The Serum Uric Acid Level Is Related to the More Severe Renal Histopathology of Female IgA Nephropathy Patients
Abstract
1. Introduction
2. Materials and Methods
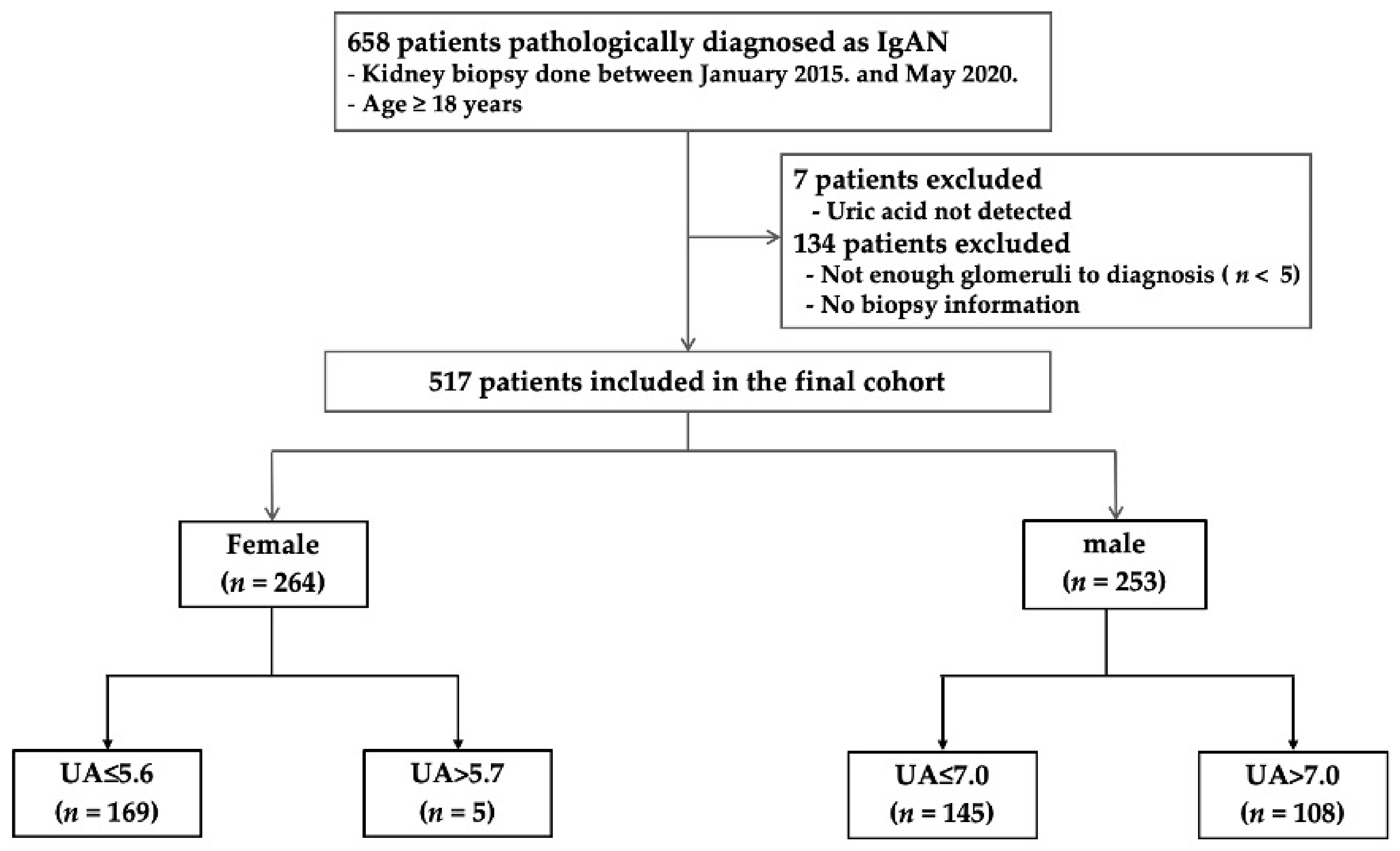
2.1. Study Design and Data
2.2. Data Collection, Definitions, and Measurements
2.3. Histopathological Parameters
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Histopathological Characteristics According to UA Levels in Males and Females
3.3. Associations between Serum UA Levels and Histopathological Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, J.H.; Kim, D.K.; Kim, H.W.; Park, S.Y.; Yoo, T.H.; Kim, B.S.; Kang, S.W.; Choi, K.H.; Han, D.S.; Jeong, H.J.; et al. Changing prevalence of glomerular diseases in Korean adults: A review of 20 years of experience. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2009, 24, 2406–2410. [Google Scholar] [CrossRef] [PubMed]
- Canetta, P.A.; Kiryluk, K.; Appel, G.B. Glomerular diseases: Emerging tests and therapies for IgA nephropathy. Clin. J. Am. Soc. Nephrol. CJASN 2014, 9, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Barbour, S.J.; Reich, H.N. Risk stratification of patients with IgA nephropathy. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2012, 59, 865–873. [Google Scholar] [CrossRef]
- Eiro, M.; Katoh, T.; Kuriki, M.; Asano, K.; Watanabe, K.; Watanabe, T. The product of duration and amount of proteinuria (proteinuria index) is a possible marker for glomerular and tubulointerstitial damage in IgA nephropathy. Nephron 2002, 90, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Radford, M.G., Jr.; Donadio, J.V., Jr.; Bergstralh, E.J.; Grande, J.P. Predicting renal outcome in IgA nephropathy. J. Am. Soc. Nephrol. JASN 1997, 8, 199–207. [Google Scholar] [CrossRef]
- D’Amico, G.; Colasanti, G.; Barbiano di Belgioioso, G.; Fellin, G.; Ragni, A.; Egidi, F.; Radaelli, L.; Fogazzi, G.; Ponticelli, C.; Minetti, L. Long-term follow-up of IgA mesangial nephropathy: Clinico-histological study in 374 patients. Semin. Nephrol. 1987, 7, 355–358. [Google Scholar]
- Goto, M.; Wakai, K.; Kawamura, T.; Ando, M.; Endoh, M.; Tomino, Y. A scoring system to predict renal outcome in IgA nephropathy: A nationwide 10-year prospective cohort study. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2009, 24, 3068–3074. [Google Scholar] [CrossRef] [PubMed]
