Imaging Predictive Factors of Abdominal Aortic Aneurysm Growth
Abstract
1. Introduction
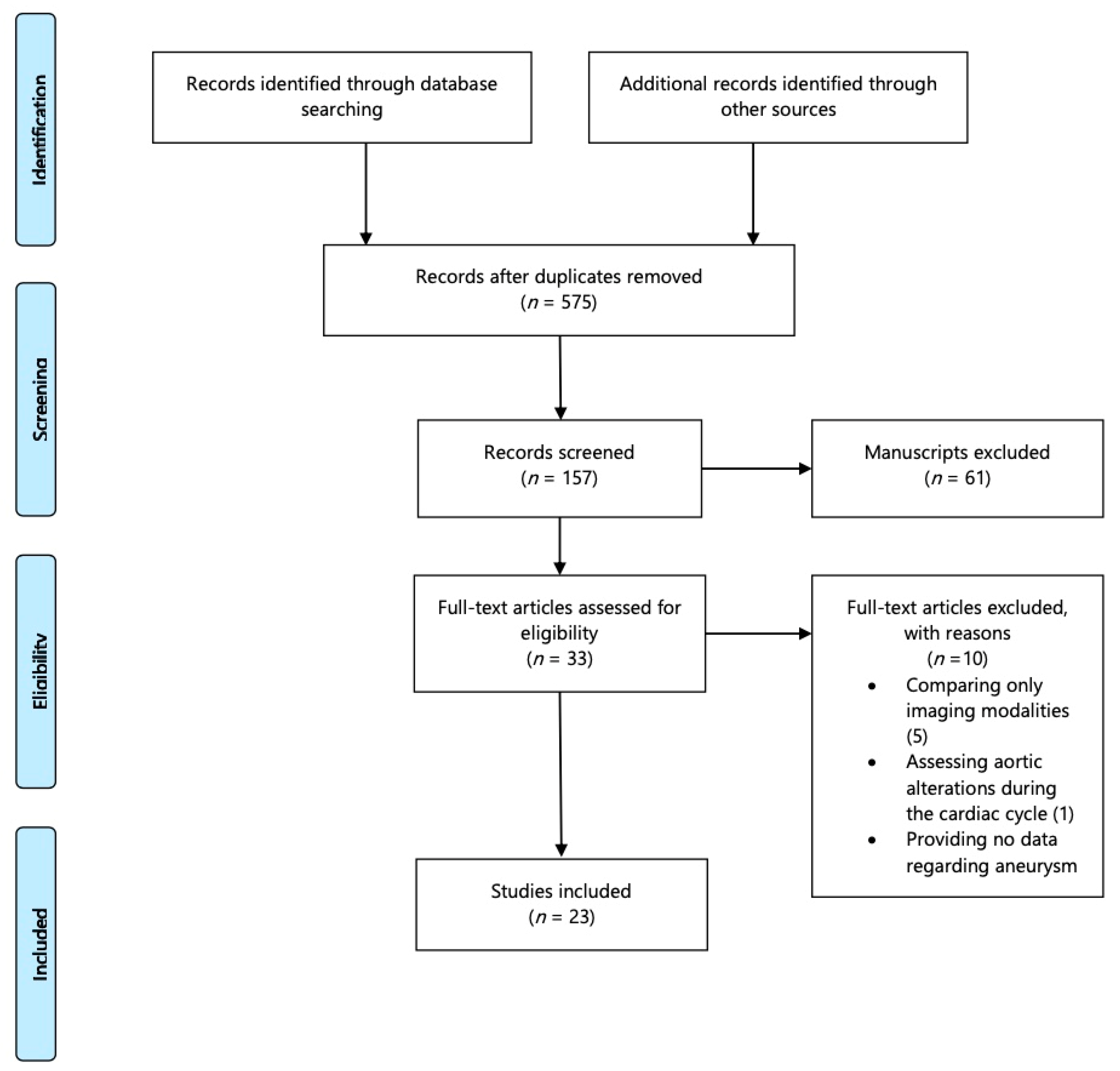
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data extraction and Quality Assessment
2.4. Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Wanhainen, A.; Mani, K.; Golledge, J. Surrogate Markers of Abdominal Aortic Aneurysm Progression. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Sweeting, M.J.; Thompson, S.G.; Brown, L.C.; Powell, J.T.; RESCAN collaborators. Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br. J. Surg. 2012, 99, 655–665. [Google Scholar] [CrossRef]
- Yu, J.; Liu, S.; Huang, J.; Wang, W. Current Theories and Clinical Trial Evidence for Limiting Human Abdominal Aortic Aneurysm Growth. Curr. Drug Targets 2018, 19, 1302–1308. [Google Scholar] [CrossRef] [PubMed]
- Salata, K.; Syed, M.; Hussain, M.A.; de Mestral, C.; Greco, E.; Mamdani, M.; Tu, J.V.; Forbes, T.L.; Bhatt, D.L.; Verma, S.; et al. Statins Reduce Abdominal Aortic Aneurysm Growth, Rupture, and Perioperative Mortality: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2018, 7, e008657. [Google Scholar] [CrossRef]
- Salata, K.; Syed, M.; Hussain, M.A.; Eikelboom, R.; de Mestral, C.; Verma, S.; Al-Omran, M. Renin-angiotensin system blockade does not attenuate abdominal aortic aneurysm growth, rupture rate, or perioperative mortality after elective repair. J. Vasc. Surg. 2018, 67, 629–636.e2. [Google Scholar] [CrossRef]
