Big Data in Studying Acute Pain and Regional Anesthesia
Abstract
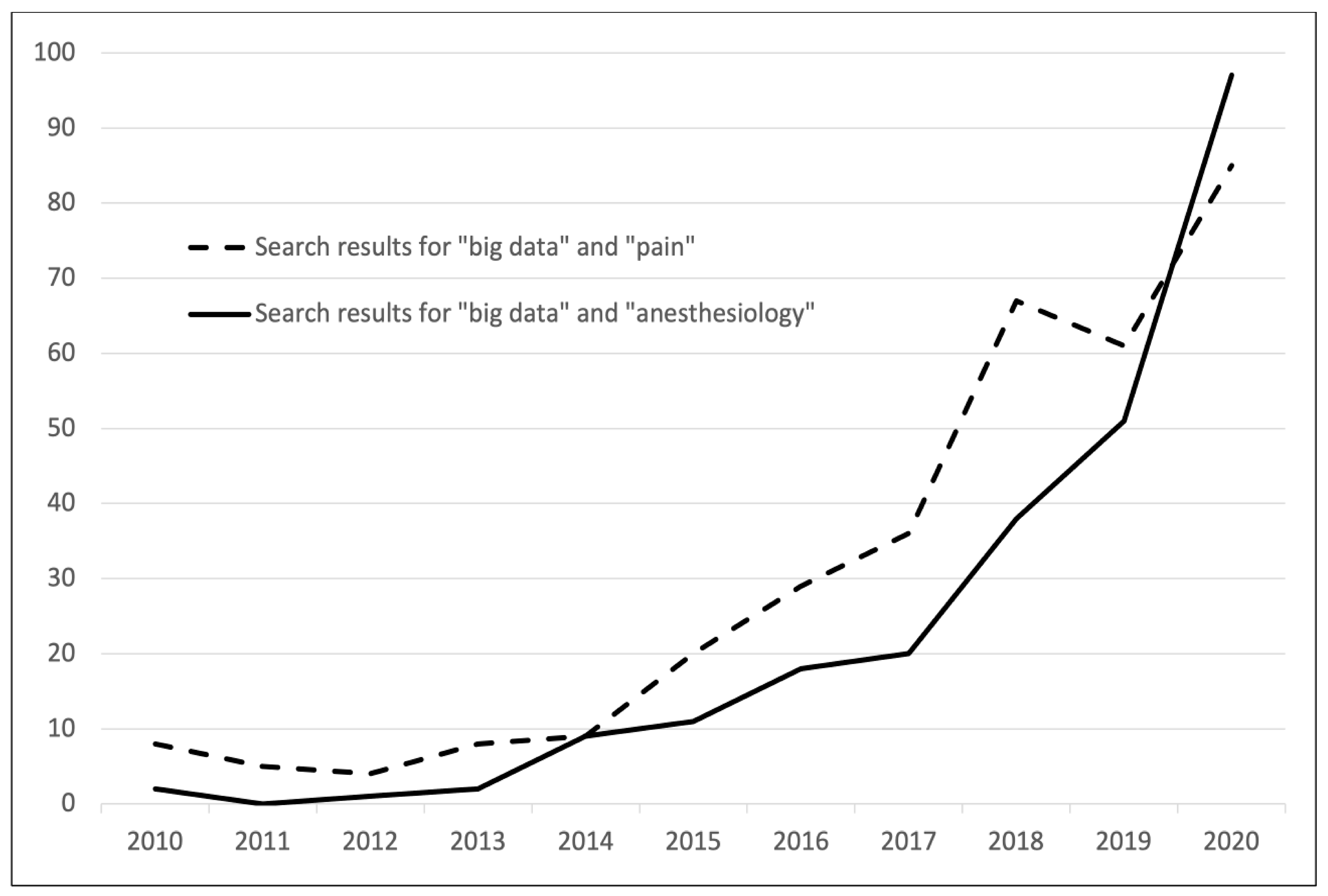
1. Introduction
2. Making Data Accessible for Research
3. Big Data Initiatives in Acute Pain and Regional Anesthesia Research
4. Artificial Intelligence and Machine-Learning Methods
5. A Look into the Future
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Franklin, J.M.; Schneeweiss, S. When and How Can Real World Data Analyses Substitute for Randomized Controlled Trials? Clin. Pharmacol. Ther. 2017, 102, 924–933. [Google Scholar] [CrossRef]
- Definition of “Big Data”. Available online: https://www.lexico.com/en/definition/big_data (accessed on 27 December 2020).
- Cadwalladr, C.; Graham-Harrison, E. Revealed: 50 million Facebook profiles harvested for Cambridge Analytica in major data breach. Guardian 2018, 17, 22. [Google Scholar]
- NHS Digital. Available online: https://digital.nhs.uk (accessed on 3 February 2021).
