Abstract
Aging is a risk factor for several pathologies, restricting one’s health span, and promoting chronic diseases (e.g., cardiovascular and neurodegenerative diseases), as well as cancer. Telomeres are regions of repetitive DNA located at chromosomal ends. Telomere length has been inversely associated with chronological age and has been considered, for a long time, a good biomarker of aging. Several lifestyle factors have been linked with telomere shortening or maintenance. However, the consistency of results is hampered by some methodological issues, including study design, sample size, measurement approaches, and population characteristics, among others. Therefore, we aimed to systematically review the current literature on the effects of three relevant lifestyle factors on telomere length in human adults: physical activity, smoking, and sleep. We conducted a qualitative systematic review of observational and intervention studies using the Preferred Reporting Item for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. The systematic literature search covered articles published in MEDLINE and EMBASE databases (from 2010 to 2020). A total of 1400 studies were identified; 83 were included after quality control. Although fewer sedentary activities, optimal sleep habits, and non- or ex-smoker status have been associated with less telomere shortening, several methodological issues were detected, including the need for more targeted interventions and standardized protocols to better understand how physical activity and sleep can impact telomere length and aging. We discuss the main findings and current limitations to gain more insights into the influence of these lifestyle factors on the healthy aging process.
1. Introduction
Life expectancy has increased in recent decades, and it is expected to rise in the coming years [1,2,3,4]. Therefore, there is a higher probability of suffering from diseases related to an aging population, such as cardiovascular diseases [1,5,6,7], diabetes [7,8,9], hypertension [10,11,12], cancer [7,13], and neurological diseases [7,14]. Owing to the social, psychological, and economic conditions associated with aging, this has now become one of the major issues facing public health [15,16,17].
Aging is defined as a diminishing of biological functions over time, in which there is a progressive loss of the function and structure of tissues and systems [6,18]. The underlying mechanisms of the this process have been studied in depth and it seems they are related with genetic and epigenetic alterations, proteostasis loss, telomere shortening, autophagy deterioration, and mitochondrial dysfunction, among others [1,4,18,19]. However, the specific role of each mechanism remains unknown. Furthermore, these mechanisms may be modulated by other risk factors, such as diet, tobacco smoking, physical activity (PA), stress, or sleep, which, in turn, have been associated with certain diseases related to aging [18]. Therefore, a better knowledge of effective strategies for slowing the aging process is an important priority for researchers and policy makers.
Currently, several biomarkers of biological aging have been developed. Telomeres are regions of repetitive sequences (TTAGGG)n and associated protective proteins located at the ends of the cap-shaped linear chromosomes that preserve the integrity and stability of chromosomes during DNA replication. They are essential to chromosome stability and protect genomic DNA through various mechanisms [20,21,22,23,24]. Usually, a relative quantification protocol by calculating the telomere/single copy gene ratio is undertaken.
The telomere is stabilized by a six-protein complex called “shelterin”, including the TRF (telomeric repeat binding factor)1, TRF2, POT1 (protection of telomeres 1), TINF2 (TERF1-interacting nuclear factor 2), RAP1 (repressor activator protein 1 and TPP1 (tripeptidyl peptidase 1) [21,22]. Telomeres are subject to shortening during each cell division as the DNA replication mechanism cannot copy the DNA in its entirely. The enzyme telomerase, however, can solve this problem by adding the repetitive sequences and maintaining telomere length (TL). Telomere shortening is one of the most frequently studied mechanisms in the aging process. Telomere attrition reflects the cumulative load of oxidative, inflammatory, and mechanical stress [18,25]. Hence, TL has been proposed as a biomarker of biological age and a risk factor for chronic diseases [4,18,25,26,27,28,29,30] and total mortality [22,25,28,29,31,32]. Nevertheless, the association between these outcomes and the TL marker are still under discussion due to inconsistent results [19,25,33,34,35,36,37,38,39,40].
One of the factors potentially contributing to the heterogeneous results is the measurement approach used to determine TL. This is an important issue given the fact that TL differs in leukocyte subtypes isolated from the same individual. Although blood leukocytes are the most commonly used samples to determine TL, it is known that TL may substantially vary across various tissue types. The terminal restriction fragment (TRF) approach is the oldest method for analyzing TL and remains the “gold standard” even in current studies. It uses the southern blot or in-gel hybridization with a specific proof for telomere DNA [17,18]. Other methods include the fluorescent in situ hybridization (FISH) by using digital microscopy (quantitative FISH as Q-FISH) and flow cytometry (Flow-FISH). Another method, telomere shortest length assay (TeSLA), measures the distribution of shortest telomeres in heterogeneous situations. It provides a better measurement of the shortest length of telomeres. However, the quantitative polymerase chain reaction (PCR) is most widely used for its high throughput. Despite the fast, highly sensitive nature of PCR approach, which requires low amounts of DNA, the distribution of long and short telomeres cannot be obtained, and it is not possible to evaluate TL of individual cells or chromosomes [17,18]. This method is often chosen for large cohort studies, using DNA from leukocytes. Additionally, telomerase activity, gene expression, or epigenetic regulation of telomere-related genes are analyzed to delve deeper on the mechanisms [20,21,24].
TL is determined by the interaction between endogenous and external factors that explain greater or lesser susceptibility to accelerated aging [22]. Therefore, the exposome could well play a fundamental role through various biological mechanisms in the maintenance of the telomeres during aging [41,42]. Several studies have analyzed the association between lifestyle and TL, both as a protective factor [16,43,44], and as inducer of their shortening [36,45,46]. Diet has been one of the most commonly studied lifestyle factors with regard to TL. Several studies have shown the benefit of consuming foods rich in antioxidants or the benefits of various diets, such as Mediterranean type diets, on telomere attrition, as witnessed in a number of the already published reviews [47,48,49,50,51,52]. However, other relevant lifestyle factors related to aging and chronic diseases [53,54,55,56,57,58,59], such as PA, smoking or sleep have not been examined in such depth. Therefore, the aim of this work is to conduct a systematic review of the current literature (including observational and intervention studies) on the effects of PA, smoking, and sleep, on TL in relatively healthy human adults.
2. Materials and Methods
2.1. Search Strategy
We conducted a literature search for studies investigating the relationship between PA, smoking and sleep on TL in adults. In line with established guidelines (PRISMA) (http://www.prisma-statement.org/; accessed on 10 November 2021), a systematic review was carried out in which studies from the MEDLINE and EMBASE databases have been included. This was supplemented by a manual search of articles published from 2010 to March 2020. The search strategy for each lifestyle factor was made independently. The search terms employed were as follows: (“Physical Activity” OR “Exercise” OR “Smoking” OR “Tobacco” OR “Sleep”) AND (“Telomere”). The protocol for the systematic review is available at PROSPERO, the NIHR International prospective register of systematic reviews (https://www.crd.york.ac.uk/PROSPERO/; accessed on 10 November 2021). Registration number: CRD42020192881.
2.2. Inclusion and Exclusion Criteria
Bibliographical inclusion was restricted to observational (cross-sectional, longitudinal studies, case-control studies and cohorts) and experimental studies (interventions) from original articles and carried out on healthy adults of both sexes, different ethnic backgrounds or with overweight, obesity or diabetes as these conditions (mainly overweight and obesity) are prevalent in studies focusing on the general population. Excluded were studies in adolescents, children, pregnant women, individuals with infectious diseases, and other chronic pathologies, or individuals consuming addictive substances, or with respiratory disorders or chronic sleep problems. Reviews, meta-analyses, conference summaries, unpublished studies, and studies published in languages other than English were also excluded from this systematic review.
2.3. Quality Control Analysis
The selection and assessment of the quality of the articles included herein were performed independently by three reviewers (R.B., C.O.-A., and J.V.S.). The quality of each study was determined by the tools provided by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) for evaluating the quality of observational and experimental studies. Once a score was obtained, the studies were grouped by quality, as good, acceptable, or low quality. Following this appraisal, 78% of the studies included in this review were classified as good quality.
3. Results
In the initial search (Figure 1), 1400 articles were identified, of which 83 were included. The detailed characteristics of these studies are presented in Table 1 [45,46,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80], Table 2 [27,81,82,83,84,85,86,87,88,89,90,91,92,93], Table 3 [44,94,95,96,97,98,99,100,101,102,103,104], Table 4 [60,67,77,93,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120], Table 5 [121,122,123,124,125,126,127], and Table 6 [43,128,129,130,131,132,133,134,135,136,137]. Most studies focused on the association between TL and PA (Table 1, Table 2 and Table 3), followed by smoking (Table 4 and Table 5), and sleep (Table 6). Four articles were included in more than one table as in those papers, both PA and smoking were analyzed separately, and the corresponding results were included in the respective Tables.
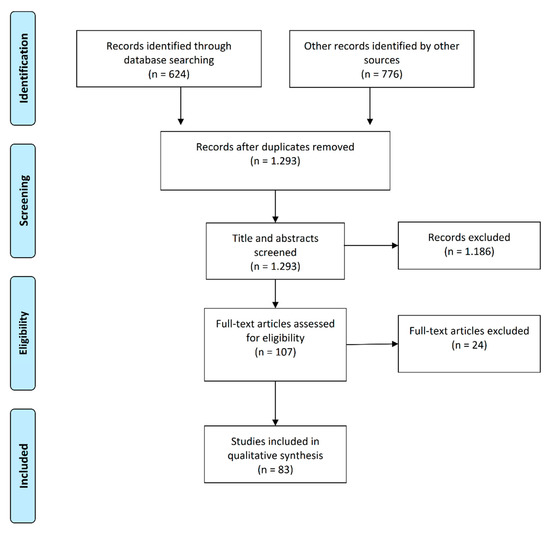
Figure 1.
Workflow of the systematic review according to PRISMA 2009 flow chart.
3.1. Association between PA and TL
The impact of PA as a relevant factor in preventing diseases associated with aging was reported in several studies [53,54,55,56,57,58,59]. However, the underlying mechanism remains to be clarified. One of the possible mechanisms could be lower telomere attrition. To date, the optimum amount of PA and the type of exercise for maintaining TL remains under debate. Of the 83 articles reviewed, 49 analyzed PA and TL [45,46,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104]. Cross-sectional studies (n = 23) are presented in Table 1 [45,46,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104]. Table 2 [27,81,82,83,84,85,86,87,88,89,90,91,92,93] shows observational studies (n = 14) using case-control and longitudinal approaches (n = 3); and Table 3 [44,94,95,96,97,98,99,100,101,102,103,104] shows intervention studies. In these tables, the details for each study including author, reference, year, design, participants and characteristics, TL analysis methods, tissue for TL analysis, exposure assessment methods, and main results, are presented.

Table 1.
Summary of cross-sectional studies on PA and TL.
Table 1.
Summary of cross-sectional studies on PA and TL.
| Author, Reference | Year | Participants | TL Measurements | Tissue for TL Analysis | Exposure Assessment Methods | Results |
|---|---|---|---|---|---|---|
| Cassidy et al. [60] | 2010 | 2284 women from NHS | PCR | Blood | PA assessed by questionnaires | No association was observed between PA and TL |
| Dankel et al. [61] | 2017 | 4881 subjects from NHANES | PCR | Blood | PA assessed by questionnaires | PA was associated with increased TL, except among those who were overweight or obese |
| Ding et al. [62] | 2018 | 588 Chinese participants (18–64 y) | PCR | Blood | PA assessed by questionnaires | No associations were found between PA and TL |
| Du et al. [63] | 2012 | 7813 women (43–70 y) from NHS | PCR | Blood | PA assessed by questionnaires | Women with moderate or vigorous activity had a longer TL than less active |
| Fretts et al. [64] | 2018 | 2312 American Indian participants from SHFS | PCR | Blood | PA reported by pedometer | Participants in the upper PA quartiles had longer TL |
| Hastings et al. [65] | 2019 | 6731 participants from NHANES | PCR | Blood | PA determined with different tests (muscle strength, cardiorespiratory capacity (VO2) and walking speed | Participants with shorter telomeres performed worse on physical function tests |
| Kim et al. [66] | 2012 | 44 healthy postmenopausal women | PCR | Blood | PA reported by interview | Regular PA was associated with longer TL |
| Latifovic et al. [67] | 2016 | 477 subjects (20–50 y) | PCR | Blood | PA assessed by questionnaires | Vigorous PA related to longer TL |
| Loprinzi [68] | 2015 | 6405 participants from NHANES | PCR | Blood | Sedentary PA on screens (TV, computer …) reported by interview | Sedentary behavior based on screen free time was inversely associated with TL |
| Loprinzi et al. [69] | 2015 | 6503 participants from NHANES | PCR | Blood | PA reported by interview | Lower TL among those who performed less PA |
| Loprinzi et al. [70] | 2016 | 6474 participants from NHANES | PCR | Blood | PA reported by interview | The specific PA of running was the only activity associated with TL |
| Ogawa et al. [45] | 2017 | 6933 participants from NHANES | PCR | Blood | PA reported by interview and VO2max in subsample | Those who undertake vigorous PA present longer TL than those who practice moderate PA or do not perform PA |
| Sassenroth et al. [71] | 2015 | 815 participants from BASII | PCR | Blood | PA assessed by questionnaires | PA was associated with longer TL only when PA was regular and ≥10 y preceding the assessment |
| Savela et al. [72] | 2013 | 204 participants from HBS | SB | Blood | PA assessed by questionnaires | An U-shaped association was found. Moderate PA associated with longer TL |
| Shadyab et al. [73] | 2017 | 1476 elderly women from WHI | SB | Blood | PA assessed by questionnaires | Longer TL in the group of more active women compared to those who undertook less PA |
| Shadyab et al. [74] | 2017 | 1481 elderly women from WHI | SB | Blood | PA assessed by questionnaires and accelerometer | Longer sedentary time was associated with shorter TL in physically inactive older women |
| Shadyab et al. [75] | 2017 | 1405 elderly women from WHI | SB | Blood | PA assessed by questionnaires and accelerometer | Women at the highest level of total PA compared to the lowest level had longer TL, but significance was lost after adjustment for confounded terms |
| Silva et al. [76] | 2017 | Elderly subjects (65–85 y) with intense and moderate training, and never trained | Flow-FISH | Blood | PA assessed by questionnaires and VO2max | TL was longer in the intense training group compared to the untrained group |
| Song et al. [77] | 2010 | 170 subjects (18–80 y) | PCR ELISA | Blood | PA assessed by questionnaires | PA was inversely correlated with biomarkers of DNA damage, and these biomarkers were negatively associated with TL |
| Tucker LA [46] | 2017 | 5.823 adults from NHANES | PCR | Blood | PA assessed by questionnaires | PA was inversely associated with TL. High levels of PA were associated with longer telomeres, with a biological aging of 9 y difference compared with the sedentary ones |
| von Känel et al. [78] | 2017 | African (n = 96) and Caucasian (n = 107) schoolteachers from SAABPAS | PCR | Blood | PA measured by accelerometry | Regular PA of different intensity was not directly associated with TL |
| Williams et al. [79] | 2017 | 5674 adults from NFBC | PCR | Blood | PA determined by physical tests | TL was associated with greater aerobic fitness and muscular endurance only in young adults |
| Xue et al. [80] | 2017 | 518 adults from China | SB | Blood | PA assessed by questionnaires | Watching TV was associated with shorter TL However, doing moderate or vigorous PA was not associated with TL |
TL: telomere length; bp: base pairs; PA: physical activity; y: years old; TV: television; h: hour; d: day; w: week; m: month; y: year; VO2max: maximal oxygen uptake; T2D: type 2 diabetes; ISRT: Individual Shear Rate Therapy; PCR: Polymerase Chain Reaction; SB: Southern blot analysis of terminal restriction fragment lengths (TRF); GE: gene expression; GWEA: genome-wide expression arrays; TERT: telomerase reverse transcriptase gene; WB: Western blotting; TERRA: telomeric repeat-containing RNA gene; FISH: fluorescence in situ hybridization; FACS: fluorescence activated cell sorting; NHS: Nurses’ Health Study; NHANES: National Health and Nutrition Examination Survey; SHFS: Strong Heart Family Study; BASII: Berlin Aging Study II; HBS: Helsinki Businessmen Study; WHI: Women’s Health Initiative Objective Physical Activity and Cardiovascular Health study; SAABPAS: Sympathetic activity and Ambulatory Blood Pressure in Africans study; NFBC: Northern Finland Birth Cohort.

