Long-Acting Reversible Contraception: Placement, Continuation, and Removal Rates at an Inner-City Academic Medical Center Clinic
Abstract
1. Introduction
2. Materials and Methods
Patient Selection
3. Results
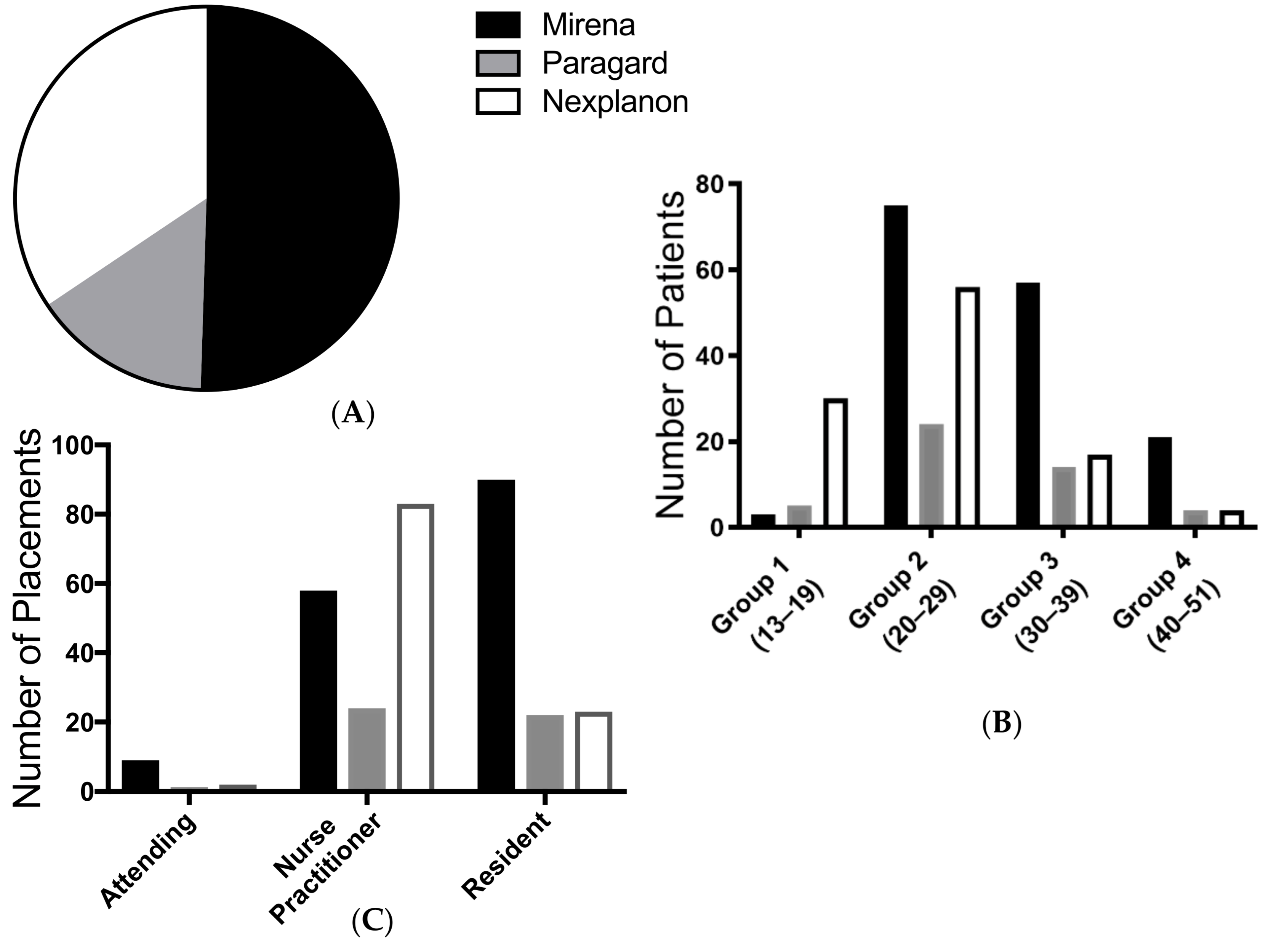
3.1. Indication for Device Placement
3.2. Device Distribution by Race
3.3. Device Distribution by Age
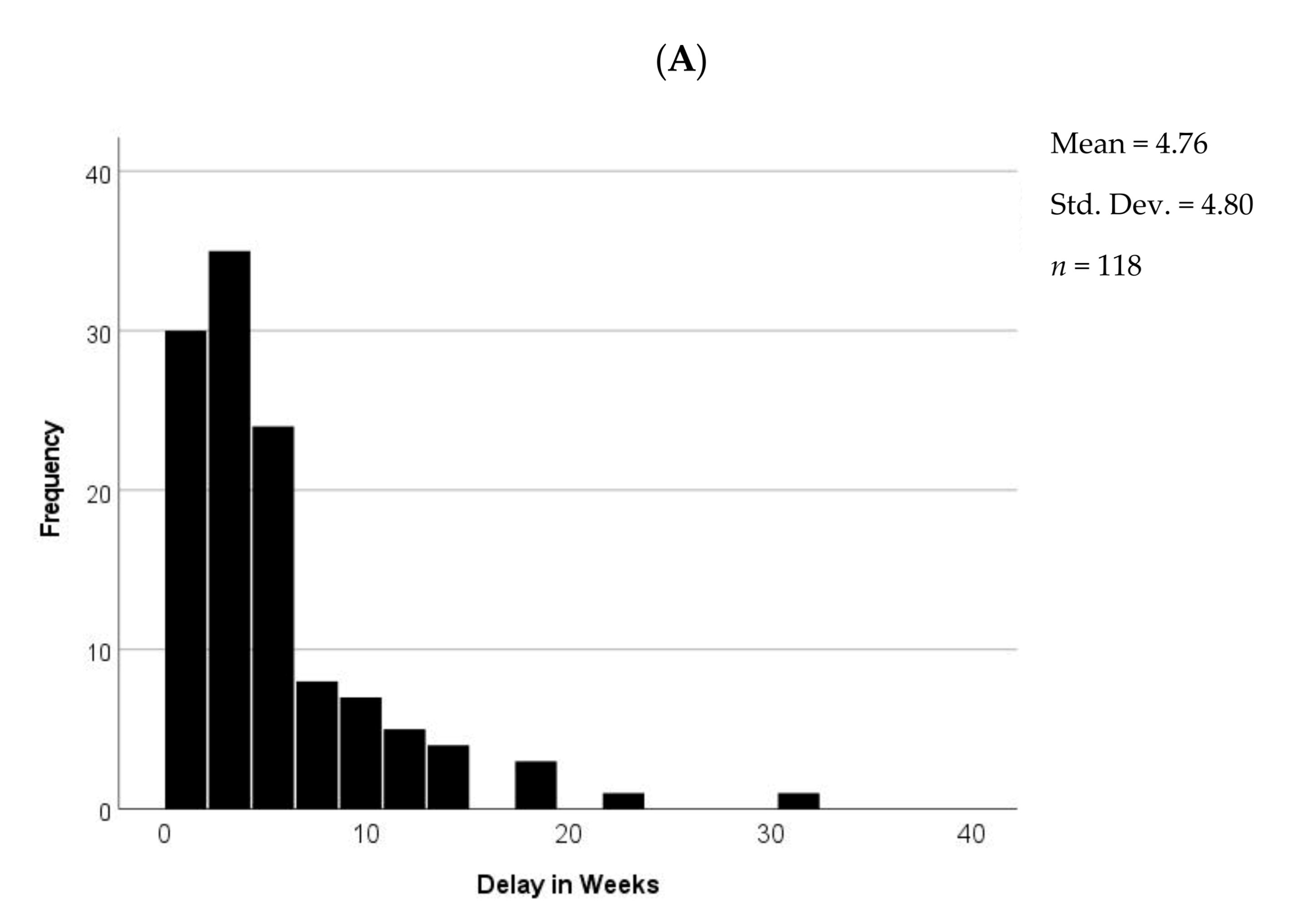
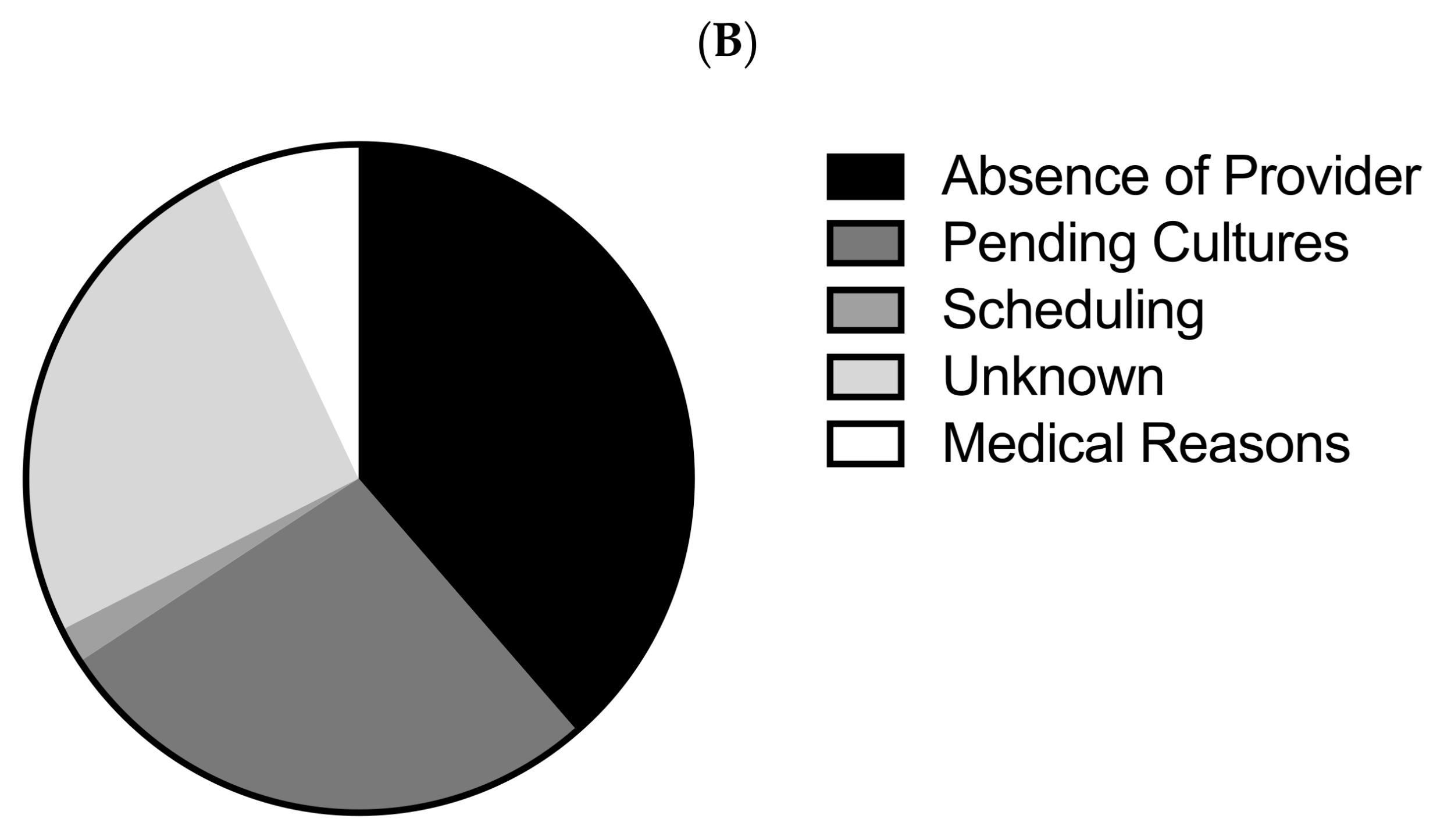
3.4. Analysis of Delays in LARC Placement
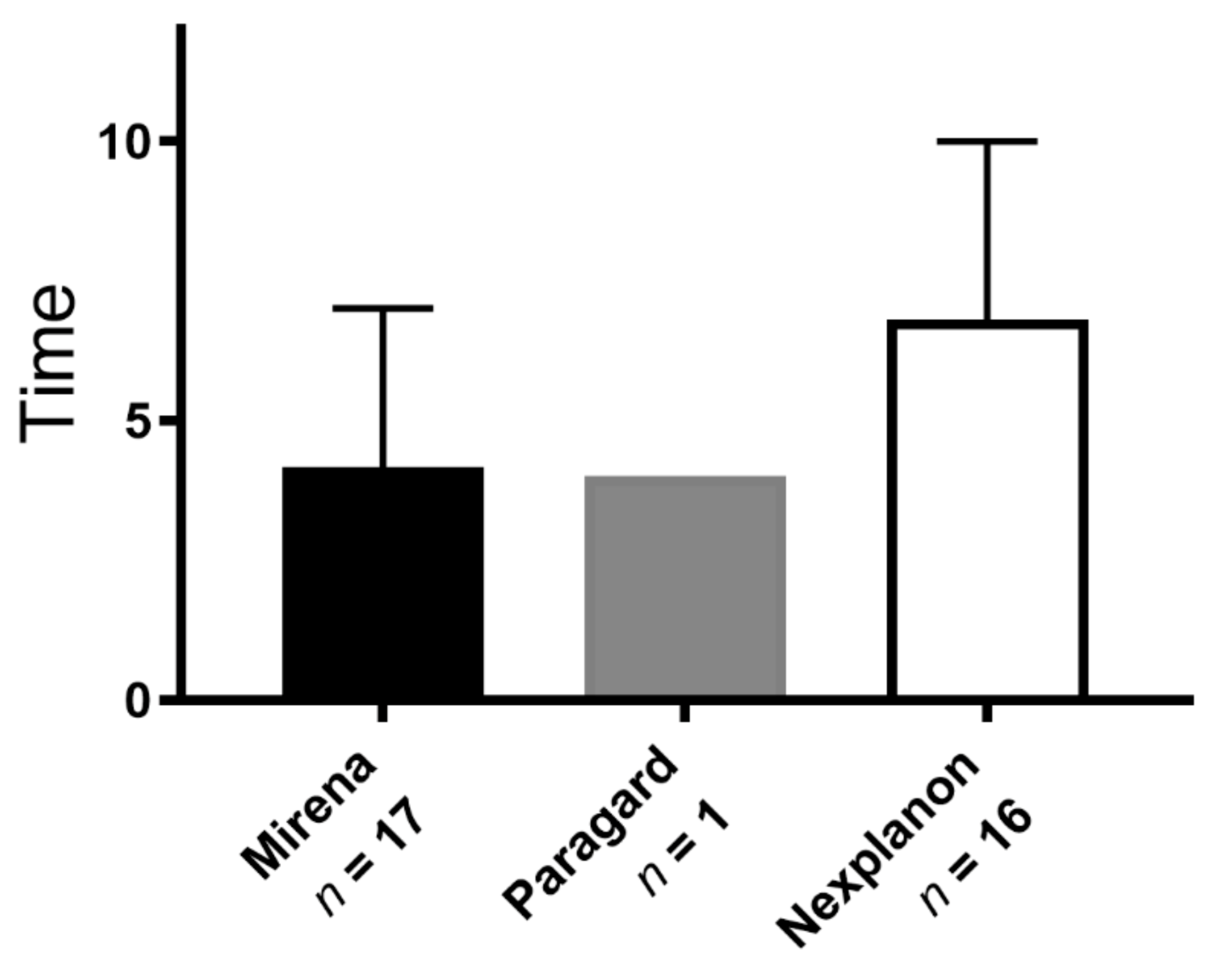
3.5. Analysis of Device Removal