- Semler, S.C.; Wissing, F.; Heyder, R. German Medical Informatics Initiative. Methods Inf. Med. 2018, 57, e50–e56. [Google Scholar] [CrossRef] [PubMed]
- Antonsen, K.; Rosenstock, C.; Hyldborg Lundstrom, L. The Danish Anaesthesia Database. Clin. Epidemiol. 2016, 8, 435–438. [Google Scholar] [CrossRef]
- Vetter, T.R.; Schober, P. Regression: The apple does not fall far from the tree. Anesth. Analg. 2018, 127, 277–283. [Google Scholar] [CrossRef]
- Aoyama, K.; Pinto, R.; Ray, J.G.; Hill, A.; Scales, D.C.; Fowler, R.A. Determining Associations and Estimating Effects with Regression Models in Clinical Anesthesia. Anesthesiology 2020, 133, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.H. Multivariable Analysis: A Primer for Readers of Medical Research. Ann. Intern. Med. 2003, 138, 644–650. [Google Scholar] [CrossRef]
- Schulte, P.J.; Mascha, E.J. Propensity score methods: Theory and practice for anesthesia research. Anesth. Analg. 2018, 127, 1074–1084. [Google Scholar] [CrossRef]
- VanderWeele, T.J. Mediation Analysis: A Practitioner’s Guide. Annu. Rev. Public Health 2016, 37, 17–32. [Google Scholar] [CrossRef]
- Mascha, E.J.; Dalton, J.E.; Kurz, A.; Saager, L. Understanding the mechanism: Mediation analysis in randomized and nonrandomized studies. Anesth. Analg. 2013, 117, 980–994. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Vetter, T.R. Repeated measures designs and analysis of longitudinal data: If at first you do not succeed-try, try again. Anesth. Analg. 2018, 127, 569–575. [Google Scholar] [CrossRef]
- Ma, Y.; Mazumdar, M.; Memtsoudis, S.G. Beyond repeated-measures analysis of variance: Advanced statistical methods for the analysis of longitudinal data in anesthesia research. Reg. Anesth. Pain Med. 2012, 37, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, A.; Yahiaoui-Doktor, M.; Meissner, W.; Zahn, P.K.; Pogatzki-Zahn, E.M. Predicting poor postoperative acute pain outcome in adults: An international, multicentre database analysis of risk factors in 50,005 patients. PAIN Rep. 2020, 5, e831. [Google Scholar] [CrossRef]
- Connor, C.W. Artificial Intelligence and Machine Learning in Anesthesiology. Anesthesiology 2019, 131, 1346–1359. [Google Scholar] [CrossRef]
- Sassenscheidt, J.; Jungwirth, B.; Kubitz, J.C. Machine learning in anesthesiology. Anaesthesist 2020, 69, 535–543. [Google Scholar] [CrossRef]
- Zaslansky, R.; Rothaug, J.; Chapman, C.R.; Bäckström, R.; Brill, S.; Fletcher, D.; Fodor, L.; Gordon, D.B.; Komann, M.; Konrad, C.; et al. PAIN OUT: The making of an international acute pain registry. Eur. J. Pain 2015, 19, 490–502. [Google Scholar] [CrossRef]
- Improvement in Postoperative PAIN OUTcome (PAIN OUT). Available online: http://pain-out.med.uni-jena.de (accessed on 4 January 2021).
- Meißner, W. Qualität der Schmerztherapie in Deutschland—Qualitätsmanagement und -sicherung in der Akutschmerztherapie. AINS—Anästhesiol. Intensivmed. Notfallmed. Schmerzther. 2016, 51, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Quality Improvement in Postoperative Pain Management (QUIPS). Available online: http://www.quips-projekt.de/en (accessed on 16 January 2021).
- Network for Safety in Regional Anesthesia and Acute Pain Medicine (net-ra). Available online: https://net-ra.eu (accessed on 16 January 2021).
- Volk, T.; Engelhardt, L.; Spies, C.; Steinfeldt, T.; Kutter, B.; Heller, A.; Werner, C.; Heid, F.; Bürkle, H.; Koch, T.; et al. Das Netzwerk Regionalanästhesie des wissenschaftlichen Arbeitskreises Regionalanästhesie der DGAI und des BDA. AINS—Anästhesiol. Intensivmed. Notfallmed. Schmerzther. 2009, 44, 778–780. [Google Scholar] [CrossRef] [PubMed]
- Premier Incorporated. Premier Healthcare Database White Paper: Data that Informs and Performs. 2020. Available online: https://www.premierinc.com/newsroom/education/premier-healthcare-database-whitepaper (accessed on 22 February 2021).
- Premier Incorporated. Premier Healthcare Database. Available online: https://www.premierinc.com (accessed on 22 February 2021).
- IBM MarketScan Research Databases. Available online: https://www.ibm.com/products/marketscan-research-databases (accessed on 22 February 2021).
