Abductor Muscle Force after Straight-Stem Compared to Short-Stem Total Hip Arthroplasty through a Modified Direct Lateral Approach: Functional Assessment of 70 Consecutive Patients of a Randomized Controlled Clinical Trial
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Patients and Demographics
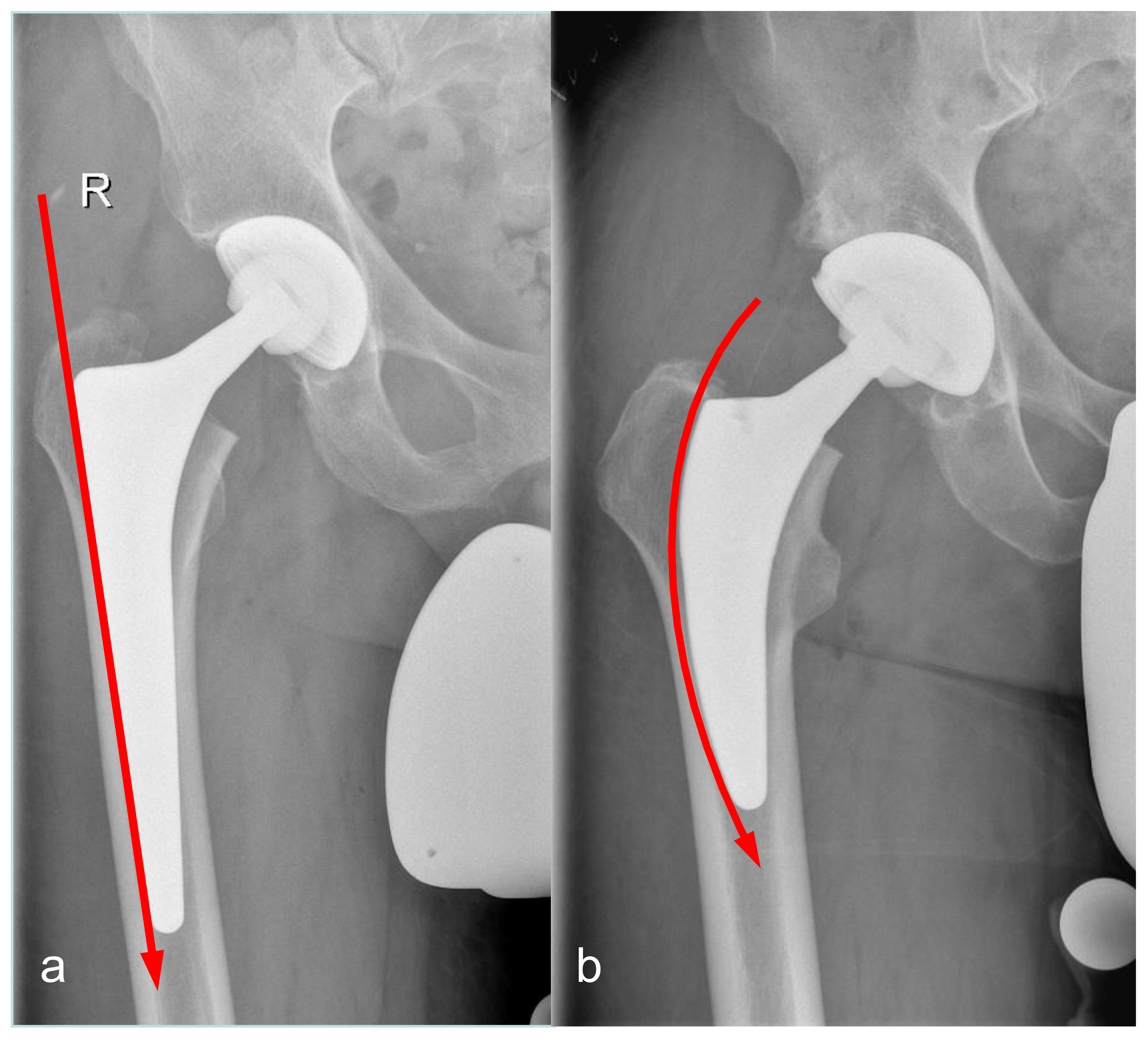
2.3. Surgeries and Implant Characteristics
2.4. Patient-Reported Outcome Measures (PROM)
2.5. Functional Assessment
2.6. Radiographic Evaluation
2.7. Statistics
3. Results
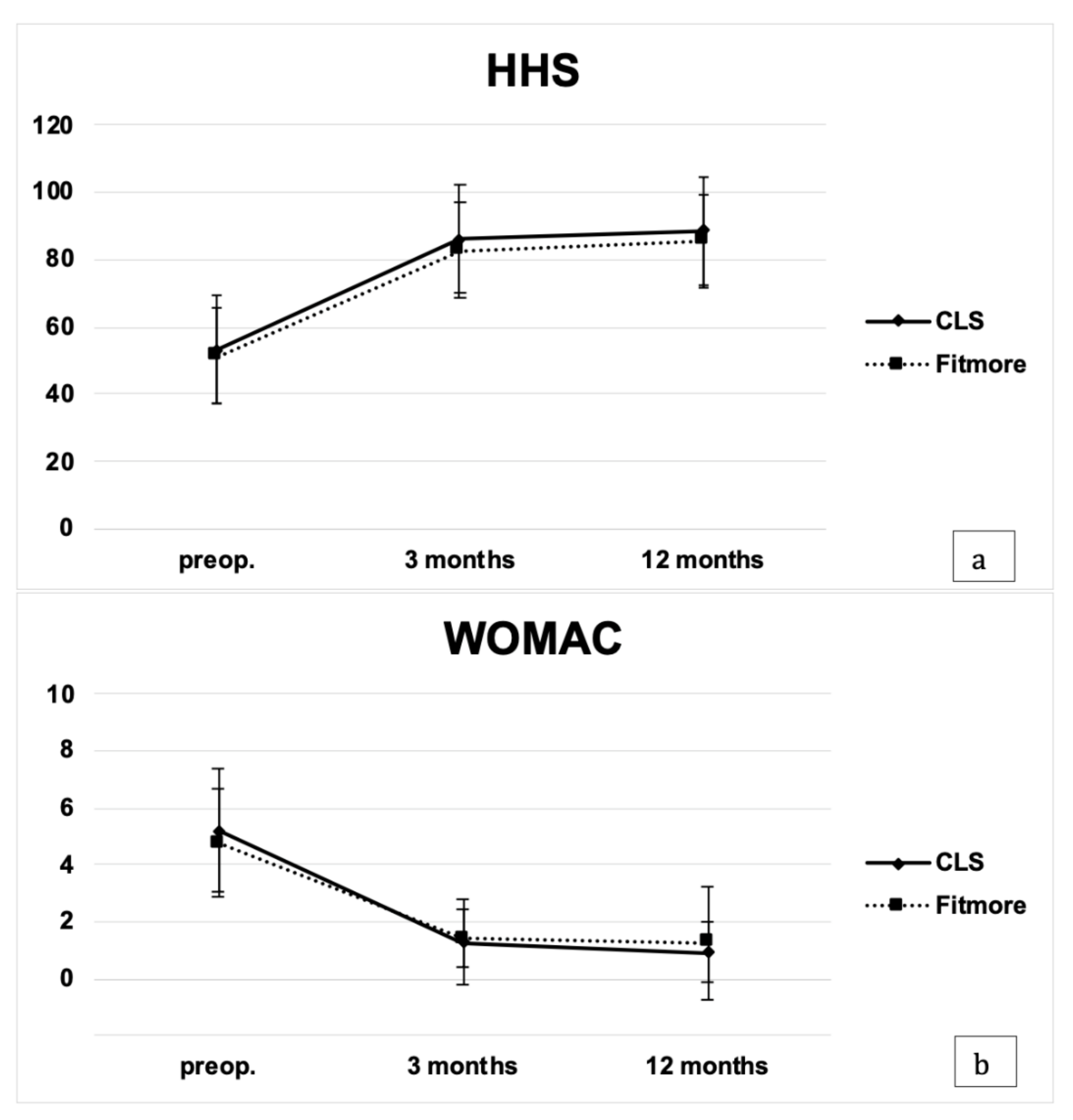
3.1. Patient-Reported Outcome Measures
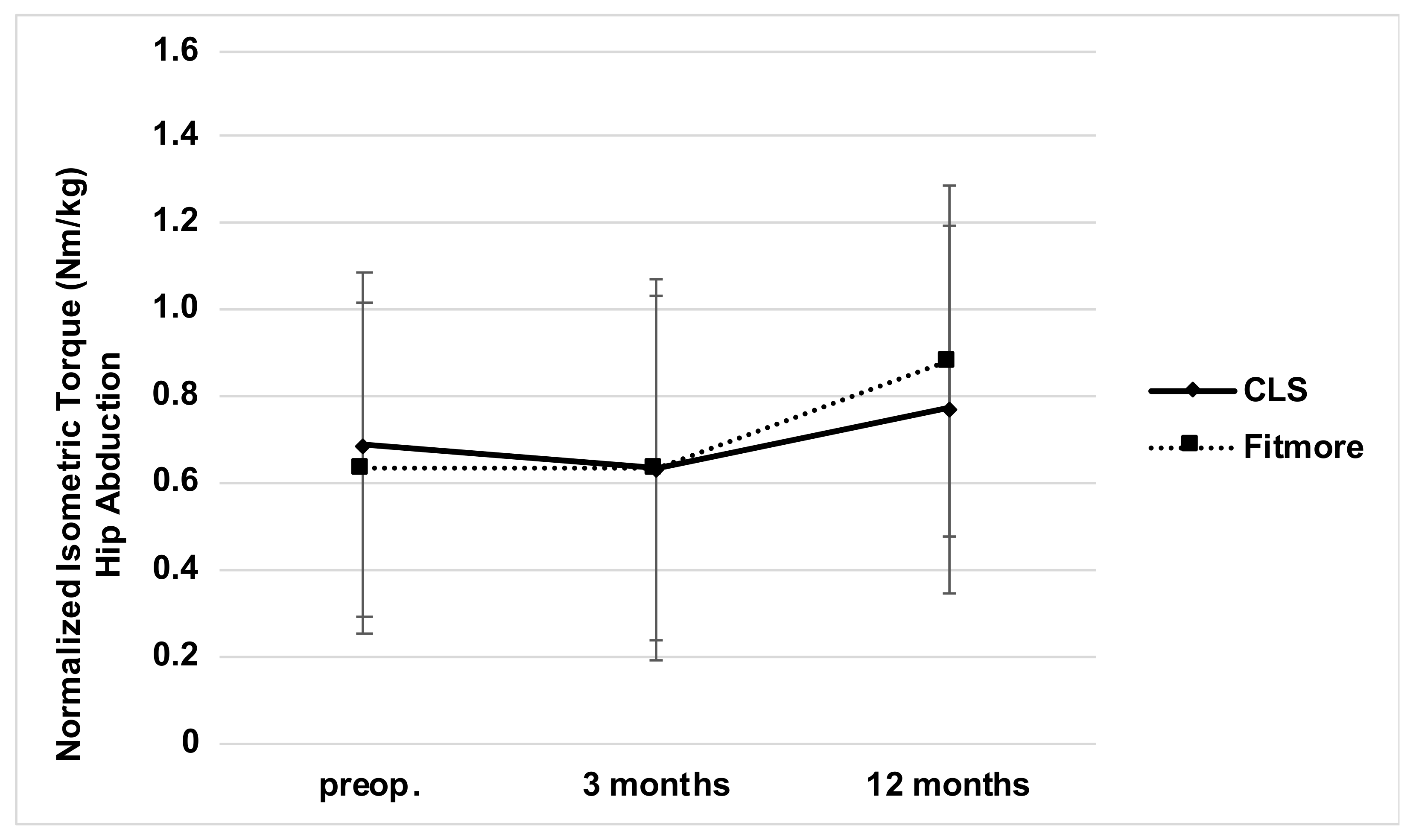
3.2. Functional Assessment
3.3. Radiographic Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muller, M.; Tohtz, S.; Winkler, T.; Dewey, M.; Springer, I.; Perka, C. MRI findings of gluteus minimus muscle damage in primary total hip arthroplasty and the influence on clinical outcome. Arch. Orthop. Trauma Surg. 2010, 130, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Odak, S.; Ivory, J. Management of abductor mechanism deficiency following total hip replacement. Bone Jt. J. 2013, 95, 343–347. [Google Scholar] [CrossRef]
- Gustke, K. Short stems for total hip arthroplasty. J. Bone Jt. Surgery. Br. 2012, 94-B, 47–51. [Google Scholar] [CrossRef]
- Schmidutz, F.; Beirer, M.; Weber, P.; Mazoochian, F.; Fottner, A.; Jansson, V. Biomechanical reconstruction of the hip: Comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int. Orthop. 2012, 36, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Kiyama, T.; Naito, M.; Shinoda, T.; Maeyama, A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J. Arthroplast. 