- Duan, Z.Y.; Cai, G.Y.; Chen, Y.Z.; Liang, S.; Liu, S.W.; Wu, J.; Qiu, Q.; Lin, S.P.; Zhang, X.G.; Chen, X.M. Aging promotes progression of IgA nephropathy: A systematic review and meta-analysis. Am. J. Nephrol. 2013, 38, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Geddes, C.C.; Rauta, V.; Gronhagen-Riska, C.; Bartosik, L.P.; Jardine, A.G.; Ibels, L.S.; Pei, Y.; Cattran, D.C. A tricontinental view of IgA nephropathy. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2003, 18, 1541–1548. [Google Scholar] [CrossRef]
- Syrjänen, J.; Mustonen, J.; Pasternack, A. Hypertriglyceridaemia and hyperuricaemia are risk factors for progression of IgA nephropathy. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2000, 15, 34–42. [Google Scholar] [CrossRef]
- Kawabe, M.; Sato, A.; Hoshi, T.; Sakai, S.; Hiraya, D.; Watabe, H.; Kakefuda, Y.; Ishibashi, M.; Abe, D.; Takeyasu, N.; et al. Gender differences in the association between serum uric acid and prognosis in patients with acute coronary syndrome. J. Cardiol. 2016, 67, 170–176. [Google Scholar] [CrossRef]
- Harrold, L.R.; Etzel, C.J.; Gibofsky, A.; Kremer, J.M.; Pillinger, M.H.; Saag, K.G.; Schlesinger, N.; Terkeltaub, R.; Cox, V.; Greenberg, J.D. Sex differences in gout characteristics: Tailoring care for women and men. BMC Musculoskelet. Disord. 2017, 18, 108. [Google Scholar] [CrossRef] [PubMed]
- Halperin Kuhns, V.L.; Woodward, O.M. Sex Differences in Urate Handling. Int. J. Mol. Sci. 2020, 21, 4269. [Google Scholar] [CrossRef]
- Kuo, C.F.; Grainge, M.J.; Zhang, W.; Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 2015, 11, 649–662. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, D.; Unwin, R. The pathophysiology of hyperuricaemia and its possible relationship to cardiovascular disease, morbidity and mortality. BMC Nephrol. 2013, 14, 164. [Google Scholar] [CrossRef]
- Zoccali, C.; Maio, R.; Mallamaci, F.; Sesti, G.; Perticone, F. Uric acid and endothelial dysfunction in essential hypertension. J. Am. Soc. Nephrol. JASN 2006, 17, 1466–1471. [Google Scholar] [CrossRef]
- Li, C.; Hsieh, M.C.; Chang, S.J. Metabolic syndrome, diabetes, and hyperuricemia. Curr. Opin. Rheumatol. 2013, 25, 210–216. [Google Scholar] [CrossRef]
- Tsai, C.W.; Lin, S.Y.; Kuo, C.C.; Huang, C.C. Serum Uric Acid and Progression of Kidney Disease: A Longitudinal Analysis and Mini-Review. PLoS ONE 2017, 12, e0170393. [Google Scholar] [CrossRef]
- Zhou, J.; Chen, Y.; Liu, Y.; Shi, S.; Li, X.; Wang, S.; Zhang, H. Plasma uric acid level indicates tubular interstitial leisions at early stage of IgA nephropathy. BMC Nephrol. 2014, 15, 11. [Google Scholar] [CrossRef] [PubMed]
- Myllymäki, J.; Honkanen, T.; Syrjänen, J.; Helin, H.; Rantala, I.; Pasternack, A.; Mustonen, J. Uric acid correlates with the severity of histopathological parameters in IgA nephropathy. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2005, 20, 89–95. [Google Scholar] [CrossRef]
