Lymphaticovenous Anastomosis Supermicrosurgery Decreases Oxidative Stress and Increases Antioxidant Capacity in the Serum of Lymphedema Patients
Abstract
1. Introduction
2. Material and Methods
2.1. Study Participants
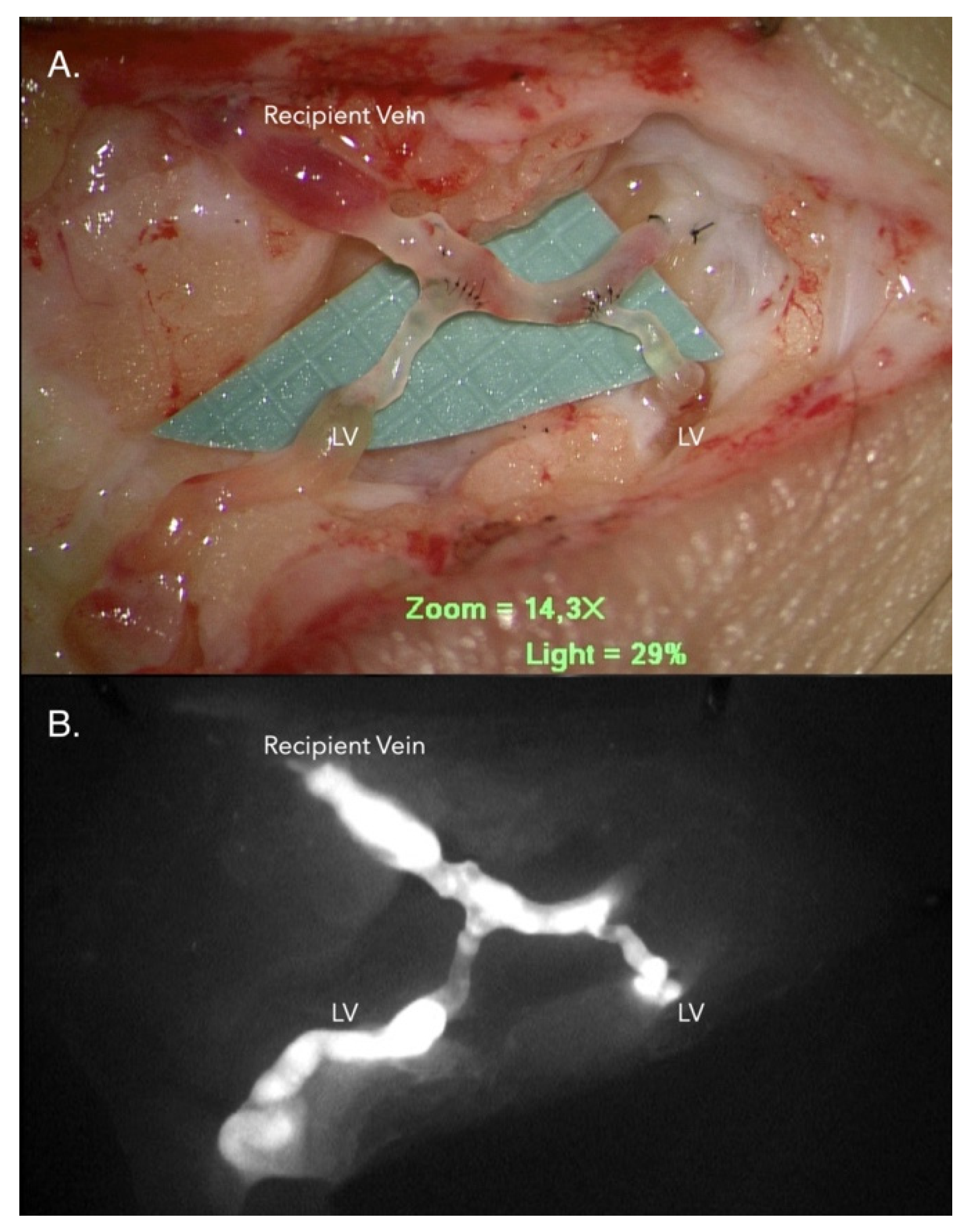
2.2. LVA Operative Technique
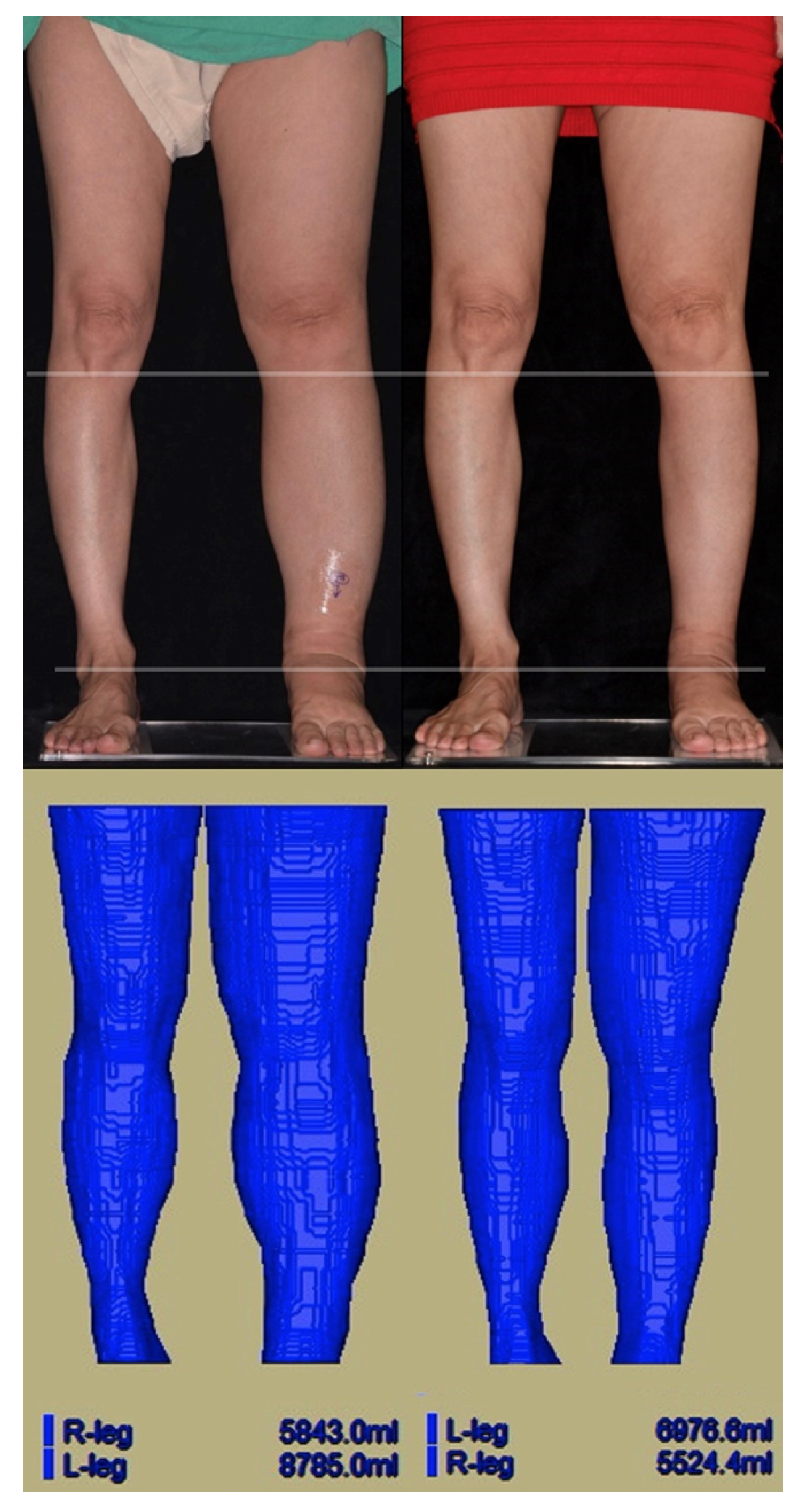
2.3. Magnetic Resonance (MR) Volumetry
2.4. Sample Collection
2.5. iTRAQ-Based Quantitative Proteomic Analysis
2.6. Validation of the Protein Expression by ELISA
2.7. Oxidative Stress Panel Kit
2.8. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. iTRAQ-Based Quantitative Proteomic Analysis
3.3. Measurement by Oxidative Stress Panel
3.4. Comparison of the Patients with Good vs. Fair Outcomes of Volume Reduction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Rockson, S.G. The lymphatics and the inflammatory response: Lessons learned from human lymphedema. Lymphat. Res. Biol. 2013, 11, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Grada, A.A.; Phillips, T.J. Lymphedema: Pathophysiology and clinical manifestations. J. Am. Acad. Dermatol. 2017, 77, 1009–1020. [Google Scholar] [CrossRef]
- Rockson, S.G.; Rivera, K.K. Estimating the population burden of lymphedema. Ann. N. Y. Acad. Sci. 2008, 1131, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, M.; Shimono, R.; Tsuru, S.; Kitamura, K.; Sakuda, H.; Oguchi, H.; Hirota, A. Risk factors for late-onset lower limb lymphedema after gynecological cancer treatment: A multi-institutional retrospective study. Eur. J. Surg. Oncol. 2020, 46, 1334–1338. [Google Scholar] [CrossRef]
- Ryan, M.; Stainton, M.C.; Slaytor, E.K.; Jaconelli, C.; Watts, S.; Mackenzie, P. Aetiology and prevalence of lower limb lymphoedema following treatment for gynaecological cancer. Aust. N. Z. J. Obstet. Gynaecol. 2003, 43, 148–151. [Google Scholar] [CrossRef]
- Cabello-Verrugio, C.; Simon, F.; Trollet, C.; Santibanez, J.F. Oxidative Stress in Disease and Aging: Mechanisms and Therapies 2016. Oxid. Med. Cell Longev. 2017, 2017, 4310469. [Google Scholar] [CrossRef]
- Steven, S.; Frenis, K.; Oelze, M.; Kalinovic, S.; Kuntic, M.; Bayo Jimenez, M.T.; Vujacic-Mirski, K.; Helmstadter, J.; Kroller-Schon, S.; Munzel, T.; et al. Vascular Inflammation and Oxidative Stress: Major Triggers for Cardiovascular Disease. Oxid. Med. Cell Longev. 2019, 2019, 7092151. [Google Scholar] [CrossRef]