- Sun, J.; Deng, H.; Zhou, Z.; Xiong, X.; Gao, L. Endothelium as a Potential Target for Treatment of Abdominal Aortic Aneurysm. Oxid. Med. Cell. Longev. 2018, 2018, 6306542. [Google Scholar] [CrossRef]
- Itoga, N.K.; Rothenberg, K.A.; Suarez, P.; Ho, T.V.; Mell, M.W.; Xu, B.; Curtin, C.M.; Dalman, R.L. Metformin prescription status and abdominal aortic aneurysm disease progression in the U.S. veteran population. J. Vasc. Surg. 2019, 69, 710–716.e3. [Google Scholar] [CrossRef]
- Baxter, B.T.; Matsumura, J.; Curci, J.A.; McBride, R.; Larson, L.; Blackwelder, W.; Lam, D.; Wijesinha, M.; Terrin, M.; N-TA3CT Investigators. Effect of Doxycycline on Aneurysm Growth Among Patients With Small Infrarenal Abdominal Aortic Aneurysms: A Randomized Clinical Trial. JAMA 2020, 323, 2029–2038. [Google Scholar] [CrossRef]
- Montgomery, W.G.; Spinosa, M.D.; Cullen, J.M.; Salmon, M.D.; Su, G.; Hassinger, T.; Sharma, A.K.; Lu, G.; Fashandi, A.; Ailawadi, G.; et al. Tamsulosin attenuates abdominal aortic aneurysm growth. Surgery 2018, 164, 1087–1092. [Google Scholar] [CrossRef]
- Golledge, J.; Norman, P.E.; Murphy, M.P.; Dalman, R.L. Challenges and opportunities in limiting abdominal aortic aneurysm growth. J. Vasc. Surg. 2017, 65, 225–233. [Google Scholar] [CrossRef]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e2. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- The University Illinois at Chicago, What Is the PICO Model? Available online: http://researchguides.uic.edu/c.php?g=252338&p=1683349 (accessed on 23 March 2021).
- The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 23 March 2021).
