Comparative Analysis of Neurodegeneration and Axonal Dysfunction Biomarkers in the Cerebrospinal Fluid of Patients with Multiple Sclerosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population—Clinical Assessment
2.2. Biomarker Analysis
2.3. Statistical Analysis
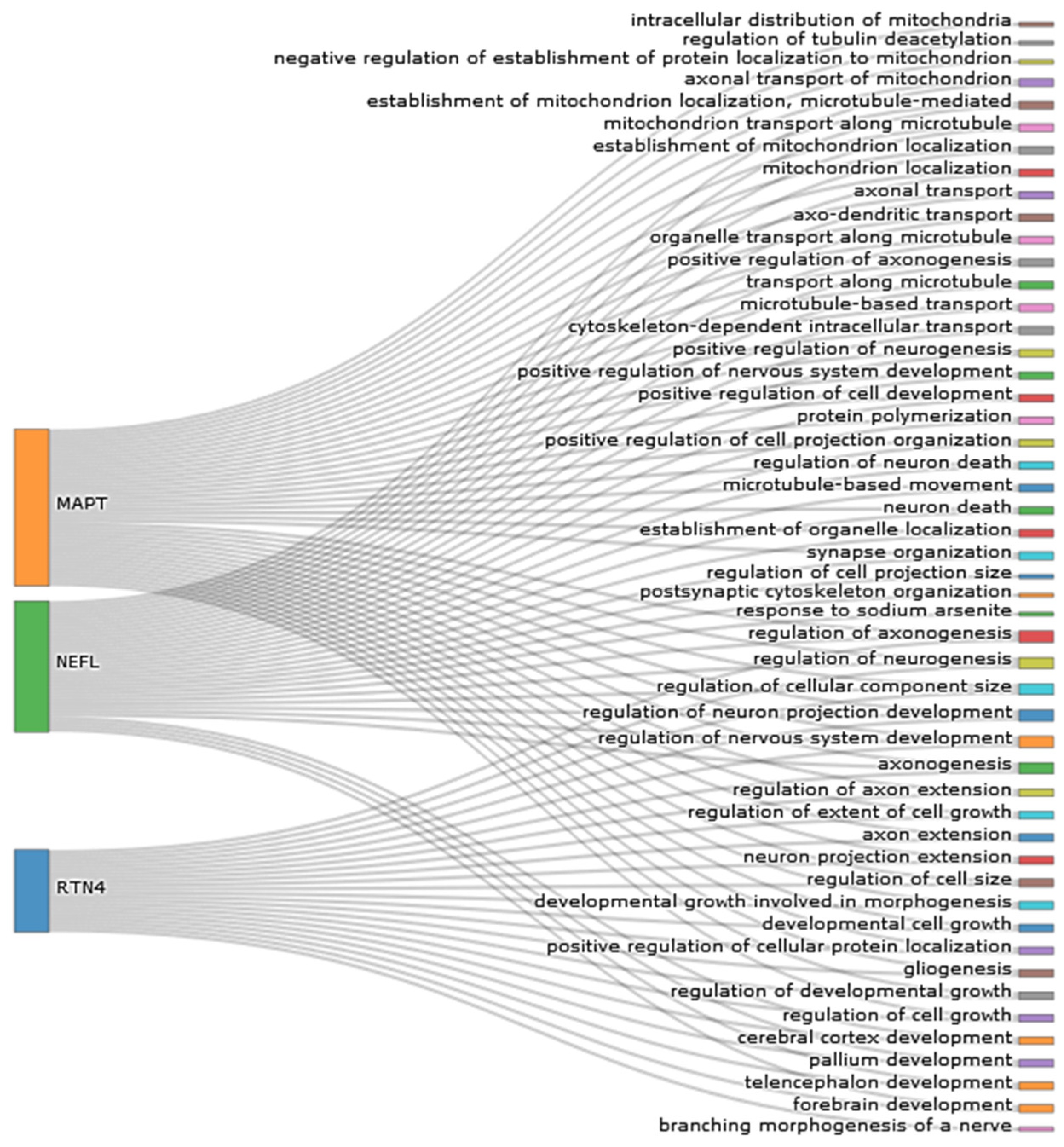
3. Results
3.1. Characteristics of Participants
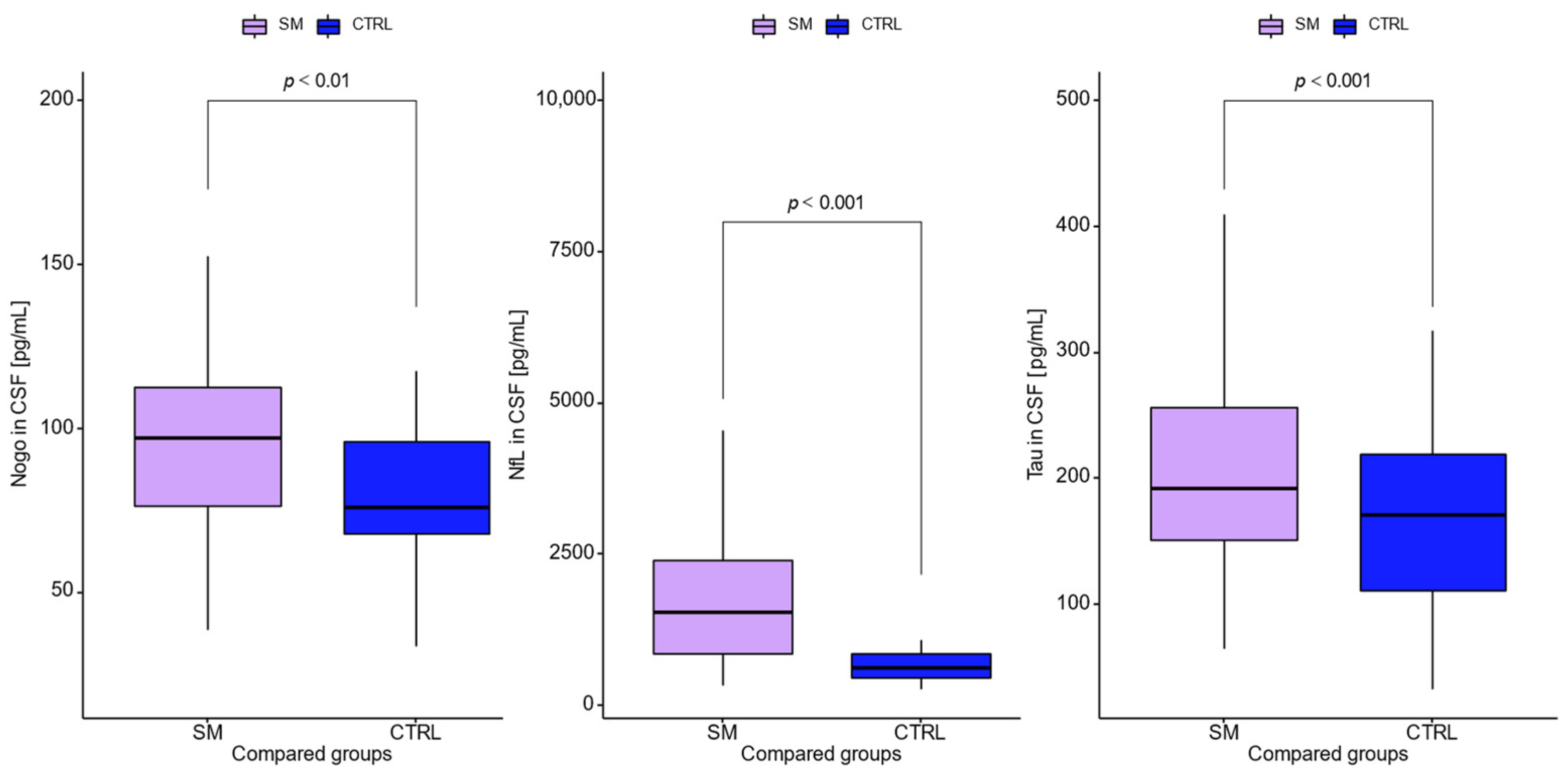
3.2. Quantification of CSF Neurodegeneration Biomarkers
3.3. Relationships between Tested Neurodegeneration Biomarkers and Immunological Parameters in Patients with MS
3.4. Diagnostic Usefulness of Tested Neurodegeneration Biomarkers in Multiple Sclerosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barkhof, F.; Calabresi, P.A.; Miller, D.H.; Reingold, S.C. Imaging outcomes for neuroprotection and repair in multiple sclerosis trials. Nat. Rev. Neurol. 2009, 5, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Friese, M.A.; Schattling, B.; Fugger, L. Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat. Rev. Neurol. 2014, 10, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Trapp, B.D.; Nave, K.A. Multiple sclerosis: An immune or neurodegenerative disorder? Annu. Rev. Neurosci. 2008, 31, 247–269. [Google Scholar] [CrossRef]