Table 2.
Summary of case-control (CC) and longitudinal (L) studies on PA and TL.
Table 2.
Summary of case-control (CC) and longitudinal (L) studies on PA and TL.
| Author, Reference | Year | Type | Participants | TL Measurements | Tissue for TL Analysis | Exposure Assessment Methods | Results |
|---|---|---|---|---|---|---|---|
| Colon et al. [81] | 2019 | CC | 7 male triathlon athletes and 7 active controls | PCR | Blood | PA assessed by questionnaires and VO2max | The triathlete subjects had longer telomeres than the active controls. Positive association between TL and VO2max |
| Denham et al. [27] | 2016 | CC | Polish endurance athletes (n = 61) and paired active controls (n = 61) | PCR GE | Blood | PA reported by questionnaires | Endurance athletes have longer TL, as well as a higher expression of TERT mRNA |
| Denham et al. [82] | 2013 | CC | 67 male ultramarathon runners and 63 controls | PCR | Blood | PA assessed by questionnaires | Ultramarathon runners had telomeres 11% longer than controls |
| LaRocca et al. [83] | 2010 | CC | 57 participants: differing by age and PA | SB | Blood | PA assessed by questionnaires and VO2max | TL of the older endurance-trained adults was greater than their sedentary peers. TL was positively related to VO2max |
| Magi et al. [84] | 2018 | CC | 26 men (20–50 y) | SB | Muscle | PA reported by interview | Regular physical training was positively with the maintenance of TL |
| Mathur et al. [85] | 2013 | CC | 17 marathon runners and 15 controls | FISH | Blood | Different tests were performed | No differences were observed in the TL of the different PA groups or tests |
| Muniesa et al. [86] | 2017 | CC | 125 young elite athletes | PCR | Blood | PA reported through a database | Elite athletes had a TL 12.4% longer than controls |
| Osthus et al. [87] | 2012 | CC | 10 young and 10 elderlies (50% endurance athletes, 50% medium level) | PCR | Muscle | PA assessed by questionnaires and VO2max | Older endurance athletes had longer TLs compared to their counterparts. These differences were not seen in the young participants |
| Puterman et al. [88] | 2010 | CC | 63 postmenopausal women | PCR | Blood | PA assessed by questionnaires | No association between PA and TL was observed. However, vigorous PA was linked to TL |
| Rae et al. [89] | 2010 | CC | 18 endurance runners vs. 19 controls | SB | Muscle | PA assessed by questionnaires | No significant differences were found between the mean and minimum TL between the endurance runners and controls |
| Simoes et al. [90] | 2017 | CC | Elite sprinters (n = 11) and untrained controls | PCR | Blood | PA reported by medical history | Elite sprinters have longer TL than their paired controls |
| Soares-Miranda et al. [91] | 2015 | L | 582 elderly subjects from CHS | SB | Blood | PA assessed by questionnaires and different tests | At baseline, higher PA was associated with longer TL. Prospective analyses show that changes in PA were associated with differences in changes in TL |
| Stenbäck et al. [92] | 2019 | L | 700 elderly subjects (Finland) | PCR | Blood | PA assessed by questionnaires and accelerometry | PA for 2-w was not associated with TL after adjustment. However, moderate PA was associated with longest TL |
| Weischer et al. [93] | 2014 | L | 4576 participants from CCHS | PCR | Blood | PA assessed by questionnaires | Increased PA was associated with short TL at baseline, but not with a change in TL during 10 years of follow-up |
TL: telomere length; bp: base pairs; PA: physical activity; y: years old; TV: television; h: hour; d: day; w: week; m: month; y: year; VO2max: maximal oxygen uptake; T2D: type 2 diabetes; PCR: Polymerase Chain Reaction; SB: Southern blot analysis of terminal restriction fragment lengths (TRF); GE: gene expression; TERT: telomerase reverse transcriptase gene; WB: Western blotting; CCHS: Copenhagen City Heart Study; HRS: Health and Retirement Study; CHS: Cardiovascular Health Study.

Table 3.
Summary of intervention studies on PA and TL.
Table 3.
Summary of intervention studies on PA and TL.
| Author, Reference | Year | Participants | TL Measurements | Tissue for TL Analysis | Intervention | Results |
| Borghini et al. [94] | 2015 | 17 male endurance athletes and 32 controls | PCR | Saliva | Ultra-endurance race in athletes (330 km in a maximum time of 150 h) | Endurance athletes present longer TL than controls. Acute extreme intervention increased TL attrition compared to baseline |
| Brandao et al. [95] | 2020 | 20 obese sedentary women (20–40 y) | PCR | Blood | Combined aerobic and strength training (55 min/d, 3 times/w, 8 w) | Combination training for 8 w promoted an increase in TL, fat-free mass, and physical performance |
| Chilton et al. [96] | 2014 | 22 healthy young men, nonsmokers | GE | Blood | 30 min of continuous running on a treadmill at 80% O2 | Increased expression of the key telomeric gene TERT mRNA, associated with longer TL |
| Diman et al. [97] | 2016 | 10 healthy and moderately active young men | FISH GE | Muscle | Two cycling exercise groups: low intensity (50% VO2) and a high intensity (75% VO2). | Endurance cycling exercise increased the TERRA gene expression, a key player in telomere integrity, associated with longer TL |
| Dimauro et al. [98] | 2017 | 24 men, 12 T2D and 12 controls. | FISH | Blood | Two groups: untrained and trained (moderate PA over at least 1 y) | Individuals who participated in the regular exercise program showed longer TL |
| Friedenreich et al. [99] | 2018 | 212 Healthy women aged (50–74 y). | PCR | Blood | Two groups: aerobic exercise (45 min, 5 d/w for y, n = 99) vs. inactivity | No association between aerobic exercise and TL |
| Laye et al. [100] | 2012 | 8 participants in the “2010 Bornholm Ultramarathon 7” | PCR GE | Muscle and whole blood | Carrying out 7 marathons on 7 consecutive d | A positive regulation of gene expression of the components of the shelterin complex was found without observing changes in TL |
| Mason C et [101] | 2013 | 439 women with overweight or obesity (50–75 y) | PCR | Blood | Four groups: weight loss with diet (n = 118), PA (n = 117), diet + exercise (n = 117) and control (n = 87); for 12 m | After 12 m, no changes were seen in the TL of the intervention groups compared to the control group |
| Puterman et al. [102] | 2018 | 68 careers of elderly people | PCR | Blood | Two groups: aerobic training and control for 24 w | Significant changes in TL were observed in aerobic exercise intervention group |
| Sjögren et al. [103] | 2014 | 49 participants (68 y) with low PA | PCR | Blood | Two groups: PA and minimal PA. Intervention for 6 m | The decrease in seated time in the intervention group was associated with TL |
| Werner et al. [44] | 2019 | 125 inactive participants | PCR FlowFISH FACS | Blood | Three groups: aerobic endurance training; high intensity exercises; resistance training | Endurance training and high intensity, but not strength training, was associated with increased telomerase activity and TL |
| Zietzer et al. [104] | 2017 | 26 youth and 14 elderly participants | PCR | Blood | Randomization to 2 trials: -ISRT-1: crossover trial (2 separate sessions). -ISRT-2: 1 session of ISRT, and subsequently 5 d/w of 90 min. | Telomerase activity in young individuals increased with exercise. In contrast, short-term ISRT exercises were not associated with telomerase activity. However, after 5 w of daily ISRT, telomerase increased |
TL: telomere length; bp: base pairs; PA: physical activity; y: years old; TV: television; h: hour; d: day; w: week; m: month; y: year; VO2max: maximal oxygen uptake; T2D: type 2 diabetes; ISRT: Individual Shear Rate Therapy; PCR: polymerase chain reaction; SB: Southern blot analysis of terminal restriction fragment lengths (TRF); GE: gene expression; TERT: telomerase reverse transcriptase gene; mRNA: micro-ribonucleic acid (RNA fragment); WB: Western blotting; TERRA: telomeric repeat-containing RNA gene;; FISH: fluorescence in situ hybridization.
Most studies on the effect of PA on TL (37/49) were analyzed at the observational level in most cross-sectional studies (Table 1); PA was associated with longer TL. However, this association was mainly reported in subgroup analyses and not for the whole population included in the study. This subgroup analysis involved participant characteristics (men or women, older or young, among others) or different levels of PA (active versus inactive, moderate versus vigorous, regular, or not regular, etc.) Thus, as multiple comparisons were carried out in the same study, some of these comparisons could be statistically significant by chance, if no correction for multiple comparisons was considered. Therefore, the effect of PA on TL in these cross-sectional studies carrying out multiple comparisons is probably overestimated in the published papers. Among the cross-sectional studies, 3 [60,62,78] did not observe any association between PA and TL. The others reported mixed results (no association for some subgroups, but associations in at least one subgroup). One study [72], reported a U-shaped association, with only moderate PA being associated with longer TL. In these cross-sectional studies [45,46,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80], heterogeneity was also detected in the methodology used. PA was assessed by questionnaires in the most studies: some also included objective assessment (accelerometers, pedometers, or several PA tests) in the whole population or in subsamples. Likewise, variability in the methods used to assess TL was detected (17/23 used quantitative PCR, 5/23 used southern blot and 1/23 used Flow-FISH). Blood was the tissue selected for analysis in cross-sectional studies.
To note, several publications (7/24) were carried out on the same epidemiological study [in the United States population of the “National Health and Nutrition Examination Survey” (NHANES)] analyzing different levels of PA or participant characteristics [45,46,61,65,68,69]. Although the results differed depending on the subgroup and exposure analyzed, in general, in NHANES, undertaking any PA is associated with longer TL [45,46,61,62,63,64,65,66,67,68,69]. Thus, individuals that undertook vigorous PA presented greater TL than those with moderate activity or those who did not undertake any PA. No differences were observed between the two latter groups [45]. However, in a subgroup analysis in NHANES, the authors reported that the presence of overweight or obesity could counter the protective effect of PA on TL [61]. Moreover, the differences between the degree of PA and TL were only observed among individuals aged 40 to 64 years [69].
In NHANES, individuals reporting vigorous activity had longer TL (reported in bp increase) (than sedentary individuals and those reporting low or moderate PA. Other studies in different populations, also estimated the effect of PA in terms of bp. Thus, Shadyab et al. [73], in a group of post-menopausal women in the Women’s Health Initiative (WHI) study, observed a significant difference in bp between those who reported greater PA compared to those reporting the least PA. Moreover, a greater TL was observed in women whose walking speed was faster [73]. Similarly, in women from the Nurses’ Health Study (NHS), it was observed that those who undertook vigorous or moderate activity for 2–4 h a week had a greater TL than those less active or sedentary women. Additionally, in the Berlin Aging Study II (BASII), it was estimated that regular PA over the previous 10 years was required to achieve a sustained effect on TL [71].