- Vallee, A.; Lecarpentier, Y.; Guillevin, R.; Vallee, J.N. Circadian rhythms, Neuroinflammation and Oxidative Stress in the Story of Parkinson’s Disease. Cells 2020, 9, 314. [Google Scholar] [CrossRef]
- Zinellu, E.; Zinellu, A.; Fois, A.G.; Fois, S.S.; Piras, B.; Carru, C.; Pirina, P. Reliability and Usefulness of Different Biomarkers of Oxidative Stress in Chronic Obstructive Pulmonary Disease. Oxid. Med. Cell Longev. 2020, 2020, 4982324. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.J.; Kang, S.W. Reactive oxygen species and tumor metastasis. Mol. Cells 2013, 35, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Novaes, R.D.; Teixeira, A.L.; de Miranda, A.S. Oxidative Stress in Microbial Diseases: Pathogen, Host, and Therapeutics. Oxid. Med. Cell Longev. 2019, 2019, 8159562. [Google Scholar] [CrossRef] [PubMed]
- Bertelli, M.; Kiani, A.K.; Paolacci, S.; Manara, E.; Dautaj, A.; Beccari, T.; Michelini, S. Molecular pathways involved in lymphedema: Hydroxytyrosol as a candidate natural compound for treating the effects of lymph accumulation. J. Biotechnol. 2020, 308, 82–86. [Google Scholar] [CrossRef]
- Michelini, S.; Cestari, M.; Michelini, S.; Camilleri, G.; De Antoni, L.; Sonna, W.N.; Bertelli, M. Study of a supplement and a genetic test for lymphedema management. Acta Biomed. 2020, 91, e2020013. [Google Scholar] [CrossRef] [PubMed]
- Beier, A.; Siems, W.; Brenke, R.; Grune, T. Increased formation of free radicals in chronic lymphedema. Z. Lymphol. 1994, 18, 8–11. [Google Scholar] [PubMed]
- Chang, T.C.; Uen, Y.H.; Chou, C.H.; Sheu, J.R.; Chou, D.S. The role of cyclooxygenase-derived oxidative stress in surgically induced lymphedema in a mouse tail model. Pharm. Biol. 2013, 51, 573–580. [Google Scholar] [CrossRef]
- Siems, W.G.; Brenke, R.; Beier, A.; Grune, T. Oxidative stress in chronic lymphoedema. QJM 2002, 95, 803–809. [Google Scholar] [CrossRef]
- Tabibiazar, R.; Cheung, L.; Han, J.; Swanson, J.; Beilhack, A.; An, A.; Dadras, S.S.; Rockson, N.; Joshi, S.; Wagner, R.; et al. Inflammatory Manifestations of Experimental Lymphatic Insufficiency. PLoS Med. 2006, 3, e254. [Google Scholar] [CrossRef]
- Chaniotakis, I.; Charalampidis, P.S.; Gaitanis, G.; Kalfakakou, V.; Simos, I.; Evangelou, A.; Bassukas, I.D. Serum anti-oxidative reserves during cellulitis: A pilot study. Eur. J. Dermatol. 2017, 27, 431–433. [Google Scholar] [CrossRef]
