Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer
Abstract
1. Introduction
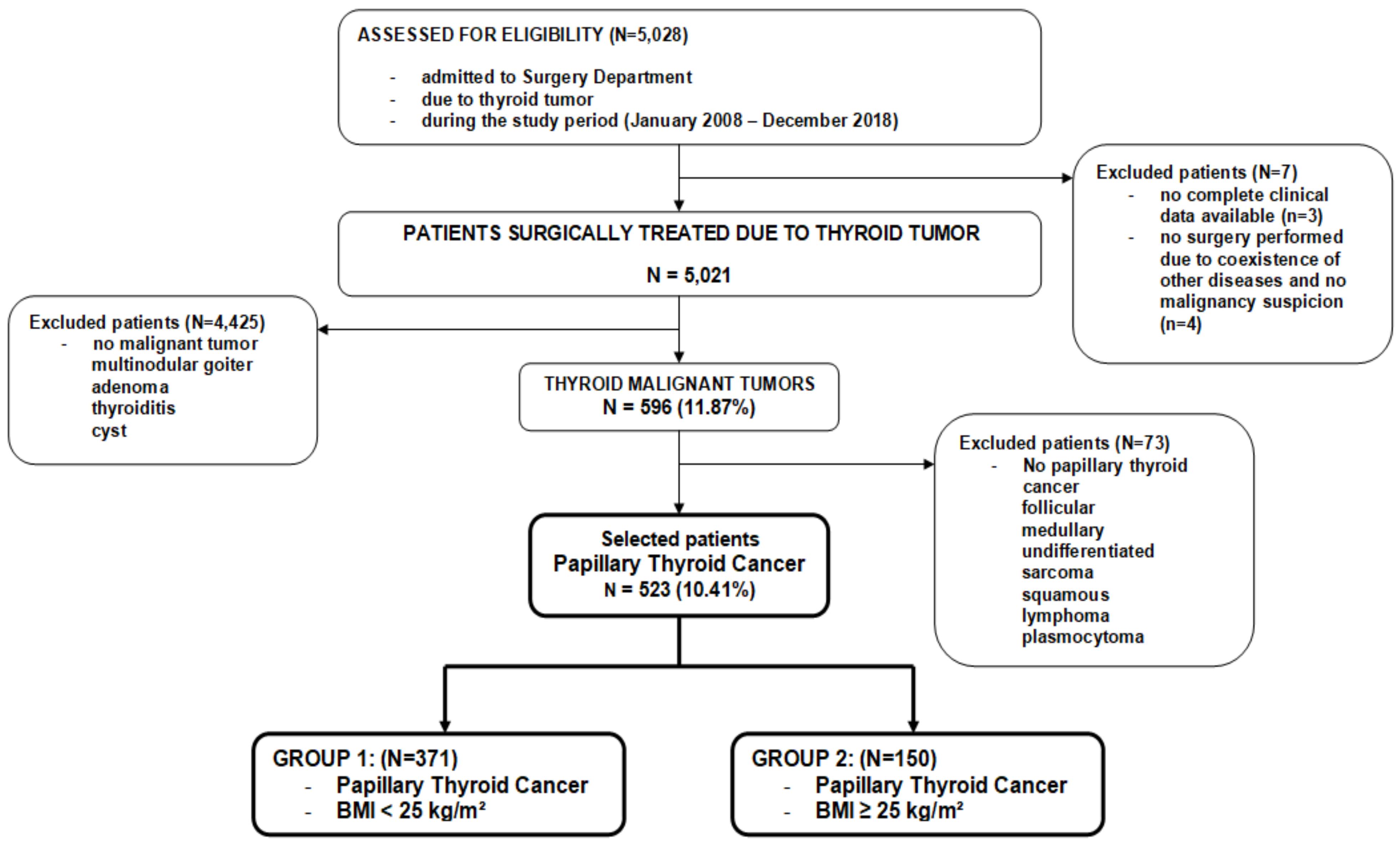
2. Materials and Methods
2.1. Study Design and Methods
2.2. Anthropometric Measurements
2.3. Measured Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients with PTC
3.2. Demographic, Clinical and Histopathological Characteristics of PTC Patients According to BMI
3.3. Selected Ultrasound and Histopathological Features with Respect to BMI. Association of BMI ≥ 25 kg/m2 with Disease Severity Indicator.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bradley, D. Obesity, thyroid nodularity, and thyroid cancer: Epiphenomenon or cause? J. Clin. Endocrinol. Metab. 2020, 105, dgaa376. [Google Scholar] [CrossRef] [PubMed]
- Gelsomino, L.; Naimo, G.D.; Malivindi, R.; Augimeri, G.; Panza, S.; Giordano, C.; Barone, I.; Bonofiglio, D.; Mauro, L.; Catalano, S.; et al. Knockdown of leptin receptor affects macrophage phenotype in the tumor microenvironment inhibiting breast cancer growth and progression. Cancers 2020, 12, 2078. [Google Scholar] [CrossRef] [PubMed]
- Han, S.J.; Boyko, E.J. The evidence for an obesity paradox in type 2 diabetes mellitus. Diabetes Metab. J. 2018, 42, 179–187. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- De Pergola, G.; Silvestris, F. Obesity as a major risk factor for cancer. J. Obes. 2013, 2013, 291546. [Google Scholar] [CrossRef]
- Wolin, K.Y.; Carson, K.; Colditz, G.A. Obesity and cancer. Oncologist 2010, 15, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Brocco, D.; Florio, R.; De Lellis, L.; Veschi, S.; Grassadonia, A.; Tinari, N.; Cama, A. The role of dysfunctional adipose tissue in pancreatic cancer: A molecular perspective. Cancers 2020, 12, 1849. [Google Scholar] [CrossRef] [PubMed]
- Steele, C.B.; Thomas, C.C.; Henley, S.J.; Massetti, G.M.; Galuska, D.A.; Agurs-Collins, T.; Puckett, M.; Richardson, L.C. Vital signs: Trends in incidence of cancers associated with overweight and obesity—United States, 2005–2014. Morb. Mortal. Wkly. Rep. 2017, 66, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Scherübl, H. Übermäßiges Körpergewicht und Krebsrisiko. Dtsch. Med. Wochenschr. 2020, 145, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Grosse, Y.; Bianchini, F.; Straif, K. Body fatness and cancer--viewpoint of the IARC working group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef]