- IBM Watson Health. IBM MarketScan Research Databases for Life Sciences Researchers (White Paper). 2019. Available online: https://www.ibm.com/downloads/cas/0NKLE57Y (accessed on 3 February 2021).
- Neuman, M.D. The Importance of Validation Studies in Perioperative Database Research. Anesthesiology 2015, 123, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Fast Healthcare Interoperability Resources (FHIR). Available online: http://hl7.org/fhir/index.html (accessed on 22 January 2021).
- Sass, J.; Bartschke, A.; Lehne, M.; Essenwanger, A.; Rinaldi, E.; Rudolph, S.; Heitmann, K.U.; Vehreschild, J.J.; von Kalle, C.; Thun, S. The German Corona Consensus Dataset (GECCO): A standardized dataset for COVID-19 research in university medicine and beyond. BMC Med. Inform. Decis. Mak. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). Available online: https://icd.who.int/browse11/l-m/en (accessed on 21 January 2021).
- SNOMED CT. Available online: https://www.snomed.org (accessed on 4 January 2021).
- Thun, S.; Dewenter, H. ICD-11, ICHI and SNOMED CT—What do the standards mean for eHealth applications? Bundesgesundheitsblatt Gesundheitsforsch Gesundheitsschutz 2018, 61, 812–820. [Google Scholar] [CrossRef]
- Gan, T.J. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J. Pain Res. 2017, 10, 2287–2298. [Google Scholar] [CrossRef]
- Glare, P.; Aubrey, K.R.; Myles, P.S. Transition from acute to chronic pain after surgery. Lancet 2019, 393, 1537–1546. [Google Scholar] [CrossRef]
- Van Boekel, R.L.M.; Warlé, M.C.; Nielen, R.G.C.; Vissers, K.C.P.; Van Der Sande, R.; Bronkhorst, E.M.; Lerou, J.G.C.; Steegers, M.A.H. Relationship between Postoperative Pain and Overall 30-Day Complications in a Broad Surgical Population: An Observational Study. Ann. Surg. 2019, 269, 856–865. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, D.; Stamer, U.M.; Pogatzki-Zahn, E.; Zaslansky, R.; Tanase, N.V.; Perruchoud, C.; Kranke, P.; Komann, M.; Lehman, T.; Meisner, W. Chronic postsurgical pain in Europe: An observational study. Eur. J. Anaesthesiol. 2015, 32, 725–734. [Google Scholar] [CrossRef]
- Weinstein, E.J.; Levene, J.L.; Cohen, M.S.; Andreae, D.A.; Chao, J.Y.; Johnson, M.; Hall, C.B.; Andreae, M.H. Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst. Rev. 2018, 6, CD007105. [Google Scholar] [CrossRef]
- Memtsoudis, S.G.; Sun, X.; Chiu, Y.L.; Stundner, O.; Liu, S.S.; Banerjee, S.; Mazumdar, M.; Sharrock, N.E. Perioperative comparative effectiveness of anesthetic technique in orthopedic patients. Anesthesiology 2013, 118, 1046–1058. [Google Scholar] [CrossRef]
- Rothaug, J.; Zaslansky, R.; Schwenkglenks, M.; Komann, M.; Allvin, R.; Backström, R.; Brill, S.; Buchholz, I.; Engel, C.; Fletcher, D.; et al. Patients’ Perception of Postoperative Pain Management: Validation of the International Pain Outcomes (IPO) Questionnaire. J. Pain 2013, 14, 1361–1370. [Google Scholar] [CrossRef]
- Gerbershagen, H.J.; Aduckathil, S.; van Wijck, A.J.M.; Peelen, L.M.; Kalkman, C.J.; Meissner, W. Pain Intensity on the First Day after Surgery. Anesthesiology 2013, 118, 934–944. [Google Scholar] [CrossRef] [PubMed]
- Roeb, M.M.; Wolf, A.; Gräber, S.S.; Meißner, W.; Volk, T. Epidural Against Systemic Analgesia: An International Registry Analysis on Postoperative Pain and Related Perceptions after Abdominal Surgery. Clin. J. Pain 2017, 33, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Donauer, K.; Bomberg, H.; Wagenpfeil, S.; Volk, T.; Meissner, W.; Wolf, A. Regional vs General Anesthesia for Total Knee and Hip Replacement: An Analysis of Postoperative Pain Perception from the International PAIN OUT Registry. Pain Pract. 2018, 18, 1036–1047. [Google Scholar] [CrossRef]
