Patient-Specific Instrumentation Accuracy Evaluated with 3D Virtual Models
Abstract
1. Introduction
2. Experimental Section
3. Results
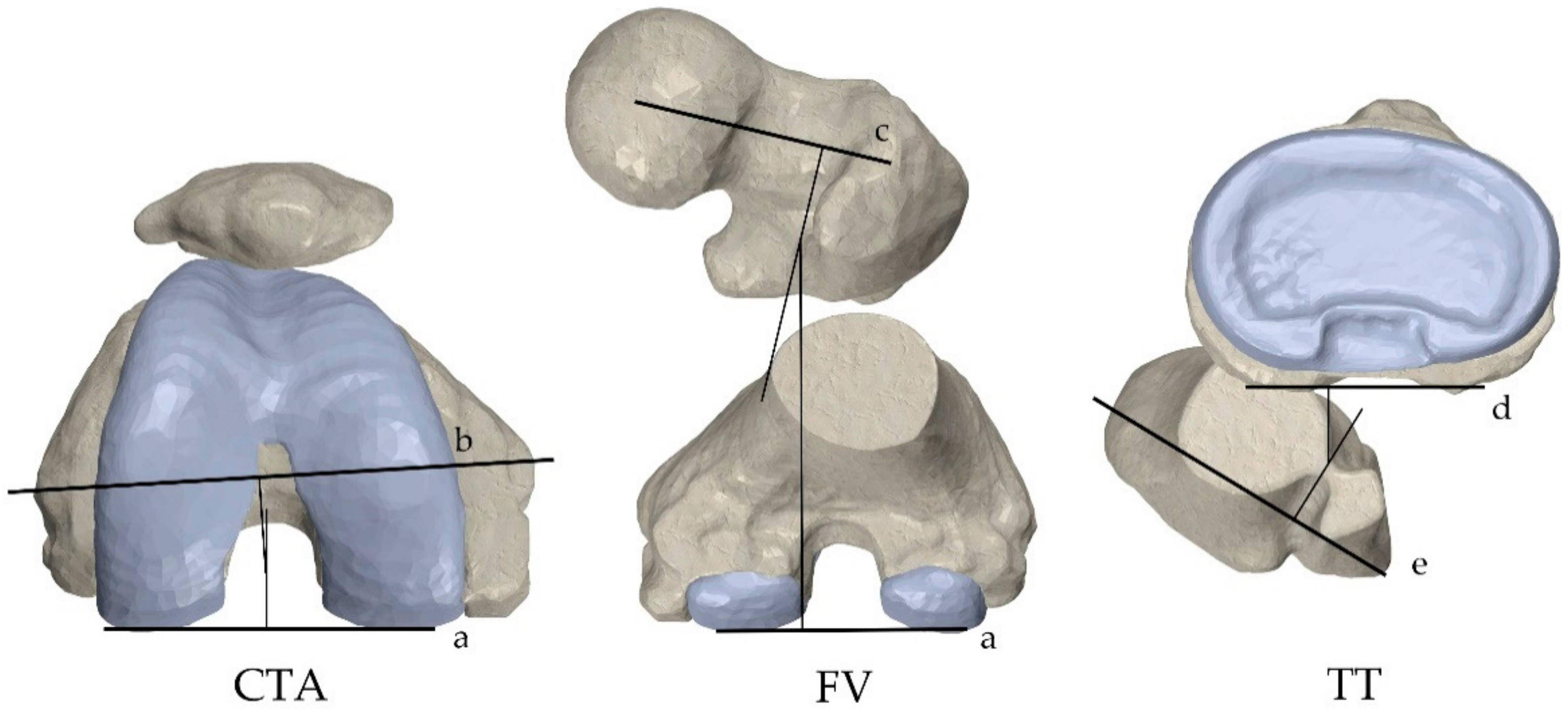
3.1. Results on the Coronal Plane
3.2. Results on the Sagittal Plane
3.3. Results on the Axial Plane
3.4. Effect Size
3.5. Implant Sizing
3.6. Clinical Assessment and Patient-Reported Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Skou, S.T.; Roos, E.M.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Simonsen, O.; Rasmussen, S. A Randomized, Controlled Trial of Total Knee Replacement. N. Engl. J. Med. 2015, 373, 1597–1606. [Google Scholar] [CrossRef] [PubMed]
- Price, A.J.; Alvand, A.; Troelsen, A.; Katz, J.N.; Hooper, G.; Gray, A.; Carr, A.; Beard, D. Knee replacement. Lancet 2018, 392, 1672–1682. [Google Scholar] [CrossRef]
- Jeffery, R.; Morris, R.; Denham, R. Coronal alignment after total knee replacement. J. Bone Jt. Surg. Br. 1991, 73, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.; Ritter, M.A. Malalignment: Forewarned Is Forearmed. Orthopedics 2009, 32, 681–682. [Google Scholar] [CrossRef]
- Abdel, M.P.; Oussedik, S.; Parratte, S.; Lustig, S.; Haddad, F.S. Coronal alignment in total knee replacement. Bone Jt. J. 2014, 96, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Parratte, S.; Pagnano, M.W.; Trousdale, R.T.; Berry, D.J. Effect of Postoperative Mechanical Axis Alignment on the Fifteen-Year Survival of Modern, Cemented Total Knee Replacements. J. Bone Jt. Surg. 2010, 92, 2143–2149. [Google Scholar] [CrossRef]
- Abdel, M.P.; Ollivier, M.; Parratte, S.; Trousdale, R.T.; Berry, D.J.; Pagnano, M.W. Effect of Postoperative Mechanical Axis Alignment on Survival and Functional Outcomes of Modern Total Knee Arthroplasties with Cement. J. Bone Jt. Surg. 2018, 100, 472–478. [Google Scholar] [CrossRef]
- Howell, S.M.; Howell, S.J.; Kuznik, K.T.; Cohen, J.; Hull, M.L. Does A Kinematically Aligned Total Knee Arthroplasty Restore Function Without Failure Regardless of Alignment Category? Clin. Orthop. Relat. Res. 2013, 471, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Rivière, C.; Vendittoli, P.-A. Personalized Hip and Knee Joint Replacement; Springer International Publishing: Cham, Switzerland, 2020; ISBN 978-3-030-24242-8. [Google Scholar]
- Xu, J.; Cao, J.Y.; Luong, J.K.; Negus, J.J. Kinematic versus mechanical alignment for primary total knee replacement: A systematic review and meta-analysis. J. Orthop. 2019, 16, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Thienpont, E.; Bellemans, J.; Victor, J.; Becker, R. Alignment in total knee arthroplasty, still more questions than answers. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2191–2193. [Google Scholar] [CrossRef]
- Rivière, C.; Vigdorchik, J.M.; Vendittoli, P.-A. Mechanical alignment: The end of an era! Orthop. Traumatol. Surg. Res. 2019, 105, 1223–1226. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Becker, R.; Tandogan, R.; Vendittoli, P.-A.; Howell, S. Alignment in TKA: What has been clear is not anymore! Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2037–2039. [Google Scholar] [CrossRef]