- Kitahara, C.M.; McCullough, M.L.; Franceschi, S.; Rinaldi, S.; Wolk, A.; Neta, G.; Adami, H.O.; Anderson, K.; Andreotti, G.; Freeman, L.E.B.; et al. Anthropometric factors and thyroid cancer risk by histological subtype: Pooled analysis of 22 prospective studies. Thyroid 2016, 26, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Han, K.-D.; Park, C.-Y. Weight change is significantly associated with risk of thyroid cancer: A nationwide population-based cohort study. Sci. Rep. 2019, 9, 1546. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Port, M.; Landi, S.; Gemignani, F.; Cipollini, M.; Elisei, R.; Goudeva, L.; Müller, J.A.; Nerlich, K.; Pellegrini, G.; et al. Obesity and the risk of papillary thyroid cancer: A pooled analysis of three case-control studies. Thyroid 2014, 24, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.G.; Cheng, S.Y. Mechanisms linking obesity and thyroid cancer development and progression in mouse models. Horm. Cancer 2018, 9, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Schmid, D.; Ricci, C.; Behrens, G.; Leitzmann, M.F. Adiposity and risk of thyroid cancer: A systematic review and meta-analysis. Obes. Rev. 2015, 16, 1042–1054. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, M.; Kim, J.H.; Kim, J.; Han, K.; Kim, B.; Kim, D.H.; Park, Y.G. Metabolic syndrome and the risk of thyroid cancer: A nationwide population-based cohort study. Thyroid 2020, 30, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.T.; Pandeya, N.; Neale, R.E.; McLeod, D.S.; Bain, C.J.; Baade, P.D.; Youl, P.H.; Allison, R.; Leonard, S.; Jordan, S.J. Obesity is associated with BRAF(V600E)-mutated thyroid cancer. Thyroid 2020, 30, 1518–1527. [Google Scholar] [CrossRef] [PubMed]
- Fussey, J.M.; Beaumont, R.N.; Wood, A.R.; Vaidya, B.; Smith, J.; Tyrrell, J. Does obesity cause thyroid cancer? A mendelian randomization study. J. Clin. Endocrinol. Metab. 2020, 105, e2398–e2407. [Google Scholar] [CrossRef]
- Kaliszewski, K.; Diakowska, D.; Wojtczak, B.; Rudnicki, J. Cancer screening activity results in overdiagnosis and overtreatment of papillary thyroid cancer: A 10-year experience at a single institution. PLoS ONE 2020, 15, e0236257. [Google Scholar] [CrossRef]
- Kwon, H.; Park, S.E.; Yun, J.S.; Park, C.Y. Serum adiponectin and progranulin level in patients with benign thyroid nodule or papillary thyroid cancer. Endocrinol. Metab. 2020, 35, 396–406. [Google Scholar] [CrossRef]
- Perrier, N.D.; Brierley, J.D.; Tuttle, R.M. Differentiated and anaplastic thyroid carcinoma: Major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2018, 68, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Cibas, E.S.; Ali, S.Z. The Bethesda System for Reporting Thyroid Cytopathology. Am. J. Clin. Pathol. 2009, 132, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Kaliszewski, K.; Diakowska, D.; Wojtczak, B.; Forkasiewicz, Z.; Pupka, D.; Nowak, Ł.; Rudnicki, J. Which papillary thyroid microcarcinoma should be treated as "true cancer" and which as “precancer”? World J. Surg. Oncol. 2019, 17, 91. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Managing The Global Epidemic: Report of a WHO Consultation; WHO Technical Report Series 894; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Biondi, B. Thyroid and obesity: An intriguing relationship. J. Clin. Endocrinol. Metab. 2010, 95, 3614–3617. [Google Scholar] [CrossRef]