2010, 25, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Hube, R.; Zaage, M.; Hein, W.; Reichel, H. [Early functional results with the Mayo-hip, a short stem system with metaphyseal-intertrochanteric fixation]. Orthopade 2004, 33, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- McCalden, R.W.; Korczak, A.; Somerville, L.; Yuan, X.; Naudie, D.D. A randomised trial comparing a short and a standard-length metaphyseal engaging cementless femoral stem using radiostereometric analysis. Bone Jt. J. 2015, 97-B, 595–602. [Google Scholar] [CrossRef]
- Muller, M.; Tohtz, S.; Springer, I.; Dewey, M.; Perka, C. Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: Minimally invasive anterolateral versus modified direct lateral approach. Arch. Orthop. Trauma Surg. 2011, 131, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Repantis, T.; Bouras, T.; Korovessis, P. Comparison of minimally invasive approach versus conventional anterolateral approach for total hip arthroplasty: A randomized controlled trial. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 111–116. [Google Scholar] [CrossRef]
- Mulliken, B.D.; Rorabeck, C.H.; Bourne, R.B.; Nayak, N. A modified direct lateral approach in total hip arthroplasty A comprehensive review. J. Arthroplast. 1998, 13, 737–747. [Google Scholar] [CrossRef]
- Kamada, S.; Naito, M.; Nakamura, Y.; Kiyama, T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch. Orthop. Trauma Surg. 2011, 131, 1723–1729. [Google Scholar] [CrossRef] [PubMed]
- Maffiuletti, N.A. Assessment of hip and knee muscle function in orthopaedic practice and research. J. Bone Jt. Surg. Am. 2010, 92, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Judd, D.L.; Dennis, D.A.; Thomas, A.C.; Wolfe, P.; Dayton, M.R.; Stevens-Lapsley, J.E. Muscle strength and functional recovery during the first year after THA. Clin. Orthop. Relat. Res. 2014, 472, 654–664. [Google Scholar] [CrossRef]