- Wolf, Y.G.; Thomas, W.S.; Brennan, F.J.; Goff, W.G.; Sise, M.J.; Bernstein, E.F. Computed tomography scanning findings associated with rapid expansion of abdominal aortic aneurysms. J. Vasc. Surg. 1994, 20, 529–535, discussion 535–538. [Google Scholar] [CrossRef][Green Version]
- Faggioli, G.L.; Stella, A.; Gargiulo, M.; Tarantini, S.; D’Addato, M.; Ricotta, J.J. Morphology of small aneurysms: Definition and impact on risk of rupture. Am. J. Surg. 1994, 168, 131–135. [Google Scholar] [CrossRef]
- Veldenz, H.C.; Schwarcz, T.H.; Endean, E.D.; Pilcher, D.B.; Dobrin, P.B.; Hyde, G.L. Morphology predicts rapid growth of small abdominal aortic aneurysms. Ann. Vasc. Surg. 1994, 8, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Kurvers, H.; Veith, F.J.; Lipsitz, E.C.; Ohki, T.; Gargiulo, N.J.; Cayne, N.S.; Suggs, W.; Timaran, C.; Kwon, G.; Rhee, S.; et al. Discontinuous, staccato, growth of abdominal aortic aneurysms. J. Am. Coll. Surg. 2004, 199, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Lindholt, J.S. Aneurysmal wall calcification predicts natural history of small abdominal aortic aneurysms. Atherosclerosis 2008, 197, 673–678. [Google Scholar] [CrossRef]
- Speelman, L.; Hellenthal, F.A.; Pulinx, B.; Bosboom, E.M.; Breeuwer, M.; van Sambeek, M.R.; van de Vossea, F.N.; Jacobs, M.J.; Wodzig, W.K.W.H.; Schurink, G.W.H. The influence of wall stress on AAA growth and biomarkers. J. Vasc. Endovasc. Surg. 2010, 39, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Badger, S.A.; Jones, C.; McClements, J.; Lau, L.L.; Young, I.S.; Patterson, C.C. Surveillance strategies according to the rate of growth of small abdominal aortic aneurysms. Vasc. Med. 2011, 16, 415–421. [Google Scholar] [CrossRef]
- Shang, E.K.; Nathan, D.P.; Woo, E.Y.; Fairman, R.M.; Wang, G.J.; Gorman, R.C.; Gorman, J.H., III; Jackson, B.M. Local wall thickness in finite element models improves prediction of abdominal aortic aneurysm growth. J. Vasc. Surg. 2015, 61, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Farsad, M.; Zeinali-Davarani, S.; Choi, J.; Baek, S. Computational Growth and Remodelling of Abdominal Aortic Aneurysms Constrained by the Spine. J. Biomech. Eng. 2015, 137, 0910081–09100812. [Google Scholar] [CrossRef] [PubMed]
- George, E.; Giannopoulos, A.A.; Aghayev, A.; Rohatgi, S.; Imanzadeh, A.; Antoniadis, A.P.; Kumamaru, K.K.; Chatzizisis, Y.S.; Dunne, R.; Steigner, M.; et al. Contrast inhomogeneity in CT angiography of the abdominal aortic aneurysm. J. Cardiovasc. Comput. Tomogr. 2016, 10, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Hendy, K.; Gunnarsson, R.; Cronin, O.; Colledge, J. Infra-renal abdominal aortic calcification volume does not predict small abdominal aortic aneurysm growth. Atherosclerosis 2015, 243, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Teng, Z.; Elkhawad, M.; Tarkin, J.M.; Joshi, N.; Boyle, J.R.; Buscombe, J.R.; Fryer, T.D.; Zhang, Y.; Park, A.Y.; et al. High Structural Stress and Presence of Intraluminal Thrombus Predict Abdominal Aortic Aneurysm 18F-FDG Uptake: Insights From Biomechanics. Circ. Cardiovasc. Imaging 2016, 9, e004656. [Google Scholar] [CrossRef]
- Joly, F.; Soulez, G.; Garcia, D.; Lessard, S.; Kauffmann, C. Flow stagnation volume and abdominal aortic aneurysm growth: Insights from patient-specific computational flow dynamics of Lagrangian-coherent structures. Comput. Biol. Med. 2018, 92, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Lindquist Liljeqvist, M.; Hultgren, R.; Gasser, T.C.; Roy, J. Volume growth of abdominal aortic aneurysms correlates with baseline volume and increasing finite element analysis-derived rupture risk. J. Vasc. Surg. 2016, 63, 1434–1442.e3. [Google Scholar] [CrossRef]