- Lai, X.; Ouyang, P.; Zhu, H.; An, S.; Xia, L.; Yao, Y.; Zhang, H.; Li, Z.; Deng, K. Detection rate of thyroid nodules in routine health check-up and its influencing factors: A 10-year survey of 309 576 cases. Nan Fang Yi Ke Da Xue Xue Bao 2020, 40, 268–273. [Google Scholar]
- Mc Allister, E.J.; Dhurandhar, N.V.; Keith, S.W. Ten putative contributors to the obesity epidemic. Crit. Rev. Food Sci. Nutr. 2009, 49, 868–913. [Google Scholar] [CrossRef]
- Kitahara, C.M.; Sosa, J.A. The changing incidence of thyroid cancer. Nat. Rev. Endocrinol. 2016, 12, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Dossus, L.; Franceschi, S.; Biessy, C.; Navionis, A.-S.; Travis, R.C.; Weiderpass, E.; Scalbert, A.; Romieu, I.; Tjønneland, A.; Olsen, A.; et al. Adipokines and inflammation markers and risk of differentiated thyroid carcinoma: The EPIC study. Int. J. Cancer 2018, 142, 1332–1342. [Google Scholar] [CrossRef] [PubMed]
- Marcello, M.A.; Cunha, L.L.; Batista, F.A.; Ward, L.S. Obesity and thyroid cancer. Endocr. Relat. Cancer 2014, 21, T255–T271. [Google Scholar] [CrossRef] [PubMed]
- Abella, V.; Pino, J.; Scotece, M.; Conde, J.; Lago, F.; Gonzalez-Gay, M.A.; Mera, A.; Gómez, R.; Mobasheri, A.; Gualillo, O. Progranulin as a biomarker and potential therapeutic agent. Drug. Discov. Today 2017, 22, 1557–1564. [Google Scholar] [CrossRef]
- Arechavaleta-Velasco, F.; Perez-Juarez, C.E.; Gerton, G.L.; Diaz-Cueto, L. Progranulin and its biological effects in cancer. Med. Oncol. 2017, 34, 194. [Google Scholar] [CrossRef]
- Choi, J.S.; Kim, E.K.; Moon, H.J.; Kwak, J.Y. Higher body mass index may be a predictor of extrathyroidal extension in patients with papillary thyroid microcarcinoma. Endocrine 2015, 48, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Kim, N.K.; Choi, J.H.; Sohn, S.Y.; Kim, S.W.; Jin, S.-M.; Jang, H.W.; Suh, S.; Min, Y.-K.; Chung, J.H.; et al. Associations between body mass index and clinico-pathological characteristics of papillary thyroid cancer. Clin. Endocrinol. 2013, 78, 134–140. [Google Scholar] [CrossRef]
