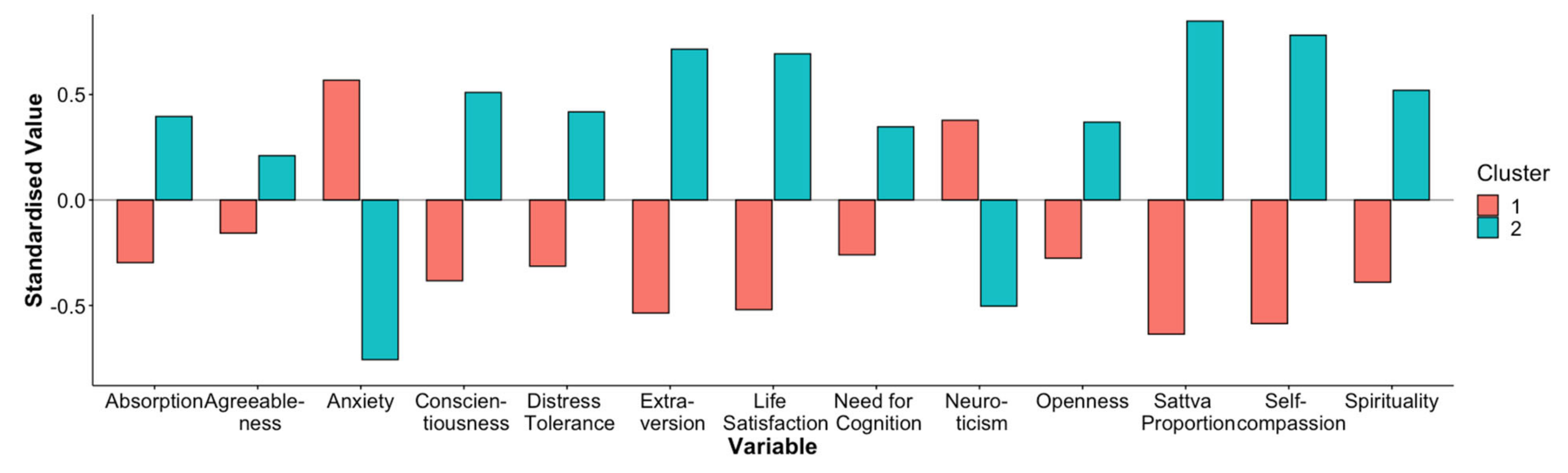
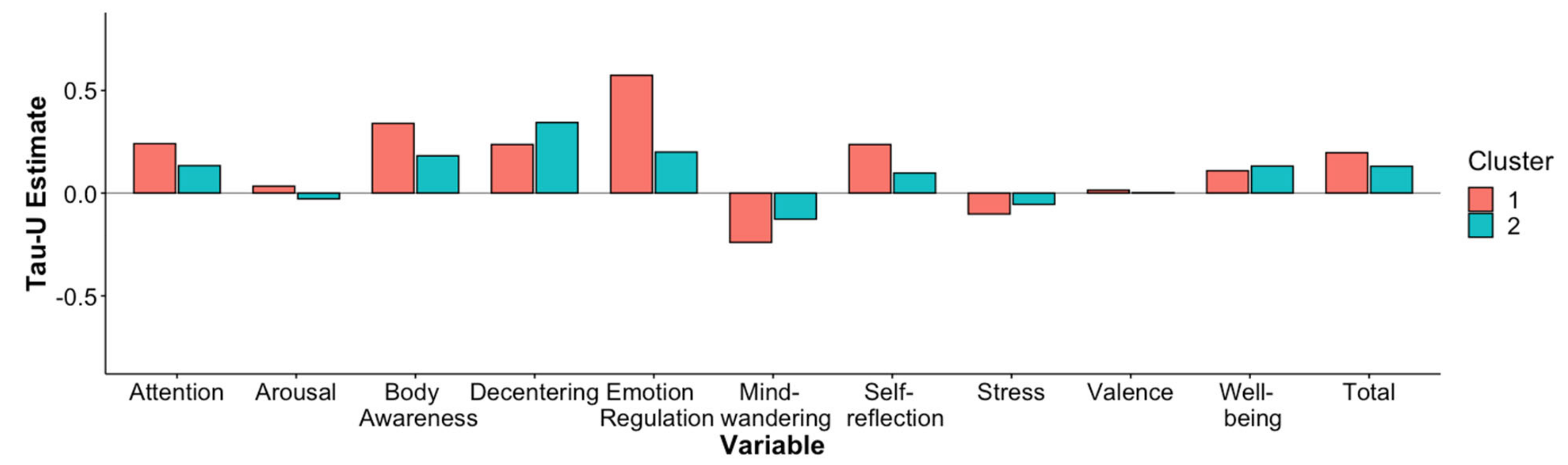
3.2. Cluster Analysis
4. Discussion
4.1. Certain Personality Traits Predict Responses to MBM Treatments
4.2. Certain Components of MBM Treatments Can Have Differential Effects and Indications
4.3. Vulnerable Populations Might Benefit More Than Healthy Populations
4.4. Limitations
4.5. Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartley, L.; Dyakova, M.; Holmes, J.; Clarke, A.; Lee, M.S.; Ernst, E.; Rees, K. Yoga for the Primary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2014, 5, CD010072. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010072.pub2/full (accessed on 30 May 2022). [CrossRef] [PubMed] [Green Version]
- Yang, Z.Y.; Zhong, H.B.; Mao, C.; Yuan, J.Q.; Huang, Y.; Wu, X.Y.; Gao, Y.-M.; Tang, J.-L. Yoga for asthma. Cochrane Database Syst. Rev. 2016, 4. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010346.pub2/full (accessed on 30 May 2022).