- Nakayama, A.; Morita, H.; Hayashi, N.; Nomura, Y.; Hoshina, K.; Shigematsu, K.; Ohtsu, H.; Miyata, T.; Komuro, I. Inverse Correlation between Calcium Accumulation and the Expansion Rate of Abdominal Aortic Aneurysms. Circ. J. 2016, 80, 332–339. [Google Scholar] [CrossRef]
- Wołoszko, T.; Skórski, M.; Kwasiborski, P.; Kmin, E.; Gałązka, Z.; Pogorzelski, R. Influence of Selective Biochemical and Morphological Agents on Natural History of Aneurysm of Abdominal Aorta Development. Med. Sci. Monit. 2016, 22, 431–437. [Google Scholar] [CrossRef][Green Version]
- Behr-Andersen, C.; Gammelgaard, L.; Fründ, E.T.; Dahl, M.; Lindholt, J.S. Magnetic resonance imaging of the intraluminal thrombus in abdominal aortic aneurysms: A quantitative and qualitative evaluation and correlation with growth rate. J. Cardiovasc. Surg. (Torino) 2019, 60, 221–229. [Google Scholar] [CrossRef]
- Forsythe, R.O.; Dweck, M.R.; McBride, O.M.; Vesey, A.T.; Semple, S.I.; Shah, A.S.; Adamson, P.D.; Wallace, W.A.; Kaczynski, J.; Ho, W.; et al. (18) F-Sodium Fluoride Uptake in Abdominal Aortic Aneurysms: The SoFIA (3) Study. J. Am. Coll. Cardiol. 2018, 71, 513–523. [Google Scholar] [CrossRef]
- MA3RS Study Investigators. Aortic Wall Inflammation Predicts Abdominal Aortic Aneurysm Expansion, Rupture and Need for Surgical Repair. Circulation 2017, 136, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Nyronning, L.A.; Skoog, P.; Videm, V.; Mattsson, E. Is the aortic size index relevant as a predictor of abdominal aortic aneurysm? A population-based prospective study: The Tromsø study. Scand. Cardiovasc. J. 2020, 54, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Tzirakis, K.; Kontopodis, N.; Metaxa, E.; Ioannou, C.V.; Papaharilaou, Y. Spatial Distribution of Abdominal Aortic Aneurysm Surface Expansion and Correlation With Maximum Diameter and Volume Growth. Ann. Vasc. Surg. 2019, 58, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Hirata, K.; Nakaura, T.; Nakagawa, M.; Kidoh, M.; Oda, S.; Utsunomiya, D.; Yamashita, Y. Machine Learning to Predict the Rapid Growth of Small Abdominal Aortic Aneurysm. J. Comput. Assist. Tomogr. 2020, 44, 37–42. [Google Scholar] [CrossRef]
- Zhu, C.; Leach, J.R.; Wang, Y.; Gasper, W.; Saloner, D.; Hope, M.D. Intraluminal Thrombus Predicts Rapid Growth of Abdominal Aortic Aneurysms. Radiology 2020, 294, 707–713. [Google Scholar] [CrossRef]
- Spanos, K.; Nana, P.; Behrendt, C.A.; Kouvelos, G.; Panuccio, G.; Heidemann, F.; Matsagkas, M.; Debus, S.; Giannoukas, A.; Kölbel, T. Management of Abdominal Aortic Aneurysm Disease: Similarities and Differences Among Cardiovascular Guidelines and NICE Guidance. J. Endovasc. Ther. 2020, 27, 889–901. [Google Scholar] [CrossRef]
- Spanos, K.; Eckstein, H.-H.; Giannoukas, A.D. Small Abdominal Aortic Aneurysms Are Not All the Same. Angiology 2020, 71, 205–207. [Google Scholar] [CrossRef]
- Cao, P.; De Rango, P.; Verzini, F.; Parlani, G.; Romano, L.; Cieri, E.; CAESAR Trial Group. Comparison of Surveillance Versus Aortic Endografting for Small Aneurysm Repair (CAESAR): Results from a randomized trial. Eur. J. Endovasc. Surg. 2011, 41, 13–25. [Google Scholar] [CrossRef]
- Ouriel, K.; Clair, D.G.; Kent, K.C.; Zarins, C.K. Positive Impact of Endovascular Options for Treating Aneurysms Early (PIVOTAL) Investigators. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms. J. Vasc. Surg. 2010, 51, 1081–1087. [Google Scholar] [CrossRef]
