Epidemiology of Posterior Cruciate Ligament Reconstructions in Italy: A 15-Year Study
Abstract
1. Introduction
2. Experimental Section
- -
- Diagnosis Code: 717.84 (old disruption of posterior cruciate ligament).
- -
- Treatment Code: 81.45 (other repairs of the cruciate ligaments).
Statistical Analysis
3. Results
3.1. Patients’ Demographics
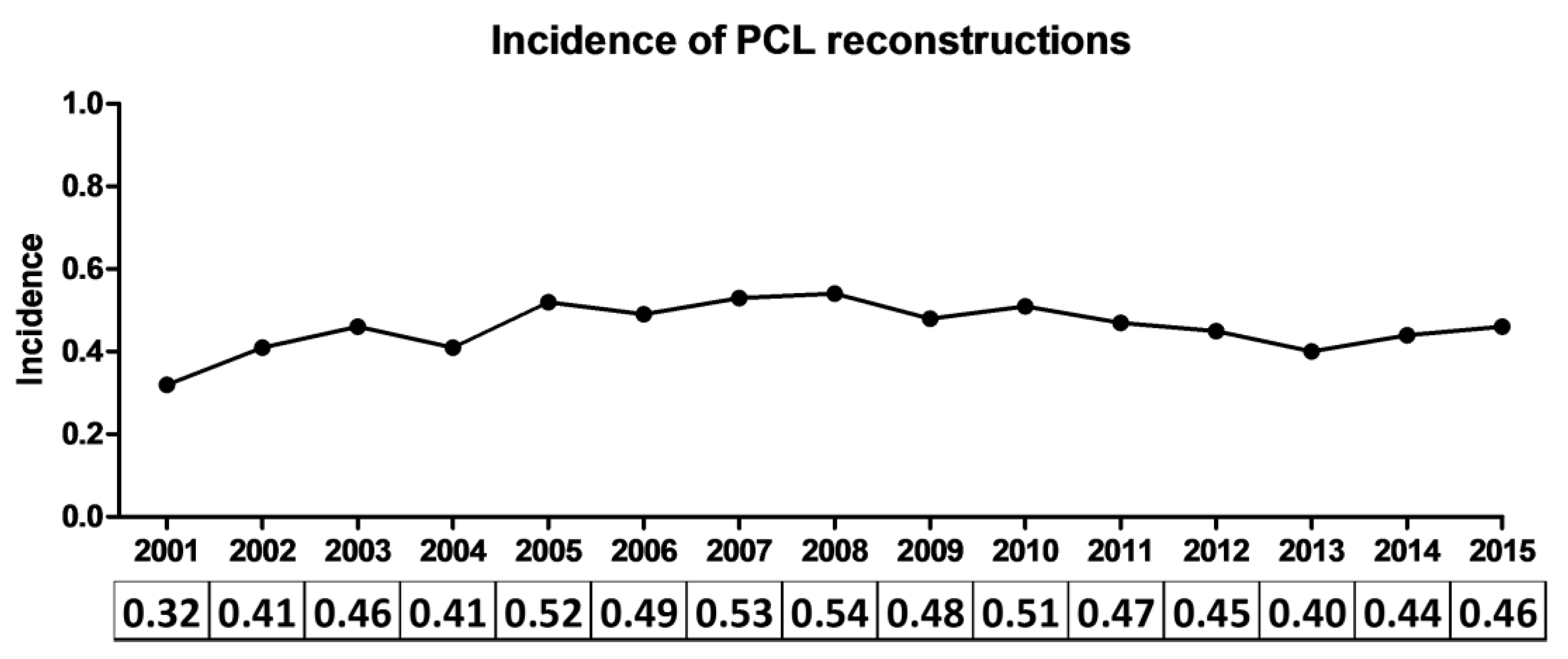
3.2. PCL Reconstruction Incidence
3.3. Length of Hospitalization and Total Expenditure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bedi, A.; Musahl, V.; Cowan, J.B. Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. J. Am. Acad. Orthop. Surg. 2016, 24, 277–289. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, C.M.; Civitarese, D.M.; Rasmussen, M.T.; LaPrade, R.F. Emerging Updates on the Posterior Cruciate Ligament: A Review of the Current Literature. Am. J. Sports Med. 2015, 43, 3077–3092. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, G.C.; Beck, J.D.; Edson, C.J. Current concepts review: The posterior cruciate ligament. J. Knee Surg. 2010, 23, 61–72. [Google Scholar] [CrossRef]
- Dennis, M.G.; Fox, J.A.; Alford, J.W.; Hayden, J.K.; Bach, B.R. Posterior cruciate ligament reconstruction: Current trends. J. Knee Surg. 2004, 17, 133–139. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fanelli, G.C. Knee Dislocation and Multiple Ligament Injuries of the Knee. Sports Med. Arthrosc. Rev. 2018, 26, 150–152. [Google Scholar] [CrossRef]
- Dick, R.; Ferrara, M.S.; Agel, J.; Courson, R.; Marshall, S.W.; Hanley, M.J.; Reifsteck, F. Descriptive Epidemiology of Collegiate Men’s Football Injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 Through 2003–2004. J. Athl. Train. 2007, 42, 221–233. [Google Scholar]
- Rothenberg, P.; Grau, L.; Kaplan, L.; Baraga, M.G. Knee Injuries in American Football: An Epidemiological Review. Am. J. Orthop. 2016, 45, 368–373. [Google Scholar]
- Dejour, H.; Walch, G.; Peyrot, J.; Eberhard, P. [The natural history of rupture of the posterior cruciate ligament]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1988, 74, 35–43. [Google Scholar]
- Parolie, J.M.; Bergfeld, J.A. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am. J. Sports Med. 1986, 14, 35–38. [Google Scholar] [CrossRef]
- Patel, D.V.; Allen, A.A.; Warren, R.F.; Wickiewicz, T.L.; Simonian, P.T. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: An intermediate-term follow-up study. HSS J. 2007, 3, 137–146. [Google Scholar] [CrossRef]