- Greimel, F.; Maderbacher, G.; Baier, C.; Keshmiri, A.; Schwarz, T.; Zeman, F.; Meissner, W.; Grifka, J.; Benditz, A. Multicenter cohort-study of 15,326 cases analyzing patient satisfaction and perioperative pain management: General, regional and combination anesthesia in knee arthroplasty. Sci. Rep. 2018, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Volk, T.; Wolf, A.; Van Aken, H.; Bürkle, H.; Wiebalck, A.; Steinfeldt, T. Incidence of spinal haematoma after epidural puncture: Analysis from the German network for safety in regional anaesthesia. Eur. J. Anaesthesiol. 2012, 29, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Volk, T.; Engelhardt, L.; Spies, C.; Steinfeldt, T.; Gruenewald, D.; Kutter, B.; Heller, A.; Werner, C.; Heid, F.; Bürkle, H.; et al. Incidence of infection from catheter procedures for regional anesthesia: First results from the network of DGAI and BDA. Anaesthesist 2009, 58, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, H.; Kubulus, C.; List, F.; Albert, N.; Schmitt, K.; Gräber, S.; Kessler, P.; Steinfeldt, T.; Standl, T.; Gottschalk, A.; et al. Diabetes A Risk Factor for Catheter-Associated Infections. Reg. Anesth. Pain Med. 2015, 40, 16–21. [Google Scholar] [CrossRef]
- Bomberg, H.; Albert, N.; Schmitt, K.; Gräber, S.; Kessler, P.; Steinfeldt, T.; Hering, W.; Gottschalk, A.; Standl, T.; Stork, J.; et al. Obesity in regional anesthesia—a risk factor for peripheral catheter-related infections. Acta Anaesthesiol. Scand. 2015, 59, 1038–1048. [Google Scholar] [CrossRef]
- Bomberg, H.; Bayer, I.; Wagenpfeil, S.; Kessler, P.; Wulf, H.; Standl, T.; Gottschalk, A.; Döffert, J.; Hering, W.; Birnbaum, J.; et al. Prolonged Catheter Use and Infection in Regional Anesthesia: A Retrospective Registry Analysis. Anesthesiology 2018, 128, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, H.; Kubulus, C.; Herberger, S.; Wagenpfeil, S.; Kessler, P.; Steinfeldt, T.; Standl, T.; Gottschalk, A.; Stork, J.; Meissner, W.; et al. Tunnelling of thoracic epidural catheters is associated with fewer catheter-related infections: A retrospective registry analysis. Br. J. Anaesth. 2016, 116, 546–553. [Google Scholar] [CrossRef]
- Bomberg, H.; Krotten, D.; Kubulus, C.; Wagenpfeil, S.; Kessler, P.; Steinfeldt, T.; Standl, T.; Gottschalk, A.; Stork, J.; Meissner, W.; et al. Single-dose Antibiotic Prophylaxis in Regional Anesthesia. Anesthesiology 2016, 125, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, H.; Wetjen, L.; Wagenpfeil, S.; Schöpe, J.; Kessler, P.; Wulf, H.; Wiesmann, T.; Standl, T.; Gottschalk, A.; Döffert, J.; et al. Risks and benefits of ultrasound, nerve stimulation, and their combination for guiding peripheral nerve blocks: A retrospective registry analysis. Anesth. Analg. 2018, 127, 1035–1043. [Google Scholar] [CrossRef]
- Walker, B.J.; Long, J.B.; Sathyamoorthy, M.; Birstler, J.; Wolf, C.; Bosenberg, A.T.; Flack, S.H.; Krane, E.J.; Sethna, N.F.; Suresh, S.; et al. Complications in Pediatric Regional Anesthesia: An Analysis of More than 100,000 Blocks from the Pediatric Regional Anesthesia Network. Anesthesiology 2018, 129, 721–732. [Google Scholar] [CrossRef]
- Long, J.B.; Birmingham, P.K.; De Oliveira, G.S.; Schaldenbrand, K.M.; Suresh, S. Transversus Abdominis plane block in children: A multicenter safety analysis of 1994 cases from the PRAN (Pediatric Regional Anesthesia Network) database. Anesth. Analg. 2014, 119, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.J.; Long, J.B.; De Oliveira, G.S.; Szmuk, P.; Setiawan, C.; Polaner, D.M.; Suresh, S. Peripheral nerve catheters in children: An analysis of safety and practice patterns from the pediatric regional anesthesia network (PRAN). Br. J. Anaesth. 2015, 115, 457–462. [Google Scholar] [CrossRef]
- Taenzer, A.H.; Hoyt, M.; Krane, E.J.; Walker, B.J.; Flack, S.; Bosenberg, A.; Sethna, N.F.; Franklin, A.D.; Polaner, D.M. Variation between and within Hospitals in Single Injection Caudal Local Anesthetic Dose: A Report from the Pediatric Regional Anesthesia Network. Anesth. Analg. 2020, 130, 1693–1701. [Google Scholar] [CrossRef] [PubMed]