- Ballotta, E.; Da Giau, G.; Bottio, T.; Toniato, A. Elective surgery for small abdominal aortic aneurysms. Cardiovasc. Surg. 1999, 7, 495–502. [Google Scholar] [CrossRef]
- Powell, J.T.; Gotensparre, S.M.; Sweeting, M.J.; Brown, L.C.; Fowkes, F.G.; Thompson, S.G. Rupture rates of small abdominal aortic aneurysms: A systematic review of the literature. Eur. J. Vasc. Endovasc. Surg. 2011, 41, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Propper, B.W.; Rasmussen, T.E.; Jones, W.T.; Gifford, S.M.; Burkhardt, G.E.; Clouse, W.D. Temporal changes of aortic neck morphology in abdominal aortic aneurysms. J. Vasc. Surg. 2010, 51, 1111–1115. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Buijs, R.V.; Willems, T.P.; Tio, R.A.; Boersma, H.H.; Tielliu, I.F.; Slart, R.H.; Zeebregts, C.J. Current state of experimental imaging modalities for risk assessment of abdominal aortic aneurysm. J. Vasc. Surg. 2013, 57, 851–859. [Google Scholar] [CrossRef][Green Version]
- Xu, X.Y.; Borghi, A.; Nchimi, A.; Leung, J.; Gomez, P.; Cheng, Z.; Defraigne, J.; Sakalihasan, N. High levels of 18F-FDG uptake in aortic aneurysm wall are associated with high wall stress. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 295–301. [Google Scholar] [CrossRef]
- Xenos, M.; Labropoulos, N.; Rambhia, S.; Alemu, Y.; Einav, S.; Tassiopoulos, A.; Sakalihasan, N.; Bluestein, D. Progression of abdominal aortic aneurysm towards rupture: Refining clinical risk assessment using a fully coupled fluid-structure interaction method. Ann. Biomed. Eng. 2015, 43, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Kyriakou, F.; Dempster, W.; Nash, D. Analysing The Cross-Section of The Abdominal Aortic Aneurysm Neck and Its Effects on Stent Deployment. Sci. Rep. 2020, 10, 4673. [Google Scholar] [CrossRef]
- Crawford, J.D.; Chivukula, V.K.; Haller, S.; Vatankhah, N.; Bohannan, C.J.; Moneta, G.L.; Rugonyi, S.; Azarbal, A.F. Aortic outflow occlusion predicts rupture of abdominal aortic aneurysm. J. Vasc. Surg. 2016, 64, 1623–1628. [Google Scholar] [CrossRef]
- Anonymous. Mortality results for randomized controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. The UK small aneurysm trial participants. Lancet 1998, 352, 1649–1655. [Google Scholar] [CrossRef]
- Lederle, F.A.; Wilson, S.E.; Johnson, G.R.; Reinke, D.B.; Littooy, F.N.; Acher, C.W.; Ballard, D.J.; Messina, L.M.; Gordon, I.L.; Chute, E.P.; et al. Immediate repair compared with surveillance of small abdominal aortic aneurysms. N. Engl. J. Med. 2002, 346, 1437–1444. [Google Scholar] [CrossRef]
- Rowbotham, S.E.; Krishna, S.M.; Moran, C.S.; Golledge, J. Fenofibrate and Telmisartan in the Management of Abdominal Aortic Aneurysm. Curr. Drug Targets 2018, 19, 1241–1246. [Google Scholar] [CrossRef] [PubMed]
- Raffort, J.; Lareyre, F.; Clément, M.; Hassen-Khodja, R.; Chinetti, G.; Mallat, Z. Diabetes and aortic aneurysm: Current state of the art. Cardiovasc. Res. 2018, 114, 1702–1713. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.I.; Greco, M.; Vorkas, P.A.; Holmes, E.; Davies, A.H. Application of Metabolic Profiling to Abdominal Aortic Aneurysm Research. J. Proteome Res. 2017, 16, 2325–2332. [Google Scholar] [CrossRef]
- Torres-Fonseca, M.; Galan, M.; Martinez-Lopez, D.; Cañes, L.; Roldan-Montero, R.; Alonso, J.; Reyero-Postigo, T.; Orriols, M.; Mendez-Barbero, N.; Sirvent, M.; et al. Pathophysiology of abdominal aortic aneurysm: Biomarkers and novel therapeutic targets. Clin. Investig. Arterioscler. 2019, 31, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Nana, P.; Dakis, K.; Brodis, A.; Spanos, K.; Kouvelos, G. Circulating Biomarkers for the Prediction of Abdominal Aortic Aneurysm Growth. J. Clin. Med. 2021, 10, 1718. [Google Scholar] [CrossRef]