- Pfister, C.; Dawzcynski, H.; Schingale, F.J. Sodium selenite and cancer related lymphedema: Biological and pharmacological effects. J. Trace Elem. Med. Biol. 2016, 37, 111–116. [Google Scholar] [CrossRef]
- Schaverien, M.V.; Coroneos, C.J. Surgical Treatment of Lymphedema. Plast. Reconstr. Surg. 2019, 144, 738–758. [Google Scholar] [CrossRef] [PubMed]
- Mihara, M.; Hara, H.; Tsubaki, H.; Suzuki, T.; Yamada, N.; Kawahara, M.; Murai, N. Combined conservative treatment and lymphatic venous anastomosis for severe lower limb lymphedema with recurrent cellulitis. Ann. Vasc. Surg. 2015, 29, 1318.e11–1318.e15. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Agko, M.; Perez Coca, J.J.; Manrique, O.J.; Chang, W.L.; Nicoli, F.; Chen, S.H.; Chen, H.C. Comparison of long-term clinical outcomes among different vascularized lymph node transfers: 6-year experience of a single center’s approach to the treatment of lymphedema. J. Surg. Oncol. 2017, 116, 671–682. [Google Scholar] [CrossRef] [PubMed]
- Di Taranto, G.; Bolletta, A.; Chen, S.H.; Losco, L.; Elia, R.; Cigna, E.; Rubino, C.; Ribuffo, D.; Chen, H.C. A prospective study on combined lymphedema surgery: Gastroepiploic vascularized lymph nodes transfer and lymphaticovenous anastomosis followed by suction lipectomy. Microsurgery 2021, 41, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.G.H.; Wallmichrath, J.; Weiss, M.; Baumeister, S.H.C.; Frick, A. Microsurgical lymphatic vascular grafting and secondary liposuction: Results of combination treatment in secondary lymphedema. Lymphology 2020, 53, 38–47. [Google Scholar] [PubMed]
- Sharkey, A.R.; King, S.W.; Ramsden, A.J.; Furniss, D. Do surgical interventions for limb lymphoedema reduce cellulitis attack frequency? Microsurgery 2017, 37, 348–353. [Google Scholar] [CrossRef]
- Koshima, I.; Inagawa, K.; Urushibara, K.; Moriguchi, T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities. J. Reconstr. Microsurg. 2000, 16, 437–442. [Google Scholar] [CrossRef]
- Koshima, I.; Nanba, Y.; Tsutsui, T.; Takahashi, Y.; Itoh, S. Long-term follow-up after lymphaticovenular anastomosis for lymphedema in the leg. J. Reconstr. Microsurg. 2003, 19, 209–215. [Google Scholar] [CrossRef]
- Mihara, M.; Hara, H.; Furniss, D.; Narushima, M.; Iida, T.; Kikuchi, K.; Ohtsu, H.; Gennaro, P.; Gabriele, G.; Murai, N. Lymphaticovenular anastomosis to prevent cellulitis associated with lymphoedema. Br. J. Surg. 2014, 101, 1391–1396. [Google Scholar] [CrossRef]