- Nagasawa, Y.; Yamamoto, R.; Shoji, T.; Shinzawa, M.; Hasuike, Y.; Nagatoya, K.; Yamauchi, A.; Hayashi, T.; Kuragano, T.; Moriyama, T.; et al. Serum Uric Acid Level Predicts Progression of IgA Nephropathy in Females but Not in Males. PLoS ONE 2016, 11, e0160828. [Google Scholar] [CrossRef]
- Oh, T.R.; Choi, H.S.; Kim, C.S.; Kang, K.P.; Kwon, Y.J.; Kim, S.G.; Ma, S.K.; Kim, S.W.; Bae, E.H. The Effects of Hyperuricemia on the Prognosis of IgA Nephropathy are More Potent in Females. J. Clin. Med. 2020, 9, 176. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Pandya, B.J.; Choi, H.K. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011, 63, 3136–3141. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, J.M.; Chang, B.S.; Matarese, R.A.; Garella, S. Use of single voided urine samples to estimate quantitative proteinuria. N. Engl. J. Med. 1983, 309, 1543–1546. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Sinniah, R. IgA mesangial nephropathy: Berger’s disease. Am. J. Nephrol. 1985, 5, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, E. Reduced glomerular function and prevalence of gout: NHANES 2009–2010. PLoS ONE 2012, 7, e50046. [Google Scholar] [CrossRef]
- Haas, M. Histologic subclassification of IgA nephropathy: A clinicopathologic study of 244 cases. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 1997, 29, 829–842. [Google Scholar] [CrossRef]
- Cattran, D.C.; Coppo, R.; Cook, H.T.; Feehally, J.; Roberts, I.S.; Troyanov, S.; Alpers, C.E.; Amore, A.; Barratt, J.; Berthoux, F.; et al. The Oxford classification of IgA nephropathy: Rationale, clinicopathological correlations, and classification. Kidney Int. 2009, 76, 534–545. [Google Scholar] [CrossRef]
- Zeng, C.H.; Le, W.; Ni, Z.; Zhang, M.; Miao, L.; Luo, P.; Wang, R.; Lv, Z.; Chen, J.; Tian, J.; et al. A multicenter application and evaluation of the oxford classification of IgA nephropathy in adult chinese patients. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2012, 60, 812–820. [Google Scholar] [CrossRef]
- Hong, Y.A.; Min, J.W.; Ha, M.A.; Koh, E.S.; Kim, H.D.; Ban, T.H.; Kim, Y.S.; Kim, Y.K.; Kim, D.; Shin, S.J.; et al. The Impact of Obesity on the Severity of Clinicopathologic Parameters in Patients with IgA Nephropathy. J. Clin. Med. 2020, 9, 2824. [Google Scholar] [CrossRef]