- Patel, S.; Thakrar, R.R.; Bhamra, J.; Hossain, F.; Tengrootenhuysen, M.; Haddad, F.S. Are leg length and hip offset comparable after hip resurfacing and cementless total hip arthroplasty? Ann. R. Coll. Surg. Engl. 2014, 93, 465–469. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Molli, R.G.; Lombardi, A.V., Jr.; Berend, K.R.; Adams, J.B.; Sneller, M.A. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin. Orthop. Relat. Res. 2012, 470, 450–461. [Google Scholar] [CrossRef]
- McGrory, B.J.; Morrey, B.F.; Cahalan, T.D.; An, K.N.; Cabanela, M.E. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J. Bone Jt. Surg. Br. 1995, 77, 865–869. [Google Scholar] [CrossRef]
- Bjordal, F.; Bjorgul, K. The role of femoral offset and abductor lever arm in total hip arthroplasty. J. Orthop. Traumatol. 2015, 16, 325–330. [Google Scholar] [CrossRef]
- Rudiger, H.A.; Guillemin, M.; Latypova, A.; Terrier, A. Effect of changes of femoral offset on abductor and joint reaction forces in total hip arthroplasty. Arch. Orthop. Trauma Surg. 2017, 137, 1579–1585. [Google Scholar] [CrossRef]
- Greidanus, N.V.; Chihab, S.; Garbuz, D.S.; Masri, B.A.; Tanzer, M.; Gross, A.E.; Duncan, C.P. Outcomes of minimally invasive anterolateral THA are not superior to those of minimally invasive direct lateral and posterolateral THA. Clin. Orthop. Relat. Res. 2013, 471, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Mjaaland, K.E.; Kivle, K.; Svenningsen, S.; Nordsletten, L. Do Postoperative Results Differ in a Randomized Trial Between a Direct Anterior and a Direct Lateral Approach in THA? Clin. Orthop. Relat. Res. 2019, 477, 145–155. [Google Scholar] [CrossRef]