- Trésallet, C.; Seman, M.; Tissier, F.; Buffet, C.; Lupinacci, R.M.; Vuarnesson, H.; Leenhardt, L.; Menegaux, F. The incidence of papillary thyroid carcinoma and outcomes in operative patients according to their body mass indices. Surgery 2014, 156, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Seiberling, K.A.; Dutra, J.C.; Grant, T.; Bajramovic, S. Role of intrathyroidal calcifications detected on ultrasound as a marker of malignancy. Laryngoscope 2004, 114, 1753–1757. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, S.; Morgan, M.P. Microcalcifications in breast cancer: From pathophysiology to diagnosis and prognosis. Biochim. Biophys. Acta Rev. Cancer 2018, 1869, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Kitzing, Y.X.; Prando, A.; Varol, C.; Karczmar, G.S.; Maclean, F.; Oto, A. Benign conditions that mimic prostate carcinoma: MRI imaging features with histopathologic correlation. Radiographics 2016, 36, 162–175. [Google Scholar] [CrossRef]
- Zapiach, M.; Yadav, D.; Smyrk, T.C.; Fletcher, J.G.; Pearson, R.K.; Clain, J.E.; Farnell, M.B.; Chari, S.T. Calcifying obstructive pancreatitis: A study of intraductal papillary mucinous neoplasm associated with pancreatic calcification. Clin. Gastroenterol. Hepatol. 2004, 2, 57–63. [Google Scholar] [CrossRef]
- Li, C.; Zhou, L.; Dionigi, G.; Li, F.; Zhao, Y.; Sun, H. The association between tumor tissue calcification, obesity, and thyroid cancer invasiveness in a cohort study. Endocr. Pract. 2020. [Google Scholar] [CrossRef]
- Kaliszewski, K.; Diakowska, D.; Wojtczak, B.; Migoń, J.; Kasprzyk, A.; Rudnicki, J. The occurrence of and predictive factors for multifocality and bilaterality in patients with papillary thyroid microcarcinoma. Medicine 2019, 98, e15609. [Google Scholar] [CrossRef]
- Li, C.L.; Dionigi, G.; Zhao, Y.S.; Liang, N.; Sun, H. Influence of body mass index on the clinicopathological features of 13,995 papillary thyroid tumors. J. Endocrinol. Invest. 2020, 43, 1283–1299. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Jia, X.; Fan, X.; Zhao, L.; Pang, P.; Wang, Y.; Luo, Y.; Wang, F.; Yang, G.; Wang, X.; et al. Association of obesity with the clinicopathological features of thyroid cancer in a large, operative population: A retrospective case-control study. Medicine 2019, 98, e18213. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Total | Group 1: BMI < 25 kg/m2 (n = 373) | Group 2: BMI ≥ 25 kg/m2 (n = 150) | p-Value |
|---|---|---|---|---|
| (n = 523) | ||||
| Sex: | 0.724 | |||
| Female | 456 (87.2) | 324 (86.9) | 132 (88.0) | |
| Male | 67 (12.8) | 49 (13.1) | 18 (12.0) | |
| Age at diagnosis (years) | 49.82 ± 15.67 | 48.59 ± 16.25 | 52.86 ± 13.73 | 0.005 * |
| Age: | 0.127 | |||
| <55 years | 306 (58.5) | 226 (60.6) | 80 (53.3) | |
| ≥55 years | 217 (41.5) | 147 (39.4) | 70 (46.7) | |
| TSH (mU/L) | 1.79 ± 1.14 | 1.45 ± 0.97 | 2.63 ± 1.08 | <0.0001 * |
| Glucose (mmol/L) | 4.86 ± 0.51 | 4.75 ± 0.49 | 5.16 ± 0.44 | <0.0001 * |
