Outcomes and Prognostic Factors Following Pars Plana Vitrectomy for Intraocular Foreign Bodies—11-Year Retrospective Analysis in a Tertiary Care Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Treatment
2.3. Statistical Analysis
3. Results
3.1. Demographic Results
3.2. IOFB Characteristics
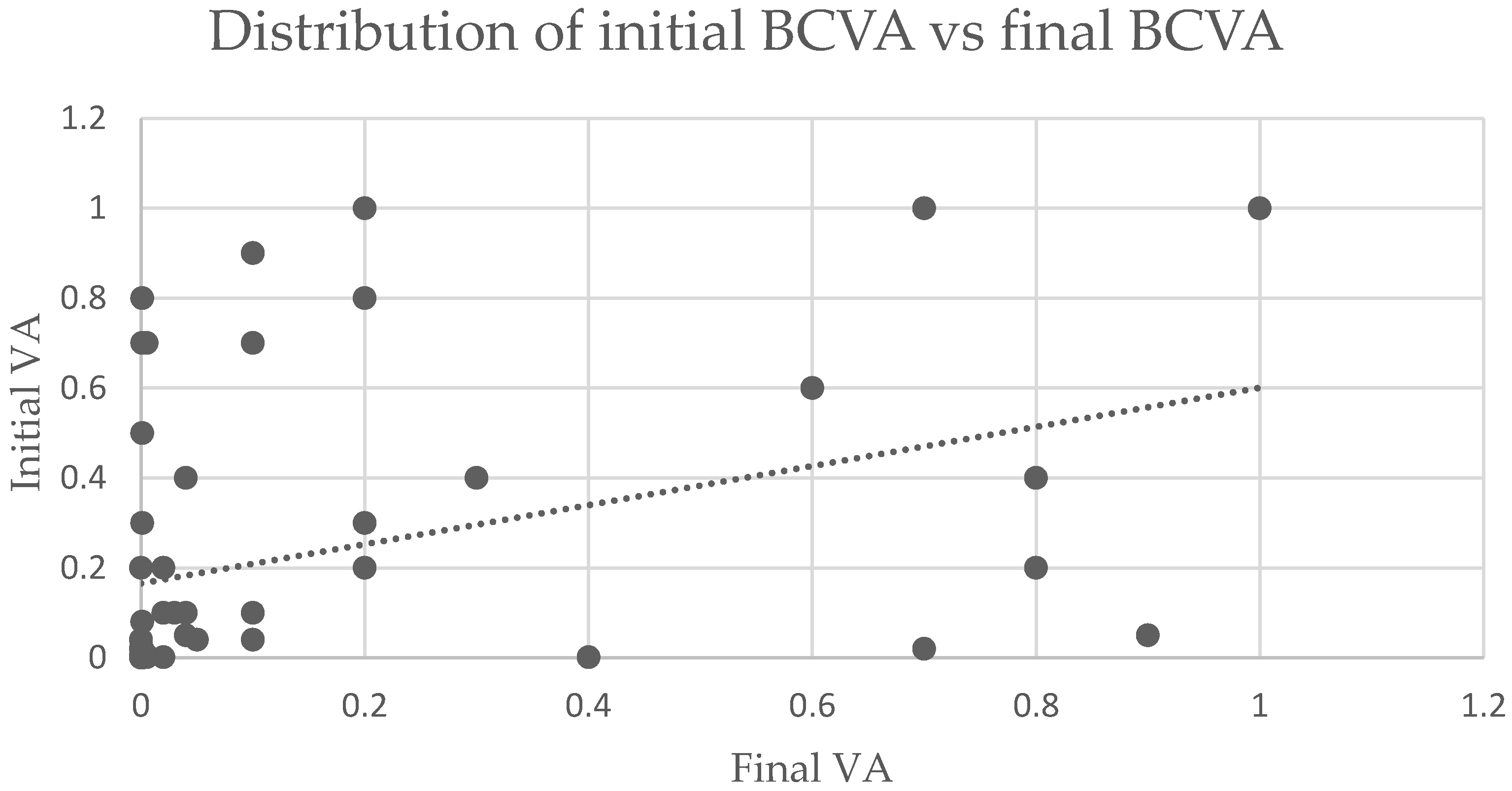
3.3. Initial BCVA, Visual Outcome and Prognostic Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nicoară, S.D.; Irimescu, I.; Călinici, T.; Cristian, C. Intraocular foreign bodies extracted by pars plana vitrectomy: Clinical characteristics, management, outcomes and prognostic factors. BMC Ophthalmol. 2015, 15, 151. [Google Scholar] [CrossRef] [PubMed]
- Négrel, A.D.; Thylefors, B. The global impact of eye injuries. Ophthalmic. Epidemiol. 1998, 5, 143–169. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.T.; Parver, L.M.; Enger, C.L.; Mieler, W.F.; Liggett, P.E. Infectious Endophthalmitis after Penetrating Injuries with Retained Intraocular Foreign Bodies. Ophthalmology 1993, 100, 1468–1474. [Google Scholar] [CrossRef]
- Thompson, W.S.; Rubsamen, P.E.; Flynn, H.W.; Schiffman, J.; Cousins, S.W. Endophthalmitis after Penetrating Trauma: Risk Factors and Visual Acuity Outcomes. Ophthalmology 1995, 102, 1696–1701. [Google Scholar] [CrossRef]
- Yeh, S.; Colyer, M.H.; Weichel, E.D. Current trends in the management of intraocular foreign bodies. Curr. Opin. Ophthalmol. 2008, 19, 225–233. [Google Scholar] [CrossRef]
- Liu, C.C.H.; Tong, J.M.K.; Li, P.S.H.; Li, K.K.W. Epidemiology and clinical outcome of intraocular foreign bodies in Hong Kong: A 13-year review. Int. Ophthalmol. 2017, 37, 55–61. [Google Scholar] [CrossRef]
- Sternberg, P.; De Juan, E.; Michels, R.G.; Auer, C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am. J. Ophthalmol. 1984, 98, 467–472. [Google Scholar] [CrossRef]
- Abu El-Asrar, A.M.; Al-Amro, S.A.; Khan, N.M.; Kangave, D. Retinal detachment after posterior segment intraocular foreign body injuries. Int. Ophthalmol. 1998, 22, 369–375. [Google Scholar] [CrossRef]
- Gao, Y.Z.; Zhang, Y.F.; Zhang, M.; Xu, H.Y.; Jin, X.R. Clinical characteristics and prognostic factors for visual outcome in 669 patients with intraocular foreign bodies. Int. J. Ophthalmol. 2021, 14, 759–765. [Google Scholar] [CrossRef]
- Ahmed, Y.; Schimel, A.M.; Pathengay, A.; Colyer, M.H.; Flynn, H.W. Endophthalmitis following open-globe injuries. Eye 2012, 26, 212–217. [Google Scholar] [CrossRef]