- Fan, S.; Zhang, P.; Wang, A.Y.; Wang, X.; Wang, L.; Li, G.; Hong, D. Hyperuricemia and its related histopathological features on renal biopsy. BMC Nephrol. 2019, 20, 95. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Koo, H.M.; Lim, B.J.; Oh, H.J.; Yoo, D.E.; Shin, D.H.; Lee, M.J.; Doh, F.M.; Park, J.T.; Yoo, T.H.; et al. Decreased circulating C3 levels and mesangial C3 deposition predict renal outcome in patients with IgA nephropathy. PLoS ONE 2012, 7, e40495. [Google Scholar] [CrossRef]
- Nam, K.H.; Joo, Y.S.; Lee, C.; Lee, S.; Kim, J.; Yun, H.R.; Park, J.T.; Chang, T.I.; Ryu, D.R.; Yoo, T.H.; et al. Predictive value of mesangial C3 and C4d deposition in IgA nephropathy. Clin. Immunol. 2020, 211, 108331. [Google Scholar] [CrossRef]
- Caliskan, Y.; Ozluk, Y.; Celik, D.; Oztop, N.; Aksoy, A.; Ucar, A.S.; Yazici, H.; Kilicaslan, I.; Sever, M.S. The Clinical Significance of Uric Acid and Complement Activation in the Progression of IgA Nephropathy. Kidney Blood Press. Res. 2016, 41, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Ryu, E.S.; Kim, M.J.; Shin, H.S.; Jang, Y.H.; Choi, H.S.; Jo, I.; Johnson, R.J.; Kang, D.H. Uric acid-induced phenotypic transition of renal tubular cells as a novel mechanism of chronic kidney disease. Am. J. Physiol. Ren. Physiol. 2013, 304, F471–F480. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Mazzali, M.; Kang, D.H.; Kanellis, J.; Watanabe, S.; Sanchez-Lozada, L.G.; Rodriguez-Iturbe, B.; Herrera-Acosta, J.; Johnson, R.J. Hyperuricemia causes glomerular hypertrophy in the rat. Am. J. Nephrol. 2003, 23, 2–7. [Google Scholar] [CrossRef]
- Sánchez-Lozada, L.G.; Tapia, E.; Santamaría, J.; Avila-Casado, C.; Soto, V.; Nepomuceno, T.; Rodríguez-Iturbe, B.; Johnson, R.J.; Herrera-Acosta, J. Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int. 2005, 67, 237–247. [Google Scholar] [CrossRef]
- Corry, D.B.; Eslami, P.; Yamamoto, K.; Nyby, M.D.; Makino, H.; Tuck, M.L. Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system. J. Hypertens. 2008, 26, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Lozada, L.G.; Tapia, E.; Avila-Casado, C.; Soto, V.; Franco, M.; Santamaría, J.; Nakagawa, T.; Rodríguez-Iturbe, B.; Johnson, R.J.; Herrera-Acosta, J. Mild hyperuricemia induces glomerular hypertension in normal rats. Am. J. Physiol. Ren. Physiol. 2002, 283, F1105–F1110. [Google Scholar] [CrossRef]
- Takiue, Y.; Hosoyamada, M.; Kimura, M.; Saito, H. The effect of female hormones upon urate transport systems in the mouse kidney. Nucleosides Nucleic Acids 2011, 30, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Kelimu, A.; Satoshi, H.; Mareki, O.; Yasuhiko, T. Influence of Estrogen on the Progression of Kidney Injury in Murine IgA Nephropathy. Juntendo Med. J. 2017, 63, 178–185. [Google Scholar] [CrossRef]