- Shelbourne, K.D.; Clark, M.; Gray, T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am. J. Sports Med. 2013, 41, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Shelbourne, K.D.; Davis, T.J.; Patel, D.V. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am. J. Sports Med. 1999, 27, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Boynton, M.D.; Tietjens, B.R. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am. J. Sports Med. 1996, 24, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Clancy, W.G.; Shelbourne, K.D.; Zoellner, G.B.; Keene, J.S.; Reider, B.; Rosenberg, T.D. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J. Bone Joint Surg. Am. 1983, 65, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Geissler, W.B.; Whipple, T.L. Intraarticular abnormalities in association with posterior cruciate ligament injuries. Am. J. Sports Med. 1993, 21, 846–849. [Google Scholar] [CrossRef]
- Keller, P.M.; Shelbourne, K.D.; McCarroll, J.R.; Rettig, A.C. Nonoperatively treated isolated posterior cruciate ligament injuries. Am. J. Sports Med. 1993, 21, 132–136. [Google Scholar] [CrossRef]
- Sanders, T.L.; Pareek, A.; Barrett, I.J.; Kremers, H.M.; Bryan, A.J.; Stuart, M.J.; Levy, B.A.; Krych, A.J. Incidence and long-term follow-up of isolated posterior cruciate ligament tears. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3017–3023. [Google Scholar] [CrossRef]
- Wang, S.-H.; Chien, W.-C.; Chung, C.-H.; Wang, Y.-C.; Lin, L.-C.; Pan, R.-Y. Long-term results of posterior cruciate ligament tear with or without reconstruction: A nationwide, population-based cohort study. PLoS ONE 2018, 13, e0205118. [Google Scholar] [CrossRef]
- Lind, M.; Nielsen, T.G.; Behrndtz, K. Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: Results from the Danish Knee Ligament Reconstruction Registry. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1190–1196. [Google Scholar] [CrossRef]
- Fanelli, G.C.; Edson, C.J. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy 1995, 11, 526–529. [Google Scholar] [CrossRef]
- Schlumberger, M.; Schuster, P.; Eichinger, M.; Mayer, P.; Mayr, R.; Immendörfer, M.; Richter, J. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg. Sports Traumatol. Arthrosc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Schulz, M.S.; Russe, K.; Weiler, A.; Eichhorn, H.J.; Strobel, M.J. Epidemiology of posterior cruciate ligament injuries. Arch. Orthop. Trauma Surg. 2003, 123, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Senter, C.; Hame, S.L. Biomechanical Analysis of Tibial Torque and Knee Flexion Angle. Sports Med. 2006, 36, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Janousek, A.T.; Jones, D.G.; Clatworthy, M.; Higgins, L.D.; Fu, F.H. Posterior cruciate ligament injuries of the knee joint. Sports Med. 1999, 28, 429–441. [Google Scholar] [CrossRef] [PubMed]