3.6. Analysis of Switching out of LARC Method
4. Discussion
4.1. Delay in Placement
4.2. Early Removal of Device
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Finer, L.B.; Zolna, M.R. Declines in Unintended Pregnancy in the United States, 2008–2011. N. Engl. J. Med. 2016, 374, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Sedgh, G.; Singh, S.; Hussain, R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud. Fam. Plan. 2014, 45, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Bearak, J.; Popinchalk, A.; Alkema, L.; Sedgh, G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: Estimates from a Bayesian hierarchical model. Lancet Glob. Health 2018, 6, e380–e389. [Google Scholar] [CrossRef]
- Jones, R.K.; Darroch, J.E.; Henshaw, S.K. Contraceptive use among U.S. women having abortions in 2000–2001. Perspect. Sex. Reprod. Health 2002, 34, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Frost, J.J.; Darroch, J.E. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect. Sex. Reprod. Health 2008, 40, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Frost, J.J.; Singh, S.; Finer, L.B. U.S. women’s one-year contraceptive use patterns, 2004. Perspect. Sex. Reprod. Health 2007, 39, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Frost, J.J.; Singh, S.; Finer, L.B. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect. Sex. Reprod. Health 2007, 39, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Daniels, K.; Mosher, W.D. Contraceptive Methods Women Have Ever Used: United States, 1982–2010; National Health Statistics Report; National Center for Health Statistics: Hyattsville, MD, USA, 2013; pp. 1–15.