- Mumford, S.L.; Dasharathy, S.S.; Pollack, A.Z.; Perkins, N.J.; Mattison, D.R.; Cole, S.R.; Wactawski-Wende, J.; Schisterman, E.F. Serum uric acid in relation to endogenous reproductive hormones during the menstrual cycle: Findings from the BioCycle study. Hum. Reprod. 2013, 28, 1853–1862. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 517) | Female (n = 264) | Male (n = 253) | |
|---|---|---|---|
| Uric acid (mg/dL) | 6.04 ± 1.88 | 5.27 ± 1.70 | 6.84 ± 1.72 |
| Age | 42.02 ± 14.68 | 42.37 ± 12.95 | 41.66 ± 16.31 |
| BMI (kg/m2) | 24.10 ± 3.98 | 23.68 ± 4.19 | 24.53 ± 3.71 |
| Alcohol (yes, %) | 92 (17.8) | 27 (10.3) | 65 (25.7) |
| Smoking (yes, %) | 71 (13.8) | 9 (3.4) | 62 (24.5) |
| DM (%) | 31 (6.0) | 16 (6.1) | 15 (5.9) |
| HTN (%) | 167 (33.3) | 79 (30.9) | 88 (35.9) |
| Systolic BP (mmHg) | 124.76 ± 16.28 | 122.28 ± 16.94 | 127.36 ± 15.16 |
| Diastolic BP (mmHg) | 76.36 ± 10.12 | 75.26 ± 9.82 | 77.51 ± 10.33 |
| Hemoglobin (g/dL) | 13.14 ± 1.95 | 12.34 ± 1.61 | 13.98 ± 1.93 |
| hs-CRP (mg/dL) | 0.59 ± 3.46 | 0.42 ± 1.46 | 0.75 ± 4.71 |
| Serum glucose (mg/dL) | 107.5 ± 31.65 | 108.94 ± 35.43 | 106.13 ± 27.24 |
| Serum creatinine (mg/dL) | 1.14 ± 0.92 | 0.98 ± 0.83 | 1.30 ± 0.99 |
| eGFR (mL/min/1.73 m2) | 81.86 ± 33.95 | 83.39 ± 33.56 | 80.25 ± 34.35 |
| Serum albumin (g/dL) | 4.01 ± 0.58 | 3.98 ± 0.53 | 4.04 ± 0.63 |
| AST (IU/L) | 23.31 ± 11.4 | 21.88 ± 10.99 | 24.80 ± 11.65 |
| ALT (IU/L) | 22.03 ± 24.6 | 17.69 ± 13.13 | 26.54 ± 32.00 |
| Total cholesterol (mg/dL) | 186.25 ± 49.8 | 192.09 ± 53.42 | 180.20 ± 45.12 |
| Triglyceride (mg/dL) | 153.95 ± 123.71 | 135.04 ± 92.71 | 173.54 ± 146.84 |
| LDL-C (mg/dL) | 107.67 ± 39.29 | 106.82 ± 35.88 | 108.56 ± 42.64 |
| HDL-C (mg/dL) | 52.17 ± 16.71 | 53.16 ± 17.82 | 51.15 ± 15.45 |
| Urine P/Cr (mg/mg) | 1.53 ± 2.49 | 1.37 ± 2.01 | 1.70 ± 2.90 |
| Urine RBCs (grade) | 2.85 ± 1.54 | 2.81 ± 1.59 | 2.89 ± 1.49 |
| Serum IgA (mg/dL) | 312.08 ± 147.8 | 307.51 ± 134.8 | 316.77 ± 160.34 |
| Uric Acid | ||||||
|---|---|---|---|---|---|---|
| Female UA ≤ 5.6 n = 169 | Female UA > 5.6 n = 95 | p Value # | Male UA ≤ 7.0 n = 145 | Male UA > 7.0 n = 108 | p Value ## | |
| Uric acid (mg/dL) | 4.28 ± 0.91 | 7.03 ± 1.33 | <0.001 | 5.67 ± 0.98 | 8.43 ± 1.12 | <0.001 |
| Age | 42.15 ± 12.30 | 42.76 ± 14.08 | 0.712 | 41.58 ± 17.27 | 41.75 ± 15.02 | 0.934 |
| Sex (%) | 169 (64) | 95 (35.9) | 145 (57.3) | 108 (42.7) | ||
| BMI (kg/m2) | 23.09 ± 3.49 | 24.75 ± 5.07 | 0.002 | 23.97 ± 3.81 | 25.8 ± 3.45 | 0.005 |
| Alcohol (yes, %) | 20 (11.8) | 5 (7.4) | 0.261 | 34 (23.4) | 31 (28.7) | 0.344 |