- Ferreira-Atuesta, C.; Reyes, S.; Giovanonni, G.; Gnanapavan, S. The Evolution of Neurofilament Light Chain in Multiple Sclerosis. Front. Neurosci. 2021, 15, 642384. [Google Scholar] [CrossRef]
- Bridel, C.; Van Wieringen, W.N.; Zetterberg, H.; Tijms, B.M.; Teunissen, C.E.; Alvarez-Cermeño, J.C.; Andreasson, U.; Axelsson, M.; Bäckström, D.C.; Bartos, A.; et al. Diagnostic Value of Cerebrospinal Fluid Neurofilament Light Protein in Neurology: A Systematic Review and Meta-analysis. JAMA Neurol. 2019, 76, 1035–1048. [Google Scholar] [CrossRef]
- Disanto, G.; Barro, C.; Benkert, P.; Naegelin, Y.; Schädelin, S.; Giardiello, A.; Zecca, C.; Blennow, K.; Zetterberg, H.; Leppert, D.; et al. Serum Neurofilament light: A biomarker of neuronal damage in multiple sclerosis. Ann. Neurol. 2017, 81, 857–870. [Google Scholar] [CrossRef]
- Bacioglu, M.; Maia, L.F.; Preische, O.; Schelle, J.; Apel, A.; Kaeser, S.A.; Schweighauser, M.; Eninger, T.; Lambert, M.; Pilotto, A.; et al. Neurofilament Light Chain in Blood and CSF as Marker of Disease Progression in Mouse Models and in Neurodegenerative Diseases. Neuron 2016, 91, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Barro, C.; Benkert, P.; Disanto, G.; Tsagkas, C.; Amann, M.; Naegelin, Y.; Leppert, D.; Gobbi, C.; Granziera, C.; Yaldizli, Ö.; et al. Serum neurofilament as a predictor of disease worsening and brain and spinal cord atrophy in multiple sclerosis. Brain 2018, 141, 2382–2391. [Google Scholar] [CrossRef]
- Hyun, J.W.; Kim, Y.; Kim, G.; Kim, S.H.; Kim, H.J. Longitudinal analysis of serum neurofilament light chain: A potential therapeutic monitoring biomarker for multiple sclerosis. Mult. Scler. J. 2020, 26, 659–667. [Google Scholar] [CrossRef]
- Kapoor, R.; Smith, K.E.; Allegretta, M.; Arnold, D.L.; Carroll, W.; Comabella, M.; Furlan, R.; Harp, C.; Kuhle, J.; Leppert, D.; et al. Serum neurofilament light as a biomarker in progressive multiple sclerosis. Neurology 2020, 95, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- R Core Team. 2021. Available online: https://www.r-project.org/ (accessed on 11 April 2022).