- Mihalko, W.M.; Boyle, J.; Clark, L.D.; Krackow, K.A. The Variability of Intramedullary Alignment of the Femoral Component During Total Knee Arthroplasty. J. Arthroplast. 2005, 20, 25–28. [Google Scholar] [CrossRef]
- Novotny, J.; Gonzalez, M.H.; Amirouche, F.M.L.; Li, Y.C. Geometric analysis of potential error in using femoral intramedullary guides in total knee arthroplasty. J. Arthroplast. 2001, 16, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Koenen, P.; Ates, D.M.; Pfeiffer, T.R.; Bouillon, B.; Bäthis, H. Femoral flexion position is a highly variable factor in total knee arthroplasty: An analysis of 593 conventionally aligned total knee replacements. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1014–1022. [Google Scholar] [CrossRef]
- Mason, J.B.; Fehring, T.K.; Estok, R.; Banel, D.; Fahrbach, K. Meta-Analysis of Alignment Outcomes in Computer-Assisted Total Knee Arthroplasty Surgery. J. Arthroplast. 2007, 22, 1097–1106. [Google Scholar] [CrossRef]
- Hetaimish, B.M.; Khan, M.M.; Simunovic, N.; Al-Harbi, H.H.; Bhandari, M.; Zalzal, P.K. Meta-Analysis of Navigation vs Conventional Total Knee Arthroplasty. J. Arthroplast. 2012, 27, 1177–1182. [Google Scholar] [CrossRef]
- Gao, J.; Dong, S.; Li, J.J.; Ge, L.; Xing, D.; Lin, J. New technology-based assistive techniques in total knee arthroplasty: A Bayesian network meta-analysis and systematic review. Int. J. Med. Robot. Comput. Assist. Surg. 2020. [Google Scholar] [CrossRef]
- León-Muñoz, V.J.; Martínez-Martínez, F.; López-López, M.; Santonja-Medina, F. Patient-specific instrumentation in total knee arthroplasty. Expert Rev. Med. Devices 2019, 16, 555–567. [Google Scholar] [CrossRef] [PubMed]
- Voleti, P.B.; Hamula, M.J.; Baldwin, K.D.; Lee, G.-C. Current Data Do Not Support Routine Use of Patient-Specific Instrumentation in Total Knee Arthroplasty. J. Arthroplast. 2014, 29, 1709–1712. [Google Scholar] [CrossRef] [PubMed]
- Thienpont, E.; Schwab, P.E.; Fennema, P. A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Jt. J. 2014, 96, 1052–1061. [Google Scholar] [CrossRef]
- Alcelik, I.; Blomfield, M.; Öztürk, C.; Soni, A.; Charity, R.; Acornley, A. A comparison of short term radiological alignment outcomes of the patient specific and standard instrumentation for primary total knee arthroplasty: A systematic review and meta-analysis. Acta Orthop. Traumatol. Turc. 2017, 51, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Thienpont, E.; Schwab, P.-E.; Fennema, P. Efficacy of Patient-Specific Instruments in Total Knee Arthroplasty. J. Bone Jt. Surg. 2017, 99, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Schotanus, M.G.M.; Thijs, E.; Heijmans, M.; Vos, R.; Kort, N.P. Favourable alignment outcomes with MRI-based patient-specific instruments in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2659–2668. [Google Scholar] [CrossRef] [PubMed]