| Smoking (yes, %) | 6 (3.6) | 3 (3.2) | 0.333 | 36 (24.8) | 26 (24.1) | 0.959 |
| DM (%) | 6 (3.6) | 10 (10.6) | 0.021 | 10 (6.9) | 5 (4.6) | 0.450 |
| HTN (%) | 54 (32.9) | 25 (27.2) | 0.339 | 51 (36.2) | 37 (35.6) | 0.924 |
| Systolic BP (mmHg) | 118.76 ± 16.17 | 128.62 ± 16.53 | <0.001 | 126.90 ± 15.64 | 128.00 ± 14.54 | 0.571 |
| Diastolic BP (mmHg) | 73.80 ± 9.94 | 77.89 ± 9.07 | 0.001 | 77.25 ± 9.63 | 77.86 ± 11.25 | 0.643 |
| Hemoglobin (g/dL) | 12.49 ± 1.30 | 12.11 ± 2.04 | 0.088 | 14.07 ± 1.86 | 13.86 ± 2.03 | 0.399 |
| hs-CRP (mg/dL) | 0.33 ± 0.98 | 0.60 ± 2.06 | 0.151 | 0.88 ± 5.94 | 0.58 ± 2.01 | 0.623 |
| Serum glucose (mg/dL) | 109.80 ± 35.76 | 107.33 ± 34.94 | 0.597 | 105.78 ± 31.20 | 106.58 ± 21.00 | 0.819 |
| Serum creatinine (mg/dL) | 0.77 ± 0.48 | 1.36 ± 1.13 | <0.001 | 1.12 ± 1.02 | 1.55 ± 0.89 | 0.001 |
| eGFR (mL/min/1.73 m2) | 95.74 ± 29.24 | 61.18 ± 29.20 | <0.001 | 91.44 ± 32.75 | 64.95 ± 30.48 | <0.001 |
| Serum albumin (g/dL) | 4.06 ± 0.49 | 3.85 ± 0.59 | 0.003 | 4.11 ± 0.63 | 3.95 ± 0.63 | 0.051 |
| AST (IU/L) | 21.69 ± 11.00 | 22.23 ± 11.02 | 0.705 | 24.55 ± 11.11 | 25.12 ± 12.38 | 0.700 |
| ALT (IU/L) | 17.53 ± 14.05 | 17.98 ± 11.37 | 0.789 | 26.70 ± 38.39 | 26.33 ± 20.81 | 0.928 |
| Total cholesterol (mg/dL) | 186.04 ± 45.34 | 203.14 ± 64.49 | 0.013 | 175.23 ± 40.33 | 186.79 ± 50.21 | 0.044 |
| Triglyceride (mg/dL) | 126.05 ± 81.65 | 151.46 ± 108.64 | 0.034 | 149.41 ± 115.07 | 205.49 ± 176.06 | 0.003 |
| LDL-C (mg/dL) | 107.06 ± 39.54 | 117.12 ± 47.9 | 0.075 | 101.08 ± 31.67 | 109.22 ± 38.73 | 0.071 |
| HDL-C (mg/dL) | 58.47 ± 19.41 | 53.51 ± 15.28 | 0.036 | 50.73 ± 13.82 | 43.20 ± 11.93 | <0.001 |
| Urine P/Cr (mg/mg) | 1.12 ± 1.79 | 2.68 ± 4.14 | <0.001 | 1.11 ± 1.46 | 1.73 ± 2.35 | 0.013 |
| Urine RBCs (grade) | 2.89 ± 1.53 | 2.76 ± 1.55 | 0.514 | 2.90 ± 1.57 | 2.78 ± 1.51 | 0.558 |
| Serum IgA (mg/dL) | 285.74 ± 97.25 | 333.46 ± 165.03 | 0.004 | 308.97 ± 129.20 | 338.48 ± 204.68 | 0.169 |
| Uric Acid | |||||||
|---|---|---|---|---|---|---|---|
| Female UA ≤ 5.6 | Female UA > 5.6 | p Value # | Male UA ≤ 7.0 | Male UA > 7.0 | p Value ## | ||
| Light microscopy | |||||||
| Global sclerosis (%) | 13.96 ± 15.12 | 25.86 ± 24.84 | <0.001 | 13.85 ± 16.44 | 21.09 ± 22.70 | 0.004 | |
| Segmental sclerosis (%) | 7.31 ± 11.99 | 13.66 ± 16.99 | 0.001 | 6.94 ± 9.67 | 11.68 ± 13.84 | 0.002 | |
| Capsular adhesion (%) | 7.31 ± 11.99 | 13.66 ± 16.99 | 0.002 | 6.84 ± 10.32 | 11.49 ± 14.63 | 0.004 | |
| Mesangial matrix expansion (0–4) | 1.97 ± 0.89 | 2.23 ± 0.83 | 0.023 | 2.10 ± 0.87 | 2.32 ± 0.78 | 0.037 | |