- Barrington, M.J.; Watts, S.A.; Gledhill, S.R.; Thomas, R.D.; Said, S.A.; Snyder, G.L.; Tay, V.S.; Jamrozik, K. Preliminary Results of the Australasian Regional Anaesthesia Collaboration. Reg. Anesth. Pain Med. 2009, 34, 534–541. [Google Scholar] [CrossRef]
- Ironfield, C.M.; Barrington, M.J.; Kluger, R.; Sites, B. Are patients satisfied after peripheral nerve blockade? Results from an international registry of regional anesthesia. Reg. Anesth. Pain Med. 2014, 39, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Sites, B.; Barrington, M.; Davis, M. Using an international clinical registry of regional anesthesia to identify targets for quality improvement. Reg. Anesth. Pain Med. 2014, 39, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Taenzer, A.H.; Sites, B.D.; Kluger, R.; Barrington, M. Settled science or unwarranted variation in local anesthetic dosing? An analysis from an International Registry of Regional Anesthesiology. Reg. Anesth. Pain Med. 2019, 44, 998–1002. [Google Scholar] [CrossRef]
- Liau, A.; Havidich, J.E.; Onega, T.; Dutton, R.P. The national anesthesia clinical outcomes registry. Anesth. Analg. 2015, 121, 1604–1610. [Google Scholar] [CrossRef]
- Lam, S.; Qu, H.; Hannum, M.; Tan, K.S.; Afonso, A.; Tokita, H.K.; McCormick, P.J. Trends in Peripheral Nerve Block Usage in Mastectomy and Lumpectomy: Analysis of a National Database From 2010 to 2018. Anesth. Analg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Fleischut, P.M.; Eskreis-Winkler, J.M.; Gaber-Baylis, L.K.; Giambrone, G.P.; Faggiani, S.L.; Dutton, R.P.; Memtsoudis, S.G. Variability in Anesthetic Care for Total Knee Arthroplasty: An Analysis From the Anesthesia Quality Institute. Am. J. Med. Qual. 2015, 30, 172–179. [Google Scholar] [CrossRef]
- Kheterpal, S. Clinical Research Using an Information System: The Multicenter Perioperative Outcomes Group. Anesthesiol. Clin. 2011, 29, 377–388. [Google Scholar] [CrossRef]
- Bateman, B.T.; Mhyre, J.M.; Ehrenfeld, J.; Kheterpal, S.; Abbey, K.R.; Argalious, M.; Berman, M.F.; Jacques, P.S.; Levy, W.; Loeb, R.G.; et al. The risk and outcomes of epidural hematomas after perioperative and obstetric epidural catheterization: A report from the multicenter perioperative outcomes group research consortium. Anesth. Analg. 2013, 116, 1380–1385. [Google Scholar] [CrossRef]
- Lee, L.O.; Bateman, B.T.; Kheterpal, S.; Klumpner, T.T.; Housey, M.; Aziz, M.F.; Hand, K.W.; MacEachern, M.; Goodier, C.G.; Bernstein, J.; et al. Risk of epidural hematoma after neuraxial techniques in thrombocytopenic parturients a report from the multicenter perioperative outcomes group. Anesthesiology 2017, 126, 1053–1064. [Google Scholar] [CrossRef] [PubMed]
- Stuart, A.R.; Kuck, K.; Naik, B.I.; Saager, L.; Pace, N.L.; Domino, K.B.; Posner, K.L.; Alpert, S.B.; Kheterpal, S.; Sinha, A.K.; et al. Multicenter Perioperative Outcomes Group Enhanced Observation Study Postoperative Pain Profiles, Analgesic Use, and Transition to Chronic Pain and Excessive and Prolonged Opioid Use Patterns Methodology. Anesth. Analg. 2020, 130, 1702–1708. [Google Scholar] [CrossRef] [PubMed]
- Fink, A.S.; Campbell, D.A.; Mentzer, R.M.; Henderson, W.G.; Daley, J.; Bannister, J.; Hur, K.; Khuri, S.F. The National Surgical Quality Improvement Program in non-veterans administration hospitals: Initial demonstration of feasibility. Ann. Surg. 2002, 236, 344–354. [Google Scholar] [CrossRef] [PubMed]
- Saied, N.N.; Helwani, M.A.; Weavind, L.M.; Shi, Y.; Shotwell, M.S.; Pandharipande, P.P. Effect of anaesthesia type on postoperative mortality and morbidities: A matched analysis of the NSQIP database. Br. J. Anaesth. 2017, 118, 105–111. [Google Scholar] [CrossRef]
- Turan, A.; Bajracharya, G.R.; Leung, S.; Yazici Kara, M.; Mao, G.; Botsford, T.; Ruetzler, K.; Maheshwari, K.; Ali Sakr Esa, W.; Elsharkawy, H.; et al. Association of neuraxial anesthesia with postoperative venous thromboembolism after noncardiac surgery: A propensity-matched analysis of acs-nsqip database. Anesth. Analg. 2019, 128, 494–501. [Google Scholar] [CrossRef]