- Lawrence, M.; Junior, F.T.C.; Matozinho, H.H.; Govan, L.; Booth, J.; Beecher, J. Yoga for Stroke Rehabilitation. Cochrane Database Syst. Rev. 2017, 12. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011483.pub2/full (accessed on 30 May 2022). [CrossRef] [PubMed] [Green Version]
- Broderick, J.; Crumlish, N.; Waugh, A.; Vancampfort, D. Yoga Versus Non-Standard Care for Schizophrenia. Cochrane Database Syst. Rev. 2017, 9, CD012052. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012052.pub2/full (accessed on 30 May 2022). [CrossRef]
- Klatte, R.; Pabst, S.; Beelmann, A.; Rosendahl, J. The efficacy of body-oriented yoga in mental disorders: A systematic review and meta-analysis. Dtsch. Ärzteblatt Int. 2016, 113, 195–202. [Google Scholar]
- Feuerstein, G. The Yoga Tradition: Its History, Literature, Philosophy and Practice, 3rd ed.; Hohm Press: Prescott, AZ, USA, 2012. [Google Scholar]
- Telles, S.; Singh, N. Science of the mind: Ancient yoga texts and modern studies. Psychiatr Clin. N. Am. 2013, 36, 93–108. [Google Scholar] [CrossRef]
- Matko, K.; Bringmann, H.C.; Sedlmeier, P. Effects of different components of yoga: A meta-synthesis. OBM Integr. Complement. Med. 2021, 6, 26. [Google Scholar]
- Bragard, I.; Etienne, A.-M.; Faymonville, M.-E.; Coucke, P.; Lifrange, E.; Schroeder, H.; Wagener, A.; Dupuis, G.; Jerusalem, G. A nonrandomized comparison study of self-hypnosis, yoga, and cognitive-behavioral therapy to reduce emotional distress in breast cancer patients. Int. J. Clin. Exp. Hypn. 2017, 65, 189–209. [Google Scholar]
- Simon, N.M.; Hofmann, S.G.; Rosenfield, D.; Hoeppner, S.S.; Hoge, E.A.; Bui, E.; Khalsa, S.B.S. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: A randomized clinical trial. JAMA Psychiatry 2021, 78, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.P.; Hampson, S.; Clarkin, J. Personality-informed interventions for healthy aging: Conclusions from a National Institute on Aging workgroup. Dev. Psychol. 2014, 50, 1426–1441. [Google Scholar] [CrossRef] [Green Version]
- Edwards, E. The role of complementary, alternative, and integrative medicine in personalized health care. Neuropsychopharmacology 2012, 37, 293–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, R.; Farquharson, L.; Palmer, L.; Bassett, P.; Clarke, J.; Clark, D.M.; Crawford, M.J. Patient preference in psychological treatment and associations with self-reported outcome: National cross-sectional survey in England and Wales. BMC Psychiatry 2016, 16, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, T.; Farb, N.A.S. Personalising practice using preferences for meditation anchor modality. Front. Psychol 2018, 9, 2521. [Google Scholar] [CrossRef] [PubMed]
- Burke, A. Comparing individual preferences for four meditation techniques: Zen, Vipassana (mindfulness), Qigong, and Mantra. Explore J. Sci. Health 2012, 8, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Carmody, J.; Baer, R.A.; LB Lykins, E.; Olendzki, N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. J. Clin. Psychol. 2009, 65, 613–626. [Google Scholar] [CrossRef]
- Matko, K.; Sedlmeier, P.; Bringmann, H.C. Differential effects of ethical education, physical Hatha yoga, and mantra meditation on well-being and stress in healthy participants—An experimental single-case study. Front. Psychol. 2021, 12, 672301. [Google Scholar] [CrossRef]
- May, C.J.; Weyker, J.R.; Spengel, S.K.; Finkler, L.J.; Hendrix, S.E. Tracking longitudinal changes in affect and mindfulness caused by concentration and loving-kindness meditation with hierarchical linear modeling. Mindfulness 2014, 5, 249–258. [Google Scholar] [CrossRef]
- Saunders, R.; Buckman, J.E.J.; Cape, J.; Fearon, P.; Leibowitz, J.; Pilling, S. Trajectories of depression and anxiety symptom change during psychological therapy. J. Affect Disord. 2019, 249, 327–335. [Google Scholar] [CrossRef]