- Colyer, M.H.; Weber, E.D.; Weichel, E.D.; Dick, J.S.; Bower, K.S.; Ward, T.P.; Haller, J.A. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology 2007, 114, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- Greven, C.M.; Engelbrecht, N.E.; Slusher, M.M.; Nagy, S.S. Intraocular foreign bodies: Management, prognostic factors, and visual outcomes. Ophthalmology 2000, 107, 608–612. [Google Scholar] [CrossRef]
- Justin, G.A.; Baker, K.M.; Brooks, D.I.; Ryan, D.S.; Weichel, E.D.; Colyer, M.H. Intraocular Foreign Body Trauma in Operation Iraqi Freedom and Operation Enduring Freedom: 2001 to 2011. Ophthalmology 2018, 125, 1675–1682. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.L.; Kung, Y.H.; Hsu, P.S.; Wu, T.T. Surgical outcomes of the removal of posterior segment metallic intraocular foreign bodies. BMC Ophthalmol. 2020, 20, 267. [Google Scholar] [CrossRef]
- Williams, D.F.; Mieler, W.F.; Abrams, G.W.; Lewis, H. Results and Prognostic Factors in Penetrating Ocular Injuries with Retained Intraocular Foreign Bodies. Ophthalmology 1988, 95, 911–916. [Google Scholar] [CrossRef]
- Wani, V.B.; Al-Ajmi, M.; Thalib, L.; Azad, R.V.; Abul, M.; Al-Ghanim, M.; Sabti, K. Vitrectomy for posterior segment intraocular foreign bodies: Visual Results and Prognostic Factors. Retina 2003, 23, 654–660. [Google Scholar] [CrossRef]
- Yuksel, K.; Celik, U.; Alagoz, C.; Dundar, H.; Celik, B.; Yazlcl, A.T. 23 Gauge pars plana vitrectomy for the removal of retained intraocular foreign bodies. BMC Ophthalmol. 2015, 15, 75. [Google Scholar] [CrossRef]
- Liang, Y.; Liang, S.; Liu, X.; Liu, D.; Duan, J. Intraocular Foreign Bodies: Clinical Characteristics and Factors Affecting Visual Outcome. J. Ophthalmol. 2021, 2021, 9933403. [Google Scholar] [CrossRef]
- Woodcock, M.G.L.; Scott, R.A.H.; Huntbach, J.; Kirkby, G.R. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology 2006, 113, 2262–2269. [Google Scholar] [CrossRef]
- Choovuthayakorn, J.; Hansapinyo, L.; Ittipunkul, N.; Patikulsila, D.; Kunavisarut, P. Predictive factors and outcomes of posterior segment intraocular foreign bodies. Eye 2011, 25, 1622–1626. [Google Scholar] [CrossRef][Green Version]
- Kuhn, F.; Maisiak, R.; Mann, L.R.; Mester, V.; Morris, R.; Witherspoon, C.D. The ocular trauma score (OTS). Ophthalmol. Clin. N. Am. 2002, 15, 163–165. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, S.; Li, Y.; Gong, Q.; Su, G.; Zhao, J. Intraocular Foreign Bodies: Clinical Characteristics and Prognostic Factors Influencing Visual Outcome and Globe Survival in 373 Eyes. J. Ophthalmol. 2019, 2019, 5208092. [Google Scholar] [CrossRef] [PubMed]