| Diagnosis of thyroid malignancy: | <0.0001 * | |||
| Before surgery | 317 (60.6) | 247 (66.4) | 70 (47.0) | |
| After surgery | 206 (39.4) | 125 (33.6) | 79 (53.0) | |
| Type of surgery: | <0.0001 * | |||
| Radical | 381 (72.8) | 291 (78.0) | 90 (60.0) | |
| Not radical | 142 (27.2) | 82 (22.0) | 60 (40.0) | |
| Reoperation needed: | 0.0001 * | |||
| No | 388 (74.2) | 294 (78.8) | 94 (62.7) | |
| Yes | 135 (25.8) | 79 (21.2) | 56 (37.3) | |
| pTNM stage: | 0.894 | |||
| I | 433 (82.8) | 307 (82.3) | 126 (84.0) | |
| II | 67 (12.8) | 50 (13.4) | 17 (11.3) | |
| III | 15 (2.9) | 10 (2.7) | 5 (3.3) | |
| IV | 8 (1.5) | 6 (1.6) | 2 (1.3) | |
| Tumor stage: | 0.012 * | |||
| pT1a | 209 (40.0) | 136 (36.5) | 73 (48.7) | |
| pT1b | 238 (45.5) | 181 (48.5) | 57 (38.0) | |
| pT2 | 61 (11.7) | 44 (11.8) | 17 (11.3) | |
| pT3 | 7 (1.3) | 7 (1.9) | 0 (0.0) | |
| pT4a | 3 (0.6) | 3 (0.8) | 0 (0.0) | |
| pT4b | 5 (0.9) | 2 (0.5) | 3 (2.0) | |
| Tumor size: | <0.0001 * | |||
| <5 mm | 89 (17.0) | 66 (17.7) | 24 (16.0) | |
| 5–10 mm | 120 (22.7) | 70 (18.7) | 49 (32.6) | |
| >10 mm | 314 (60.3) | 237 (63.6) | 77 (51.4) | |
| Lymph node metastasis: | 0.008 * | |||
| pN0 | 350 (66.9) | 266 (71.3) | 84 (56.0) | |
| pN1a | 145 (27.7) | 89 (23.9) | 56 (37.3) | |
| pN1b | 6 (1.1) | 3 (0.8) | 3 (2.0) | |
| pNx | 22 (4.2) | 15 (4.0) | 7 (4.7) | |
| Distant metastasis: | <0.0001 * | |||
| pM0 | 450 (86.0) | 337 (90.4) | 113 (75.3) | |
| pM1 | 19 (3.6) | 15 (4.0) | 4 (2.7) | |
| pMx | 54 (10.4) | 21 (5.6) | 33 (22.0) |
| Parameters | Total | Group1: BMI < 25 kg/m2 | Group2: BMI ≥ 25 kg/m2 | p-Value |
|---|---|---|---|---|
| (n = 523) | (n = 373) | (n = 150) | ||
| Microcalcification: | <0.0001 * | |||
| Yes | 299 (57.2) | 190 (50.9) | 109 (72.7) | |
| No | 224 (42.8) | 183 (49.1) | 41 (27.3) | |
| Echogenicity: | 0.032 * | |||
| Hyperechoic | 100 (19.1) | 80 (21.4) | 20 (13.3) | |
| Hypoechoic | 423 (80.9) | 293 (78.6) | 130 (86.7) | |
| Vascularity: | <0.0001 * | |||
| High | 269 (51.4) | 166 (44.5) | 103 (68.7) | |
| Low | 254 (48.6) | 207 (55.5) | 47 (31.3) | |
| Extrathyroidal extension: | <0.0001 * | |||
| Yes | 234 (44.7) | 131 (35.1) | 103 (68.7) | |
| No | 289 (55.3) | 242 (64.9) | 47 (31.3) | |
| Capsular invasion: | <0.044 * | |||
| Yes | 185 (35.4) | 122 (32.7) | 63 (42.0) | |
| No | 338 (64.6) | 251 (67.3) | 87 (58.0) | |
| Vascular invasion | 0.051 | |||
| Yes | 186 (35.6) | 123 (32.9) | 63 (42.0) | |
| No | 337 (64.4) | 250 (67.1) | 87 (58.0) | |
| Tumor shape | <0.0001 * | |||
| Regular | 255 (48.8) | 207 (55.5) | 48 (32.0) | |
| Irregular | 268 (51.2) | 166 (44.5) | 102 (68.0) | |
| Sharp margins | <0.0001 * | |||
| Yes | 250 (47.8) | 206 (55.2) | 44 (29.3) | |