- Stulz, N.; Lutz, W.; Leach, C.; Lucock, M.; Barkham, M. Shapes of early change in psychotherapy under routine outpatient conditions. J. Consult. Clin. Psychol. 2007, 75, 864. [Google Scholar] [CrossRef]
- Hölzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef]
- Schmalzl, L.; Powers, C.; Henje Blom, E. Neurophysiological and neurocognitive mechanisms underlying the effects of yoga-based practices: Towards a comprehensive theoretical framework. Front. Hum. Neurosci. 2015, 9, 235. [Google Scholar] [CrossRef] [Green Version]
- Tang, R.; Braver, T.S. Towards an individual differences perspective in mindfulness training research: Theoretical and empirical considerations. Front. Psychol. 2020, 11, 818. [Google Scholar] [CrossRef]
- de Vibe, M.; Solhaug, I.; Tyssen, R.; Friborg, O.; Rosenvinge, J.H.; Sørlie, T.; Halland, E.; Bjørndal, A. Does personality moderate the effects of mindfulness training for medical and psychology students? Mindfulness 2015, 6, 281–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyklíček, I.; Irrmischer, M. For whom does Mindfulness-Based Stress Reduction work? Moderating effects of personality. Mindfulness 2017, 8, 1106–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van den Hurk, P.A.; Wingens, T.; Giommi, F.; Barendregt, H.P.; Speckens, A.E.; van Schie, H.T. On the relationship between the practice of mindfulness meditation and personality—An exploratory analysis of the mediating role of mindfulness skills. Mindfulness 2011, 2, 194–200. [Google Scholar] [CrossRef] [Green Version]
- Caspi, O.; Bell, I.R. One size does not fit all: Aptitude x Treatment Interaction (ATI) as a conceptual framework for complementary and alternative medicine outcome research. Part 1—What is ATI Research? J. Altern. Complement. Med. 2004, 10, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Bringmann, H.C.; Bringmann, N.; Jeitler, M.; Brunnhuber, S.; Michalsen, A.; Sedlmeier, P. Meditation-Based Lifestyle Modification: Development of an integrative mind-body program for mental health and human flourishing. Complement. Med. Res. 2021, 28, 252–262. [Google Scholar] [CrossRef]
- Bringmann, H.C.; Bringmann, N.; Jeitler, M.; Brunnhuber, S.; Michalsen, A.; Sedlmeier, P. Meditation Based Lifestyle Modification (MBLM) in outpatients with mild to moderate depression: A mixed-methods feasibility study. Complement. Ther. Med. 2021, 56, 102598. [Google Scholar] [CrossRef]
- Barlow, D.H.; Nock, M.; Hersen, M. Single Case Experimental Designs: Strategies for Studying Behavior for Change, 3rd ed.; Pearson: Boston, MA, USA, 2009. [Google Scholar]
- Ferron, J.M.; Moeyaert, M.; Van den Noortgate, W.; Beretvas, S.N. Estimating causal effects from multiple-baseline studies: Implications for design and analysis. Psychol. Methods 2014, 19, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Pustejovsky, J.E. Procedural sensitivities of effect sizes for single-case designs with directly observed behavioral outcome measures. Psychol. Methods 2019, 24, 217. [Google Scholar] [CrossRef]
- Tate, R.L.; Perdices, M.; Rosenkoetter, U.; Shadish, W.; Vohra, S.; Barlow, D.H.; Horner, R.; Kazdin, A.; Kratochwill, T.; McDonald, S.; et al. The Single-Case Reporting guideline In Behavioural Interventions (SCRIBE) 2016 statement. Phys. Ther. 2016, 96, e1-10. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 30 May 2022).
- Kassambara, A. Ggpubr: “ggplot2” Based Publication Ready Plots 2020. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 3 December 2020).
- Behrendt, S. lm.beta: Add Standardized Regression Coefficients to Lm-Objects 2014. Available online: https://CRAN.R-project.org/package=lm.beta (accessed on 30 May 2022).