- Gong, S.; Xu, W.; Wang, R.; Wang, Z.; Wang, B.; Han, L.; Chen, G. Patient-specific instrumentation improved axial alignment of the femoral component, operative time and perioperative blood loss after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1083–1095. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Yang, Z.; Liao, W.; Wang, W.; Zou, Y.; Pan, Y.; Feng, Z. Fewer femoral rotational outliers produced with CT- than with MRI-based patient-specific instrumentation in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2930–2941. [Google Scholar] [CrossRef] [PubMed]
- Kizaki, K.; Shanmugaraj, A.; Yamashita, F.; Simunovic, N.; Duong, A.; Khanna, V.; Ayeni, O.R. Total knee arthroplasty using patient-specific instrumentation for osteoarthritis of the knee: A meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 561. [Google Scholar] [CrossRef]
- Russell, R.; Brown, T.; Huo, M.; Jones, R. Patient-Specific Instrumentation Does Not Improve Alignment in Total Knee Arthroplasty. J. Knee Surg. 2014, 27, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Cavaignac, E.; Pailhé, R.; Laumond, G.; Murgier, J.; Reina, N.; Laffosse, J.M.; Bérard, E.; Chiron, P. Evaluation of the accuracy of patient-specific cutting blocks for total knee arthroplasty: A meta-analysis. Int. Orthop. 2015, 39, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Wang, J.; Zhou, S.; Cheng, T.; Zhang, W.; Wang, Q.; Zhang, X. No difference in mechanical alignment and femoral component placement between patient-specific instrumentation and conventional instrumentation in TKA. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3288–3295. [Google Scholar] [CrossRef]
- Mannan, A.; Smith, T.O.; Sagar, C.; London, N.J.; Molitor, P.J.A. No demonstrable benefit for coronal alignment outcomes in PSI knee arthroplasty: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2015, 101, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Tang, Z.-H.; Hu, J.-Z.; Zou, G.-Y.; Xiao, R.-C.; Yan, D.-X. Patient-Specific Instrumentation Does Not Improve Accuracy in Total Knee Arthroplasty. Orthopedics 2015, 38, e178–e188. [Google Scholar] [CrossRef] [PubMed]
- Sharareh, B.; Schwarzkopf, R. Review Article: Patient-Specific versus Standard Instrumentation for Total Knee Arthroplasty. J. Orthop. Surg. 2015, 23, 100–106. [Google Scholar] [CrossRef]
- Huijbregts, H.J.T.A.M.; Khan, R.J.K.; Sorensen, E.; Fick, D.P.; Haebich, S. Patient-specific instrumentation does not improve radiographic alignment or clinical outcomes after total knee arthroplasty. Acta Orthop. 2016, 87, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Mannan, A.; Smith, T.O. Favourable rotational alignment outcomes in PSI knee arthroplasty: A Level 1 systematic review and meta-analysis. Knee 2016, 23, 186–190. [Google Scholar] [CrossRef]
- Wu, X.-D.; Xiang, B.-Y.; Schotanus, M.G.M.; Liu, Z.-H.; Chen, Y.; Huang, W. CT- versus MRI-based patient-specific instrumentation for total knee arthroplasty: A systematic review and meta-analysis. Surgeon 2017, 15, 336–348. [Google Scholar] [CrossRef]