- Wu, T.; Hu, E.; Xu, S.; Chen, M.; Guo, P.; Dai, Z.; Feng, T.; Zhou, L.; Tang, W.; Zhan, L.; et al. clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation 2021, 2, 100141. [Google Scholar] [CrossRef] [PubMed]
- Plotly Technologies. Collaborative Data Science; Plotly Technologies Inc.: Montréal, QC, Canada, 2015. [Google Scholar]
- Jurewicz, A.; Matysiak, M.; Raine, C.S.; Selmaj, K. Soluble Nogo-A, an inhibitor of axonal regeneration, as a biomarker for multiple sclerosis. Neurology 2007, 68, 283–287. [Google Scholar] [CrossRef]
- Reindl, M.; Khantane, S.; Ehling, R.; Schanda, K.; Lutterotti, A.; Brinkhoff, C.; Oertle, T.; Schwab, M.E.; Deisenhammer, F.; Berger, T.; et al. Serum and cerebrospinal fluid antibodies to Nogo-A in patients with multiple sclerosis and acute neurological disorders. J. Neuroimmunol. 2003, 145, 139–147. [Google Scholar] [CrossRef]
- Fialová, L.; Bartos, A.; Švarcová, J.; Zimova, D.; Kotoucova, J.; Malbohan, I. Serum and cerebrospinal fluid light neurofilaments and antibodies against them in clinically isolated syndrome and multiple sclerosis. J. Neuroimmunol. 2013, 262, 113–120. [Google Scholar] [CrossRef]
- Sandelius, Å.; Zetterberg, H.; Blennow, K.; Adiutori, R.; Malaspina, A.; Laura, M.; Reilly, M.M.; Rossor, A.M. Plasma neurofilament light chain concentration in the inherited peripheral neuropathies. Neurology 2018, 90, e518–e524. [Google Scholar] [CrossRef] [Green Version]
- Rosengren, L.E.; Karlsson, J.E.; Karlsson, J.O.; Persson, L.I.; Wikkelsø, C. Patients with amyotrophic lateral sclerosis and other neurodegenerative diseases have increased levels of neurofilament protein in CSF. J. Neurochem. 1996, 67, 2013–2018. [Google Scholar] [CrossRef]
- Gaetani, L.; Blennow, K.; Calabresi, P.; Di Filippo, M.; Parnetti, L.; Zetterberg, H. Neurofilament light chain as a biomarker in neurological disorders. J. Neurol. Neurosurg. Psychiatry 2019, 90, 870–881. [Google Scholar] [CrossRef]
- Novakova, L.; Zetterberg, H.; Sundström, P.; Axelsson, M.; Khademi, M.; Gunnarsson, M.; Malmeström, C.; Svenningsson, A.; Olsson, T.; Piehl, F.; et al. Monitoring disease activity in multiple sclerosis using serum neurofilament light protein. Neurology 2017, 89, 2230–2237. [Google Scholar] [CrossRef] [Green Version]
- Thebault, S.; Abdoli, M.; Fereshtehnejad, S.M.; Tessier, D.; Tabard-Cossa, V.; Freedman, M.S. Serum neurofilament light chain predicts long term clinical outcomes in multiple sclerosis. Sci. Rep. 2020, 10, 10381. [Google Scholar] [CrossRef] [PubMed]
- Bjornevik, K.; Munger, K.L.; Cortese, M.; Barro, C.; Healy, B.C.; Niebuhr, D.W.; Scher, A.I.; Kuhle, J.; Ascherio, A. Serum Neurofilament Light Chain Levels in Patients with Presymptomatic Multiple Sclerosis. JAMA Neurol. 2020, 77, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Håkansson, I.; Tisell, A.; Cassel, P.; Blennow, K.; Zetterberg, H.; Lundberg, P.; Dahle, C.; Vrethem, M.; Ernerudh, J. Neurofilament light chain in cerebrospinal fluid and prediction of disease activity in clinically isolated syndrome and relapsing–remitting multiple sclerosis. Eur. J. Neurol. 2017, 24, 703–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaetani, L.; Eusebi, P.; Mancini, A.; Gentili, L.; Borrelli, A.; Parnetti, L.; Calabresi, P.; Sarchielli, P.; Blennow, K.; Zetterberg, H.; et al. Cerebrospinal fluid neurofilament light chain predicts disease activity after the first demyelinating event suggestive of multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 35, 228–232. [Google Scholar] [CrossRef]