- Mangione, C.M.; Lee, P.P.; Gutierrez, P.R.; Spritzer, K.; Coleman, A.L. Development of the 25-item National Eye Institute visual function questionnaire. Evid.-Based Eye Care 2002, 3, 58–59. [Google Scholar] [CrossRef] [PubMed]
- Yüksel, H.; Türkcü, F.M.; Ahin, M.; Cinar, Y.; Cingü, A.K.; Ozkurt, Z.; Bez, Y.; Caça, H. Vision-related quality of life in patients after ocular penetrating injuries. Arq. Bras. Oftalmol. 2014, 77, 95–98. [Google Scholar] [CrossRef]
- Schrader, W.F. Open globe injuries: Epidemiological study of two eye clinics in Germany, 1981–1999. Croat. Med. J. 2004, 45, 268–274. [Google Scholar]
- Jung, H.C.; Lee, S.Y.; Yoon, C.K.; Park, U.C.; Heo, J.W.; Lee, E.K. Intraocular foreign body: Diagnostic protocols and treatment strategies in ocular trauma patients. J. Clin. Med. 2021, 10, 1861. [Google Scholar] [CrossRef]
- Ma, J.; Wang, Y.; Zhang, L.; Chen, M.; Ai, J.; Fang, X. Clinical characteristics and prognostic factors of posterior segment intraocular foreign body in a tertiary hospital. BMC Ophthalmol. 2019, 19, 17. [Google Scholar] [CrossRef]
- Anguita, R.; Moya, R.; Saez, V.; Bhardwaj, G.; Salinas, A.; Kobus, R.; Nazar, C.; Manriquez, R.; Charteris, D.G. Clinical presentations and surgical outcomes of intraocular foreign body presenting to an ocular trauma unit. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 263–268. [Google Scholar] [CrossRef]
- Andreoli, M.T.; Andreoli, C.M. Geriatric traumatic open globe injuries. Ophthalmology 2011, 118, 156–159. [Google Scholar] [CrossRef]
- Jonas, J.B.; Budde, W.M. Early versus late removal of retained intraocular foreign bodies. Retina 1999, 19, 193–197. [Google Scholar] [CrossRef]
- Jonas, J.B.; Knorr, H.L.J.; Budde, W.M. Prognostic factors inocular injuries caused byintraocular or retrobulbar foreign bodies. Evid. -Based Eye Care 2000, 1, 278–279. [Google Scholar] [CrossRef]
- De Souza, S.; Howcroft, M.J. Management of posterior segment intraocular foreign bodies: 14 years’ experience. Can. J. Ophthalmol. 1999, 34, 23–29. [Google Scholar] [PubMed]
- Kuhn, F.; Schrader, W. Prophylactic Chorioretinectomy for Eye Injuries With High Proliferative-Vitreoretinopathy Risk. Clin Anat. 2018, 1, 28–38. [Google Scholar] [CrossRef]
- Han, S.B.; Yu, H.G. Visual outcome after open globe injury and its predictive factors in korea. J. Trauma 2010, 69, E66–E72. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, M.; Jiang, C.; Qiu, H.Y. Intraocular foreign bodies in China: Clinical characteristics, prognostic factors, and visual outcomes in 1421 eyes. Am. J. Ophthalmol. 2011, 152, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Albert, D.M.; Miller, J.W.; Azar, D.T. Albert & Jakobiec’s Principles and Practice of Ophthalmology, 3rd ed.; Saunders Elsevier: Philadelphia, PA, USA, 2008. [Google Scholar]