Furthermore, the role of type of PA, such as easy or fast walking, cycling, or undertaking aerobic or callisthenic exercises, on TL was assessed. Studies note an increase in TL in those performing aerobic or callisthenic exercise only [63]. Nevertheless, these results are contradictory to those found in this same study in a population of lower sample size in previous years [60]. In NHANES, only running was associated with greater TL, this relationship perhaps explaining the benefits of aerobic activity on certain pathologies or on total mortality [70]. Regarding more moderate activities—participants who accumulated more steps or who were in the highest quartile had longer TL than those with fewer steps per day [64]. In longitudinal studies, an increase in exercise-induced caloric expenditure was associated with less shortening of the telomeres over time [73]. Regarding only sedentary individuals in a women’s accelerometer study, a difference of 170 bp was observed between the women in the highest sedentary quartile and those of the lowest level. However, when the self-reported sedentary lifestyle of the participants was studied, this was not associated with TL, possible due to the imprecise nature of self-reported questionnaires [75]. With regard to a sedentary lifestyle in a young adult population, it was observed that adults who spent more time watching the television presented shorter TL than those who watched it less [68]. For each hourly increase of television, the risk of having short telomeres increased by 7% [68]. On classifying the subjects into age groups, this association was only significant in adults from 20 to 40 years old [80].
Table 2 [27,81,82,83,84,85,86,87,88,89,90,91,92,93] shows case-control (n = 11) and longitudinal studies (n = 3) analyzing the association between PA and TL. The results were mixed. In a majority of studies (n = 8/11), TL was longer in physically active cases than in controls. However, in three studies, no differences between TL in cases and control were found [85,88,89]. In general, sample size in the case-control studies was smaller than in the cross-sectional studies and participants characteristics were maximized in terms of PA (for example cases being elite sprinters in comparison with untrained controls [90], or cases being ultramarathon runners in comparison with controls [82]. The methods to assess TL were diverse, including PCR (7/11), Southern blot (3/11) or FISH (1/11). Regarding the type of tissue analyzed, although in general leukocytes were isolated from blood, two studies analyzed muscle [87,89]. Moreover, in one study, gene expression analysis of the Telomerase Reverse Transcriptase gene (TERT) gene was also examined [27]. Specifically, Denham et al. [27] compared several factors associated with cellular aging in endurance athletes with their corresponding active controls and found a greater TL and greater expression of the TERT and TPP1 genes in athletes.
The three prospective studies [91,92,93] also presented mixed results. Weisher et al. [93] found no association between changes in PA and changes in TL over 10 years of follow-up in a large sample size of participants in the Copenhagen City Heart Study (CCHS). However, Soares-Miranda et al. [91] found an association between changes in PA and in TL in subjects participating in the Cardiovascular Health Study (CHS). Subgroup associations were found in the third study [92].
Table 3 [44,94,95,96,97,98,99,100,101,102,103,104] shows intervention studies (n = 12) analyzing the association between PA and TL. Several trials (9/11) found that individuals in active PA interventions had an increase in TL relative to controls, but others did not observe such differences (3/11) or reported subgroup results. Again, mixed results were found, mainly due to the great heterogeneity of the interventions, study designs (non-controlled or controlled, and different control groups among the randomized trials), sample size, as well as the participant’s characteristics. Thus, seven studies measured TL using only PCR; in one study, PCR was used combined with gene expression or Flow-FISH; one study used FISH, and in two, gene expression (combined with microRNA analysis in one of them), was used. Likewise, some heterogeneity was detected in the tissue analyzed (mainly in blood, but two in muscle and one in saliva). All of this contributed to the possible heterogeneity.
Three intervention trials did not report associations between PA and TL [99,100,101], but even these trials were very heterogeneous. Friedenreich et al. [99], analyzing 212 healthy women aged 50–74 years and comparing 1 year intervention (in two groups: a group with aerobic exercise, 45 min/d, 5 d/week versus an inactivity group) did not find significant association between aerobic exercise intervention and TL. Laye et al. [100] did not observe changes in TL by subjecting eight trained individuals to seven marathons in seven consecutive days. However, there was greater mRNA regulation of the shelterin complex, involved in TL protection [100]. A trial of 439 elderly post-menopausal women [101] compared TL after 12 months of PA and/or dietary intervention, plus a control group, and did not find any differences between the different groups. However, after 12 months, in a subgroup analysis, the women with the shortest baseline telomeres had a greater mean increase in TL than those with the longest baseline TL.
An important consideration for intervention trials is the length of the intervention. Brandao et al. [95] observed that an 8-w intervention combining aerobic and strength training in sedentary women with obesity increased TL. However, it has been reported that different training modalities may exert different effects. Thus, Werner et al. [44] in a complex intervention showed that endurance and interval training increased TL, but not endurance training. In this study, telomerase activity was also measured and was positively correlated with TL. Similarly, Zietzer et al. [104] in an intervention study carried out in youth and elderly participants showed that in the youngest population, telomerase activity increased significantly in a single session of aerobic exercise [104]. When endurance athletes were compared with individuals with an average level of activity, a greater TL was observed compared with the control group.
However, on stratifying by age, this difference was not observed in the youngest group (22–27 years) but was much more noticeable in the elderly group (66–77 years) [104].
With regard to the different types of PA, the results have been mixed, mainly due to the heterogeneity of the intervention, tissue, and assessment method and to the small sample sizes. Bicycle endurance exercise has been associated with increased gene expression levels of “Telomeric repeat-containing RNA” (TERRA) that is transcribed from the telomeres and is associated with longer TL, suggesting benefits of aerobic exercise [97]. Likewise, an upregulation of various telomeric genes, such as the TERT or SIRT6 (Sirtuin 6) genes, as well as a differential regulation in microRNA that codifies genes involved in the homeostasis of telomeres was found after 30 min of intense cardio-respiratory exercise in young males [96].
3.2. Association between Telomere Length and Tobacco Smoking
Of the 83 articles reviewed, 27 analyzed cigarette smoking and TL, all of which were observational studies (ethical reasons are crucial here explaining the lack of intervention studies). We grouped these observational studies in cross-sectional (Table 4) [60,67,77,93,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120] and in case-control and longitudinal studies (Table 5) [121,122,123,124,125,126,127]. There were 20 cross-sectional studies [60,67,77,93,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120], 2 case-control studies [124,127], and 5 longitudinal studies [121,122,123,125,126]. Despite some heterogeneity in the results, population characteristics, and methodology used, most studies show an association between tobacco smoking and reduced TL.
Only 2 of the 21 cross-sectional studies report no association between tobacco smoking and TL [60,105]; in one additional study, the initial association between tobacco smoking and TL was non-significant after adjusting for BMI [120]. In another report [108], although smoking status was not associated with TL, there was an inverse association between the number of cigarettes smoked and TL. The initial investigation by the NHS, analyzing the association between smoking and TL in 2284 women, found no relationship between both variables [60]. Two years later, in 5862 women, that same study observed a slight association between TL and smoking, specifically 8% greater TL in subjects who had never smoked as opposed to smokers [117] The authors stated that the combined effect of various risk factors (diet, PA, weight, alcohol, and tobacco) was much greater than the individual additive effect [117]. Various authors have also found greater telomere shortening in smokers as opposed to non-smokers [119,121,122,123]. Tobacco possibly accounts for 0.64–1.23% of TL variation [116]. More specifically, there could exist 50 bp of variation between smokers and non-smokers [119], 73 bp [125], or 190 bp according to others [112].

Table 4.
Summary of cross-sectional studies on smoking and TL.
Table 4.
Summary of cross-sectional studies on smoking and TL.
| Author, Reference | Year | Participants | TL Measurements | Tissue for TL Analysis | Exposure Assessment Methods | Results |
|---|---|---|---|---|---|---|
| Cassidy et al. [60] | 2010 | 2284 women from NHS | PCR | Blood | Tobacco smoking reported by questionnaire | Tobacco use was not associated with TL |
| Flannagan et al. [105] | 2017 | 20 smokers and 20 non-smokers | PCR | Blood | Tobacco smoking reported by questionnaire | No association was detected between smoking and TL |
| Gao et al. [106] | 2016 | 548 participants from ESTHER | PCR and methylation | Blood | Tobacco smoking reported by questionnaire | Lower methylation was observed in current smokers associated with TL |
| Huzen et al. [107] | 2014 | 8592 subjects from PREVEND | PCR | Blood | Tobacco smoking reported by questionnaire | Dose-dependent association between number of cigarettes smoked and baseline TL |
| Khan et al. [108] | 2019 | 5864 participants from NHANES | PCR | Blood | Tobacco smoking reported by questionnaire | No association was detected between TL and smoker status, but there was an inverse association between the number of cigarettes smoked and shorter TL |
| Latifovic et al. [67] | 2016 | 477 subjects (20–50 y) | PCR | Blood | Tobacco smoking reported by questionnaire | Smokers had shorter TL than those who had never smoked |
| Lei et al. [109] | 2020 | 500 African Americans from FACHS | Methylation arrays | Blood | Tobacco smoking reported by questionnaire | Associations between smoking and aging by differences in methylation |
| Lu et al. [110] | 2019 | 2256 participants from WHI and JHS; 1078 participants from FHS | SB and methylation arrays | Blood | Tobacco smoking reported by questionnaire | Being a smoker was associated with lower values of mtlDNA (level of DNA methylation as an estimator of TL). In addition, smoking was associated with a shorter TL |
| Lu et al. [111] | 2017 | 1303 non-smoking adult participants from GS:GFHS | PCR | Blood | Tobacco smoking reported by questionnaire | TL decreased more rapidly with increasing age among passive smokers compared to those who were not exposed |
| Nawrot et al. [112] | 2010 | 216 non-smokers and 89 smokers from FLEMENGHO | SB | Blood | Tobacco smoking reported by questionnaire | The TL of smokers was shorter than in non-smokers |
| Needham et al. [113] | 2013 | 5360 subjects from NHANES | PCR | Blood | Tobacco smoking reported by questionnaire (number of cigarettes/d and years of smoking) | Smokers of 60 packs of cigarettes/y or more showed significantly shorter TL than those who had never smoked |
| Patel et al. [114] | 2017 | 461 subjects NHANES | PCR and GE | Blood | Tobacco smoking reported by questionnaire | The number of cigarettes smoked/d was associated with a shorter TL, but no differences were detected in the expression levels of candidate genes |
| Rode et al. [115] | 2014 | 55,568 participants from CGPS | PCR | Blood | Tobacco smoking reported by questionnaire | An association was observed between high cumulative tobacco use and short TL |
| Song et al. [77] | 2010 | 170 adults (18–80 y) | PCR | Blood | Tobacco smoking reported by questionnaire | Inverse association between smoking and TL |
| Sulastri et al. [116] | 2017 | 130 Minangkabau men (40–50 y) | PCR | Blood | Tobacco smoking reported by questionnaire | Smoking was a risk factor for telomere shortening |
| Sun et al. [117] | 2012 | 5862 women from NHS | PCR | Blood | Tobacco smoking reported by questionnaire | Compared to current smokers, women who had never smoked had longer TLs |
| Verde et al. [118] | 2015 | 147 healthy smokers from Spain | PCR | Blood | Smoking habit was determined by survey and Fagerström test | Association between cumulative tobacco use and years of smoking and reduction in TL. No significant differences between the values of metabolized nicotine and TL |
| Weischer et al. [93] | 2014 | 4576 participants from CCHS | PCR | Blood | Tobacco smoking reported by questionnaire | Short TL was associated with increased tobacco use |
| Wulaningsih et al. [119] | 2016 | 6456 participants from NHANES | PCR | Blood | Questionnaires for smoking and serum cotinine levels were evaluated | Being a smoker was associated with a 50 bp decrease in TL compared to those who had never smoked |
| Yun et al. [120] | 2019 | 1037 adults (729 white and 308 African American) | SB | Blood | Tobacco smoking reported by questionnaire | An association was observed between smoking and TL. Body weight had a suppressing effect on this association |
TL: telomere length; PCR: polymerase chain reaction; SB: Southern blot analysis of terminal restriction fragment lengths (TRF); GE: gene expression; NHS: Nurses’ Health Study; ESTHER: Epidemiologische Studie zu Chancen der Verhütung, Früherkennung und optimierten Therapie chronischer Erkrankungen in der älteren Bevölkerung (German); PREVEND: Prevention of Renal and Vascular End-Stage Disease study; NHANES: National Health and Nutrition Examination Survey; y: year; FACHS: Family and Community Health Study; WHI: Women’s Health Initiative Objective Physical Activity and Cardio-vascular Health study; JHS: Jackson Heart Study; GFHS: Scottish Family Health Study; FLEMENGHO: Flemish Study on Environment, Genes and Health Outcomes; CGPS: Copenhagen General Population Study; CCHS: Copenhagen City Heart Study; HRS: Health and Retirement Study.
Ex-smokers have a lower loss of TL compared to current smokers [119]. Similarly, a significant inverse relationship was found between the number of cigarettes consumed and TL [108,114].
Regarding longitudinal studies (Table 5) [121,122,123,125,126], more discrepancies were found. Although in these studies, significant associations between tobacco smoking and TL were found at baseline, some of these studies, such as the Epidemiologische Studie zu Chancen der Verhütung, Früherkennung und optimierten Therapie chronischer Erkrankungen in der älteren Bevölkerung (ESTHER) cohort [125], did not detect longitudinal associations. However, other longitudinal studies [122,123] reported significant associations in the follow-up. In order to explain the potential discrepancies in cross-sectional and longitudinal associations, Zhang et al. [121] analyzed in 5624 participants from an American population. They analyzed differences in TL between smokers and non-smokers following 16 years of follow-up, with concurrent and past smoking status reported biennially, and taking into account the sex influence. The authors observed that smoking was associated with reduction in TL over time, but this association was attenuated in men. The reason for this attenuation was a higher rate of smoking cessation among men with shorter TL, probably because of the poor health of these individual with shorter TL. In conclusion, this study suggested that time-varying and sex-specific associations should be measured in the studies analyzing the association between tobacco smoking and TL.