| Mesangial cell proliferation (0–4) | 2.01 ± 0.88 | 2.17 ± 0.86 | 0.162 | 2.15 ± 0.83 | 2.23 ± 0.84 | 0.444 | |
| Endocapillary proliferation (0–4) | 0.11 ± 0.40 | 0.25 ± 0.76 | 0.058 | 0.08 ± 0.33 | 0.29 ± 0.64 | 0.001 | |
| Interstitial fibrosis (0–4) | 1.08 ± 0.86 | 1.67 ± 1.03 | <0.001 | 1.22 ± 0.95 | 1.77 ± 0.93 | <0.001 | |
| Tubular atrophy (0–4) | 1.04 ± 0.86 | 1.62 ± 1.07 | <0.001 | 1.22 ± 0.95 | 1.72 ± 0.94 | <0.001 | |
| Immunofluorescence microscopy | |||||||
| IgA Mesangial deposit (0–4) | 3.24 ± 0.95 | 3.27 ± 1.11 | 0.794 | 3.36 ± 0.84 | 3.35 ± 0.98 | 0.895 | |
| C3 Mesangial deposit (0–4) | 1.97 ± 1.18 | 2.18 ± 1.35 | 0.199 | 2.20 ± 1.10 | 2.26 ± 1.05 | 0.676 | |
| C4d Mesangial deposit (0–4) | 0.02 ± 0.22 | 0.02 ± 0.20 | 0.882 | 0.05 ± 0.32 | 0.05 ± 0.33 | 0.940 | |
| WHO classification (n = 437) | |||||||
| Grade (1–6) | 2.83 ± 0.72 | 3.38 ± 0.83 | <0.001 | 2.86 ± 0.83 | 3.25 ± 0.97 | 0.002 | |
| Univariable | Multivariable | |||||||
|---|---|---|---|---|---|---|---|---|
| β | t | r2 | p Value | β | t | r2 | p Value | |
| Global sclerosis | 0.258 | 6.071 | 0.001 | <0.001 | 0.146 | 3.075 | 0.059 | 0.002 |
| Segmental sclerosis | 0.166 | 3.812 | 0.001 | <0.001 | 0.130 | 2.860 | 0.087 | 0.004 |
| Mesangial matrix expansion | 0.172 | 3.950 | 0.007 | <0.001 | 0.168 | 3.6660 | 0.031 | <0.001 |
| Capsular adhesion | −0.003 | −0.071 | 0.000 | 0.943 | - | - | - | - |
| Endocapillary proliferation | 0.200 | 4.623 | 0.001 | <0.001 | 0.164 | 2.240 | 0.037 | 0.026 |
| Interstitial fibrosis | 0.332 | 7.951 | 0.001 | <0.001 | 0.218 | 4.743 | 0.023 | <0.001 |
| Tubular atrophy | 0.340 | 8.169 | 0.001 | <0.001 | 0.260 | 5.452 | 0.030 | <0.001 |
| IgA mesangial deposit | 0.003 | 0.078 | 0.000 | 0.938 | - | - | - | - |
| C3 mesangial deposit | 0.118 | 2.680 | 0.002 | 0.008 | 0.093 | 20.90 | 0.027 | 0.037 |
| C4 mesangial deposit | 0.074 | 1.679 | 0.002 | 0.094 | - | - | - | |
| (a) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Univariable | ||||||||
| Female | Male | |||||||
| β | t | r2 | p Value | β | t | r2 | p Value | |
| Global sclerosis | 0.359 | 6.184 | 0.129 | <0.001 | 0.176 | 2.811 | 0.031 | 0.005 |
| Segmental sclerosis | 0.225 | 3.730 | 0.025 | <0.001 | 0.157 | 2.500 | 0.025 | 0.013 |
| Mesangial matrix expansion | 0.208 | 3.444 | 0.043 | 0.001 | 0.097 | 1.542 | 0.009 | 0.124 |
| Capsular adhesion | 0.187 | 2.996 | 0.035 | 0.003 | 0.146 | 2.297 | 0.017 | 0.022 |
| Endocapillary proliferation | 0.268 | 4.488 | 0.072 | <0.001 | 0.155 | 2.485 | 0.024 | 0.014 |
| Interstitial fibrosis | 0.392 | 6.886 | 0.154 | <0.001 | 0.263 | 4.280 | 0.069 | <0.001 |