- Mihara, M.; Hara, H.; Tange, S.; Zhou, H.P.; Kawahara, M.; Shimizu, Y.; Murai, N. Multisite Lymphaticovenular Bypass Using Supermicrosurgery Technique for Lymphedema Management in Lower Lymphedema Cases. Plast. Reconstr. Surg. 2016, 138, 262–272. [Google Scholar] [CrossRef]
- Yamamoto, T.; Koshima, I. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast. Reconstr. Surg. 2014, 133, 887e–888e. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Yamamoto, N.; Fuse, Y.; Narushima, M.; Koshima, I. Optimal Sites for Supermicrosurgical Lymphaticovenular Anastomosis: An Analysis of Lymphatic Vessel Detection Rates on 840 Surgical Fields in Lower Extremity Lymphedema Patients. Plast. Reconstr. Surg. 2018, 142, 924e–930e. [Google Scholar] [CrossRef]
- Yang, J.C.; Wu, S.C.; Chiang, M.H.; Lin, W.C.; Chiang, P.L.; Hsieh, C.H. Supermicrosurgical Lymphaticovenous Anastomosis as an Alternative Treatment Option for Moderate-to-Severe Lower Limb Lymphedema. J. Am. Coll. Surg. 2020, 230, 216–227. [Google Scholar] [CrossRef]
- Yang, J.C.; Yen, Y.H.; Wu, S.C.; Lin, W.C.; Chiang, M.H.; Hsieh, C.H. Supermicrosurgical Lymphaticovenous Anastomosis as an Alternative Treatment Option for Patients with Lymphorrhea. Plast. Reconstr. Surg. 2019, 14, 1214–1224. [Google Scholar] [CrossRef]
- Rocha, S.; Gomes, D.; Lima, M.; Bronze-da-Rocha, E.; Santos-Silva, A. Peroxiredoxin 2, glutathione peroxidase, and catalase in the cytosol and membrane of erythrocytes under H2O2-induced oxidative stress. Free Radic. Res. 2015, 49, 990–1003. [Google Scholar] [CrossRef] [PubMed]
- Gaetani, G.F.; Ferraris, A.M.; Rolfo, M.; Mangerini, R.; Arena, S.; Kirkman, H.N. Predominant role of catalase in the disposal of hydrogen peroxide within human erythrocytes. Blood 1996, 87, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Sepasi Tehrani, H.; Moosavi-Movahedi, A.A. Catalase and its mysteries. Prog. Biophys. Mol. Biol. 2018, 140, 5–12. [Google Scholar] [CrossRef]
- Bayer, S.B.; Maghzal, G.; Stocker, R.; Hampton, M.B.; Winterbourn, C.C. Neutrophil-mediated oxidation of erythrocyte peroxiredoxin 2 as a potential marker of oxidative stress in inflammation. FASEB J. 2013, 27, 3315–3322. [Google Scholar] [CrossRef]