As with PA, several methodologies were used in studying the association between tobacco smoking and TL. The most frequent method was by PCR, followed by southern blot. However, other techniques were also used. It is interesting to mention the assessment of DNA methylation in several studies [106,109,110], taking into account the strong association between tobacco smoking and DNA methylation.

Table 5.
Summary of case-control and longitudinal studies on smoking and TL.
Table 5.
Summary of case-control and longitudinal studies on smoking and TL.
| Author, Reference | Year | Type of Study | Participants | TL Measurements | Tissue for TL Analysis | Exposure Assessment Methods | Results |
|---|---|---|---|---|---|---|---|
| Zhang et al. [121] | 2016 | Longitudinal | 5624 participants from HRS, 16 y follow up | PCR | Saliva | Tobacco smoking reported by questionnaire | Shorter TL observed in smokers. The number of cigarettes was also inversely associated with TL in women, but not in men. Sex-specific prospective changes on smokers and TL were detected |
| Bendix et al. [122] | 2014 | Longitudinal | 1356 individuals (30–70 y). 10-y follow-up | PCR | Blood | Tobacco smoking reported by questionnaire | Tobacco influences the change in TL after follow-up, with smokers having a greater risk of telomere shortening |
| Chen et al. [123] | 2011 | Longitudinal | Follow-up of 271 participants at 3 times | SB | Blood | Tobacco smoking reported by survey | Smoking at baseline was associated with shorter TL and accelerated shortening |
| Marcon et al. [124] | 2017 | Twin study (case-control) | 22 homozygous twins (one smoker and the other non-smoker) | SB and methylation arrays | Blood | Tobacco smoking reported by questionnaire, and urine cotinine | Statistically significant higher values of TL in smokers compared to non-smoking twins |
| Müezzinler et al. [125] | 2015 | Longitudinal | 3600 elderly adults. Follow-up on 1000 participants | PCR | Blood | Tobacco smoking reported by questionnaire | Smoking was inversely associated with TL at baseline. On average, current smokers had 73 bp shorter telomeres, but this relationship could not be shown longitudinally |
| Strandberg et al. [126] | 2011 | Longitudinal | 622 participants from Finland (30–45 y). Follow-up at 30–40 years | SB | Blood | Tobacco smoking reported by questionnaire | Age-adjusted TL was significantly longer among lifelong non-smokers compared to past or present smokers |
| Walters et al. [127] | 2014 | Case-Control | Healthy smokers (n = 29) vs. non-smokers (n = 29) | SB | Epithelial cells or whole blood | Tobacco smoking reported by questionnaire, and urine cotinine | No differences were observed between TL and being a smoker or not |
TL: telomere length; y: years; bp: base pairs; PCR: polymerase chain reaction; SB: Southern blot analysis of terminal restriction fragment lengths (TRF); HRS: Health and Retirement Study; CHS: Cardiovascular Health Study.
In addition, some protein biomarkers and gene expression assays have been assessed in various studies (Table 4 and Table 5). For example, Song et al. identifying a higher level of different protein biomarkers of DNA damage and dysfunction of the telomeres in smokers compared to non-smokers [77]. Patel et al. could not find any differences on the levels of candidate gene expression between smokers and non-smokers [114]. On the other hand, contradictory findings were reported in a methylation and gene expression study carried out on twins. The authors observed greater telomerase activity and greater TL in smokers than in non-smokers [124].
Lastly, the effect of second-hand smoke or “passive smoking” and TL has been analyzed and it was suggested that high degree of exposure to second-hand smoke could accelerate the shortening of the telomeres that naturally occurs with aging [111]. However, another publication did not find any association between passive smoking and TL [119]. More research is needed to evaluate the effects of second-hand smoke on TL that takes into account various confounders such as air pollution, environmental work pollutants, and other related factors.
3.3. Association between Telomere Length and Sleep
In this systematic review, we analyzed 11 articles on the association between TL and sleep (Table 6) [43,128,129,130,131,132,133,134,135,136,137]. In comparison with the other considered lifestyle factors in this review (PA and tobacco smoking), very few studies focused on sleep. The influence of sleep quality and sleep disorders on aging and on physical and mental health has been recognized more recently [138,139]. In general, aging is associated with poor sleep. Sleep quantity and efficiency vary across the lifespan, sleep duration being shorter, and sleep efficiency being lower at older ages; these difficulties worsen after 60 years, and with some differences between men and women [139,140,141]. Sex-specific differences are complex and vary by outcome [140]. A recent review including 1.1 million people from the Netherlands, United Kingdom and United States, noted that women aged 41 years and older, despite self-reporting shorter sleep duration and lower sleep efficiency than men, had longer and more efficient sleep objectively measured by actigraphy [142], suggesting that the studies analyzing the association between sleep and TL should consider this heterogeneity. Currently there is a great scarcity of intervention trials on this issue.
All but one study identified for this review were observational (Table 6). Moreover, data from the intervention study only analyzed associations between sleep and TL cross-sectionally at baseline [132]. Only one study [135] had longitudinal data. Ten articles measured TL using PCR and 1/11 used southern blot [129]. Similarly, most studies have relied on self-reported sleep characteristics, with only two studies assessing objective data (polysomnography, actigraphy, etc.) [131,134], contributing to a low evidence level. Furthermore, even when self-reported sleep characteristics were assessed by questionnaires, high heterogeneity was observed. In several studies sleep quality and duration was assessed using the Pittsburgh Sleep Quality Index (PSQI). The PSQI [143], assesses sleep habits with a scale including 19 items used to derive seven component scores (sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, sleep medication and daytime dysfunction. These scores are summed to yield a “global sleep quality score”. Some used the global sleep quality score [132] to analyze the association between sleep quality and TL, while others [128] used the sleep quality sub-scale score. More heterogeneity was observed in other studies analyzing the association between the self-reported sleep quality and TL in which the PSQI was not administered [43,129,130,131,135,136,137].
Another variable commonly investigated was sleep duration. In general, this sleep characteristic was obtained by asking participants to state their average nightly sleep duration. Studies differed in their inclusion of weekend nights and in the response categories used. Some studies also analyzed the influence of insomnia or sleep disturbances on TL [129,135,136] using various questionnaires. Despite this heterogeneity, several studies found a significant association between poorer sleep quality (or sleep duration) and shorter TL [43,128,129,130,135,137]. However, several of these studies observed subgroup-specific effects. For example, Jackowska et al. [130], found an association between sleep duration and TL in men but not in women. Grieshober et al. [129] noted that the association found between longer sleep duration and longer TL in 3145 postmenopausal women from the WHIS cohort was stronger in African American than White women, and did not reach the statistical significance in White individuals when the analysis was stratified by race. Likewise, Liang et al. [43], observed a significant positive association between sleep duration and TL in the NHS. This study further uncovered a modifying effect of age, such that sleep duration was only associated with TL in women younger than 50. Differences by age were also observed by Cribbet et al., [128], but in the opposite direction.

Table 6.
Summary of studies on sleep and TL.
Table 6.
Summary of studies on sleep and TL.
| Author, Reference | Year | Type of Study | Participants | TL Measurements | Tissue for TL Analysis | Exposure Assessment Methods | Results |
|---|---|---|---|---|---|---|---|
| Cribbet et al. [128] | 2014 | Cross-sectional | 154 subjects (45–77 y) | PCR | Blood | Sleep quality and duration by questionnaire (PSQI) | Better quality of sleep was significantly associated with longer TL. Sleep durations of >7 h/night or ≤5 h/night associated with shorter TL in older adults. Sleep duration in middle-aged adults was not associated with TL |
| Grieshober et al. [129] | 2019 | Cross-sectional | 3145 post-menopausal women (EA, AA) from the WHIS | SB | Blood | Sleep duration and sleep disturbance by questionnaires (WHIIRS) | Longer TL was associated with longer sleep duration in the whole sample (associations being strongest among AA). No associations were observed with sleep disturbances |
| Jackowska et al. [130] | 2012 | Cross-sectional | 494 men and women (mean age 63.3 y) from the WIIS | PCR | Blood | Sleep duration assessed by interview | Sleep duration was associated with TL in men, but not in women. TL was 6% shorter in men who sleep ≤5 h/night compared to >7 h/night |
| Liang et al. [43] | 2011 | Cross-sectional | 4117 women from the NHS | PCR | Blood | Sleep duration and rotating night shifts assessed by questionnaires | Sleep duration was associated with TL (compared to women in the 9 h/night, those in the <6 h/night category, had decreased TL). However, heterogeneity by age was observed (sleep duration and TL were only associated in women <50 y, and not older). No significant associations were found between rotating shift history and TL |
| Nguyen et al. [131] | 2020 | Cross-sectional | 1070 parents/careers with a (mean age 44 y), from the LSAC | PCR | Blood | Sleep behavior determined by interview and actigraphy over 8 d | Sleep duration and most other sleep metrics were not associated with TL |
| Prather et al. [132] | 2015 | Cross-sectional | 87 obese adults from a trial (San Francisco, CA) at baseline | PCR (DTC) | Blood | Sleep quality and duration by questionnaire (PSQI) | Poorer global sleep quality was associated with shorter TL in lymphocytes, but not in granulocytes. Sleep duration was not related to TL |
| Prather et al. [133] | 2011 | Cross-sectional | 245 women (49 to 66 y) | PCR | Blood | Sleep quality and duration by questionnaire (adapted from the PSQI) | Lower sleep quality was associated to shorter TL |
| Tempaku et al. [134] | 2018 | Cross-sectional | 925 participants from EPISONO cohort | PCR | Blood | Sleep quality and duration assessed by questionnaires (PSQI, UNIFESP, Epworth, ISI, PSPDN), and polysomnography | Insomnia disorders and long sleepers were associated with shorter TL |
| Wynchank et al. [135] | 2019 | Longitudinal | 2936 European subjects from the NSDA analyzed at two waves 6 y apart | PCR | Blood | Sleep duration and insomnia symptoms by questionnaire (ISR). Chronotype determined by the MCTQ | Indicators of delayed circadian rhythm, Late MSFsc, late sleep onset time, and moderately late chronotype, were associated with shorter TL at both waves. No predictors showed accelerated TL attrition over 6 y. Sleep duration and insomnia were not associated with TL |
| Zgheib et al. [136] | 2018 | Cross-sectional | 497 Lebanese (men and women >18 y) | PCR | Blood | Sleep habits determined by questionnaire (3 questions) | Difficulties to sleep (but not short sleep duration) were associated with shorter TL |
| Zhao H [137] | 2017 | Cross-sectional | 12,178 Mexican Americans (20–85 y, 80% women) from the MM:MACS | PCR | Blood | Sleep duration determined by questionnaire | TL was associated with sleeping time per d (longer in those participants who slept at least 9 h/d, followed by those who slept between 7–8 h/d, and shortest in those who slept ≤6 h/d) |
TL: telomere length; bp: base pairs; y: years old; h: hour; d: day; y: year; PCR: Polymerase Chain Reaction; PSQI: Pittsburgh Sleep Quality Index; EA: European-American; AA. African-American; WHI: Women’s Health Initiative Objective Physical Activity and Cardio-vascular Health study; WHIIRS: “Women’s Health Initiative” Insomnia Rating Scale; WIIS: Whitehall II study; NHS: Nurses’ Health Study; LSAC: Longitudinal Study of Australian Children; EPISONO: São Paulo Epidemiologic Sleep Study; DTC: PCR in different type of cells; UNIFESP: “Universidade Federal De São Paulo” (UNIFESP) Sleep Questionnaire; Epworth: Epworth Sleepiness Scale; ISI: Insomnia Severity Index; PSPDN: Pre-Sleep–Previous Day and Night; NSDA: Netherlands Study of Depression and Anxiety; ISR: Insomnia Rating Scale; MCTQ: Munich Chronotype Questionnaire; MSFsc: Lack of sleep on days off; MM:MACS: Mano a Mano: Mexican American Cohort Study.
In this population [128], sleep duration was associated with TL only in older, but not in middle-aged, adults. In addition, mixed results were reported on the effect of long sleep on TL (U-shaped or linear effect). For example, Zhao et al. [137], observed longer TL in Mexican Americans who reported sleeping at least 9 h/night, whereas Tempaku et al. [134] in Brazil, observed associations between longer sleep and shorter TL. Cribbet et al. [128] also described a U-shaped association between sleep duration and TL, with the extreme of sleep duration having the shortest TL. Interestingly, in one study examining TL in different types of leukocytes [132], poorer global sleep quality was associated with shorter TL in lymphocytes, but not in granulocytes. This is the only study analyzing the sleep influence in different cell types and additional studies are needed to better understand this relationship. Furthermore, Nguyen et al. [131], using objective measures of sleep (actigraphy), did not find any association between sleep duration, and most other sleep metrics, and TL.
Only one study was identified that assessed the relation between chronotype and TL [135]. Individuals with an evening chronotype had a shorter TL. However, when longitudinal analyses were performed, chronotype did not predict changes in TL. Overall, despite many observational studies reported associations between self-reported sleep duration and sleep quality and TL, these results are mainly cross-sectional, limiting the ability to draw causal inference. More longitudinal and intervention studies are needed to increase our understanding on how poor sleep characteristics affects TL.