- Jensen, C.; Aagaard, P.; Overgaard, S. Recovery in mechanical muscle strength following resurfacing vs. standard total hip arthroplasty-a randomised clinical trial. Osteoarthr. Cartil. 2011, 19, 1108–1116. [Google Scholar] [CrossRef] [PubMed]
- Von Roth, P.; Perka, C.; Mayr, H.O.; Preininger, B.; Ziebula, F.; Matziolis, G.; Hube, R. Reproducibility of femoral offset following short stem and straight stem total hip arthroplasty. Orthopedics 2014, 37, e678–e684. [Google Scholar] [CrossRef] [PubMed]


| CLS (35 hips) | Fitmore (32 hips) | p-Value | |
|---|---|---|---|
| Age at surgery (years) | 59 ± 8 (42–71) | 56 ± 10 (33–74) | 0.36 |
| Height | 170 ± 9 (156–188) | 169 ± 7 (153–188) | 0.77 |
| Weight (kg) | 84 ± 19 (62–138) | 82 ± 16 (53–116) | 0.94 |
| Body mass index (kg/m2) | 29 ± 5 (22–45) | 29 ± 5 (21–37) | 0.89 |
| Gender (F:M) | 16:19 | 15:17 | 0.39 |
| Affected side (L:R) | 14:21 | 14:18 | 0.53 |
| CLS (35 hips) | Fitmore (32 hips) | p-Value | |
|---|---|---|---|
| Abductor muscle strength preop. (Nm/kg) | 0.68 ± 0.41 | 0.63 ± 0.38 | 0.79 |
| Abductor muscle strength at 3 months (Nm/kg) | 0.67 ± 0.39 | 0.68 ± 0.42 | 0.48 |
| Abductor muscle strength at 12 months (Nm/kg) | 0.77 ± 0.43 | 0.88 ± 0.41 | 0.38 |
| HHS preop. | 53.4 ± 15.0 | 51.3 ± 14.4 | 0.50 |
| HHS at 3 months | 82.8 ± 14.3 | 86.1 ± 18.7 | 0.20 |
| HHS at 12 months | 88.8 ± 11.9 | 85.5 ± 14.8 | 0.48 |
| WOMAC preop. | 5.2 ± 2.2 | 4.8 ± 1.9 | 0.38 |
| WOMAC at 3 months | 1.3 ± 1.5 | 1.4 ± 1.0 | 0.24 |
| WOMAC at 12 months | 0.9 ± 1.0 | 1.3 ± 2.0 | 0.71 |
| Change femoral offset (mm) | 3.8 ± 6.6 | 4.3 ± 5.5 | 0.16 |