- Kim, Y.; Jang, H.H. Role of Cytosolic 2-Cys Prx1 and Prx2 in Redox Signaling. Antioxidants 2019, 8, 169. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Su, G.; Gao, J.; Tian, Y.; Liu, X.; Zhang, Z. Effects of Peroxiredoxin 2 in Neurological Disorders: A Review of its Molecular Mechanisms. Neurochem. Res. 2020, 45, 720–730. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.H.; Kim, S.U.; Kwon, T.H.; Lee, D.S.; Ha, H.L.; Park, D.S.; Woo, E.J.; Lee, S.H.; Kim, J.M.; Chae, H.B.; et al. Peroxiredoxin II is essential for preventing hemolytic anemia from oxidative stress through maintaining hemoglobin stability. Biochem. Biophys. Res. Commun. 2012, 426, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Sharapov, M.G.; Novoselov, V.I.; Penkov, N.V.; Fesenko, E.E.; Vedunova, M.V.; Bruskov, V.I.; Gudkov, S.V. Protective and adaptogenic role of peroxiredoxin 2 (Prx2) in neutralization of oxidative stress induced by ionizing radiation. Free Radic. Biol. Med. 2019, 134, 76–86. [Google Scholar] [CrossRef] [PubMed]
- de Godoy, J.M.; de Godoy, M.F.; Valente, A.; Camacho, E.L.; Paiva, E.V. Lymphoscintigraphic evaluation in patients after erysipelas. Lymphology 2000, 33, 177–180. [Google Scholar] [PubMed]
- Ghiselli, A.; Serafini, M.; Natella, F.; Scaccini, C. Total antioxidant capacity as a tool to assess redox status: Critical view and experimental data. Free Radic. Biol. Med. 2000, 29, 1106–1114. [Google Scholar] [CrossRef]
- Lorente, L.; Martin, M.M.; Perez-Cejas, A.; Abreu-Gonzalez, P.; Lopez, R.O.; Ferreres, J.; Sole-Violan, J.; Labarta, L.; Diaz, C.; Palmero, S.; et al. Serum total antioxidant capacity during the first week of sepsis and mortality. J. Crit. Care 2018, 47, 139–144. [Google Scholar] [CrossRef]
- Lorente, L.; Martin, M.M.; Almeida, T.; Abreu-Gonzalez, P.; Ferreres, J.; Sole-Violan, J.; Labarta, L.; Diaz, C.; Jimenez, A. Association between serum total antioxidant capacity and mortality in severe septic patients. J. Crit. Care 2015, 30, 217.e7–217.e12. [Google Scholar] [CrossRef]
- Benhar, M. Roles of mammalian glutathione peroxidase and thioredoxin reductase enzymes in the cellular response to nitrosative stress. Free Radic. Biol. Med. 2018, 127, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Michiels, C.; Raes, M.; Toussaint, O.; Remacle, J. Importance of Se-glutathione peroxidase, catalase, and Cu/Zn-SOD for cell survival against oxidative stress. Free Radic. Biol. Med. 1994, 17, 235–248. [Google Scholar] [CrossRef]