- Daniels, K.; Daugherty, J.; Jones, J. Current Contraceptive Status among Women Aged 15–44: United States, 2011–2013; NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2014; pp. 1–8.
- Eeckhaut, M.C.; Sweeney, M.M.; Gipson, J.D. Who is using long-acting reversible contraceptive methods? Findings from nine low-fertility countries. Perspect. Sex. Reprod. Health 2014, 46, 149–155. [Google Scholar] [CrossRef]
- Trussell, J. Contraceptive failure in the United States. Contraception 2011, 83, 397–404. [Google Scholar] [CrossRef]
- Forrest, J.D. U.S. women’s perceptions of and attitudes about the IUD. Obstet. Gynecol. Surv. 1996, 51, S30–S34. [Google Scholar] [CrossRef]
- Madden, T.; Allsworth, J.E.; Hladky, K.J.; Secura, G.M.; Peipert, J.F. Intrauterine contraception in Saint Louis: A survey of obstetrician and gynecologists’ knowledge and attitudes. Contraception 2010, 81, 112–116. [Google Scholar] [CrossRef]
- Diaz, V.A.; Hughes, N.; Dickerson, L.M.; Wessell, A.M.; Carek, P.J. Clinician knowledge about use of intrauterine devices in adolescents in South Carolina AHEC. Fam. Med. 2011, 43, 407–411. [Google Scholar]
- Phillips, J.; Sandhu, P. Barriers to implementation of long-acting reversible contraception: A systematic review. J. Am. Assoc. Nurse Pract. 2018, 30, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Trussell, J.; Lalla, A.M.; Doan, Q.V.; Reyes, E.; Pinto, L.; Gricar, J. Cost effectiveness of contraceptives in the United States. Contraception 2009, 79, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.L.; Espey, E.; Ogburn, T.; Zite, N.B. Use of Long-Acting Reversible Contraception by Obstetrics and Gynecology Residents: An Examination of Access for All Women. Obstet. Gynecol. 2018, 131, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Secura, G.M.; Allsworth, J.E.; Madden, T.; Mullersman, J.L.; Peipert, J.F. The Contraceptive CHOICE Project: Reducing barriers to long-acting reversible contraception. Am. J. Obstet. Gynecol. 2010, 203, 115.e1–115.e7. [Google Scholar] [CrossRef]
- Peipert, J.F.; Zhao, Q.; Allsworth, J.E.; Petrosky, E.; Madden, T.; Eisenberg, D.; Secura, G. Continuation and satisfaction of reversible contraception. Obstet. Gynecol. 2011, 117, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.R.; Peipert, J.F.; Madden, T.; Zhao, Q.; Secura, G.M. Continuation of reversible contraception in teenagers and young women. Obstet. Gynecol. 2012, 120, 1298–1305. [Google Scholar] [CrossRef]
- Curtis, K.M.; Tepper, N.K.; Jatlaoui, T.C.; Berry-Bibee, E.; Horton, L.G.; Zapata, L.B.; Simmons, K.B.; Pagano, H.P.; Jamieson, D.J.; Whiteman, M.K. US medical eligibility criteria for contraceptive use, 2016. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2016, 65, 1–103. [Google Scholar] [CrossRef]
- Lohr, P.A.; Lyus, R.; Prager, S. Use of intrauterine devices in nulliparous women. Contraception 2017, 95, 529–537. [Google Scholar] [CrossRef]
- Logan, R.G.; Thompson, E.L.; Vamos, C.A.; Griner, S.B.; Vazquez-Otero, C.; Daley, E.M. Is Long-Acting Reversible Contraceptive Use Increasing? Assessing Trends Among U.S. College Women, 2008–2013. Matern. Child Health J. 2018. [Google Scholar] [CrossRef] [PubMed]
- Sonfield, A.; Kost, K.; Gold, R.B.; Finer, L.B. The Public Costs of Births Resulting from Unintended Pregnancies: National and State-Level Estimates. Perspect. Sex. Reprod. Health 2011, 43, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Dehlendorf, C.; Rodriguez, M.I.; Levy, K.; Borrero, S.; Steinauer, J. Disparities in family planning. Am. J. Obstet. Gynecol. 2010, 202, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Bergin, A.; Tristan, S.; Terplan, M.; Gilliam, M.L.; Whitaker, A.K. A missed opportunity for care: Two-visit IUD insertion protocols inhibit placement. Contraception 2012, 86, 694–697. [Google Scholar] [CrossRef] [PubMed]