| P | Patient, Population or Problem | Patients with AAA |
| I | Intervention, prognostic factor or exposure | Pre-operative surveillance with imaging modalities of patients with AAA |
| C | Comparison of intervention | AAA expansion rate during surveillance defined as the difference between the initial and latest available diameter devised by time (mm/year) |
| O | Outcome you would like to measure or achieve | Imaging findings associated to aneurysm growth |
| What type of question are you asking? | Are there imaging factors that could predict AAA evolution? | |
| Are there imaging factors that affect positively or negatively aneurysm growth? | ||
| Type of study you want to find | Cohort observational trials; prospective and retrospective reporting on AAA growth and predictive imaging findings |
| Author | Year | Journal | Study Period | Type | Imaging Modality |
|---|---|---|---|---|---|
| Wolf, et al. [16] | 1994 | JVS | 1986–1992 | Retrospective | CTA |
| Faggioli, et al. [17] | 1994 | Am J Surg | NA | Prospective | Angiography, CTA |
| Veldenz, et al. [18] | 1994 | Ann Vasc Surg | 1988–1992 | Retrospective | CTA |
| Kurvers, et al. [19] | 2004 | J Am Col Surg | 1996–2002 | Retrospective | CTA |
| Lindholt, et al. [20] | 2008 | Atherosclerosis | 1994 | Prospective | US |
| Speelman, et al. [21] | 2010 | EJVES | NA | Prospective | CTA |
| Badger, et al. [22] | 2011 | Vasc Med | 2004–2006 | Retrospective | US |
| Shang, et al. [23] | 2013 | JVS | NA | Retrospective | CTA |
| Farsad, et al. [24] | 2015 | J Cardiovasc Comput Tomogr | NA | Prospective | CTA |
| George, et al. [25] | 2015 | J Cardiovasc Comput Tomogr | 2010–2011 | Retrospective | CTA |
| Hendy, et al. [26] | 2015 | Atheroscl | 2003–2013 | Prospective | CTA |
| Huang, et al. [27] | 2016 | Mol Imaging | NA | Prospective | PET-CT, CTA |
| Joly, et al. [28] | 2016 | Comput Biol Med | 2006–2013 | Retrospective | CTA, MRI |
| Lindquist, et al. [29] | 2016 | JVS | 2009–2013 | Retrospective | CTA |
| Nakayama, et al. [30] | 2016 | Circ J | 2003–2011 | Retrospective | CTA |
| Woloszko, et al. [31] | 2016 | Med Sci Monit | 2005–2010 | Prospective | US, CTA |
| Behr, et al. [32] | 2017 | J Cardiovasc Surg | 2014–2015 | Retrospective | MRI, US |
| Forsythe, et al. [33] | 2017 | JACC | NA | Prospective | PET-CT |
| MARS investigators [34] | 2017 | Circ | 2012–2014 | Prospective | MRI |
| Nyronning, et al. [35] | 2019 | Scand Cardiovasc J | 1994–2005 | Prospective | US |
| Tzirakis, et al. [36] | 2019 | Ann Vasc Surg | NA | Retrospective | CTA |
| Hirata, et al. [37] | 2020 | J Comput Assist Tomogr | 2010–2016 | Retrospective | CTA |
| Zhu, et al. [38] | 2020 | Radiology | 2004–2018 | Retrospective | CTA, MRI, PET CT |
| Authors | AAA Diameter Threshold for Inclusion | Initial AAA Diameter | Follow-Up (Months) | AAA Diameter at Follow-Up | AAA Growth Rate in mm/year |
|---|---|---|---|---|---|
| Wolf, et al. [16] | >30 mm | 44 ± 6 mm | 22 ± 12 | NA | 2.5 ± 2.4 |
| Faggioli, et al. [17] | <50 mm | NA | NA | NA | NA |
| Veldenz, et al. [18] | <50 mm | NA | 15 | NA | NA |
| Kurvers, et al. [19] | NA | 50 ± 9 mm | 42 | NA | 3.6 ± 2.4 |
| Lindholt, et al. [20] | NA | 32 mm | 6.15 ± 3.61 | NA | 2.45 |
| Speelman, et al. [21] | NA | NA | 12 | NA | NA |