- Brodowska, K.; Stryjewski, T.P.; Papavasileiou, E.; Chee, Y.E.; Eliott, D. Validation of the Retinal Detachment after Open Globe Injury (RD-OGI) Score as an Effective Tool for Predicting Retinal Detachment. Ophthalmology 2017, 124, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Colyer, M.H.; Chun, D.W.; Bower, K.S.; Dick, J.S.B.; Weichel, E.D. Perforating Globe Injuries during Operation Iraqi Freedom. Ophthalmology 2008, 115, 2087–2093. [Google Scholar] [CrossRef]
- Cardillo, J.A.; Stout, J.T.; LaBree, L.; Azen, S.P.; Omphroy, L.; Cui, J.Z.; Kimura, H.; Hinton, D.R.; Ryan, S.J. Post-traumatic proliferative vitreoretinopathy: The epidemiologic profile, onset, risk factors, and visual outcome. Ophthalmology 1997, 104, 1166–1173. [Google Scholar] [CrossRef]
- Assi, A.; Khoueir, Z.; Helou, C.; Fakhoury, H.; Cherfan, G. Intraocular application of Mitomycin C to prevent proliferative vitreoretinopathy in perforating and severe intraocular foreign body injuries. Eye 2019, 33, 1261–1270. [Google Scholar] [CrossRef]
- Amarnani, D.; Machuca-Parra, A.I.; Wong, L.L.; Marko, C.K.; Stefater, J.A.; Stryjewski, T.P.; Eliott, D.; Arboleda-Velasquez, J.F.; Kim, L.A. Effect of Methotrexate on an In Vitro Patient-Derived Model of Proliferative Vitreoretinopathy. Invest. Ophthalmol. Vis. Sci. 2017, 58, 3940–3949. [Google Scholar] [CrossRef]
- Kuhn, F.; Morris, R.; Witherspoon, C.D.; Mann, L. Blunt-force injuries involving the posterior segment. Retin. Physician 2007, 20, 4. [Google Scholar]
- Ferreira, N.; Monteiro, S.; Meireles, A.; Kuhn, F. Outcome of Vitrectomy and Chorioretinectomy in Perforating. Ophthalmic Res. 2015, 53, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Ozdek, S.; Hasanreisoglu, M.; Yuksel, E. Chorioretinectomy for perforating eye injuries. Eye 2013, 27, 722–727. [Google Scholar] [CrossRef] [PubMed]

| Variable | BCVA < 0.1 | BCVA 0.1–<0.5 | BCVA ≥ 0.5 | p Value |
|---|---|---|---|---|
| Age | 35.5 (25.5; 47) | 39 (23; 50) | 32 (27; 43) | 0.809 |
| Gender | ||||
| Female | 1 (3.3%) | 0 (0%) | 0 (0%) | 0.643 |
| Male | 29 (96.7%) | 15 (100%) | 11 (100%) | |
| Eye | ||||
| Right | 12 (40%) | 7 (46.6%) | 5 (45.5%) | 0.697 |
| Left | 18 (60%) | 8 (53.3%) | 6 (54.5%) | |
| Eye protection | ||||
| Yes | - | - | - | |
| No | 30 (100%) | 15 (100%) | 11 (100%) | |
| Location | ||||
| Rural | 24 (80.0%) | 10 (66.7%) | 6 (54.5%) | 0.249 |
| Urban | 6 (20%) | 5 (33.3%) | 5 (45.5%) | |
| Type of accident | ||||
| Work | 2 (6.7%) | 1 (6.7%) | 1 (9.1%) | 0.962 |