4. Discussion
This systematic review evaluated the current evidence on the influence of three relevant lifestyle factors (PA, tobacco smoking and sleep characteristics) on TL in adults. In the selected studies on TL, PA was the most studied lifestyle factor, followed by smoking and sleep. In general, being physical active, not smoking and having good sleep quality are associated with a reduced risk of morbimortality for the main chronic diseases [8,9,10,11,144,145,146,147]. There is a challenge in searching for the best biomarker of aging and despite these limitations and the advantage of measuring a combination of biomarkers instead of only one [148,149], TL is the most extensively studied biomarker of age-related diseases [7,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. In this regard, many results have been obtained focusing on the association between TL, aging, cardiovascular diseases, diabetes, obesity and mortality [35,36,37,38,39,40,148,149]. Therefore, the demonstration of an effect of these lifestyle factors on TL could provide important information on the mechanisms by which these factors have protective health effects, as well as providing evidence to validate TL as a good biomarker of aging with a good capacity to capture healthy lifestyle interventions based on these factors.
However, we have detected that the evidence level of the results obtained on the association among these lifestyle factors and TL is low, these being mainly based on cross-sectional studies. Thus, in this review, no intervention studies were detected analyzing the effect of sleep characteristics on TL. Likewise, due to ethical limitations, no experimental publications have analyzed the effects of tobacco smoking on TL on humans. Regarding PA, there are several intervention studies (12/49) examining the effect of different PA intervention on TL. However, the complexity of the PA interventions hinders comparison between publications and precludes definitive conclusions. Moreover, there is a scarcity of longitudinal studies for all three lifestyle factors. In addition, most of the articles have relied on the self-reported measurement of PA, smoking or sleep parameters, instead of using objective determinations (accelerometers, plasma/urine cotinine, actigraphy, respectively, among others). Moreover, substantial heterogeneity existed across the review studies for several study parameters including sample size and statistical power, participant characteristics (sex, age-group, ethnicity, etc.); biological sample and method used to analyze TL (although in general TL was measured by PCR in leukocytes isolated from blood); and statistical control for potential confounders (adjustment for anthropometric and other lifestyle factors). All of this may contribute to the variations in observed results.
Despite the low-level of scientific evidence provided by the cross-sectional studies analyzed for the three lifestyle factors, and the fact that we cannot discuss the associations in terms of causality, in general, most studies [43,44,46,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137] have reported (for the whole population or at the subgroup level) that physically active individuals have longer TL; that tobacco smoking is associated with shorter TL; and that a poor sleep quality and duration were related to shorter TL. Some studies have postulated several mechanisms by which PA may have an effect on TL. It is speculated that exercise can induce different signaling mechanisms, either epigenetic or transcriptomic [69,150]. Chilton et al. [151], in a comprehensive review on the relationship between exercise, aging and telomeres in human and animal models discussed the lack of good evidence at the mechanistic level to support this association, but suggested reductions in oxidative stress and inflammation as potential mediators. As noted in this systematic review, the optimum amount and the type of PA for maintaining TL remains under debate. Lack of agreement among studies could result from different factors, such as: time—need for interventions longer than 12 months to see the long-term effect of PA on telomeres; variability in trials—major random error and consequent lower precision in estimating the effect and low statistical power in the intervention studies due to the complexity of the intervention; or specific characteristics of the participant that could hinder the protective effect of exercise on telomeres [99]. In addition, a U-shaped relationship is thought to exist between endurance exercise and the regenerative capacity of skeletal muscle [72,89]. The possible negative effect on TL of high intensity exercise could be due to an inducing oxidative stress through an increase in reactive oxygen metabolites and free radicals [150].
Tobacco is one of the main risk factors for cardiovascular events and mortality. In addition, those who start smoking at an early age and continue during adulthood lose a decade of life expectancy compared to never smokers [152]. Tobacco smoking is a source of free radicals and oxidants that increase inflammatory response and oxidative stress [111,119,153]. Both processes could increase telomere shortening, contributing to the acceleration of aging and possibly an increased risk of age-related diseases [115,119,120,125]. Although several cross-sectional studies have reported an inverse association between tobacco smoking and TL, evidence for the causality of this association is low and several confounding factors may play a role.
Finally, interest in analyzing sleep and health status has increased in recent years. The relation between short and long sleep with numerous cardiometabolic pathologies has been studied, and a U-shaped association has been demonstrated [154,155]. However, some inconclusive results exist due to uncertainties in self-reported sleep characteristics, different methodological designs and the different populations analyzed [154,155,156]. Furthermore, the sleep process is highly affected during aging, and elderly individuals suffer the greatest disturbances in their sleep patterns [157]. Several authors claim that aging or the presence of other comorbidities could be the cause of the association found between sleep and TL [131,136]. Our systematic review suggests that there is a possible association between shorter TL and various sleep-related parameters, but without establishing a causal relationship between the two factors. Therefore, more longitudinal and intervention studies on sleep and TL are needed. The methodological differences in the evaluation of sleep and TL increase the inconsistency in the results obtained.
In general, a great number of studies analyzed for PA, smoking and sleep reported statistically significant results in subgroup analysis. These associations may be false positive associations due to multiple comparisons or real associations based on heterogeneous effects such as the previously described differences per sex [158] or per age groups [139]. Furthermore, the beneficial effect of PA, non-smoking, or quality sleep on TL may be due to the interaction between various lifestyle factors, such as those studied in this systematic review, or even with others (diet, educational level, etc.), and more studies are needed to assess the role of healthy lifestyle factor combinations in diverse populations.
5. Conclusions
The results obtained in this systematic review show that the influence of PA, smoking, and sleep on TL of adults is mixed, and depends on the type of study, population analyzed, and methodology (study design, exposure and TL assessment, subgroup analysis, etc.). The evidence level of the associations is very low due to the cross-sectional nature of the studies. Future research using prospective and well-powered intervention trials with standardized protocols and objective measures is needed. Despite these limitations, current studies suggest a low-evidence level association between moderate, regular, and daily non-sedentary activities and longer TL. Likewise, not smoking and having optimal sleep duration (7 h) and quality, are associated with longer TL. Further research is needed to improve design and reduce heterogeneity and to consider the diversity by sex, age, ethnic groups, and other lifestyle characteristics.
Author Contributions
Conceptualization (initiated the idea of this review and participated in the study design), R.B., J.V.S., E.M.A. and D.C.; methodology, R.B., C.O.-A. and J.V.S.; formal analysis, R.B., C.O.-A., J.V.S., E.M.A. and O.P.; resources, D.C.; writing original draft preparation, R.B.; writing—review and editing, C.O.-A., J.V.S., O.C., M.-P.S.-O. and D.C.; supervision, D.C.; funding acquisition, J.V.S. and D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was partially funded by the Conselleria de Innovación, Universidades, Ciencia y Sociedad Digital de la Generalitat Valenciana (grants PROMETEO 17/2017, PROMETEO 21/2021 and APOSTD/2019/136); and the Spanish Ministry of Health (Instituto de Salud Carlos III) and the Ministerio de Economía y Competitividad-Fondo Europeo de Desarrollo Regional (FEDER) (grants PI19/00781 and SAF2016–80532-R). This study is also supported by the grant PID2019-108858RB-I00 funded by AEI 10.13039/501100011033 and by “ERDF A way of making Europe”; and the University Jaume I (grant UJI-B2018-69). The APC was funded by the University of Valencia.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abdellatif, M.; Sedej, S.; Carmona-Gutierrez, D.; Madeo, F.; Kroemer, G. Autophagy in Cardiovascular Aging. Circ. Res. 2018, 123, 803–824. [Google Scholar] [CrossRef]
- Johnson, N.B.; Hayes, L.D.; Brown, K.; Hoo, E.C.; Ethier, K.A.; Centers for Disease Control and Prevention (CDC). CDC National Health Report: Leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013. MMWR Suppl. 2014, 63, 3–27. [Google Scholar] [PubMed]
- North, B.J.; Sinclair, D.A. The intersection between aging and cardiovascular disease. Circ. Res. 2012, 110, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Paneni, F.; Diaz Canestro, C.; Libby, P.; Luscher, T.F.; Camici, G.G. The Aging Cardiovascular System: Understanding It at the Cellular and Clinical Levels. J. Am. Coll. Cardiol. 2017, 69, 1952–1967. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Pesce, M. Stiffness and Aging in Cardiovascular Diseases: The Dangerous Relationship between Force and Senescence. Int. J. Mol. Sci. 2021, 22, 3404. [Google Scholar] [CrossRef]
- Strait, J.B.; Lakatta, E.G. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail. Clin. 2012, 8, 143–164. [Google Scholar] [CrossRef]
- Wagner, K.H.; Cameron-Smith, D.; Wessner, B.; Franzke, B. Biomarkers of Aging: From Function to Molecular Biology. Nutrients 2016, 8, 338. [Google Scholar] [CrossRef] [PubMed]
- Ismail, L.; Materwala, H.; Al Kaabi, J. Association of risk factors with type 2 diabetes: A systematic review. Comput. Struct. Biotechnol. J. 2021, 19, 1759–1785. [Google Scholar] [CrossRef]
- Zhu, B.; Bronas, U.G.; Fritschi, C. Sleep assessment in aging adults with type 2 diabetes: Agreement between actigraphy and sleep diaries. Sleep Med. 2018, 46, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Buford, T.W. Hypertension and aging. Ageing Res. Rev. 2016, 26, 96–111. [Google Scholar] [CrossRef]
- Fan, Z.Y.; Yang, Y.; Zhang, C.H.; Yin, R.Y.; Tang, L.; Zhang, F. Prevalence and Patterns of Comorbidity among Middle-Aged and Elderly People in China: A Cross-Sectional Study Based on CHARLS Data. Int. J. Gen. Med. 2021, 14, 1449–1455. [Google Scholar] [CrossRef] [PubMed]
- Higashi, Y.; Kihara, Y.; Noma, K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012, 35, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Berben, L.; Floris, G.; Wildiers, H.; Hatse, S. Cancer and Aging: Two Tightly Interconnected Biological Processes. Cancers 2021, 13, 1400. [Google Scholar] [CrossRef]
- Cano, A.; Turowski, P.; Ettcheto, M.; Duskey, J.T.; Tosi, G.; Sanchez-Lopez, E.; Garcia, M.L.; Camins, A.; Souto, E.B.; Ruiz, A.; et al. Nanomedicine-based technologies and novel biomarkers for the diagnosis and treatment of Alzheimer’s disease: From current to future challenges. J. Nanobiotechnol. 2021, 19, 122. [Google Scholar] [CrossRef]