- Koch, P.P.; Müller, D.; Pisan, M.; Fucentese, S.F. Radiographic accuracy in TKA with a CT-based patient-specific cutting block technique. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2200–2205. [Google Scholar] [CrossRef] [PubMed]
- Helmy, N.; Dao Trong, M.L.; Kühnel, S.P. Accuracy of Patient Specific Cutting Blocks in Total Knee Arthroplasty. Biomed. Res. Int. 2014, 2014, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Anderl, W.; Pauzenberger, L.; Kölblinger, R.; Kiesselbach, G.; Brandl, G.; Laky, B.; Kriegleder, B.; Heuberer, P.; Schwameis, E. Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 102–111. [Google Scholar] [CrossRef]
- Pauzenberger, L.; Munz, M.; Brandl, G.; Frank, J.K.; Heuberer, P.R.; Laky, B.; Schwameis, E.; Anderl, W. Patient-specific instrumentation improved three-dimensional accuracy in total knee arthroplasty: A comparative radiographic analysis of 1257 total knee arthroplasties. J. Orthop. Surg. Res. 2019, 14, 437. [Google Scholar] [CrossRef] [PubMed]
- Parratte, S.; Blanc, G.; Boussemart, T.; Ollivier, M.; Le Corroller, T.; Argenson, J.-N. Rotation in total knee arthroplasty: No difference between patient-specific and conventional instrumentation. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2213–2219. [Google Scholar] [CrossRef] [PubMed]
- Roh, Y.W.; Kim, T.W.; Lee, S.; Seong, S.C.; Lee, M.C. Is TKA Using Patient-specific Instruments Comparable to Conventional TKA? A Randomized Controlled Study of One System. Clin. Orthop. Relat. Res. 2013, 471, 3988–3995. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Sampaio, R.; Pinto, E. Patient-specific instrumentation improves tibial component rotation in TKA. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Victor, J.; Dujardin, J.; Vandenneucker, H.; Arnout, N.; Bellemans, J. Patient-specific Guides Do Not Improve Accuracy in Total Knee Arthroplasty: A Prospective Randomized Controlled Trial. Clin. Orthop. Relat. Res. 2014, 472, 263–271. [Google Scholar] [CrossRef]
- Woolson, S.T.; Harris, A.H.; Wagner, D.W.; Giori, N.J. Component Alignment During Total Knee Arthroplasty with Use of Standard or Custom Instrumentation. J. Bone Jt. Surg. 2014, 96, 366–372. [Google Scholar] [CrossRef]
- Boonen, B.; Schotanus, M.G.M.; Kerens, B.; Hulsmans, F.-J.; Tuinebreijer, W.E.; Kort, N.P. Patient-specific positioning guides for total knee arthroplasty: No significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2809–2817. [Google Scholar] [CrossRef]
- De Vloo, R.; Pellikaan, P.; Dhollander, A.; Vander Sloten, J. Three-dimensional analysis of accuracy of component positioning in total knee arthroplasty with patient specific and conventional instruments: A randomized controlled trial. Knee 2017, 24, 1469–1477. [Google Scholar] [CrossRef]