- Turok, D.K.; Eisenberg, D.L.; Teal, S.B.; Keder, L.M.; Creinin, M.D. A prospective assessment of pelvic infection risk following same-day sexually transmitted infection testing and levonorgestrel intrauterine system placement. Am. J. Obstet. Gynecol. 2016, 215, 599.e1–599.e6. [Google Scholar] [CrossRef] [PubMed]
- Jatlaoui, T.C.; Simmons, K.B.; Curtis, K.M. The safety of intrauterine contraception initiation among women with current asymptomatic cervical infections or at increased risk of sexually transmitted infections. Contraception 2016, 94, 701–712. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet. Gynecol. 2011, 118, 184–196. [Google Scholar] [CrossRef]
- Romano, M.J.; Toye, P.; Patchen, L. Continuation of long-acting reversible contraceptives among Medicaid patients. Contraception 2018. [Google Scholar] [CrossRef]
- Hubacher, D. Copper intrauterine device use by nulliparous women: Review of side effects. Contraception 2007, 75, S8–S11. [Google Scholar] [CrossRef]
- Hoggart, L.; Newton, V.L.; Dickson, J. “I think it depends on the body, with mine it didn’t work”: Explaining young women’s contraceptive implant removal. Contraception 2013, 88, 636–640. [Google Scholar] [CrossRef]
- Berenson, A.B.; Tan, A.; Hirth, J.M. Complications and continuation rates associated with 2 types of long-acting contraception. Am. J. Obstet. Gynecol. 2015, 212, 761.e1–761.e8. [Google Scholar] [CrossRef] [PubMed]
- Chiles, D.P.; Roberts, T.A.; Klein, D.A. Initiation and continuation of long-acting reversible contraception in the United States military healthcare system. Am. J. Obstet. Gynecol. 2016, 215, 328.e1–328.e9. [Google Scholar] [CrossRef]
- Grunloh, D.S.; Casner, T.; Secura, G.M.; Peipert, J.F.; Madden, T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet. Gynecol. 2013, 122, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Amico, J.R.; Bennett, A.H.; Karasz, A.; Gold, M. “I wish they could hold on a little longer”: physicians’ experiences with requests for early IUD removal. Contraception 2017, 96, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Foster, D.G.; Grossman, D.; Turok, D.K.; Peipert, J.F.; Prine, L.; Schreiber, C.A.; Jackson, A.V.; Barar, R.E.; Schwarz, E.B. Interest in and experience with IUD self-removal. Contraception 2014, 90, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.M.; Jatlaoui, T.C.; Tepper, N.K.; Zapata, L.B.; Horton, L.G.; Jamieson, D.J.; Whiteman, M.K. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2016, 65, 1–66. [Google Scholar] [CrossRef]
- Long-Acting Reversible Contraception Working Group. ACOG Committee Opinion no. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet. Gynecol. 2009, 114, 1434–1438. [Google Scholar] [CrossRef] [PubMed]
- Morroni, C.; Findley, M.; Westhoff, C. Does using the “pregnancy checklist” delay safe initiation of contraception? Contraception 2017, 95, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Amico, J.; Wu, J. Providing Long-Acting Reversible Contraception in an Academic Family Medicine Center. Fam. Med. 2015, 47, 727–731. [Google Scholar]
- Raine, T.R.; Foster-Rosales, A.; Upadhyay, U.D.; Boyer, C.B.; Brown, B.A.; Sokoloff, A.; Harper, C.C. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet. Gynecol. 2011, 117, 363–371. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Committee opinion no. 539: Adolescents and long-acting reversible contraception: Implants and intrauterine devices. Obstet. Gynecol. 2012, 120, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, L.M.; Diaz, V.A.; Jordon, J.; Davis, E.; Chirina, S.; Goddard, J.A.; Carr, K.B.; Carek, P.J. Satisfaction, early removal, and side effects associated with long-acting reversible contraception. Fam. Med. 2013, 45, 701–707. [Google Scholar] [PubMed]