- Fahy, G.M.; Brooke, R.T.; Watson, J.P.; Good, Z.; Vasanawala, S.S.; Maecker, H.; Leipold, M.D.; Lin, D.T.S.; Kobor, M.S.; Horvath, S. Reversal of epigenetic aging and immunosenescent trends in humans. Aging Cell 2019, 18, e13028. [Google Scholar] [CrossRef] [PubMed]
- Freitas-Simoes, T.M.; Cofan, M.; Blasco, M.A.; Soberon, N.; Foronda, M.; Serra-Mir, M.; Roth, I.; Valls-Pedret, C.; Domenech, M.; Ponferrada-Ariza, E.; et al. Walnut Consumption for Two Years and Leukocyte Telomere Attrition in Mediterranean Elders: Results of a Randomized Controlled Trial. Nutrients 2018, 10, 1907. [Google Scholar] [CrossRef]
- Pataky, M.W.; Young, W.F.; Nair, K.S. Hormonal and Metabolic Changes of Aging and the Influence of Lifestyle Modifications. Mayo Clin. Proc. 2021, 96, 788–814. [Google Scholar] [CrossRef]
- Zhang, W.; Song, M.; Qu, J.; Liu, G.H. Epigenetic Modifications in Cardiovascular Aging and Diseases. Circ. Res. 2018, 123, 773–786. [Google Scholar] [CrossRef]
- Marian, A.J.; Bhatnagar, A.; Bolli, R.; Izpisua Belmonte, J.C. Introduction to Cardiovascular Aging Compendium. Circ. Res. 2018, 123, 737–739. [Google Scholar] [CrossRef]
- Falus, A.; Marton, I.; Borbenyi, E.; Tahy, A.; Karadi, P.; Aradi, J.; Stauder, A.; Kopp, M. A challenging epigenetic message: Telomerase activity is associated with complex changes in lifestyle. Cell Biol. Int. 2011, 35, 1079–1083. [Google Scholar] [CrossRef]
- Fouquerel, E.; Opresko, P.L. Convergence of The Nobel Fields of Telomere Biology and DNA Repair. Photochem. Photobiol. 2017, 93, 229–237. [Google Scholar] [CrossRef]
- Martinez, P.; Blasco, M.A. Heart-Breaking Telomeres. Circ. Res. 2018, 123, 787–802. [Google Scholar] [CrossRef] [PubMed]
- Munoz-Lorente, M.A.; Cano-Martin, A.C.; Blasco, M.A. Mice with hyper-long telomeres show less metabolic aging and longer lifespans. Nat. Commun. 2019, 10, 4723. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Pan, X.; Liu, L.; Liu, N. Telomere length maintenance, shortening, and lengthening. J. Cell Physiol. 2014, 229, 1323–1329. [Google Scholar] [CrossRef] [PubMed]
- Bekaert, S.; De Meyer, T.; Rietzschel, E.R.; De Buyzere, M.L.; De Bacquer, D.; Langlois, M.; Segers, P.; Cooman, L.; Van Damme, P.; Cassiman, P.; et al. Telomere length and cardiovascular risk factors in a middle-aged population free of overt cardiovascular disease. Aging Cell 2007, 6, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Aviv, A. Genetics of leukocyte telomere length and its role in atherosclerosis. Mutat. Res. 2012, 730, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Denham, J.; O’Brien, B.J.; Prestes, P.R.; Brown, N.J.; Charchar, F.J. Increased expression of telomere-regulating genes in endurance athletes with long leukocyte telomeres. J. Appl. Physiol. 2016, 120, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, M.; Pusceddu, I.; Marz, W.; Herrmann, W. Telomere biology and age-related diseases. Clin. Chem. Lab. Med. 2018, 56, 1210–1222. [Google Scholar] [CrossRef]
- Mons, U.; Muezzinler, A.; Schottker, B.; Dieffenbach, A.K.; Butterbach, K.; Schick, M.; Peasey, A.; De Vivo, I.; Trichopoulou, A.; Boffetta, P.; et al. Leukocyte Telomere Length and All-Cause, Cardiovascular Disease, and Cancer Mortality: Results From Individual-Participant-Data Meta-Analysis of 2 Large Prospective Cohort Studies. Am. J. Epidemiol. 2017, 185, 1317–1326. [Google Scholar] [CrossRef]
- Rizvi, S.; Raza, S.T.; Mahdi, F. Telomere length variations in aging and age-related diseases. Curr. Aging Sci. 2014, 7, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Goglin, S.E.; Farzaneh-Far, R.; Epel, E.S.; Lin, J.; Blackburn, E.H.; Whooley, M.A. Change in Leukocyte Telomere Length Predicts Mortality in Patients with Stable Coronary Heart Disease from the Heart and Soul Study. PLoS ONE 2016, 11, e0160748. [Google Scholar] [CrossRef]
- Turner, K.J.; Vasu, V.; Griffin, D.K. Telomere Biology and Human Phenotype. Cells 2019, 8, 73. [Google Scholar] [CrossRef] [PubMed]
- Brouilette, S.; Singh, R.K.; Thompson, J.R.; Goodall, A.H.; Samani, N.J. White cell telomere length and risk of premature myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 842–846. [Google Scholar] [CrossRef] [PubMed]
- Brouilette, S.W.; Moore, J.S.; McMahon, A.D.; Thompson, J.R.; Ford, I.; Shepherd, J.; Packard, C.J.; Samani, N.J.; West of Scotland Coronary Prevention Study, G. Telomere length, risk of coronary heart disease, and statin treatment in the West of Scotland Primary Prevention Study: A nested case-control study. Lancet 2007, 369, 107–114. [Google Scholar] [CrossRef]
- Carty, C.L.; Kooperberg, C.; Liu, J.; Herndon, M.; Assimes, T.; Hou, L.; Kroenke, C.H.; LaCroix, A.Z.; Kimura, M.; Aviv, A.; et al. Leukocyte Telomere Length and Risks of Incident Coronary Heart Disease and Mortality in a Racially Diverse Population of Postmenopausal Women. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 2225–2231. [Google Scholar] [CrossRef]
- De Meyer, T.; Nawrot, T.; Bekaert, S.; De Buyzere, M.L.; Rietzschel, E.R.; Andres, V. Telomere Length as Cardiovascular Aging Biomarker: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2018, 72, 805–813. [Google Scholar] [CrossRef]
- Haycock, P.C.; Heydon, E.E.; Kaptoge, S.; Butterworth, A.S.; Thompson, A.; Willeit, P. Leucocyte telomere length and risk of cardiovascular disease: Systematic review and meta-analysis. BMJ 2014, 349, g4227. [Google Scholar] [CrossRef]
- Okuda, K.; Khan, M.Y.; Skurnick, J.; Kimura, M.; Aviv, H.; Aviv, A. Telomere attrition of the human abdominal aorta: Relationships with age and atherosclerosis. Atherosclerosis 2000, 152, 391–398. [Google Scholar] [CrossRef]
- Sharifi-Sanjani, M.; Oyster, N.M.; Tichy, E.D.; Bedi, K.C., Jr.; Harel, O.; Margulies, K.B.; Mourkioti, F. Cardiomyocyte-Specific Telomere Shortening is a Distinct Signature of Heart Failure in Humans. J. Am. Heart Assoc. 2017, 6, 25211. [Google Scholar] [CrossRef]
- Willeit, P.; Willeit, J.; Brandstatter, A.; Ehrlenbach, S.; Mayr, A.; Gasperi, A.; Weger, S.; Oberhollenzer, F.; Reindl, M.; Kronenberg, F.; et al. Cellular aging reflected by leukocyte telomere length predicts advanced atherosclerosis and cardiovascular disease risk. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 1649–1656. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, E.H.; Epel, E.S.; Lin, J. Human telomere biology: A contributory and interactive factor in aging, disease risks, and protection. Science 2015, 350, 1193–1198. [Google Scholar] [CrossRef] [PubMed]
- Opresko, P.L.; Shay, J.W. Telomere-associated aging disorders. Ageing Res. Rev. 2017, 33, 52–66. [Google Scholar] [CrossRef] [PubMed]
- Liang, G.; Schernhammer, E.; Qi, L.; Gao, X.; De Vivo, I.; Han, J. Associations between rotating night shifts, sleep duration, and telomere length in women. PLoS ONE 2011, 6, e23462. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.M.; Hecksteden, A.; Morsch, A.; Zundler, J.; Wegmann, M.; Kratzsch, J.; Thiery, J.; Hohl, M.; Bittenbring, J.T.; Neumann, F.; et al. Differential effects of endurance, interval, and resistance training on telomerase activity and telomere length in a randomized, controlled study. Eur. Heart J. 2019, 40, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, E.F.; Leveille, S.G.; Wright, J.A.; Shi, L.; Camhi, S.M.; You, T. Physical Activity Domains/Recommendations and Leukocyte Telomere Length in U.S. Adults. Med. Sci. Sports Exerc. 2017, 49, 1375–1382. [Google Scholar] [CrossRef] [PubMed]
- Tucker, L.A. Physical activity and telomere length in U.S. men and women: An NHANES investigation. Prev. Med. 2017, 100, 145–151. [Google Scholar] [CrossRef]
- Crous-Bou, M.; Molinuevo, J.L.; Sala-Vila, A. Plant-Rich Dietary Patterns, Plant Foods and Nutrients, and Telomere Length. Adv. Nutr. 2019, 10, S296–S303. [Google Scholar] [CrossRef]
- Freitas-Simoes, T.M.; Ros, E.; Sala-Vila, A. Nutrients, foods, dietary patterns and telomere length: Update of epidemiological studies and randomized trials. Metabolism 2016, 65, 406–415. [Google Scholar] [CrossRef]
- Galie, S.; Canudas, S.; Muralidharan, J.; Garcia-Gavilan, J.; Bullo, M.; Salas-Salvado, J. Impact of Nutrition on Telomere Health: Systematic Review of Observational Cohort Studies and Randomized Clinical Trials. Adv. Nutr. 2020, 11, 576–601. [Google Scholar] [CrossRef]
- Marti, A.; Echeverria, R.; Morell-Azanza, L.; Ojeda-Rodriguez, A. Telomeres and diet quality. Nutr. Hosp. 2017, 34, 1226–1245. [Google Scholar] [CrossRef]
- Perez, L.M.; Amaral, M.A.; Mundstock, E.; Barbe-Tuana, F.M.; Guma, F.; Jones, M.H.; Machado, D.C.; Sarria, E.E.; Marques, E.M.M.; Preto, L.T.; et al. Effects of Diet on Telomere Length: Systematic Review and Meta-Analysis. Public Health Genom. 2017, 20, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Rafie, N.; Golpour Hamedani, S.; Barak, F.; Safavi, S.M.; Miraghajani, M. Dietary patterns, food groups and telomere length: A systematic review of current studies. Eur. J. Clin. Nutr. 2017, 71, 151–158. [Google Scholar] [CrossRef]
- Bray, N.W.; Pieruccini-Faria, F.; Bartha, R.; Doherty, T.J.; Nagamatsu, L.S.; Montero-Odasso, M. The effect of physical exercise on functional brain network connectivity in older adults with and without cognitive impairment. A systematic review. Mech. Ageing Dev. 2021, 196, 111493. [Google Scholar] [CrossRef] [PubMed]
- Duggal, N.A.; Niemiro, G.; Harridge, S.D.R.; Simpson, R.J.; Lord, J.M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat. Rev. Immunol. 2019, 19, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Harridge, S.D.; Lazarus, N.R. Physical Activity, Aging, and Physiological Function. Physiology 2017, 32, 152–161. [Google Scholar] [CrossRef]
- Jakovljevic, D.G. Physical activity and cardiovascular aging: Physiological and molecular insights. Exp. Gerontol. 2018, 109, 67–74. [Google Scholar] [CrossRef]
- Orkaby, A.R.; Forman, D.E. Physical activity and CVD in older adults: An expert’s perspective. Expert Rev. Cardiovasc. Ther. 2018, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rosique-Esteban, N.; Diaz-Lopez, A.; Martinez-Gonzalez, M.A.; Corella, D.; Goday, A.; Martinez, J.A.; Romaguera, D.; Vioque, J.; Aros, F.; Garcia-Rios, A.; et al. Leisure-time physical activity, sedentary behaviors, sleep, and cardiometabolic risk factors at baseline in the PREDIMED-PLUS intervention trial: A cross-sectional analysis. PLoS ONE 2017, 12, e0172253. [Google Scholar] [CrossRef]
- Talar, K.; Hernandez-Belmonte, A.; Vetrovsky, T.; Steffl, M.; Kalamacka, E.; Courel-Ibanez, J. Benefits of Resistance Training in Early and Late Stages of Frailty and Sarcopenia: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. J. Clin. Med. 2021, 10, 1630. [Google Scholar] [CrossRef]
- Cassidy, A.; De Vivo, I.; Liu, Y.; Han, J.; Prescott, J.; Hunter, D.J.; Rimm, E.B. Associations between diet, lifestyle factors, and telomere length in women. Am. J. Clin. Nutr. 2010, 91, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Dankel, S.J.; Loenneke, J.P.; Loprinzi, P.D. The impact of overweight/obesity duration and physical activity on telomere length: An application of the WATCH paradigm. Obes. Res. Clin. Pract. 2017, 11, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.X.; Zhang, Y.H.; Xu, X.Z.; Zhang, J.; Ming, S.U.N.; Liu, D.; Zhao, Z.Y.; Zhou, Y.; Zhang, Q.; Wang, Y.X. Association between Physical Activity and Telomere Length in a North Chinese Population: A China Suboptimal Health Cohort Study. Biomed. Environ. Sci. 2018, 31, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Prescott, J.; Kraft, P.; Han, J.; Giovannucci, E.; Hankinson, S.E.; De Vivo, I. Physical activity, sedentary behavior, and leukocyte telomere length in women. Am. J. Epidemiol. 2012, 175, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Fretts, A.M.; Mete, M.; Howard, B.V.; Best, L.G.; Siscovick, D.S.; Eilat-Adar, S.; Zhao, J. Physical activity and telomere length in American Indians: The Strong Heart Study. Eur. J. Epidemiol. 2018, 33, 497–500. [Google Scholar] [CrossRef] [PubMed]
- Hastings, W.J.; Shalev, I.; Belsky, D.W. Comparability of biological aging measures in the National Health and Nutrition Examination Study, 1999–2002. Psychoneuroendocrinology 2019, 106, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Ko, J.H.; Lee, D.C.; Lim, I.; Bang, H. Habitual physical exercise has beneficial effects on telomere length in postmenopausal women. Menopause 2012, 19, 1109–1115. [Google Scholar] [CrossRef]