- Kassambara, A. rstatix: Pipe-Friendly Framework for Basic Statistical Tests 2021. Available online: https://CRAN.R-project.org/package=rstatix (accessed on 30 May 2022).
- Wilbert, J.; Lueke, T. scan: Single-Case Data Analyses for Single and Multiple Baseline Designs 2021. Available online: https://CRAN.R-project.org/package=scan (accessed on 30 May 2022).
- Leiner, D.J. SoSci Survey 2019. Available online: https://www.soscisurvey.de (accessed on 30 May 2021).
- Ritz, T.; Dahme, B. Die Absorption-Skala: Konzeptuelle Aspekte, psychometrische Kennwerte und Dimensionalität einer deutschsprachigen Adaptation. Diagnostica 1995, 41, 53–61. [Google Scholar]
- Rammstedt, B.; John, O.P. Kurzversion des Big Five Inventory (BFI-K). Diagnostica 2005, 51, 195–206. [Google Scholar] [CrossRef]
- Simons, J.S.; Gaher, R.M. The Distress Tolerance Scale: Development and validation of a self-report measure. Motiv. Emot. 2005, 29, 83–102. [Google Scholar] [CrossRef]
- Keller, J.; Bohner, G.; Erb, H.P. Intuitive und heuristische Urteilsbildung–verschiedene Prozesse? Präsentation einer deutschen Fassung des “Rational-Experiential Inventory“ sowie neuer Selbstberichtskalen zur Heuristiknutzung. Z Soz. 2000, 31, 87–101. [Google Scholar]
- Hupfeld, J.; Ruffieux, N. Validierung einer deutschen Version der Self-Compassion Scale (SCS-D). Z Klin. Psychol. Psychother. 2011, 40, 115–123. [Google Scholar] [CrossRef]
- Büssing, A.; Pilchowska, I.; Baumann, K.; Surzykiewicz, J. Aspects of spirituality in German and Polish adolescents and young adults—Factorial structure of the ASP students’ questionnaire. Religions 2014, 5, 109–125. [Google Scholar] [CrossRef] [Green Version]
- Laux, L.; Glanzmann, P.; Schaffner, P.; Spielberger, C. The State-Trait Anxiety Inventory: Theoretical Foundations and Manual; Beltz Test GmbH: Weinh, Germany, 1981. [Google Scholar]
- Glaesmer, H.; Grande, G.; Braehler, E.; Roth, M. The German version of the Satisfaction with Life Scale (SWLS). Eur. J. Psychol. Assess. 2011, 27, 127–132. [Google Scholar] [CrossRef]
- Puta, M. Promoting health by Sattva-Guna [Internet] [Doctoral dissertation]. [Chemnitz, Germany]: Chemnitz University of Technology. 2015. Available online: http://www.qucosa.de/fileadmin/data/qucosa/documents/22407/Maika_Puta_2015_Promoting_Health_by_Sattva_Guna_mit_Link.pdf (accessed on 24 October 2018).
- Puta, M.; Sedlmeier, P. The concept of tri-guna: A working model. In Meditation: Neuroscientific Approaches and Philosophical Implications Studies in Neuroscience, Consciousness and Spirituality; Schmidt, S., Walach, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 317–364. [Google Scholar]
- Russell, J.A.; Weiss, A.; Mendelsohn, G.A. Affect grid: A single-item scale of pleasure and arousal. J. Pers. Soc. Psychol. 1989, 57, 493–502. [Google Scholar] [CrossRef]
- Matko, K.; Sedlmeier, P.; Bringmann, H.C. Embodied cognition in meditation, yoga, and ethics: An experimental single-case study on differential effects of four treatments. PsyArXiv 2021. Available online: https://psyarxiv.com/kvw34/ (accessed on 28 September 2021).
- Fresco, D.M.; Moore, M.T.; van Dulmen, M.H.; Segal, Z.V.; Ma, S.H.; Teasdale, J.D.; Williams, J.M.G. Initial psychometric properties of the Experiences Questionnaire: Validation of a self-report measure of decentering. Behav. Ther. 2007, 38, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2003, 26, 41–54. [Google Scholar] [CrossRef]
- Mrazek, M.D.; Phillips, D.T.; Franklin, M.S.; Broadway, J.M.; Schooler, J.W. Young and restless: Validation of the Mind-Wandering Questionnaire (MWQ) reveals disruptive impact of mind-wandering for youth. Front. Psychol. 2013, 4, 560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greif, S.; Berg, C. Result-Oriented Self-Reflection: Report on the Construct Validation of Theory-Based Scales. University of Osnabrück: Osnabrück, Germany. 2011. Available online: http://www.home.uniosnabrueck.de/sgreif/english/downloads.html (accessed on 30 May 2021).