- Brovman, E.Y.; Wallace, F.C.; Weaver, M.J.; Beutler, S.S.; Urman, R.D. Anesthesia Type Is Not Associated With Postoperative Complications in the Care of Patients With Lower Extremity Traumatic Fractures. Anesth. Analg. 2019, 129, 1034–1042. [Google Scholar] [CrossRef]
- Basques, B.A.; Bohl, D.D.; Golinvaux, N.S.; Samuel, A.M.; Grauer, J.G. General versus spinal anaesthesia for patients aged 70 years and older with a fracture of the hip. Bone Jt. J. 2015, 97, 689–695. [Google Scholar] [CrossRef]
- Helwani, M.A.; Avidan, M.S.; Ben Abdallah, A.; Kaiser, D.J.; Clohisy, J.C.; Hall, B.L.; Kaiser, H.A. Effects of Regional Versus General Anesthesia on Outcomes After Total Hip Arthroplasty. J. Bone Jt. Surg. 2015, 97, 186–193. [Google Scholar] [CrossRef]
- Cummings, K.C., III; Zimmerman, N.M.; Maheshwari, K.; Cooper, G.S.; Cummings, L.C. Epidural compared with non-epidural analgesia and cardiopulmonary complications after colectomy: A retrospective cohort study of 20,880 patients using a national quality database. J. Clin. Anesth. 2018, 47, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Malik, O.S.; Brovman, E.Y.; Urman, R.D. The Use of Regional or Local Anesthesia for Carotid Endarterectomies May Reduce Blood Loss and Pulmonary Complications. J. Cardiothorac. Vasc. Anesth. 2019, 33, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Leichtle, S.W.; Mouawad, N.J.; Welch, K.; Lampman, R.; Whitehouse, W.M.; Heidenreich, M. Outcomes of carotid endarterectomy under general and regional anesthesia from the American College of Surgeons’ National Surgical Quality Improvement Program. J. Vasc. Surg. 2012, 56, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Sidawy, A.N.; Dezee, K.; Neville, R.F.; Weiswasser, J.; Arora, S.; Aidinian, G.; Abularrage, C.; Adams, E.; Khuri, S.; et al. The effects of the type of anesthesia on outcomes of lower extremity infrainguinal bypass. J. Vasc. Surg. 2006, 44, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.L.; Hurley, R.W.; Anderson, G.F.; Herbert, R.; Rowlingson, A.J.; Fleisher, L.A. Effect of postoperative epidural analgesia on morbidity and mortality following surgery in medicare patients. Reg. Anesth. Pain Med. 2004, 29, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.L.; Rowlingson, A.J.; Herbert, R.; Richman, J.M.; Andrews, R.A.F.; Fleisher, L.A. Correlation of postoperative epidural analgesia on morbidity and mortality after colectomy in Medicare patients. J. Clin. Anesth. 2006, 18, 594–599. [Google Scholar] [CrossRef]
- Cummings, K.C.; Kou, T.D.; Chak, A.; Schluchter, M.D.; Margevicius, S.; Cooper, G.S.; Meropol, N.J.; Perry, Y.; Linden, P.A.; Cummings, L.C. Surgical approach and the impact of epidural analgesia on survival after esophagectomy for cancer: A population-based retrospective cohort study. PLoS ONE 2019, 14, 1–18. [Google Scholar] [CrossRef]
- Wu, C.L.; Sapirstein, A.; Herbert, R.; Rowlingson, A.J.; Michaels, R.K.; Petrovic, M.A.; Fleisher, L.A. Effect of postoperative epidural analgesia on morbidity and mortality after lung resection in Medicare patients. J. Clin. Anesth. 2006, 18, 515–520. [Google Scholar] [CrossRef]
- Wu, C.L.; Anderson, G.F.; Herbert, R.; Lietman, S.A.; Fleisher, L.A. Effect of postoperative epidural analgesia on morbidity and mortality after total hip replacement surgery in medicare patients. Reg. Anesth. Pain Med. 2003, 28, 271–278. [Google Scholar] [CrossRef]
- Oderda, G.M.; Senagore, A.J.; Morland, K.; Iqbal, S.U.; Kugel, M.; Liu, S.; Habib, A.S. Opioid-related respiratory and gastrointestinal adverse events in patients with acute postoperative pain: Prevalence, predictors, and burden. J. Pain Palliat. Care Pharmacother. 2019, 33, 82–97. [Google Scholar] [CrossRef]