| Daily life | 28 (93.3%) | 14 (93.3%) | 10 (90.9%) |
| Factor | Nr. Eyes | BCVA < 0.1 | BCVA 0.1- < 0.5 | BCVA ≥ 0.5 | p-Value |
|---|---|---|---|---|---|
| Age | |||||
| ≤50 years | 47 (83.9%) | 24 (80%) | 12 (80%) | 11 (100%) | 0.270 |
| >50 years | 9 (16.1%) | 6 (20%) | 3 (20%) | 0 (0%) | |
| IOFB location | |||||
| Retina | 27 (48.2%) | 19 (66.3%) | 4 (26.7%) | 4 (36.4%) | 0.046 |
| Vitreous | 29 (51.8%) | 11 (36.7%) | 11 (73.3%) | 7 (63.6%) | |
| Entry site | |||||
| Cornea | 38 (67.8%) | 29 (63.3%) | 11 (73.4%) | 8 (72.7%) | 0.932 |
| Sclera <5 mm | 7 (12.5%) | 4 (13.3%) | 2 (13.3%) | 1 (9.1%) | |
| Sclera >5 mm | 11 (19.7%) | 7 (23.4%) | 2 (13.3%) | 2 (18.2%) | |
| Endophthalmitis | |||||
| Yes | 17 (30.4%) | 13 (43.3%) | 1 (6.7%) | 3 (27.3%) | 0.040 |
| No | 39 (69.6%) | 17 (56.7%) | 14 (93.3%) | 8 (72.7%) | |
| RD at presentation | |||||
| Yes | 12 (21.4%) | 11 (36.6%) | 1 (6.7%) | 0 (0%) | 0.010 |
| No | 44 (78.6%) | 19 (63.3%) | 14 (93.3%) | 11 (100%) | |
| Lens Injury | |||||
| Yes | 36 (64.3%) | 19 (63.3%) | 10 (66.7%) | 7 (63.6%) | 0.974 |
| No | 20 (35.7%) | 11 (36.7%) | 5 (33.3%) | 4 (36.4%) | |
| Initial VA | |||||
| <0.1 | 38 (67.9%) | 26 (86.7%) | 8 (53.3%) | 4 (36.4%) | 0.018 |
| 0.1–<0.5 | 11 (19.6%) | 2 (6.7%) | 5 (33.3%) | 4 (36.4%) | |
| ≥0.5 | 7 (12.5%) | 2 (6.7%) | 2 (13.3%) | 3 (27.3%) | |
| IOFB size | |||||
| ≤3 mm | 26 (46.4%) | 10 (33.3%) | 9 (60%) | 7 (63.6%) | 0.105 |
| >3 mm | 30 (53.6%) | 20 (66.7%) | 6 (40%) | 4 (36.3%) | |
| IOFB type | |||||
| Metallic | 54 (96.4%) | 29 (96.7%) | 14 (93.3%) | 11 (100%) | 0.660 |
| Nonmetallic | 2 (3.6%) | 1 (3.3%) | 1 (6.7%) | 0 (0%) | |
| IOFB time extraction | |||||
| <48 h | 30 (53.6%) | 13 (43.3%) | 9 (60%) | 8 (72.7%) | 0.208 |
| >48 h | 26 (46.4%) | 17 (56.7%) | 6 (40%) | 3 (27.3%) |
| Variable | Number of Eyes with IOFB |
|---|---|
| IOFB initially retrieved | 53 (94.6%) |
| Number of hospitalization days 1st admission | 8.16 ± 5.61 |
| Primary surgical procedures performed | |
| PPV with IOFB extraction | 53 (94.6%) |
| Lensectomy | 25 (44.6%) |
| Phacoemulsification | 3 (5.4%) |
| Suture of wound | 25 (44.6%) |
| Intravitreal antibiotic injection | 12 (21.4%) |
| Laser of retinal impact site | 24 (42.9%) |
| Additional surgical procedures performed | |
| PPV | 21 (37.5%) |
| Phacoemulsification | 5 (8.9%) |
| IOL implantation | 12 (21.4%) |
| Intravitreal antibiotic injection | 5 (8.9%) |
| Number of surgical procedures performed | 2.14 ± 1.25 |
| RD—Overall | RD—Postoperative | ||||||
|---|---|---|---|---|---|---|---|
| Factor | Yes | No | p Value | Factor | Yes | No | p Value |