- Valavanidis, A.; Vlachogianni, T.; Fiotakis, C. 8-hydroxy-2′ -deoxyguanosine (8-OHdG): A critical biomarker of oxidative stress and carcinogenesis. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2009, 27, 120–139. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B. Can oxidative DNA damage be used as a biomarker of cancer risk in humans? Problems, resolutions and preliminary results from nutritional supplementation studies. Free Radic. Res. 1998, 29, 469–486. [Google Scholar] [CrossRef]
- Halliwell, B. Why and how should we measure oxidative DNA damage in nutritional studies? How far have we come? Am. J. Clin. Nutr. 2000, 72, 1082–1087. [Google Scholar] [CrossRef]
- Heffernan, A.L.; Aylward, L.L.; Toms, L.M.; Sly, P.D.; Macleod, M.; Mueller, J.F. Pooled biological specimens for human biomonitoring of environmental chemicals: Opportunities and limitations. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Bignert, A.; Eriksson, U.; Nyberg, E.; Miller, A.; Danielsson, S. Consequences of using pooled versus individual samples for designing environmental monitoring sampling strategies. Chemosphere 2014, 94, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Skoumas, I.; Papademetriou, L.; Economou, M.; Stefanadis, C. The implication of obesity on total antioxidant capacity in apparently healthy men and women: The ATTICA study. Nutr. Metab. Cardiovasc. Dis. 2007, 17, 590–597. [Google Scholar] [CrossRef] [PubMed]
| Gene Names | Protein Names | Fold Change | p Value |
|---|---|---|---|
| IGHV3-30 | Ig heavy chain V-III region CAM | 4.58 | 0.384 |
| KRT1 | Keratin, type II cytoskeletal 1 | 2.18 | 0.408 |
| ALB | Serum albumin | 1.69 | 0.259 |
| KRT9 | Keratin, type I cytoskeletal 9 | 1.69 | 0.402 |
| THBS1 | Thrombospondin-1 | −1.53 | 0.101 |
| CAT | Catalase | −1.58 | 0.049 |
| PRDX2 | Peroxiredoxin-2 | −1.68 | 0.022 |
| RPS27A | Ubiquitin-40S ribosomal protein S27a | −1.69 | 0.169 |
| SAA1 | Serum amyloid A-1 protein | −1.73 | 0.289 |
| CA1 | Carbonic anhydrase 1 | −1.89 | 0.039 |
| HBD | Hemoglobin subunit delta | −2.42 | 0.140 |
| HBB | Hemoglobin subunit beta | −2.62 | 0.067 |
| CA2 | Carbonic anhydrase 2 | −2.64 | 0.066 |
| HBA1 | Hemoglobin subunit alpha | −3.09 | 0.035 |
| Pre-LVA | Post-LVA | p Value | |
|---|---|---|---|
| iTRAQ-identified protein | |||