- Cozowicz, C.; Poeran, J.; Zubizarreta, N.; Liu, J.; Weinstein, S.M.; Pichler, L.; Mazumdar, M.; Memtsoudis, S.G. Non-opioid analgesic modes of pain management are associated with reduced postoperative complications and resource utilisation: A retrospective study of obstructive sleep apnoea patients undergoing elective joint arthroplasty. Br. J. Anaesth. 2019, 122, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Memtsoudis, S.G.; Poeran, J.; Zubizarreta, N.; Cozowicz, C.; Mörwald, E.E.; Mariano, E.R.; Mazumdar, M. Association of Multimodal Pain Management Strategies with Perioperative Outcomes and Resource Utilization: A Population-based Study. Anesthesiology 2018, 128, 891–902. [Google Scholar] [CrossRef] [PubMed]
- Cozowicz, C.; Bekeris, J.; Poeran, J.; Zubizarreta, N.; Schwenk, E.; Girardi, F.; Memtsoudis, S.G. Multimodal Pain Management and Postoperative Outcomes in Lumbar Spine Fusion Surgery: A Population-based Cohort Study. Spine 2020, 45, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Bekeris, J.; Fiasconaro, M.; Della Valle, A.G.; Liu, J.; Shanaghan, K.A.; Poeran, J.; Wilson, L.A.; Memtsoudis, S.G. Modifiable Analgesia-/Anesthesia-Related Factors and Risk of Severe Gastrointestinal Complications After Lower Extremity Total Joint Arthroplasty: A Nationwide Analysis. J. Arthroplasty 2020, 35, 2624–2630. [Google Scholar] [CrossRef] [PubMed]
- Haines, K.L.; Fuller, M.; Vaughan, J.G.; Krishnamoorthy, V.; Raghunathan, K.; Kasotakis, G.; Agarwal, S.; Ohnuma, T. The Impact of Nonsteroidal Anti-inflammatory Drugs on Older Adult Trauma Patients With Hip Fractures. J. Surg. Res. 2020, 255, 583–593. [Google Scholar] [CrossRef]
- Stundner, O.; Poeran, J.; Ladenhauf, H.N.; Berger, M.M.; Levy, S.B.; Zubizarreta, N.; Mazumdar, M.; Bekeris, J.; Liu, J.; Galatz, L.M.; et al. Effectiveness of intravenous acetaminophen for postoperative pain management in hip and knee arthroplasties: A population-based study. Reg. Anesth. Pain Med. 2019, 44, 565–572. [Google Scholar] [CrossRef]
- Memtsoudis, S.G.; Rasul, R.; Suzuki, S.; Poeran, J.; Danninger, T.; Wu, C.; Mazumdar, M.; Vougioukas, V. Does the Impact of the Type of Anesthesia on Outcomes Differ by Patient Age and Comorbidity Burden? Reg. Anesth. Pain Med. 2014, 39, 112–119. [Google Scholar] [CrossRef]
- Sun, E.C.; Darnall, B.D.; Baker, L.C.; MacKey, S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern. Med. 2016, 176, 1286–1293. [Google Scholar] [CrossRef]
- Brummett, C.M.; England, C.; Evans-shields, J.; Zimmerman, N.M.; Pawasauskas, J.; Oderda, G. Health Care Burden Associated with Outpatient. J. Manag Care Spec. Pharm. 2019, 25, 973–983. [Google Scholar] [PubMed]
- Tighe, P.J.; Harle, C.A.; Hurley, R.W.; Aytug, H.; Boezaart, A.P.; Fillingim, R.B. Teaching a Machine to Feel Postoperative Pain: Combining High-Dimensional Clinical Data with Machine Learning Algorithms to Forecast Acute Postoperative Pain. Pain Med. 2015, 16, 1386–1401. [Google Scholar] [CrossRef] [PubMed]
- Lötsch, J.; Sipilä, R.; Tasmuth, T.; Kringel, D.; Estlander, A.M.; Meretoja, T.; Kalso, E.; Ultsch, A. Machine-learning-derived classifier predicts absence of persistent pain after breast cancer surgery with high accuracy. Breast Cancer Res. Treat. 2018, 171, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.A.; Velagapudi, M.A.; Lang, J.A.; Behara, L.; Venigandla, R.; Velagapudi, N.; Fong, C.T.; Horibe, M.; Lang, J.D.; Nair, B.G. Machine learning approach to predict postoperative opioid requirements in ambulatory surgery patients. PLoS ONE 2020, 15, e0236833. [Google Scholar] [CrossRef] [PubMed]
- Tighe, P.; Laduzenski, S.; Edwards, D.; Ellis, N.; Boezaart, A.P.; Aygtug, H. Use of Machine Learning Theory to Predict the Need for Femoral Nerve Block Following ACL Repair. Pain Med. 2011, 12, 1566–1575. [Google Scholar] [CrossRef] [PubMed]
- Churpek, M.M.; Yuen, T.C.; Winslow, C.; Meltzer, D.O.; Kattan, M.W.; Edelson, D.P. Multicenter Comparison of Machine Learning Methods and Conventional Regression for Predicting Clinical Deterioration on the Wards. Crit. Care Med. 2016, 44, 368–374. [Google Scholar] [CrossRef]