- Peterson, H.B.; Cates, W. Evidence-based medicine in action: The United States Selected Practice Recommendations for Contraceptive Use. Contraception 2013, 87, 509–510. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, C.; Battaglia, B.; Casadio, P.; Rizzo, R.; Artini, P.G. Metformin metabolic and vascular effects in normal weight hyperinsulinemic polycystic ovary syndrome patients treated with contraceptive vaginal ring. A pilot study. Gynecol. Endocrinol. 2020, 36, 1062–1069. [Google Scholar] [CrossRef]
- Morotti, E.; Casadio, P.; Guasina, F.; Battaglia, B.; Mattioli, M.; Battaglia, C. Weight gain, body image and sexual function in young patients treated with contraceptive vaginal ring. A prospective pilot study. Gynecol. Endocrinol. 2017, 33, 660–664. [Google Scholar] [CrossRef]
- Battaglia, C.; Morotti, E.; Persico, N.; Battaglia, B.; Busacchi, P.; Casadio, P.; Paradisi, R.; Venturoli, S. Clitoral vascularization and sexual behavior in young patients treated with drospirenone-ethinyl estradiol or contraceptive vaginal ring: A prospective, randomized, pilot study. J. Sex. Med. 2014, 11, 471–480. [Google Scholar] [CrossRef]
- Amico, J.R.; Bennett, A.H.; Karasz, A.; Gold, M. Taking the provider “out of the loop:” patients’ and physicians’ perspectives about IUD self-removal. Contraception 2018. [Google Scholar] [CrossRef]
- Godfrey, E.M.; West, I.I.; Holmes, J.; Keppel, G.A.; Baldwin, L.M. Use of an electronic health record data sharing system for identifying current contraceptive use within the WWAMI region Practice and Research Network. Contraception 2018, 98, 476–481. [Google Scholar] [CrossRef]
| N (%) | Mirena | Paragard | Nexplanon | |
|---|---|---|---|---|
| Average Age (±SD) | 28.2 (±7.9) | 30.9 (±7.6) | 28.4 (±7.4) | 24.1 (±6.8) |
| Age range | 13–51 | 14–51 | 17–46 | 13–44 |
| African American | 266 (85) | 146 | 18 | 102 |
| Middle Eastern | 18 (6) | 3 | 14 | 1 |
| Asian | 15 (5) | 2 | 13 | 0 |
| White | 10 (3) | 5 | 2 | 3 |
| Hispanic | 2 (<1) | 1 | 0 | 1 |
| Family Planning—New device insertions | 220 (71) | 90 | 43 | 87 |
| Family Planning—Replacement of expired device | 60 (19) | 36 | 4 | 20 |
| Abnormal Uterine Bleeding | 31 (10) | 31 | 0 | 0 |
| Total | 311 (100) | 157 | 47 | 107 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Runyan, A.; Welch, R.A.; Kramer, K.J.; Cortez, S.; Roberts, L.J.; Asamoah, C.; Ottum, S.; Sanders, J.; Shafi, A.; Recanati, M.-A. Long-Acting Reversible Contraception: Placement, Continuation, and Removal Rates at an Inner-City Academic Medical Center Clinic. J. Clin. Med. 2021, 10, 1918. https://doi.org/10.3390/jcm10091918
Runyan A, Welch RA, Kramer KJ, Cortez S, Roberts LJ, Asamoah C, Ottum S, Sanders J, Shafi A, Recanati M-A. Long-Acting Reversible Contraception: Placement, Continuation, and Removal Rates at an Inner-City Academic Medical Center Clinic. Journal of Clinical Medicine. 2021; 10(9):1918. https://doi.org/10.3390/jcm10091918
Chicago/Turabian StyleRunyan, Aliye, Robert A. Welch, Katherine J. Kramer, Sarah Cortez, LeAnne J. Roberts, Clementina Asamoah, Sarah Ottum, Jessica Sanders, Adib Shafi, and Maurice-Andre Recanati. 2021. "Long-Acting Reversible Contraception: Placement, Continuation, and Removal Rates at an Inner-City Academic Medical Center Clinic" Journal of Clinical Medicine 10, no. 9: 1918. https://doi.org/10.3390/jcm10091918
APA StyleRunyan, A., Welch, R. A., Kramer, K. J., Cortez, S., Roberts, L. J., Asamoah, C., Ottum, S., Sanders, J., Shafi, A., & Recanati, M.-A. (2021). Long-Acting Reversible Contraception: Placement, Continuation, and Removal Rates at an Inner-City Academic Medical Center Clinic. Journal of Clinical Medicine, 10(9), 1918. https://doi.org/10.3390/jcm10091918