| Age | Age | ||||||
| ≤50 years (n = 47) | 19(39.6%) | 28(60.4%) | 0.40 | ≤50 years (n = 37) | 9(24.3%) | 28 (75.7%) | 0.34 |
| >50 years (n = 9) | 5 (55.6%) | 4 (44.4%) | >50 years (n = 7) | 3 (42.9%) | 4 (57.1%) | ||
| Endophthalmitis | Endophthalmitis | ||||||
| Yes (n = 17) | 10(58.8%) | 7 (41.2%) | 0.11 | Yes (n = 12) | 5 (41.7%) | 7 (58.3%) | 0.18 |
| No (n = 39) | 14(35.9%) | 25(64.1%) | No (n = 32) | 7 (21.9%) | 25 (78.1%) | ||
| IOFB size | IOFB size | ||||||
| ≤3 mm (n = 26) | 7 (26.9%) | 19(73.1%) | 0.02 | ≤3 mm (n = 24) | 5 (20.8%) | 19 (79.2%) | 0.29 |
| >3 mm (n = 30) | 17(56.7%) | 13(43.3%) | >3 mm (n = 20) | 7 (35.0%) | 13 (65.0%) | ||
| IOFB location | IOFB location | ||||||
| Retina (n = 27) | 18(66.7%) | 9 (33.3%) | 0.000 | Retina (n = 18) | 9(50%) | 9 (50%) | 0.004 |
| Vitreous (n = 29) | 6 (20.7%) | 23(79.3%) | Vitreous (n = 26) | 3 (11.5%) | 23 (88.5%) | ||
| IOFB entry site | IOFB entry site | ||||||
| Zone I (n = 38) | 14(35.9%) | 24 (64.1%) | 0.28 | Zone I (n = 32) | 8 (25%) | 24 (75%) | 0.85 |
| Zone II (n = 7) | 3 (42.9%) | 4 (57.1%) | Zone II (n = 6) | 2 (33.3%) | 4 (66.7%) | ||
| Zone III (n = 11) | 7 (63.6%) | 4 (36.4%) | Zone III (n = 6) | 2 (33.3%) | 4 (66.7%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hapca, M.C.; Muntean, G.A.; Drăgan, I.A.N.; Vesa, Ș.C.; Nicoară, S.D. Outcomes and Prognostic Factors Following Pars Plana Vitrectomy for Intraocular Foreign Bodies—11-Year Retrospective Analysis in a Tertiary Care Center. J. Clin. Med. 2022, 11, 4482. https://doi.org/10.3390/jcm11154482
Hapca MC, Muntean GA, Drăgan IAN, Vesa ȘC, Nicoară SD. Outcomes and Prognostic Factors Following Pars Plana Vitrectomy for Intraocular Foreign Bodies—11-Year Retrospective Analysis in a Tertiary Care Center. Journal of Clinical Medicine. 2022; 11(15):4482. https://doi.org/10.3390/jcm11154482
Chicago/Turabian StyleHapca, Mădălina Claudia, George Adrian Muntean, Iulia Andrada Nemeș Drăgan, Ștefan Cristian Vesa, and Simona Delia Nicoară. 2022. "Outcomes and Prognostic Factors Following Pars Plana Vitrectomy for Intraocular Foreign Bodies—11-Year Retrospective Analysis in a Tertiary Care Center" Journal of Clinical Medicine 11, no. 15: 4482. https://doi.org/10.3390/jcm11154482
APA StyleHapca, M. C., Muntean, G. A., Drăgan, I. A. N., Vesa, Ș. C., & Nicoară, S. D. (2022). Outcomes and Prognostic Factors Following Pars Plana Vitrectomy for Intraocular Foreign Bodies—11-Year Retrospective Analysis in a Tertiary Care Center. Journal of Clinical Medicine, 11(15), 4482. https://doi.org/10.3390/jcm11154482