- Cohen, S.; Williamson, G.M. Perceived stress in a probability sample of the United States. In The Social Psychology of Health: Claremont Symposium on Applied Social Psychology; Spacapan, S., Oskamp, S., Eds.; Sage: Newsbury Park, CA, USA, 1988; pp. 31–67. [Google Scholar]
- World Health Organization. Info Package: Mastering Depression in Primary Care, 2.2nd ed.; WHO Reg. Off. Eur. Psychiatr. Res. Unit: Copenhagen, DK, 1998; Available online: https://www.euro.who.int/__data/assets/pdf_file/0016/130750/E60246.pdf (accessed on 11 February 2021).
- Robertson, I.H.; Manly, T.; Andrade, J.; Baddeley, B.T.; Yiend, J. Oops!’: Performance correlates of everyday attentional failures in traumatic brain injured and normal subjects. Neuropsychologia 1997, 35, 747–758. [Google Scholar] [CrossRef]
- Anwyl-Irvine, A.L.; Massonnié, J.; Flitton, A.; Kirkham, N.; Evershed, J.K. Gorilla in our midst: An online behavioral experiment builder. Behav. Res. Methods 2020, 52, 388–407. [Google Scholar] [CrossRef] [Green Version]
- Machalicek, W.; Horner, R.H. Special issue on advances in single-case research design and analysis. Dev. Neurorehabilit. 2018, 21, 209–211. [Google Scholar] [CrossRef]
- Shadish, W.R. Analysis and meta-analysis of single-case designs: An introduction. J. Sch. Psychol. 2014, 52, 109–122. [Google Scholar] [CrossRef]
- Parker, R.I.; Vannest, K.J.; Davis, J.L.; Sauber, S.B. Combining nonoverlap and trend for single-case research: Tau-U. Behav. Ther. 2011, 42, 284–299. [Google Scholar] [CrossRef]
- Solomon, B.G.; Howard, T.K.; Stein, B.L. Critical assumptions and distribution features pertaining to contemporary single-case effect sizes. J. Behav. Educ. 2015, 24, 438–458. [Google Scholar] [CrossRef]
- Jamieson, G.A. The modified Tellegen absorption scale: A clearer window on the structure and meaning of absorption. Aust. J. Clin. Exp. Hypnosis 2005, 33, 119–139. [Google Scholar]
- Neff, K.D. The development and validation of a scale to measure self-compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Hölzel, B.K.; Ott, U. Relationships between meditation depth, absorption, meditation practice, and mindfulness: A latent variable approach. J. Transpers. Psychol. 2006, 38, 179–199. [Google Scholar]
- Lifshitz, M.; van Elk, M.; Luhrmann, T.M. Absorption and spiritual experience: A review of evidence and potential mechanisms. Conscious. Cogn. 2019, 73, 102760. [Google Scholar] [CrossRef] [PubMed]
- Berkovich-Ohana, A.; Glicksohn, J. Meditation, absorption, transcendent experience, and affect: Tying it all together via the Consciousness State Space (CSS) model. Mindfulness 2017, 8, 68–77. [Google Scholar] [CrossRef]
- Krick, A.; Felfe, J. Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. J. Occup. Health Psychol. 2020, 25, 99–112. [Google Scholar] [CrossRef]
- Barkan, T.; Hoerger, M.; Gallegos, A.M.; Turiano, N.A.; Duberstein, P.R.; Moynihan, J.A. Personality predicts utilization of Mindfulness-Based Stress Reduction during and post-intervention in a community sample of older adults. J. Altern. Complement. Med. 2016, 22, 390–395. [Google Scholar] [CrossRef] [Green Version]
- Greeson, J.M.; Smoski, M.J.; Suarez, E.C.; Brantley, J.G.; Ekblad, A.G.; Lynch, T.R.; Wolever, R.Q. Decreased symptoms of depression after mindfulness-based stress reduction: Potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. J. Altern. Complement. Med. 2015, 21, 166–174. [Google Scholar] [CrossRef] [Green Version]
- Ratcliff, C.G.; Fowler, S.N.; Sinclair, K.L.; Prinsloo, S.; Chaoul, A.; Zepeda, S.G.; Spelman, A.; Yang, W.T.; Cohen, L. Who benefits most from a brief mindfulness intervention to reduce anxiety during stereotactic breast biopsy: The moderating effect of trait mindfulness, spiritual well-being, and distress tolerance. Mindfulness 2021, 12, 1127–1137. [Google Scholar] [CrossRef]