- Rojas, J.C.; Carey, K.A.; Edelson, D.P.; Venable, L.R.; Howell, M.D.; Churpek, M.M. Predicting intensive care unit readmission with machine learning using electronic health record data. Ann. Am. Thorac. Soc. 2018, 15, 846–853. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, S.; Cho, J.; Kim, Y.S.; Sol, I.S.; Sung, Y.; Cho, I.; Park, M.; Jang, H.; Kim, Y.H.; et al. A deep learning model for real-time mortality prediction in critically ill children. Crit. Care 2019, 23, 1–10. [Google Scholar] [CrossRef]
- Nemati, S.; Holder, A.; Razmi, F.; Stanley, M.D.; Clifford, G.D.; Buchman, T.G. An Interpretable Machine Learning Model for Accurate Prediction of Sepsis in the ICU. Crit. Care Med. 2018, 46, 547–553. [Google Scholar] [CrossRef]
- Schmidt, C.M.D. Anderson Breaks With IBM Watson, Raising Questions About Artificial Intelligence in Oncology. J. Natl. Cancer Inst. 2017, 109, 315–322. [Google Scholar] [CrossRef]
- IEEE Spectrum How IBM Watson Overpromised and Underdelivered on AI Health Care. Available online: https://spectrum.ieee.org/biomedical/diagnostics/how-ibm-watson-overpromised-and-underdelivered-on-ai-health-care (accessed on 11 March 2021).
- Neuman, M.D.; Ellenberg, S.S.; Sieber, F.E.; Magaziner, J.S.; Feng, R.; Carson, J.L. Regional versus General Anesthesia for Promoting Independence after Hip Fracture (REGAIN): Protocol for a pragmatic, international multicentre trial. BMJ Open 2016, 6, e013473. [Google Scholar] [CrossRef] [PubMed]
- Kowark, A.; Adam, C.; Ahrens, J.; Bajbouj, M.; Bollheimer, C.; Borowski, M.; Dodel, R.; Dolch, M.; Hachenberg, T.; Henzler, D.; et al. Improve hip fracture outcome in the elderly patient (iHOPE): A study protocol for a pragmatic, multicentre randomised controlled trial to test the efficacy of spinal versus general anaesthesia. BMJ Open 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
| Short Title | Title | Est. | Webpage |
|---|---|---|---|
| Acute postoperative pain on the first postoperative day | |||
| PAIN OUT | Improvement in Postoperative Pain Outcome | 2009 | pain-out.med.uni-jena.de |
| QUIPS | Quality Improvement in Postoperative Pain Management | 2005 | quips-projekt.de |
| Regional anesthesia and acute postoperative pain | |||
| net-ra | German Network for Safety in Regional Anesthesia and Acute Pain Medicine | 2007 | net-ra.eu |
| Regional anesthesia | |||
| PRAN | Pediatric Regional Anesthesia Network | 2007 | pedsanesthesia.org |
| IRORA | International Registry of Regional Anesthesia | 2006 | regionalanaesthesia.wordpress.com |
| Administrative databases | |||
| Medicare | Medicare and Medicaid healthcare claims database | 1999 | medicare.gov resdac.org |
| Premier | Premier healthcare database | 1997 | premierinc.com |
| MarketScan | IBM MarketScan research database (previously: Truven Health MarketScan Database) | 1989 | ibm.com/products/marketscan-research-databases |
| Anesthesiology and Perioperative Medicine | |||
| NACOR | National Anesthesia Clinical Outcomes Registry | 2008 | aqihq.org |
| MPOG | Multicenter Perioperative Outcomes Group | 2008 | mpog.org |
| NSQIP | American College of Surgeons National Surgical Quality Improvement Program | 1991 | facs.org |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller-Wirtz, L.M.; Volk, T. Big Data in Studying Acute Pain and Regional Anesthesia. J. Clin. Med. 2021, 10, 1425. https://doi.org/10.3390/jcm10071425
Müller-Wirtz LM, Volk T. Big Data in Studying Acute Pain and Regional Anesthesia. Journal of Clinical Medicine. 2021; 10(7):1425. https://doi.org/10.3390/jcm10071425
Chicago/Turabian StyleMüller-Wirtz, Lukas M., and Thomas Volk. 2021. "Big Data in Studying Acute Pain and Regional Anesthesia" Journal of Clinical Medicine 10, no. 7: 1425. https://doi.org/10.3390/jcm10071425
APA StyleMüller-Wirtz, L. M., & Volk, T. (2021). Big Data in Studying Acute Pain and Regional Anesthesia. Journal of Clinical Medicine, 10(7), 1425. https://doi.org/10.3390/jcm10071425