| Tubular atrophy | 0.396 | 6.970 | 0.157 | <0.001 | 0.265 | 4.317 | 0.070 | <0.001 |
| IgA mesangial deposit | 0.030 | 0.483 | 0.001 | 0.629 | −0.080 | −1.269 | 0.006 | 0.206 |
| C3 mesangial deposit | 0.130 | 2.111 | 0.017 | 0.036 | 0.052 | 0.822 | 0.003 | 0.412 |
| C4 mesangial deposit | 0.055 | 0.885 | 0.003 | 0.377 | −0.026 | −0.398 | 0.001 | 0.691 |
| (b) | ||||||||
| Multivariable | ||||||||
| Female | Male | |||||||
| β | t | r2 | p Value | β | t | r2 | p Value | |
| Global sclerosis | 0.112 | 1.689 | 0.316 | 0.092 | - | - | - | |
| Segmental sclerosis | 0.584 | 0.044 | 0.171 | 0.573 | - | - | - | |
| Mesangial matrix expansion | 0.189 | 2.989 | 0.036 | 0.003 | - | - | - | |
| Capsular adhesion | - | - | - | - | - | - | - | |
| Endocapillary proliferation | 0.224 | 3.367 | 0.117 | 0.001 | - | - | - | |
| Interstitial fibrosis | 0.155 | 2.282 | 0.301 | 0.023 | 0.093 | 1.432 | 0.357 | 0.154 |
| Tubular atrophy | 0.188 | 2.769 | 0.304 | 0.006 | 0.102 | 1.581 | 0.354 | 0.115 |
| IgA mesangial deposit | - | - | - | −0.105 | −1.623 | 0.063 | 0.106 | |
| C3 mesangial deposit | - | - | - | - | - | - | ||
| C4 mesangial deposit | - | - | - | - | - | - | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, W.J.; Hong, Y.A.; Min, J.W.; Koh, E.S.; Kim, H.D.; Ban, T.H.; Kim, Y.S.; Kim, Y.K.; Shin, S.J.; Kim, S.Y.; et al. The Serum Uric Acid Level Is Related to the More Severe Renal Histopathology of Female IgA Nephropathy Patients. J. Clin. Med. 2021, 10, 1885. https://doi.org/10.3390/jcm10091885
Choi WJ, Hong YA, Min JW, Koh ES, Kim HD, Ban TH, Kim YS, Kim YK, Shin SJ, Kim SY, et al. The Serum Uric Acid Level Is Related to the More Severe Renal Histopathology of Female IgA Nephropathy Patients. Journal of Clinical Medicine. 2021; 10(9):1885. https://doi.org/10.3390/jcm10091885
Chicago/Turabian StyleChoi, Won Jung, Yu A Hong, Ji Won Min, Eun Sil Koh, Hyung Duk Kim, Tae Hyun Ban, Young Soo Kim, Yong Kyun Kim, Seok Joon Shin, Seok Young Kim, and et al. 2021. "The Serum Uric Acid Level Is Related to the More Severe Renal Histopathology of Female IgA Nephropathy Patients" Journal of Clinical Medicine 10, no. 9: 1885. https://doi.org/10.3390/jcm10091885
APA StyleChoi, W. J., Hong, Y. A., Min, J. W., Koh, E. S., Kim, H. D., Ban, T. H., Kim, Y. S., Kim, Y. K., Shin, S. J., Kim, S. Y., Kim, Y. O., Yang, C. W., & Chang, Y.-K. (2021). The Serum Uric Acid Level Is Related to the More Severe Renal Histopathology of Female IgA Nephropathy Patients. Journal of Clinical Medicine, 10(9), 1885. https://doi.org/10.3390/jcm10091885