- Latifovic, L.; Peacock, S.D.; Massey, T.E.; King, W.D. The Influence of Alcohol Consumption, Cigarette Smoking, and Physical Activity on Leukocyte Telomere Length. Cancer Epidemiol. Biomark. Prev. 2016, 25, 374–380. [Google Scholar] [CrossRef]
- Loprinzi, P.D. Leisure-Time Screen-Based Sedentary Behavior and Leukocyte Telomere Length: Implications for a New Leisure-Time Screen-Based Sedentary Behavior Mechanism. Mayo Clin. Proc. 2015, 90, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Loenneke, J.P.; Blackburn, E.H. Movement-Based Behaviors and Leukocyte Telomere Length among US Adults. Med. Sci. Sports Exerc. 2015, 47, 2347–2352. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Sng, E. Mode-specific physical activity and leukocyte telomere length among U.S. adults: Implications of running on cellular aging. Prev. Med. 2016, 85, 17–19. [Google Scholar] [CrossRef]
- Sassenroth, D.; Meyer, A.; Salewsky, B.; Kroh, M.; Norman, K.; Steinhagen-Thiessen, E.; Demuth, I. Sports and Exercise at Different Ages and Leukocyte Telomere Length in Later Life—Data from the Berlin Aging Study II (BASE-II). PLoS ONE 2015, 10, e0142131. [Google Scholar] [CrossRef]
- Savela, S.; Saijonmaa, O.; Strandberg, T.E.; Koistinen, P.; Strandberg, A.Y.; Tilvis, R.S.; Pitkala, K.H.; Miettinen, T.A.; Fyhrquist, F. Physical activity in midlife and telomere length measured in old age. Exp. Gerontol. 2013, 48, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Shadyab, A.H.; LaMonte, M.J.; Kooperberg, C.; Reiner, A.P.; Carty, C.L.; Manini, T.M.; Hou, L.; Di, C.; Macera, C.A.; Gallo, L.C.; et al. Leisure-time physical activity and leukocyte telomere length among older women. Exp. Gerontol. 2017, 95, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Shadyab, A.H.; Macera, C.A.; Shaffer, R.A.; Jain, S.; Gallo, L.C.; LaMonte, M.J.; Reiner, A.P.; Kooperberg, C.; Carty, C.L.; Di, C.; et al. Associations of Accelerometer-Measured and Self-Reported Sedentary Time With Leukocyte Telomere Length in Older Women. Am. J. Epidemiol. 2017, 185, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Shadyab, A.H.; LaMonte, M.J.; Kooperberg, C.; Reiner, A.P.; Carty, C.L.; Manini, T.M.; Hou, L.; Di, C.; LaCroix, A.Z. Association of Accelerometer-Measured Physical Activity With Leukocyte Telomere Length Among Older Women. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 1532–1537. [Google Scholar] [CrossRef]
- Silva, L.C.; de Araujo, A.L.; Fernandes, J.R.; Matias Mde, S.; Silva, P.R.; Duarte, A.J.; Garcez Leme, L.E.; Benard, G. Moderate and intense exercise lifestyles attenuate the effects of aging on telomere length and the survival and composition of T cell subpopulations. Age 2016, 38, 24. [Google Scholar] [CrossRef]
- Song, Z.; von Figura, G.; Liu, Y.; Kraus, J.M.; Torrice, C.; Dillon, P.; Rudolph-Watabe, M.; Ju, Z.; Kestler, H.A.; Sanoff, H.; et al. Lifestyle impacts on the aging-associated expression of biomarkers of DNA damage and telomere dysfunction in human blood. Aging Cell 2010, 9, 607–615. [Google Scholar] [CrossRef] [PubMed]
- von Kanel, R.; Bruwer, E.J.; Hamer, M.; de Ridder, J.H.; Malan, L. Association between objectively measured physical activity, chronic stress and leukocyte telomere length. J. Sports Med. Phys. Fit. 2017, 57, 1349–1358. [Google Scholar] [CrossRef]
- Williams, D.M.; Buxton, J.L.; Kantomaa, M.T.; Tammelin, T.H.; Blakemore, A.I.F.; Jarvelin, M.R. Associations of Leukocyte Telomere Length With Aerobic and Muscular Fitness in Young Adults. Am. J. Epidemiol. 2017, 185, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Xue, H.M.; Liu, Q.Q.; Tian, G.; Quan, L.M.; Zhao, Y.; Cheng, G. Television Watching and Telomere Length Among Adults in Southwest China. Am. J. Public Health 2017, 107, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
- Colon, M.; Hodgson, A.; Donlon, E.; Murphy, J.E.J. Effects of Competitive Triathlon Training on Telomere Length. J Aging Phys. Act. 2019, 27, 510–514. [Google Scholar] [CrossRef]
- Denham, J.; Nelson, C.P.; O’Brien, B.J.; Nankervis, S.A.; Denniff, M.; Harvey, J.T.; Marques, F.Z.; Codd, V.; Zukowska-Szczechowska, E.; Samani, N.J.; et al. Longer leukocyte telomeres are associated with ultra-endurance exercise independent of cardiovascular risk factors. PLoS ONE 2013, 8, e69377. [Google Scholar] [CrossRef]
- LaRocca, T.J.; Seals, D.R.; Pierce, G.L. Leukocyte telomere length is preserved with aging in endurance exercise-trained adults and related to maximal aerobic capacity. Mech. Ageing Dev. 2010, 131, 165–167. [Google Scholar] [CrossRef]
- Magi, F.; Dimauro, I.; Margheritini, F.; Duranti, G.; Mercatelli, N.; Fantini, C.; Ripani, F.R.; Sabatini, S.; Caporossi, D. Telomere length is independently associated with age, oxidative biomarkers, and sport training in skeletal muscle of healthy adult males. Free Radic. Res. 2018, 52, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Mathur, S.; Ardestani, A.; Parker, B.; Cappizzi, J.; Polk, D.; Thompson, P.D. Telomere length and cardiorespiratory fitness in marathon runners. J. Investig. Med. 2013, 61, 613–615. [Google Scholar] [CrossRef] [PubMed]
- Muniesa, C.A.; Verde, Z.; Diaz-Urena, G.; Santiago, C.; Gutierrez, F.; Diaz, E.; Gomez-Gallego, F.; Pareja-Galeano, H.; Soares-Miranda, L.; Lucia, A. Telomere Length in Elite Athletes. Int. J. Sports Physiol. Perform. 2017, 12, 994–996. [Google Scholar] [CrossRef]
- Osthus, I.B.; Sgura, A.; Berardinelli, F.; Alsnes, I.V.; Bronstad, E.; Rehn, T.; Stobakk, P.K.; Hatle, H.; Wisloff, U.; Nauman, J. Telomere length and long-term endurance exercise: Does exercise training affect biological age? A pilot study. PLoS ONE 2012, 7, e52769. [Google Scholar] [CrossRef]
- Puterman, E.; Lin, J.; Blackburn, E.; O’Donovan, A.; Adler, N.; Epel, E. The power of exercise: Buffering the effect of chronic stress on telomere length. PLoS ONE 2010, 5, e10837. [Google Scholar] [CrossRef]
- Rae, D.E.; Vignaud, A.; Butler-Browne, G.S.; Thornell, L.E.; Sinclair-Smith, C.; Derman, E.W.; Lambert, M.I.; Collins, M. Skeletal muscle telomere length in healthy, experienced, endurance runners. Eur. J. Appl. Physiol. 2010, 109, 323–330. [Google Scholar] [CrossRef]
- Simoes, H.G.; Sousa, C.V.; Dos Santos Rosa, T.; da Silva Aguiar, S.; Deus, L.A.; Rosa, E.; Amato, A.A.; Andrade, R.V. Longer Telomere Length in Elite Master Sprinters: Relationship to Performance and Body Composition. Int. J. Sports Med. 2017, 38, 1111–1116. [Google Scholar] [CrossRef]
- Soares-Miranda, L.; Imamura, F.; Siscovick, D.; Jenny, N.S.; Fitzpatrick, A.L.; Mozaffarian, D. Physical Activity, Physical Fitness, and Leukocyte Telomere Length: The Cardiovascular Health Study. Med. Sci. Sports Exerc. 2015, 47, 2525–2534. [Google Scholar] [CrossRef] [PubMed]
- Stenback, V.; Mutt, S.J.; Leppaluoto, J.; Gagnon, D.D.; Makela, K.A.; Jokelainen, J.; Keinanen-Kiukaanniemi, S.; Herzig, K.H. Association of Physical Activity With Telomere Length Among Elderly Adults-The Oulu Cohort 1945. Front. Physiol. 2019, 10, 444. [Google Scholar] [CrossRef]
- Weischer, M.; Bojesen, S.E.; Nordestgaard, B.G. Telomere shortening unrelated to smoking, body weight, physical activity, and alcohol intake: 4,576 general population individuals with repeat measurements 10 years apart. PLoS Genet. 2014, 10, e1004191. [Google Scholar] [CrossRef] [PubMed]
- Borghini, A.; Giardini, G.; Tonacci, A.; Mastorci, F.; Mercuri, A.; Mrakic-Sposta, S.; Moretti, S.; Andreassi, M.G.; Pratali, L. Chronic and acute effects of endurance training on telomere length. Mutagenesis 2015, 30, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Brandao, C.F.C.; Nonino, C.B.; de Carvalho, F.G.; Nicoletti, C.F.; Noronha, N.Y.; San Martin, R.; de Freitas, E.C.; Junqueira-Franco, M.V.M.; Marchini, J.S. The effects of short-term combined exercise training on telomere length in obese women: A prospective, interventional study. Sports Med. Open 2020, 6, 5. [Google Scholar] [CrossRef]
- Chilton, W.L.; Marques, F.Z.; West, J.; Kannourakis, G.; Berzins, S.P.; O’Brien, B.J.; Charchar, F.J. Acute exercise leads to regulation of telomere-associated genes and microRNA expression in immune cells. PLoS ONE 2014, 9, e92088. [Google Scholar] [CrossRef]
- Diman, A.; Boros, J.; Poulain, F.; Rodriguez, J.; Purnelle, M.; Episkopou, H.; Bertrand, L.; Francaux, M.; Deldicque, L.; Decottignies, A. Nuclear respiratory factor 1 and endurance exercise promote human telomere transcription. Sci. Adv. 2016, 2, e1600031. [Google Scholar] [CrossRef]
- Dimauro, I.; Sgura, A.; Pittaluga, M.; Magi, F.; Fantini, C.; Mancinelli, R.; Sgadari, A.; Fulle, S.; Caporossi, D. Regular exercise participation improves genomic stability in diabetic patients: An exploratory study to analyse telomere length and DNA damage. Sci. Rep. 2017, 7, 4137. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Wang, Q.; Ting, N.S.; Brenner, D.R.; Conroy, S.M.; McIntyre, J.B.; Mickle, A.; Courneya, K.S.; Beattie, T. Effect of a 12-month exercise intervention on leukocyte telomere length: Results from the ALPHA Trial. Cancer Epidemiol. 2018, 56, 67–74. [Google Scholar] [CrossRef]
- Laye, M.J.; Solomon, T.P.; Karstoft, K.; Pedersen, K.K.; Nielsen, S.D.; Pedersen, B.K. Increased shelterin mRNA expression in peripheral blood mononuclear cells and skeletal muscle following an ultra-long-distance running event. J. Appl. Physiol. 2012, 112, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Mason, C.; Risques, R.A.; Xiao, L.; Duggan, C.R.; Imayama, I.; Campbell, K.L.; Kong, A.; Foster-Schubert, K.E.; Wang, C.Y.; Alfano, C.M.; et al. Independent and combined effects of dietary weight loss and exercise on leukocyte telomere length in postmenopausal women. Obesity 2013, 21, E549–E554. [Google Scholar] [CrossRef] [PubMed]
- Puterman, E.; Weiss, J.; Lin, J.; Schilf, S.; Slusher, A.L.; Johansen, K.L.; Epel, E.S. Aerobic exercise lengthens telomeres and reduces stress in family caregivers: A randomized controlled trial-Curt Richter Award Paper 2018. Psychoneuroendocrinology 2018, 98, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Sjögren, P.; Fisher, R.; Kallings, L.; Svenson, U.; Roos, G.; Hellenius, M.L. Stand up for health--avoiding sedentary behaviour might lengthen your telomeres: Secondary outcomes from a physical activity RCT in older people. Br. J. Sports Med. 2014, 48, 1407–1409. [Google Scholar] [CrossRef] [PubMed]
- Zietzer, A.; Buschmann, E.E.; Janke, D.; Li, L.; Brix, M.; Meyborg, H.; Stawowy, P.; Jungk, C.; Buschmann, I.; Hillmeister, P. Acute physical exercise and long-term individual shear rate therapy increase telomerase activity in human peripheral blood mononuclear cells. Acta Physiol. 2017, 220, 251–262. [Google Scholar] [CrossRef]
- Flannagan, K.S.; Jansen, E.C.; Rozek, L.S.; Rentschler, K.M.; Roman, A.V.; Ramirez-Zea, M.; Villamor, E.; Nine Mesoamerican Countries Metabolic Syndrome Study (NiMeCoMeS) Group. Sociodemographic correlates and family aggregation of leukocyte telomere length in adults and children from Mesoamerica. Am. J. Hum. Biol. 2017, 29, e22942. [Google Scholar] [CrossRef]
- Gao, X.; Mons, U.; Zhang, Y.; Breitling, L.P.; Brenner, H. DNA methylation changes in response to active smoking exposure are associated with leukocyte telomere length among older adults. Eur. J. Epidemiol. 2016, 31, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- Huzen, J.; Wong, L.S.; van Veldhuisen, D.J.; Samani, N.J.; Zwinderman, A.H.; Codd, V.; Cawthon, R.M.; Benus, G.F.; van der Horst, I.C.; Navis, G.; et al. Telomere length loss due to smoking and metabolic traits. J. Intern. Med. 2014, 275, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.J.; Gebreab, S.Y.; Gaye, A.; Crespo, P.R.; Xu, R.; Davis, S.K. Associations of smoking indicators and cotinine levels with telomere length: National Health and Nutrition Examination Survey. Prev. Med. Rep. 2019, 15, 100895. [Google Scholar] [CrossRef] [PubMed]
- Lei, M.K.; Gibbons, F.X.; Simons, R.L.; Philibert, R.A.; Beach, S.R.H. The Effect of Tobacco Smoking Differs across Indices of DNA Methylation-Based Aging in an African American Sample: DNA Methylation-Based Indices of Smoking Capture These Effects. Genes 2020, 11, 311. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.T.; Seeboth, A.; Tsai, P.C.; Sun, D.; Quach, A.; Reiner, A.P.; Kooperberg, C.; Ferrucci, L.; Hou, L.; Baccarelli, A.A.; et al. DNA methylation-based estimator of telomere length. Aging 2019, 11, 5895–5923. [Google Scholar] [CrossRef]