- León-Muñoz, V.J.; Parrinello, A.; López-López, M.; Martínez-Martínez, F.; Santonja-Medina, F. Revision of total knee arthroplasty with the use of patient-specific instruments: An alternative surgical technique. Expert Rev. Med. Devices 2020, 17, 795–806. [Google Scholar] [CrossRef] [PubMed]
- León-Muñoz, V.J.; López-López, M.; Martínez-Martínez, F.; Santonja-Medina, F. Comparison of weight-bearing full-length radiographs and computed-tomography-scan-based three-dimensional models in the assessment of knee joint coronal alignment. Knee 2020, 27, 543–551. [Google Scholar] [CrossRef]
- Behrend, H.; Giesinger, K.; Giesinger, J.M.; Kuster, M.S. The “Forgotten Joint” as the Ultimate Goal in Joint Arthroplasty. J. Arthroplast. 2012, 27, 430–436. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Lei, K.; Liu, L.; Chen, X.; Feng, Q.; Yang, L.; Guo, L. Navigation and robotics improved alignment compared with PSI and conventional instrument, while clinical outcomes were similar in TKA: A network meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Delport, H.P.; Vander Sloten, J. Evaluation of Patient Specific Instruments. To measure is to know! J. Arthroplast. 2015, 30, 720–721. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Iranpour, F.; Konala, P.; Kerner, A.; Rasch, H.; Cobb, J.P.; Friederich, N.F. A novel standardized algorithm for evaluating patients with painful total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Holme, T.J.; Henckel, J.; Cobb, J.; Hart, A.J. Quantification of the difference between 3D CT and plain radiograph for measurement of the position of medial unicompartmental knee replacements. Knee 2011, 18, 300–305. [Google Scholar] [CrossRef]
- De Valk, E.J.; Noorduyn, J.C.A.; Mutsaerts, E.L.A.R. How to assess femoral and tibial component rotation after total knee arthroplasty with computed tomography: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3517–3528. [Google Scholar] [CrossRef] [PubMed]
- Jonkergouw, F.; Allé, F.; Chellaoui, K.; Vander Sloten, J.; Vangeneugden, D. Three-dimensional measurement technique to assess implant position and orientation after total knee arthroplasty. Med. Eng. Phys. 2016, 38, 1513–1517. [Google Scholar] [CrossRef]
- Bugbee, W.D.; Mizu-Uchi, H.; Patil, S.; D’Lima, D. Accuracy of Implant Placement Utilizing Customized Patient Instrumentation in Total Knee Arthroplasty. Adv. Orthop. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Moopanar, T.R.; Amaranath, J.E.; Sorial, R.M. Component position alignment with patient-specific jigs in total knee arthroplasty. ANZ J. Surg. 2014, 84, 628–632. [Google Scholar] [CrossRef]
- Heyse, T.J.; Tibesku, C.O. Improved femoral component rotation in TKA using patient-specific instrumentation. Knee 2014, 21, 268–271. [Google Scholar] [CrossRef] [PubMed]
- MacDessi, S.J.; Jang, B.; Harris, I.A.; Wheatley, E.; Bryant, C.; Chen, D.B. A comparison of alignment using patient specific guides, computer navigation and conventional instrumentation in total knee arthroplasty. Knee 2014, 21, 406–409. [Google Scholar] [CrossRef]