| CAT, ng/mL | 2651 ± 2101 | 1448 ± 593 | 0.033 |
| PRDX2, pg/mL | 4444 ± 5972 | 1083 ± 2260 | 0.066 |
| CA1, IU/mL | 576 ± 296 | 593 ± 378 | 0.703 |
| CA2, pg/mL | 436 ± 335 | 427 ± 391 | 0.752 |
| Oxidative Stress Panel | |||
| TAC, umole/L | 441 ± 81 | 488 ± 59 | 0.031 |
| GPX, U/g | 73 ± 20 | 92 ± 29 | 0.018 |
| 8-OHdG, ng/mg | 41 ± 12 | 45 ± 10 | 0.501 |
| MPO, ng/mL | 67 ± 21 | 79 ± 23 | 0.255 |
| Good Outcome | Fair Outcome | p Value | |
|---|---|---|---|
| iTRAQ-identified protein | |||
| CAT, ng/mL | −2593 ± 2363 | 178 ± 603 | 0.021 |
| PRDX2, pg/mL | −7782 ± 7347 | −397 ± 1235 | 0.037 |
| CA1, IU/mL | 14 ± 175 | 126 ± 312 | 0.426 |
| CA2, pg/mL | 0.05 ± 0.04 | −0.03 ± 0.14 | 0.199 |
| Oxidative Stress Panel | |||
| TAC, umole/L | 21 ± 23 | 40 ± 39 | 0.406 |
| GPX, U/g | 12 ± 14 | 20 ± 25 | 0.557 |
| 8-OHdG, ng/mg | 4 ± 15 | 7 ± 19 | 0.799 |
| MPO, ng/mL | 9.0 ± 13 | 14 ± 45 | 0.833 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, J.C.-S.; Huang, L.-H.; Wu, S.-C.; Kuo, P.-J.; Wu, Y.-C.; Wu, C.-J.; Lin, C.-W.; Tsai, P.-Y.; Hsieh, C.-H. Lymphaticovenous Anastomosis Supermicrosurgery Decreases Oxidative Stress and Increases Antioxidant Capacity in the Serum of Lymphedema Patients. J. Clin. Med. 2021, 10, 1540. https://doi.org/10.3390/jcm10071540
Yang JC-S, Huang L-H, Wu S-C, Kuo P-J, Wu Y-C, Wu C-J, Lin C-W, Tsai P-Y, Hsieh C-H. Lymphaticovenous Anastomosis Supermicrosurgery Decreases Oxidative Stress and Increases Antioxidant Capacity in the Serum of Lymphedema Patients. Journal of Clinical Medicine. 2021; 10(7):1540. https://doi.org/10.3390/jcm10071540
Chicago/Turabian StyleYang, Johnson Chia-Shen, Lien-Hung Huang, Shao-Chun Wu, Pao-Jen Kuo, Yi-Chan Wu, Chia-Jung Wu, Chia-Wei Lin, Pei-Yu Tsai, and Ching-Hua Hsieh. 2021. "Lymphaticovenous Anastomosis Supermicrosurgery Decreases Oxidative Stress and Increases Antioxidant Capacity in the Serum of Lymphedema Patients" Journal of Clinical Medicine 10, no. 7: 1540. https://doi.org/10.3390/jcm10071540
APA StyleYang, J. C.-S., Huang, L.-H., Wu, S.-C., Kuo, P.-J., Wu, Y.-C., Wu, C.-J., Lin, C.-W., Tsai, P.-Y., & Hsieh, C.-H. (2021). Lymphaticovenous Anastomosis Supermicrosurgery Decreases Oxidative Stress and Increases Antioxidant Capacity in the Serum of Lymphedema Patients. Journal of Clinical Medicine, 10(7), 1540. https://doi.org/10.3390/jcm10071540