- Lu, L.; Johnman, C.; McGlynn, L.; Mackay, D.F.; Shiels, P.G.; Pell, J.P. Association between exposure to second-hand smoke and telomere length: Cross-sectional study of 1303 non-smokers. Int. J. Epidemiol. 2017, 46, 1978–1984. [Google Scholar] [CrossRef] [PubMed]
- Nawrot, T.S.; Staessen, J.A.; Holvoet, P.; Struijker-Boudier, H.A.; Schiffers, P.; Van Bortel, L.M.; Fagard, R.H.; Gardner, J.P.; Kimura, M.; Aviv, A. Telomere length and its associations with oxidized-LDL, carotid artery distensibility and smoking. Front Biosci 2010, 2, 1164–1168. [Google Scholar] [CrossRef][Green Version]
- Needham, B.L.; Adler, N.; Gregorich, S.; Rehkopf, D.; Lin, J.; Blackburn, E.H.; Epel, E.S. Socioeconomic status, health behavior, and leukocyte telomere length in the National Health and Nutrition Examination Survey, 1999–2002. Soc. Sci. Med. 2013, 85, 1–8. [Google Scholar] [CrossRef]
- Patel, C.J.; Manrai, A.K.; Corona, E.; Kohane, I.S. Systematic correlation of environmental exposure and physiological and self-reported behaviour factors with leukocyte telomere length. Int. J. Epidemiol. 2017, 46, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Rode, L.; Bojesen, S.E.; Weischer, M.; Nordestgaard, B.G. High tobacco consumption is causally associated with increased all-cause mortality in a general population sample of 55,568 individuals, but not with short telomeres: A Mendelian randomization study. Int. J. Epidemiol. 2014, 43, 1473–1483. [Google Scholar] [CrossRef] [PubMed]
- Sulastri, D.; Lestari, Y.; Afriwardi; Desmawati. Relationship Between Body Composition and Smoking Habit with Telomere Length of Minangkabau Ethnicity Men, in West Sumatera, Indonesia. Pak. J. Biol. Sci. 2017, 20, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Shi, L.; Prescott, J.; Chiuve, S.E.; Hu, F.B.; De Vivo, I.; Stampfer, M.J.; Franks, P.W.; Manson, J.E.; Rexrode, K.M. Healthy lifestyle and leukocyte telomere length in U.S. women. PLoS ONE 2012, 7, e38374. [Google Scholar] [CrossRef] [PubMed]
- Verde, Z.; Reinoso-Barbero, L.; Chicharro, L.; Garatachea, N.; Resano, P.; Sanchez-Hernandez, I.; Rodriguez Gonzalez-Moro, J.M.; Bandres, F.; Santiago, C.; Gomez-Gallego, F. Effects of cigarette smoking and nicotine metabolite ratio on leukocyte telomere length. Environ. Res. 2015, 140, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Wulaningsih, W.; Serrano, F.E.; Utarini, A.; Matsuguchi, T.; Watkins, J.; Network, P.R. Smoking, second-hand smoke exposure and smoking cessation in relation to leukocyte telomere length and mortality. Oncotarget 2016, 7, 60419–60431. [Google Scholar] [CrossRef] [PubMed]
- Yun, M.; Li, S.; Yan, Y.; Zhang, T.; Bazzano, L.; He, J.; Chen, W. Suppression effect of body weight on the association between cigarette smoking and telomere length: The Bogalusa Heart Study. Aging 2019, 11, 9893–9900. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Lauderdale, D.S.; Pierce, B.L. Sex-Specific and Time-Varying Associations between Cigarette Smoking and Telomere Length among Older Adults. Am. J. Epidemiol. 2016, 184, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Bendix, L.; Thinggaard, M.; Fenger, M.; Kolvraa, S.; Avlund, K.; Linneberg, A.; Osler, M. Longitudinal changes in leukocyte telomere length and mortality in humans. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Kimura, M.; Kim, S.; Cao, X.; Srinivasan, S.R.; Berenson, G.S.; Kark, J.D.; Aviv, A. Longitudinal versus cross-sectional evaluations of leukocyte telomere length dynamics: Age-dependent telomere shortening is the rule. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Marcon, F.; Siniscalchi, E.; Andreoli, C.; Allione, A.; Fiorito, G.; Medda, E.; Guarrera, S.; Matullo, G.; Crebelli, R. Telomerase activity, telomere length and hTERT DNA methylation in peripheral blood mononuclear cells from monozygotic twins with discordant smoking habits. Environ. Mol. Mutagen. 2017, 58, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Muezzinler, A.; Mons, U.; Dieffenbach, A.K.; Butterbach, K.; Saum, K.U.; Schick, M.; Stammer, H.; Boukamp, P.; Holleczek, B.; Stegmaier, C.; et al. Smoking habits and leukocyte telomere length dynamics among older adults: Results from the ESTHER cohort. Exp. Gerontol. 2015, 70, 18–25. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Saijonmaa, O.; Tilvis, R.S.; Pitkala, K.H.; Strandberg, A.Y.; Miettinen, T.A.; Fyhrquist, F. Association of telomere length in older men with mortality and midlife body mass index and smoking. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Walters, M.S.; De, B.P.; Salit, J.; Buro-Auriemma, L.J.; Wilson, T.; Rogalski, A.M.; Lief, L.; Hackett, N.R.; Staudt, M.R.; Tilley, A.E.; et al. Smoking accelerates aging of the small airway epithelium. Respir Res. 2014, 15, 94. [Google Scholar] [CrossRef]
- Cribbet, M.R.; Carlisle, M.; Cawthon, R.M.; Uchino, B.N.; Williams, P.G.; Smith, T.W.; Gunn, H.E.; Light, K.C. Cellular aging and restorative processes: Subjective sleep quality and duration moderate the association between age and telomere length in a sample of middle-aged and older adults. Sleep 2014, 37, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Grieshober, L.; Wactawski-Wende, J.; Hageman Blair, R.; Mu, L.; Liu, J.; Nie, J.; Carty, C.L.; Hale, L.; Kroenke, C.H.; LaCroix, A.Z.; et al. A Cross-Sectional Analysis of Telomere Length and Sleep in the Women’s Health Initiative. Am. J. Epidemiol. 2019, 188, 1616–1626. [Google Scholar] [CrossRef]
- Jackowska, M.; Hamer, M.; Carvalho, L.A.; Erusalimsky, J.D.; Butcher, L.; Steptoe, A. Short sleep duration is associated with shorter telomere length in healthy men: Findings from the Whitehall II cohort study. PLoS ONE 2012, 7, e47292. [Google Scholar] [CrossRef]
- Nguyen, M.T.; Lycett, K.; Olds, T.; Matricciani, L.; Vryer, R.; Ranganathan, S.; Burgner, D.; Saffery, R.; Wake, M. Objectively measured sleep and telomere length in a population-based cohort of children and midlife adults. Sleep 2020, 43, zsz200. [Google Scholar] [CrossRef]
- Prather, A.A.; Gurfein, B.; Moran, P.; Daubenmier, J.; Acree, M.; Bacchetti, P.; Sinclair, E.; Lin, J.; Blackburn, E.; Hecht, F.M.; et al. Tired telomeres: Poor global sleep quality, perceived stress, and telomere length in immune cell subsets in obese men and women. Brain Behav. Immun. 2015, 47, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Prather, A.A.; Puterman, E.; Lin, J.; O’Donovan, A.; Krauss, J.; Tomiyama, A.J.; Epel, E.S.; Blackburn, E.H. Shorter leukocyte telomere length in midlife women with poor sleep quality. J. Aging Res. 2011, 2011, 721390. [Google Scholar] [CrossRef]
- Tempaku, P.; Hirotsu, C.; Mazzotti, D.; Xavier, G.; Maurya, P.; Brietzke, E.; Belangero, S.; Poyares, D.; Bittencourt, L.; Tufik, S. Long Sleep Duration, Insomnia, and Insomnia With Short Objective Sleep Duration Are Independently Associated with Short Telomere Length. J. Clin. Sleep Med. 2018, 14, 2037–2045. [Google Scholar] [CrossRef]
- Wynchank, D.; Bijlenga, D.; Penninx, B.W.; Lamers, F.; Beekman, A.T.; Kooij, J.J.S.; Verhoeven, J.E. Delayed sleep-onset and biological age: Late sleep-onset is associated with shorter telomere length. Sleep 2019, 42, zsz139. [Google Scholar] [CrossRef]
- Zgheib, N.K.; Sleiman, F.; Nasreddine, L.; Nasrallah, M.; Nakhoul, N.; Isma’eel, H.; Tamim, H. Short Telomere Length is Associated with Aging, Central Obesity, Poor Sleep and Hypertension in Lebanese Individuals. Aging Dis. 2018, 9, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Han, L.; Chang, D.; Ye, Y.; Shen, J.; Daniel, C.R.; Gu, J.; Chow, W.-H.; Wu, X. Social-Demographics, Health Behaviors, and Telomere Length in the Mexican American Mano a Mano Cohort. Oncotarget 2017, 8, 96553–96567. [Google Scholar] [CrossRef]
- Sella, E.; Miola, L.; Toffalini, E.; Borella, E. The Relationship between Sleep Quality and Quality of Life in Aging: A Systematic Review and Meta-Analysis. Health Psychol. Rev. 2021, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Taillard, J.; Gronfier, C.; Bioulac, S.; Philip, P.; Sagaspe, P. Sleep in Normal Aging, Homeostatic and Circadian Regulation and Vulnerability to Sleep Deprivation. Brain Sci. 2021, 11, 1003. [Google Scholar] [CrossRef]
- Carrier, J.; Semba, K.; Deurveilher, S.; Drogos, L.; Cyr-Cronier, J.; Lord, C.; Sekerovick, Z. Sex Differences in Age-Related Changes in the Sleep-Wake Cycle. Front. Neuroendocrinol. 2017, 47, 66–85. [Google Scholar] [CrossRef]
- Evans, M.A.; Buysse, D.J.; Marsland, A.L.; Wright, A.G.C.; Foust, J.; Carroll, L.W.; Kohli, N.; Mehra, R.; Jasper, A.; Srinivasan, S.; et al. Meta-Analysis of Age and Actigraphy-Assessed Sleep Characteristics across the Lifespan. Sleep 2021, 44, zsab088. [Google Scholar] [CrossRef]
- Kocevska, D.; Lysen, T.S.; Dotinga, A.; Koopman-Verhoeff, M.E.; Luijk, M.P.C.M.; Antypa, N.; Biermasz, N.R.; Blokstra, A.; Brug, J.; Burk, W.J.; et al. Sleep Characteristics across the Lifespan in 1.1 Million People from the Netherlands, United Kingdom and United States: A Systematic Review and Meta-Analysis. Nat. Hum. Behav. 2021, 5, 113–122. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Ye, L.; Elstgeest, L.E.M.; Zhang, X.; Alhambra-Borrás, T.; Tan, S.S.; Raat, H. Factors Associated with Physical, Psychological and Social Frailty among Community-Dwelling Older Persons in Europe: A Cross-Sectional Study of Urban Health Centres Europe (UHCE). BMC Geriatr. 2021, 21, 422. [Google Scholar] [CrossRef]
- Tsai, M.-C.; Yeh, T.-L.; Hsu, H.-Y.; Hsu, L.-Y.; Lee, C.-C.; Tseng, P.-J.; Chien, K.-L. Comparison of Four Healthy Lifestyle Scores for Predicting Cardiovascular Events in a National Cohort Study. Sci. Rep. 2021, 11, 22146. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Mattei, J.; Cook, N.R.; Hu, F.B.; Willett, W.C.; Chiuve, S.E.; Rimm, E.B.; Sesso, H.D. Association Between a 20-Year Cardiovascular Disease Risk Score Based on Modifiable Lifestyles and Total and Cause-Specific Mortality Among US Men and Women. J. Am. Heart Assoc. 2018, 7, e010052. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, G.; Ray, D.W. Sleep, Circadian Rhythms, and Type 2 Diabetes Mellitus. Clin. Endocrinol. 2021, 96, 12–20. [Google Scholar] [CrossRef]
- Lohman, T.; Bains, G.; Berk, L.; Lohman, E. Predictors of Biological Age: The Implications for Wellness and Aging Research. Gerontol. Geriatr. Med. 2021, 7. [Google Scholar] [CrossRef]
- Gruber, H.-J.; Semeraro, M.D.; Renner, W.; Herrmann, M. Telomeres and Age-Related Diseases. Biomedicines 2021, 9, 1335. [Google Scholar] [CrossRef]
- Rostron, B.L.; Chang, C.M.; Pechacek, T.F. Estimation of cigarette smoking-attributable morbidity in the United States. JAMA Intern. Med. 2014, 174, 1922–1928. [Google Scholar] [CrossRef] [PubMed]
- Chilton, W.; O’Brien, B.; Charchar, F. Telomeres, Aging and Exercise: Guilty by Association? Int. J. Mol. Sci. 2017, 18, 2573. [Google Scholar] [CrossRef]
- Von Zglinicki, T.; Pilger, R.; Sitte, N. Accumulation of single-strand breaks is the major cause of telomere shortening in human fibroblasts. Free Radic. Biol. Med. 2000, 28, 64–74. [Google Scholar] [CrossRef]
- Grandner, M.A. Sleep, Health, and Society. Sleep Med. Clin. 2017, 12, 1–22. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P. Sleep-obesity relation: Underlying mechanisms and consequences for treatment. Obes. Rev. 2017, 18 (Suppl. 1), 34–39. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E.; Yorifuji, T.; Ueshima, K.; Takao, S.; Sugiyama, M.; Ohta, T.; Ishikawa-Takata, K.; Doi, H. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: A population-based cohort study. Prev. Med. 2009, 49, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Tempaku, P.F.; Mazzotti, D.R.; Tufik, S. Telomere length as a marker of sleep loss and sleep disturbances: A potential link between sleep and cellular senescence. Sleep Med. 2015, 16, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Lotfi, R.A.; El Zawahry, K.M.; Kamar, Z.A.; Hashem, Z. Effects of smoking on human telomerase reverse transcriptase expression in the skin. Int. J. Dermatol. 2014, 53, 1205–1212. [Google Scholar] [CrossRef]
- Gardner, M.; Bann, D.; Wiley, L.; Cooper, R.; Hardy, R.; Nitsch, D.; Martin-Ruiz, C.; Shiels, P.; Sayer, A.A.; Barbieri, M.; et al. Gender and Telomere Length: Systematic Review and Meta-Analysis. Exp. Gerontol. 2014, 51, 15–27. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).