- Ng, V.Y.; Arnott, L.; Li, J.; Hopkins, R.; Lewis, J.; Sutphen, S.; Nicholson, L.; Reader, D.; McShane, M.A. Comparison of custom to standard TKA instrumentation with computed tomography. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Chotanaphuti, T.; Wangwittayakul, V.; Khuangsirikul, S.; Foojareonyos, T. The accuracy of component alignment in custom cutting blocks compared with conventional total knee arthroplasty instrumentation: Prospective control trial. Knee 2014, 21, 185–188. [Google Scholar] [CrossRef]
- Ferrara, F.; Cipriani, A.; Magarelli, N.; Rapisarda, S.; De Santis, V.; Burrofato, A.; Leone, A.; Bonomo, L. Implant Positioning in TKA: Comparison Between Conventional and Patient-Specific Instrumentation. Orthopedics 2015, 38, e271–e280. [Google Scholar] [CrossRef] [PubMed]
- Boonen, B.; Schotanus, M.G.M.; Kerens, B.; van der Weegen, W.; van Drumpt, R.A.M.; Kort, N.P. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: A multicentre, randomised controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2206–2212. [Google Scholar] [CrossRef]
- Hamilton, W.G.; Parks, N.L. Patient-Specific Instrumentation Does Not Shorten Surgical Time: A Prospective, Randomized Trial. J. Arthroplast. 2014, 29, 1508–1509. [Google Scholar] [CrossRef]
- Kotela, A.; Kotela, I. Patient-specific computed tomography based instrumentation in total knee arthroplasty: A prospective randomized controlled study. Int. Orthop. 2014, 38, 2099–2107. [Google Scholar] [CrossRef] [PubMed]
- Abane, L.; Anract, P.; Boisgard, S.; Descamps, S.; Courpied, J.P.; Hamadouche, M. A comparison of patient-specific and conventional instrumentation for total knee arthroplasty. Bone Jt. J. 2015, 97, 56–63. [Google Scholar] [CrossRef]
- Yan, C.H.; Chiu, K.Y.; Ng, F.Y.; Chan, P.K.; Fang, C.X. Comparison between patient-specific instruments and conventional instruments and computer navigation in total knee arthroplasty: A randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3637–3645. [Google Scholar] [CrossRef] [PubMed]
- Carlson, V.R.; Post, Z.D.; Orozco, F.R.; Davis, D.M.; Lutz, R.W.; Ong, A.C. When Does the Knee Feel Normal Again: A Cross-Sectional Study Assessing the Forgotten Joint Score in Patients After Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 700–703. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.R.; Corbett, J.A.; Wastnedge, E.; Nicolai, P. Forgotten Joint Score: Comparison between total and unicondylar knee arthroplasty. Knee 2021, 29, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Behrend, H.; Zdravkovic, V.; Bösch, M.; Hochreiter, B. No difference in joint awareness after TKA: A matched-pair analysis of a classic implant and its evolutional design. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2124–2129. [Google Scholar] [CrossRef]
- León-Muñoz, V.J.; López-López, M.; Martínez-Martínez, F.; Santonja-Medina, F. Impact of surgical instrumentation on hospital length of stay and cost of total knee arthroplasty. Expert Rev. Pharm. Outcomes Res. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