- Virgilio, E.; Vecchio, D.; Crespi, I.; Serino, R.; Cantello, R.; Dianzani, U.; Comi, C. Cerebrospinal Tau levels as a predictor of early disability in multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 56, 103231. [Google Scholar] [CrossRef]
- Kuhle, J.; Kropshofer, H.; Haering, D.A.; Kundu, U.; Meinert, R.; Barro, C.; Dahlke, F.; Tomic, D.; Leppert, D.; Kappos, L. Blood neurofilament light chain as a biomarker of MS disease activity and treatment response. Neurology 2019, 92, e1007–e1015. [Google Scholar] [CrossRef]
- Romme Christensen, J.; Komori, M.; von Essen, M.R.; Ratzer, R.; Börnsen, L.; Bielekova, B.; Sellebjerg, F. CSF inflammatory biomarkers responsive to treatment in progressive multiple sclerosis capture residual inflammation associated with axonal damage. Mult. Scler. J. 2019, 25, 937–946. [Google Scholar] [CrossRef]
- Axelsson, M.; Malmeström, C.; Gunnarsson, M.; Zetterberg, H.; Sundström, P.; Lycke, J.; Svenningsson, A. Immunosuppressive therapy reduces axonal damage in progressive multiple sclerosis. Mult. Scler. J. 2014, 20, 43–50. [Google Scholar] [CrossRef]
- Molinuevo, J.L.; Ayton, S.; Batrla, R.; Bednar, M.M.; Bittner, T.; Cummings, J.; Fagan, A.M.; Hampel, H.; Mielke, M.M.; Mikulskis, A.; et al. Current state of Alzheimer’s fluid biomarkers. Acta Neuropathol. 2018, 136, 821–853. [Google Scholar] [CrossRef] [Green Version]
- Kuhle, J.; Barro, C.; Disanto, G.; Mathias, A.; Soneson, C.; Bonnier, G.; Yaldizli, Ö.; Regeniter, A.; Derfuss, T.; Canales, M.; et al. Serum neurofilament light chain in early relapsing remitting MS is increased and correlates with CSF levels and with MRI measures of disease severity. Mult. Scler. J. 2016, 22, 1550–1559. [Google Scholar] [CrossRef]
- Chitnis, T.; Gonzalez, C.; Healy, B.C.; Saxena, S.; Rosso, M.; Barro, C.; Michalak, Z.; Paul, A.; Kivisakk, P.; Diaz-Cruz, C.; et al. Neurofilament light chain serum levels correlate with 10-year MRI outcomes in multiple sclerosis. Ann. Clin. Transl. Neurol. 2018, 5, 1478–1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikić, I.; Merkler, D.; Sorbara, C.; Brinkoetter, M.; Kreutzfeldt, M.; Bareyre, F.M.; Brück, W.; Bishop, D.; Misgeld, T.; Kerschensteiner, M. A reversible form of axon damage in experimental autoimmune encephalomyelitis and multiple sclerosis. Nat. Med. 2011, 17, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Jitoku, D.; Hattori, E.; Iwayama, Y.; Yamada, K.; Toyota, T.; Kikuchi, M.; Maekawa, M.; Nishikawa, T.; Yoshikawa, T. Association study of Nogo-related genes with schizophrenia in a Japanese case-control sample. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2011, 156, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Cui, Y.; Li, Y.; Mi, Y. A Novel Role of Nogo Proteins: Regulating Macrophages in Inflammatory Disease. Cell. Mol. Neurobiol. 2021. [Google Scholar] [CrossRef]