- Unterrainer, H.F.; Ladenhauf, K.H.; Moazedi, M.L.; Wallner-Liebmann, S.J.; Fink, A. Dimensions of religious/spiritual well-being and their relation to personality and psychological well-being. Personal. Individ. Differ. 2010, 49, 192–197. [Google Scholar] [CrossRef]
- Naragon-Gainey, K.; McMahon, T.P.; Strowger, M.; Lackner, R.; Seah, T.; Moore, M.T.; Fresco, D.M. A comparison of decentering across demographic groups and meditation experience: Support for the measurement invariance of the Experiences Questionnaire. Psychol. Assess. 2020, 32, 197–204. [Google Scholar] [CrossRef]
- Strohmaier, S. The relationship between doses of mindfulness-based programs and depression, anxiety, stress, and mindfulness: A dose-response meta-regression of randomized controlled trials. Mindfulness 2020, 11, 1315–1335. [Google Scholar] [CrossRef]
- Kobylińska, D.; Lewczuk, K.; Marchlewska, M.; Pietraszek, A. For body and mind: Practicing yoga and emotion regulation. Soc. Psychol. Bull. 2018, 13, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Smillie, L.D.; DeYoung, C.G.; Hall, P.J. Clarifying the relation between extraversion and positive affect. J. Pers. 2015, 83, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Gawrysiak, M.J.; Leong, S.H.; Grassetti, S.N.; Wai, M.; Shorey, R.C.; Baime, M.J. Dimensions of distress tolerance and the moderating effects on mindfulness-based stress reduction. Anxiety Stress Coping 2016, 29, 552–560. [Google Scholar] [CrossRef]
- Franquesa, A.; Cebolla, A.; García-Campayo, J.; Demarzo, M.; Elices, M.; Pascual, J.C.; Soler, J. Meditation practice is associated with a values-oriented life: The mediating role of decentering and mindfulness. Mindfulness 2017, 8, 1259–1268. [Google Scholar] [CrossRef] [Green Version]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change, 2nd ed.; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Gard, T.; Noggle, J.J.; Park, C.L.; Vago, D.R.; Wilson, A. Potential self-regulatory mechanisms of yoga for psychological health. Front. Hum. Neurosci. 2014, 8, 770. [Google Scholar] [CrossRef] [Green Version]
- Brandmeyer, T.; Delorme, A. Meditation and the wandering mind: A theoretical framework of underlying neurocognitive mechanisms. Perspect. Psychol. Sci. 2021, 16, 39–66. [Google Scholar] [CrossRef]
- Saoji, A.A.; Raghavendra, B.R.; Madle, K.; Manjunath, N.K. Additional practice of yoga breathing with intermittent breath holding enhances psychological functions in yoga practitioners: A randomized controlled trial. EXPLORE 2018, 14, 379–384. [Google Scholar] [CrossRef]
- Mrazek, M.D.; Smallwood, J.; Schooler, J.W. Mindfulness and mind-wandering: Finding convergence through opposing constructs. Emotion 2012, 12, 442. [Google Scholar] [CrossRef]
- Riley, K.E.; Park, C.L. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol. Rev. 2015, 9, 379–396. [Google Scholar] [CrossRef]
- Tellhed, U.; Daukantaitė, D.; Maddux, R.E.; Svensson, T.; Melander, O. Yogic breathing and mindfulness as stress coping mediate positive health outcomes of yoga. Mindfulness 2019, 10, 2703–2715. [Google Scholar] [CrossRef] [Green Version]
- Sierpina, V.; Levine, R.; Astin, J.; Tan, A. Use of mind-body therapies in psychiatry and family medicine faculty and residents: Attitudes, barriers, and gender differences. EXPLORE 2007, 3, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Chaieb, L.; Hoppe, C.; Fell, J. Mind wandering and depression: A status report. Neurosci. Biobehav. Rev. 2022, 133, 104505. [Google Scholar] [CrossRef] [PubMed]