| Weight (kg) | Height (cm) | BMI (kg/m2) | Age (Years) | |
|---|---|---|---|---|
| Female cases | 71.1 (6.9) (57–84) | 159.3 (4.3) (149–165) | 28.1 (3.1) (21.7–33.2) | 72.3 (5.8) (59–81) |
| Male cases | 75 (6.9) (63–84) | 165.2 (6) (157–175) | 27.5 (2.3) (22.6–32.1) | 69.8 (7.5) (57–81) |
| sFLDA (°) | PMTA (°) | HKA (°) | |
|---|---|---|---|
| Engineer 1 | 90.96 (1.52) (88–94.5) | 88.73 (1.34) (86–92) | 179.09 (1.95) (175–184) |
| Engineer 2 | 91.03 (1.5) (88.5–94.5) | 88.91 (1.22) (86–92) | 179.23 (1.93) (175–183.5) |
| Mean CT-scan | 90.99 (1.5) (88–94.5) | 88.82 (1.27) (86–92) | 179.16 (1.93) (175–184) |
| Evaluator 1 # | 90.19 (1.43) (87–94) | 88.7 (1.13) (86.5–92) | 179.1 (2.34) (174–185) |
| Evaluator 2 # | 90.16 (1.67) (86–94) | 88.69 (1.08) (86.5–91.5) | 179.16 (2.33) (174–185) |
| Mean X-ray # | 90.17 (1.55) (86–94) | 88.69 (1.1) (86.5–92) | 179.13 (2.32) (174–185) |
| sFLDA (°) | PMTA (°) | HKA (°) | |
|---|---|---|---|
| Engineer 1 | 1.44 (1.05) (0–4.5) | 1.56 (0.98) (0–4) | 1.71 (1.28) (0–5) |
| Engineer 2 | 1.46 (1.08) (0–4.5) | 1.31 (0.96) (0–4) | 1.57 (1.34) (0–5) |
| Mean values | 1.45 (1.06) (0–4.5) | 1.44 (0.97) (0–4) | 1.64 (1.3) (0–5) |
| Pre-Operative | Engineer 1 * | Engineer 2 * | |
|---|---|---|---|
| FV (°) | 12.79 (7.17) (−2.5–31.5) | 10.32 (7.49) (−2.5–26.5) | 10.91 (7.16) (−1–27) |
| TT (°) | 24.6 (7.76) (6.5–39) | 24.09 (7.33) (10–36) | 25.3 (7.54) (13.5–38.5) |
| d-Value for Engineer 1 | d-Value for Engineer 2 | |
|---|---|---|
| Planned vs. measured sFLDA | −0.89 | −0.97 |
| Planned vs. measured PMTA | 1.35 | 1.26 |
| Planned vs. measured HKA | 0.66 | 0.56 |
| Planned vs. measured FFA | −0.58 | −0.53 |
| Planned vs. measured tibial slope | −0.76 | −0.76 |
| Planned vs. measured CTA | 0.36 | 0.32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
León-Muñoz, V.J.; Parrinello, A.; Manca, S.; Galloni, G.; López-López, M.; Martínez-Martínez, F.; Santonja-Medina, F. Patient-Specific Instrumentation Accuracy Evaluated with 3D Virtual Models. J. Clin. Med. 2021, 10, 1439. https://doi.org/10.3390/jcm10071439
León-Muñoz VJ, Parrinello A, Manca S, Galloni G, López-López M, Martínez-Martínez F, Santonja-Medina F. Patient-Specific Instrumentation Accuracy Evaluated with 3D Virtual Models. Journal of Clinical Medicine. 2021; 10(7):1439. https://doi.org/10.3390/jcm10071439
Chicago/Turabian StyleLeón-Muñoz, Vicente J., Andrea Parrinello, Silvio Manca, Gianluca Galloni, Mirian López-López, Francisco Martínez-Martínez, and Fernando Santonja-Medina. 2021. "Patient-Specific Instrumentation Accuracy Evaluated with 3D Virtual Models" Journal of Clinical Medicine 10, no. 7: 1439. https://doi.org/10.3390/jcm10071439
APA StyleLeón-Muñoz, V. J., Parrinello, A., Manca, S., Galloni, G., López-López, M., Martínez-Martínez, F., & Santonja-Medina, F. (2021). Patient-Specific Instrumentation Accuracy Evaluated with 3D Virtual Models. Journal of Clinical Medicine, 10(7), 1439. https://doi.org/10.3390/jcm10071439