| Change total offset (mm) | 0.3 ± 9.6 | 0.1 ± 9.5 | 0.47 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuchs, M.; Hein, M.-A.; Faschingbauer, M.; Sgroi, M.; Bieger, R.; Reichel, H.; Freitag, T. Abductor Muscle Force after Straight-Stem Compared to Short-Stem Total Hip Arthroplasty through a Modified Direct Lateral Approach: Functional Assessment of 70 Consecutive Patients of a Randomized Controlled Clinical Trial. J. Clin. Med. 2021, 10, 1235. https://doi.org/10.3390/jcm10061235
Fuchs M, Hein M-A, Faschingbauer M, Sgroi M, Bieger R, Reichel H, Freitag T. Abductor Muscle Force after Straight-Stem Compared to Short-Stem Total Hip Arthroplasty through a Modified Direct Lateral Approach: Functional Assessment of 70 Consecutive Patients of a Randomized Controlled Clinical Trial. Journal of Clinical Medicine. 2021; 10(6):1235. https://doi.org/10.3390/jcm10061235
Chicago/Turabian StyleFuchs, Michael, Marie-Anne Hein, Martin Faschingbauer, Mirco Sgroi, Ralf Bieger, Heiko Reichel, and Tobias Freitag. 2021. "Abductor Muscle Force after Straight-Stem Compared to Short-Stem Total Hip Arthroplasty through a Modified Direct Lateral Approach: Functional Assessment of 70 Consecutive Patients of a Randomized Controlled Clinical Trial" Journal of Clinical Medicine 10, no. 6: 1235. https://doi.org/10.3390/jcm10061235
APA StyleFuchs, M., Hein, M.-A., Faschingbauer, M., Sgroi, M., Bieger, R., Reichel, H., & Freitag, T. (2021). Abductor Muscle Force after Straight-Stem Compared to Short-Stem Total Hip Arthroplasty through a Modified Direct Lateral Approach: Functional Assessment of 70 Consecutive Patients of a Randomized Controlled Clinical Trial. Journal of Clinical Medicine, 10(6), 1235. https://doi.org/10.3390/jcm10061235