- Smyth, J.M.; Arigo, D. Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Curr. Opin. Psychiatry 2009, 22, 205–210. [Google Scholar] [CrossRef] [PubMed]
- ter Avest, M.J.; Dusseldorp, E.; Huijbers, M.J.; van Aalderen, J.R.; Cladder-Micus, M.B.; Spinhoven, P.; Greven, C.U.; Speckens, A.E. Added value of Mindfulness-Based Cognitive Therapy for depression: A tree-based qualitative interaction analysis. Behav. Res. Ther. 2019, 122, 103467. [Google Scholar] [CrossRef]
- Braun, S.E.; Deeb, G.; Carrico, C.; Kinser, P.A. Brief yoga intervention for dental and dental hygiene students: A feasibility and acceptability study. J. Evid.-Based Integr. Med. 2019, 24, 2515690X19855303. [Google Scholar] [CrossRef] [Green Version]
- Bringmann, H.C.; Michalsen, A.; Jeitler, M.; Kessler, C.S.; Brinkhaus, B.; Brunnhuber, S.; Sedlmeier, P. Meditation-based lifestyle modification in mild to moderate depression—A randomized controlled trial. Depress Anxiety 2022, 39, 363–375. [Google Scholar] [CrossRef]
- Gross, J.J.; Muñoz, R.F. Emotion regulation and mental health. Clin. Psychol. Sci. Pract. 1995, 2, 151–164. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Menezes, C.B.; Dalpiaz, N.R.; Kiesow, L.G.; Sperb, W.; Hertzberg, J.; Oliveira, A.A. Yoga and emotion regulation: A review of primary psychological outcomes and their physiological correlates. Psychol. Neurosci. 2015, 8, 82–101. [Google Scholar] [CrossRef]
- Goldin, P.R.; Gross, J.J. Effects of Mindfulness-Based Stress Reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion 2010, 10, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Chambers, R.; Gullone, E.; Allen, N.B. Mindful emotion regulation: An integrative review. Clin. Psychol. Rev. 2009, 29, 560–572. [Google Scholar] [CrossRef] [PubMed]
- Iani, L.; Lauriola, M.; Chiesa, A.; Cafaro, V. Associations between mindfulness and emotion regulation: The key role of describing and nonreactivity. Mindfulness 2019, 10, 366–375. [Google Scholar] [CrossRef]
- Price, C.J.; Hooven, C. Interoceptive awareness skills for emotion regulation: Theory and approach of Mindful Awareness in Body-Oriented Therapy (MABT). Front. Psychol. 2018, 9, 798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlson, L.E.; Tamagawa, R.; Stephen, J.; Doll, R.; Faris, P.; Dirkse, D.; Speca, M. Tailoring mind-body therapies to individual needs: Patients’ program preference and psychological traits as moderators of the effects of mindfulness-based cancer recovery and supportive-expressive therapy in distressed breast cancer survivors. JNCI Monogr. 2014, 2014, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Brakemeier, E.-L.; Herpertz, S.C. Innovative Psychotherapieforschung: Auf dem Weg zu einer evidenz- und prozessbasierten individualisierten und modularen Psychotherapie. Nervenarzt 2019, 90, 1125–1134. [Google Scholar] [CrossRef] [Green Version]
| Our Sample | Comparative Sample | ||||
|---|---|---|---|---|---|
| Variable | M | SD | M | SD | Source |
| Absorption | 3.20 | 0.67 | 2.92 | 0.64 | Jamieson, 2005 [64] |
| Agreeableness | 3.11 | 0.79 | 3.02 | 0.73 | Rammstedt & John, 2005 (Study 1) [41] |
| Anxiety | 2.69 | 0.67 | 2.05 | 0.47 | Laux et al., 1981 [46] |
| Conscientiousness | 3.57 | 0.58 | 3.53 | 0.69 | Rammstedt & John, 2005 (Study 1) [41] |
| Distress tolerance | 3.41 | 0.73 | 3.43 | 0.76 | Simons & Gaher, 2005 [42] |
| Extraversion | 3.24 | 1.03 | 3.48 | 0.87 | Rammstedt & John, 2005 (Study 1) [41] |
| Life satisfaction | 4.89 | 1.22 | 4.98 | 1.25 | Glaesmer et al., 2011 [47] |
| Need for cognition | 3.70 | 0.77 | 3.76 | n.a. | Keller et al., 2000 [43] |
| Neuroticism | 3.22 | 0.93 | 2.88 | 0.77 | Rammstedt & John, 2005 (Study 1) [41] |