| No | 273 (52.2) | 167 (44.8) | 106 (70.7) | |
| Diagnosed as multifocal: | <0.0001 * | |||
| No | 397 (75.9) | 349 (93.6) | 48 (32.0) | |
| yes | 126 (24.1) | 24 (6.4) | 102 (68.0) | |
| Diagnosed as bilateral: | <0.0001 * | |||
| No | 475 (90.8) | 370 (99.2) | 105 (70.0) | |
| Yes | 48 (9.2) | 3 (0.8) | 45 (30.0) | |
| Number of foci: | <0.0001 * | |||
| 1 | 397 (75.9) | 349 (93.6) | 48 (32.0) | |
| 2 | 102 (19.5) | 22 (5.9) | 80 (53.3) | |
| 3 | 24 (4.6) | 2 (0.5) | 22 (14.7) |
| PTC Severity Indicators | Univariable Logistic Regression Model | Multivariable Logistic Regression Model | ||||
|---|---|---|---|---|---|---|
| OR | ±95% CI | p-Value | OR | ±95% CI | p-Value | |
| Advanced pTNM stage (III + IV) | 1.09 | 0.43–2.72 | 0.849 | - | - | - |
| pT progression (3 + 4) | 0.61 | 0.17–2.21 | 0.452 | - | - | - |
| Lymph node metastasis (pN1) | 2.03 | 1.34–3.05 | <0.001 * | 1.41 | 0.86–2.31 | 0.168 |
| Distant metastasis (pM1) | 0.79 | 0.25–2.45 | 0.689 | - | - | - |
| Bilaterality | 52.85 | 16.05–173.90 | <0.0001 * | 22.76 | 6.39–81.08 | <0.0001 * |
| Multifocality | 30.90 | 18.0–52.9 | <0.0001 * | 20.07 | 9.54–42.24 | <0.0001 * |
| Microcalcifications | 2.56 | 1.69–3.87 | <0.0001 * | 1.65 | 0.99–2.75 | 0.051 |
| Hypoechogenicity | 1.77 | 1.04–3.02 | 0.034 * | 1.46 | 0.79–2.71 | 0.224 |
| High vascularity | 2.73 | 1.82–4.08 | <0.0001 * | 1.9 | 1.20–3.03 | 0.006 * |
| Capsular invasion | 1.49 | 1.00–2.20 | 0.045 * | 1.07 | 0.67–1.72 | 0.768 |
| Vascular invasion | 1.47 | 0.99–2.17 | 0.052 | 1.06 | 0.66–1.71 | 0.795 |
| Extrathyroidal extension | 4.04 | 2.69–6.07 | <0.0001 * | 2.34 | 1.45–3.76 | <0.001 * |
| Irregular tumor shape | 2.64 | 1.77–3.95 | <0.0001 * | 1.87 | 1.18–2.97 | 0.007 * |
| Sharp margins | 0.34 | 0.22–0.50 | <0.0001 * | 0.47 | 0.29–0.75 | 0.002 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaliszewski, K.; Diakowska, D.; Rzeszutko, M.; Rudnicki, J. Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer. J. Clin. Med. 2021, 10, 970. https://doi.org/10.3390/jcm10050970
Kaliszewski K, Diakowska D, Rzeszutko M, Rudnicki J. Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer. Journal of Clinical Medicine. 2021; 10(5):970. https://doi.org/10.3390/jcm10050970
Chicago/Turabian StyleKaliszewski, Krzysztof, Dorota Diakowska, Marta Rzeszutko, and Jerzy Rudnicki. 2021. "Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer" Journal of Clinical Medicine 10, no. 5: 970. https://doi.org/10.3390/jcm10050970
APA StyleKaliszewski, K., Diakowska, D., Rzeszutko, M., & Rudnicki, J. (2021). Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer. Journal of Clinical Medicine, 10(5), 970. https://doi.org/10.3390/jcm10050970