| Badger, et al. [22] | 46 mm | 39 mm | NA | NA | 0.75 for AAA <35 mm & 4.32 for AAA >50 mm |
| Shang, et al. [23] | NA | 45.8 ± 7.7 mm | 22.0 ± 13.6 | 50.6 ± 9.0 mm | 2.8 ± 1.7 |
| Farsad, et al. [24] | <5 cm | NA | NA | NA | NA |
| George, et al. [25] | NA | NA | 26 | NA | NA |
| Hendy, et al. [26] | NA | NA | 16 | NA | 1.6 vs. 1.8 in AAA with > or < than 50% of wall calcification, respectively |
| Huang, et al. [27] | NA | 41 ± 5.4 mm | NA | NA | NA |
| Joly, et al. [28] | <55 mm | NA | 96 | NA | NA |
| Lindquist, et al. [29] | <50 mm | 52 mm | 12 | 55 mm | 3.1 |
| Nakayama, et al. [30] | <55 mm | 44.7 ± 14.6 mm | 19 | 52.9 ± 2.9 mm | NA |
| Woloszko, et al. [31] | NA | 39 mm | 24 | 43 mm | NA |
| Behr, et al. [32] | >30 mm | 31.9 mm | 67 | 42.3 mm | 1.95; 2.04 in case of circumferential thrombus |
| Forsythe, et al. [33] | <50 mm | NA | 16.7± 6.4 | NA | 2.20 |
| MARS investigators [34] | NA | 49.6 ± 7.7 mm | 33 ± 9.2 | NA | 2.8 ± 2.4 |
| Nyronning, et al. [35] | <40 mm | 19.9 mm | 120 | 20.3 mm | 3.1 in 2 years of FUP |
| Tzirakis, et al. [36] | >40 mm | NA | NA | NA | 3.35 |
| Hirata, et al. [37] | NA | 42.8 ± 6.7 mm | NA | NA | 3.0 ± 2.3 |
| Zhu, et al. [38] | 32–56 mm | 38 mm | 39.6 ± 30 | 44 mm | 1.5; 2.0 in AAA with intra-luminal thrombus |
| Author | Number of Imaging Predictive Factors Per Study | Initial AAA Diameter | Presence of Intra-Luminal Thrombus | Type of Thrombus Associated to Expansion | Presence of Aortic Wall Calcification | AAA Volume |
|---|---|---|---|---|---|---|
| Wolf, et al. [16] | 1 | Positive | ||||
| Faggioli, et al. [17] | 1 | |||||
| Veldenz, et al. [18] | 1 | |||||
| Kurvers, et al. [19] | 1 | Positive | ||||
| Lindholt, et al. [20] | 1 | Negative | ||||
| Speelman, et al. [21] | 1 | |||||
| Badger, et al. [22] | 2 | Positive | ||||
| Shang, et al. [23] | 2 | No associated | ||||
| Farsad, et al. [24] | ||||||
| George, et al. [25] | 2 | Positive | Positive | Inhomogeneous | ||
| Hendy, et al. [26] | 2 | Positive | ||||
| Huang, et al. [27] | 2 | Positive | ||||
| Joly, et al. [28] | 1 | |||||
| Lindquist, et al. [29] | 1 | Positive | ||||
| Nakayama, et al. [30] | 2 | Positive | Negative | |||
| Woloszko, et al. [31] | 3 | Positive | Positive | |||
| Behr, et al. [32] | 1 | Positive | Positive | Inhomogeneous Circumferential | ||
| Forsythe, et al. [33] | 1 | |||||
| MARS investigators [34] | 3 | Positive | ||||
| Nyronning, et al. [35] | 2 | Positive | ||||
| Tzirakis, et al. [36] | 3 | Positive | Positive | Positive | ||
| Hirata, et al. [37] | 2 | Positive | Not associated | |||
| Zhu, et al. [38] | 2 | Positive | Positive |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nana, P.; Spanos, K.; Dakis, K.; Brodis, A.; Kouvelos, G. Imaging Predictive Factors of Abdominal Aortic Aneurysm Growth. J. Clin. Med. 2021, 10, 1917. https://doi.org/10.3390/jcm10091917
Nana P, Spanos K, Dakis K, Brodis A, Kouvelos G. Imaging Predictive Factors of Abdominal Aortic Aneurysm Growth. Journal of Clinical Medicine. 2021; 10(9):1917. https://doi.org/10.3390/jcm10091917
Chicago/Turabian StyleNana, Petroula, Konstantinos Spanos, Konstantinos Dakis, Alexandros Brodis, and George Kouvelos. 2021. "Imaging Predictive Factors of Abdominal Aortic Aneurysm Growth" Journal of Clinical Medicine 10, no. 9: 1917. https://doi.org/10.3390/jcm10091917
APA StyleNana, P., Spanos, K., Dakis, K., Brodis, A., & Kouvelos, G. (2021). Imaging Predictive Factors of Abdominal Aortic Aneurysm Growth. Journal of Clinical Medicine, 10(9), 1917. https://doi.org/10.3390/jcm10091917