| Openness | 4.14 | 0.67 | 3.96 | 0.62 | Rammstedt & John, 2005 (Study 1) [41] |
| Sattva proportion | 0.40 | 0.06 | n.a. | n.a. | n.a. |
| Self-compassion | 2.99 | 0.59 | 3.04 | 0.63 | Neff, 2003 [65] |
| Spirituality | 3.18 | 0.66 | n.a. | n.a. | n.a. |
| Attention | Arousal | Body Awareness | Decentering | Emotion Regulation | Mind-Wandering | Self-Reflection | Stress | Valence | Wellbeing | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ethical education (y/n) | −0.07 | −0.17 | −0.12 | −0.21 | 0.15 | −0.01 | 0.12 | −0.02 | 0.40 ° | 0.61 ** |
| Physical yoga (y/n) | −0.20 | −0.12 | 0.30 | 0.15 | 0.11 | −0.47 * | −0.11 | −0.11 | 0.05 | 0.30 |
| Absorption | −0.36 | 0.18 | 0.57 ° | 0.42 ° | 0.19 | −0.60 * | −0.01 | −0.13 | 0.02 | 0.61 * |
| Agreeableness | 0.61 ° | −0.11 | −0.21 | −0.27 | −0.26 | 0.18 | 0.16 | 0.07 | −0.59 ° | 0.17 |
| Anxiety | 1.11 | −0.15 | −0.09 | 0.92 * | 0.72 ° | −0.08 | 0.21 | −0.06 | 0.40 | −0.08 |
| Conscientiousness | −0.80 | −0.07 | −0.04 | −0.38 ° | −0.28 | 0.15 | −0.23 | 0.27 | −0.01 | −0.31 |
| Distress tolerance | −0.24 | 0.15 | 0.08 | 0.01 | 0.18 | 0.07 | −0.01 | 0.20 | 0.23 | −0.13 |
| Extraversion | −0.41 | 0.63 * | −0.05 | 0.05 | −0.22 | −0.03 | 0.24 | 0.33 | 0.04 | −0.25 |
| Life satisfaction | 0.41 | −0.66 * | −0.23 | 0.42 | 0.08 | −0.09 | 0.24 | −0.26 | 0.18 | 0.30 |
| Need for cognition | 0.84 | −0.43 ° | 0.11 | 0.01 | 0.19 | −0.24 | 0.33 | −0.18 | −0.18 | 0.28 |
| Neuroticism | −0.97 ° | 0.40 | 0.10 | −0.20 | 0.02 | −0.48 | −0.06 | 0.22 | 0.08 | 0.41 |
| Openness | −0.79 ° | −0.25 | −0.39 | −0.54 * | −0.07 | 0.27 | −0.47 | 0.13 | 0.29 | 0.08 |
| Sattva proportion | 0.67 | 0.74 ° | 0.54 | 1.07 ** | 0.54 | −0.35 | −0.34 | −0.07 | 0.37 | 0.47 |
| Self-compassion | −0.41 | −0.37 | −0.38 | 0.08 | −0.42 ° | 0.02 | −0.08 | 0.05 | −0.03 | −0.07 |
| Spirituality | 0.52 | −0.46 | −0.29 | −0.46 ° | −0.41 | 0.68 * | 0.31 | 0.09 | −0.44 | −0.83 ** |
| Age | 0.37 | −0.47 ° | −0.46 | −0.46 * | −0.25 | 0.31 | −0.03 | 0.13 | −0.13 | −0.51 * |
| Baseline | 0.13 | −0.29 | 0.04 | −0.09 | −0.30 | 0.47 * | 0.00 | −0.01 | −0.22 | −0.01 |
| Gender (male) | 0.03 | −0.07 | −0.15 | −0.37 ° | −0.18 | 0.19 | 0.03 | 0.41 | −0.20 | −0.21 |
| Occupation (employed) | −0.62 | 0.40 | 0.46 | 0.05 | −0.09 | −0.08 | −0.02 | 0.11 | 0.04 | 0.09 |
| Total practice time | −0.11 | 0.20 | 0.06 | −0.08 | 0.02 | 0.15 | 0.19 | −0.08 | −0.06 | −0.51 * |
| df | 13 | 21 | 21 | 21 | 18 | 21 | 20 | 21 | 21 | 21 |
| R2 | 0.53 | 0.62 | 0.32 | 0.70 | 0.72 | 0.51 | 0.44 | 0.20 | 0.26 | 0.60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matko, K.; Berghöfer, A.; Jeitler, M.; Sedlmeier, P.; Bringmann, H.C. Who Benefits Most? Interactions between Personality Traits and Outcomes of Four Incremental Meditation and Yoga Treatments. J. Clin. Med. 2022, 11, 4553. https://doi.org/10.3390/jcm11154553
Matko K, Berghöfer A, Jeitler M, Sedlmeier P, Bringmann HC. Who Benefits Most? Interactions between Personality Traits and Outcomes of Four Incremental Meditation and Yoga Treatments. Journal of Clinical Medicine. 2022; 11(15):4553. https://doi.org/10.3390/jcm11154553
Chicago/Turabian StyleMatko, Karin, Anne Berghöfer, Michael Jeitler, Peter Sedlmeier, and Holger C. Bringmann. 2022. "Who Benefits Most? Interactions between Personality Traits and Outcomes of Four Incremental Meditation and Yoga Treatments" Journal of Clinical Medicine 11, no. 15: 4553. https://doi.org/10.3390/jcm11154553
APA StyleMatko, K., Berghöfer, A., Jeitler, M., Sedlmeier, P., & Bringmann, H. C. (2022). Who Benefits Most? Interactions between Personality Traits and Outcomes of Four Incremental Meditation and Yoga Treatments. Journal of Clinical Medicine, 11(15), 4553. https://doi.org/10.3390/jcm11154553