- Lee, J.Y.; Petratos, S. Multiple sclerosis: Does Nogo play a role? Neuroscientist 2013, 19, 394–408. [Google Scholar] [CrossRef]
- Satoh, J.-I.; Onoue, H.; Arima, K.; Yamamura, T. Nogo-A and Nogo Receptor Expression in Demyelinating Lesions of Multiple Sclerosis. J. Neuropathol. Exp. Neurol. 2005, 64, 129–138. [Google Scholar] [CrossRef]
- Bedri, S.K.; Nilsson, O.B.; Fink, K.; Månberg, A.; Hamsten, C.; Ayoglu, B.; Manouchehrinia, A.; Nilsson, P.; Olsson, T.; Hillert, J.; et al. Plasma protein profiling reveals candidate biomarkers for multiple sclerosis treatment. PLoS ONE 2019, 14, e0217208. [Google Scholar] [CrossRef]
- Zagrebelsky, M.; Schweigreiter, R.; Bandtlow, C.E.; Schwab, M.E.; Korte, M. Nogo-A stabilizes the architecture of hippocampal neurons. J. Neurosci. 2010, 30, 13220–13234. [Google Scholar] [CrossRef] [Green Version]
- Karnezis, T.; Mandemakers, W.; McQualter, J.L.; Zheng, B.; Ho, P.P.; Jordan, K.A.; Murray, B.M.; Barres, B.; Tessier-Lavigne, M.; Bernard, C.C.A. The neurite outgrowth inhibitor Nogo A is involved in autoimmune-mediated demyelination. Nat. Neurosci. 2004, 7, 736–744. [Google Scholar] [CrossRef]
- Ineichen, B.V.; Plattner, P.S.; Good, N.; Martin, R.; Linnebank, M.; Schwab, M.E. Nogo-A Antibodies for Progressive Multiple Sclerosis. CNS Drugs 2017, 31, 187–198. [Google Scholar] [CrossRef] [Green Version]
- Theotokis, P.; Touloumi, O.; Lagoudaki, R.; Nousiopoulou, E.; Kesidou, E.; Siafis, S.; Tselios, T.; Lourbopoulos, A.; Karacostas, D.; Grigoriadis, N.; et al. Nogo receptor complex expression dynamics in the inflammatory foci of central nervous system experimental autoimmune demyelination. J. Neuroinflamm. 2016, 13, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Tong, Q.; Ye, J.; Ning, Y.; Xiong, Y.; Yang, M.; Xiao, H.; Lu, J.; Li, J.; Xu, W.; et al. Nogo-B facilitates LPS-mediated immune responses by up-regulation of TLR4-signaling in macrophage RAW264.7. Cell. Physiol. Biochem. 2017, 41, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Ullah, H.M.A.; Elfadl, A.K.; Park, S.; Kim, Y.D.; Chung, M.-J.; Son, J.-Y.; Yun, H.-H.; Park, J.-M.; Yim, J.-H.; Jung, S.-J.; et al. Nogo-A Is Critical for Pro-Inflammatory Gene Regulation in Myocytes and Macrophages. Cells 2021, 10, 282. [Google Scholar] [CrossRef] [PubMed]


| Variables | MS | Controls |
|---|---|---|
| Number | 37 | 22 |
| Sex | ||
| Female | 25 | 11 |
| Male | 12 | 11 |
| Duration of disease, months | 32 | 33 |
| Oligoclonal bands, % positive (n) | 76% (28) | 0% (0/22) |
| Type 1 OCBs, % positive (n) | 0% | 22% |
| Type 2 OCBs, % positive (n) | 82% (23) | 0% |
| Type 3 OCBs, % positive (n) | 18% (5) | 0% |
| MRI demyelination changes, % positive (n) | 78% (29) | 0% (0/22) |
| T2 and FLAIR lesions, % positive (n) | 45% (13) | 0% |
| T2 or FLAIR lesions, % positive (n) | 55% (16) | 0% |
| Albumin serum (mg/dL) | 4.36 ± 0.54 | 4.31 ± 0.65 |
| IgG serum (g/L) | 10.20 ± 2.03 | 9.27 ± 1.71 |
| IgM serum (g/L) | 1.46 ± 0.84 | 1.13 ± 0.46 |
| IgA serum (g/L) | 1.98 ± 0.66 | 2.24 ± 0.98 |
| CRP (mg/dL) | 3.5 ± 6.3 | 1.67 ± 1.32 |
| WBC (103/µl) | 7.8 ± 2.05 | 6.9 ± 1.83 |
| Glucose (mg/dL) | 98 ± 23 | 99 ± 28 |
| Cholesterol (mg/dL) | 181 ± 46 | 204 ± 41 |
| HDL (mg/dL) | 47 ± 10 | 60 ± 21 |
| LDL (mg/dL) | 136 ± 48 | 140 ± 38 |
| Comorbidities | ||
| Hypertension, % positive | 8% | 23% |
| Spine disorders, % positive | 16% | 14% |
| Thyroid disorders, % positive | 11% | 9% |
| Type 2 diabetes, % positive | 3% | 5% |
| Eye diseases, % positive | 11% | 0% |
| CSF Data | MS | Controls | p-Value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Albumin (mg/dL) | 203 ± 128 | 136 ± 91 | 0.041 |
| QAlb | 5.85 ± 1.56 | 5.28 ± 2.20 | 0.3 |
| IgG (mg/L) | 5.22 ± 3.2 | 2.55 ± 0.85 | <0.001 |
| QIgG | 5.38 ± 3.14 | 2.77 ± 0.82 | <0.001 |
| IgM (mg/L) | 1.70 ± 1.6 | 0.462 ± 0.32 | 0.002 |
| QIgM | 1.18 ± 0.91 | 0.37 ± 0.19 | <0.001 |
| IgA (mg/L) | 5.14 ± 4.5 | 3.52 ± 2.03 | 0.126 |
| QIgA | 2.79 ± 2.82 | 1.57 ± 0.51 | 0.05 |
| RTN4 (pg/mL) | 96 ± 26 | 79 ± 25 | 0.012 |
| NfL (pg/mL) | 2059 ± 1845 | 778 ± 449 | 0.001 |
| Tau (pg/mL) | 211 ± 80 | 167 ± 82 | 0.05 |
| NfL/RTN4 | 24 ± 26 | 11 ± 9 | 0.03 |
| NfL/tau | 10 ± 8 | 6 ± 7 | 0.091 |
| Protein | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC |
|---|---|---|---|---|---|
| NfL | 78 | 77 | 85 | 68 | 0.836 |
| RTN4 | 81 | 50 | 73 | 61 | 0.684 |
| Tau | 95 | 32 | 70 | 78 | 0.630 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kulczyńska-Przybik, A.; Dulewicz, M.; Doroszkiewicz, J.; Borawska, R.; Litman-Zawadzka, A.; Arslan, D.; Kułakowska, A.; Kochanowicz, J.; Mroczko, B. Comparative Analysis of Neurodegeneration and Axonal Dysfunction Biomarkers in the Cerebrospinal Fluid of Patients with Multiple Sclerosis. J. Clin. Med. 2022, 11, 4122. https://doi.org/10.3390/jcm11144122
Kulczyńska-Przybik A, Dulewicz M, Doroszkiewicz J, Borawska R, Litman-Zawadzka A, Arslan D, Kułakowska A, Kochanowicz J, Mroczko B. Comparative Analysis of Neurodegeneration and Axonal Dysfunction Biomarkers in the Cerebrospinal Fluid of Patients with Multiple Sclerosis. Journal of Clinical Medicine. 2022; 11(14):4122. https://doi.org/10.3390/jcm11144122
Chicago/Turabian StyleKulczyńska-Przybik, Agnieszka, Maciej Dulewicz, Julia Doroszkiewicz, Renata Borawska, Ala Litman-Zawadzka, Daria Arslan, Alina Kułakowska, Jan Kochanowicz, and Barbara Mroczko. 2022. "Comparative Analysis of Neurodegeneration and Axonal Dysfunction Biomarkers in the Cerebrospinal Fluid of Patients with Multiple Sclerosis" Journal of Clinical Medicine 11, no. 14: 4122. https://doi.org/10.3390/jcm11144122
APA StyleKulczyńska-Przybik, A., Dulewicz, M., Doroszkiewicz, J., Borawska, R., Litman-Zawadzka, A., Arslan, D., Kułakowska, A., Kochanowicz, J., & Mroczko, B. (2022). Comparative Analysis of Neurodegeneration and Axonal Dysfunction Biomarkers in the Cerebrospinal Fluid of Patients with Multiple Sclerosis. Journal of Clinical Medicine, 11(14), 4122. https://doi.org/10.3390/jcm11144122