- Majewski, M.; Susanne, H.; Klaus, S. Epidemiology of athletic knee injuries: A 10-year study. Knee 2006, 13, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Logan, C.A.; Beaulieu-Jones, B.R.; Sanchez, G.; Chahla, J.; Kennedy, N.I.; Cinque, M.E.; LaPrade, R.F.; Whalen, J.M.; Vopat, B.G.; Price, M.D.; et al. Posterior Cruciate Ligament Injuries of the Knee at the National Football League Combine: An Imaging and Epidemiology Study. Arthroscopy 2018, 34, 681–686. [Google Scholar] [CrossRef]
- Owesen, C.; Sandven-Thrane, S.; Lind, M.; Forssblad, M.; Granan, L.-P.; Årøen, A. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2384–2391. [Google Scholar] [CrossRef]
- Swenson, D.M.; Collins, C.L.; Best, T.M.; Flanigan, D.C.; Fields, S.K.; Comstock, R.D. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med. Sci. Sports Exerc. 2013, 45, 462–469. [Google Scholar] [CrossRef]
- Popolazione Residente al 1° Gennaio. Available online: http://dati.istat.it/Index.aspx?QueryId=18460 (accessed on 1 December 2020).
- Ministero del Lavoro, Della Salute E Delle Politiche Sociali Aggiornamento dei Sistemi di Classificazione Adottati per la Codifica Delle Informazioni Cliniche Contenute Nella Scheda di Dimissione Ospedaliera e per la Remunerazione Delle Prestazioni Ospedaliere. 2008. Available online: https://www.gazzettaufficiale.it/eli/id/2009/03/09/09A02110/sg (accessed on 1 December 2020).
- R Core Team. R: A Language and Environment for Statistical Computing 2013. Available online: https://www.R-project.org/ (accessed on 1 December 2020).
- Hsuan, H.-F.; Lin, Y.-C.; Chiu, C.-H.; Ni Mhuircheartaigh, J.; Juan, Y.-H.; Chan, Y.-S.; Wu, J.S. Posterior cruciate ligament tears in Taiwan: An analysis of 140 surgically treated cases. Clin. Imaging 2016, 40, 856–860. [Google Scholar] [CrossRef]
- Sutton, K.M.; Bullock, J.M. Anterior cruciate ligament rupture: Differences between males and females. J. Am. Acad. Orthop. Surg. 2013, 21, 41–50. [Google Scholar] [CrossRef]
- Battaglia, T.C.; Mulhall, K.J.; Miller, M.D. Chapter 53—Posterior Cruciate Ligament. In Clinical Sports Medicine; Johnson, D.L., Mair, S.D., Eds.; Mosby: Philadelphia, CA, USA, 2006; pp. 547–559. ISBN 978-0-323-02588-1. [Google Scholar]
- Kozanek, M.; Fu, E.C.; Van de Velde, S.K.; Gill, T.J.; Li, G. Posterolateral structures of the knee in posterior cruciate ligament deficiency. Am. J. Sports Med. 2009, 37, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Logan, M.; Williams, A.; Lavelle, J.; Gedroyc, W.; Freeman, M. The effect of posterior cruciate ligament deficiency on knee kinematics. Am. J. Sports Med. 2004, 32, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, G.C.; Fanelli, D.G. Knee Dislocations and PCL-Based Multiligament Knee Injuries in Patients Aged 18 Years and Younger: Surgical Technique and Outcomes. J. Knee Surg. 2016, 29, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, O.G.; Faunø, P.; Christiansen, S.E.; Lind, M. Posterior cruciate ligament reconstruction in skeletal immature children. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3901–3905. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, M. Reducing Length of Stay by Enhancing Patients’ Discharge: A Practical Approach to Improve Hospital Efficiency. Stud. Health Technol. Inform. 2017, 238, 157–160. [Google Scholar] [PubMed]
- Boddapati, V.; Fu, M.C.; Nwachukwu, B.U.; Camp, C.L.; Spiker, A.M.; Williams, R.J.; Ranawat, A.S. Procedure Length Is Independently Associated with Overnight Hospital Stay and 30-Day Readmission Following Anterior Cruciate Ligament Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 432–438. [Google Scholar] [CrossRef] [PubMed]
| Total Procedures | 4029 |
| Age (median; interquartile range) (in years) | 30 (22–39) |
| Males (n; %) | 3393 (84.3%) |
| Females (n; %) | 636 (15.7%) |
| Ratio (M:F) | 5.3 |
| Geographic distribution (n; %) | |
| North | 2573 (63.9%) |
| Central | 951 (23.6%) |
| South | 505 (12.5%) |
| Associated lesions (%) 1 | |
| None (Isolated PCL injury) | 39.7% |
| ACL injury | 31.1% |
| Medial meniscus injury | 13.2% |
| Sprain of cruciate ligament of the knee | 7.8% |
| Lateral collateral ligament lesion | 5.2% |
| Medial collateral ligament lesion | 3.9% |
| Lateral meniscus injury | 2.8% |
| Other | 29.7% |
| Year | LOS (Median; IQR) | Total Expenditure |
|---|---|---|
| 2001 | 5 (3–8) | €461,962.00 |
| 2002 | 4 (3–6) | €569,778.00 |
| 2003 | 4 (3–6) | €639,423.00 |
| 2004 | 3 (2–6) | €575,713.00 |
| 2005 | 3 (2–5) | €726,214.00 |
| 2006 | 3 (2–4) | €670,852.00 |
| 2007 | 3 (2–4) | €716,043.00 |
| 2008 | 3 (2–4.5) | €744,411.00 |
| 2009 | 2 (2–4) | €663,232.00 |
| 2010 | 3 (2–4) | €708,769.00 |
| 2011 | 2 (2–4) | €627,971.00 |
| 2012 | 2 (2–4) | €599,268.00 |
| 2013 | 2 (2–4) | €541,446.00 |
| 2014 | 2 (2–3) | €595,158.00 |
| 2015 | 2 (1–3) | €462,680.00 |
| Median (range): 3 (2–4) | Total: € 9,302,920.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Viganò, M.; Candela, V.; de Girolamo, L.; Cella, E.; Thiebat, G.; Salvatore, G.; Ciccozzi, M.; Denaro, V. Epidemiology of Posterior Cruciate Ligament Reconstructions in Italy: A 15-Year Study. J. Clin. Med. 2021, 10, 499. https://doi.org/10.3390/jcm10030499
Longo UG, Viganò M, Candela V, de Girolamo L, Cella E, Thiebat G, Salvatore G, Ciccozzi M, Denaro V. Epidemiology of Posterior Cruciate Ligament Reconstructions in Italy: A 15-Year Study. Journal of Clinical Medicine. 2021; 10(3):499. https://doi.org/10.3390/jcm10030499
Chicago/Turabian StyleLongo, Umile Giuseppe, Marco Viganò, Vincenzo Candela, Laura de Girolamo, Eleonora Cella, Gabriele Thiebat, Giuseppe Salvatore, Massimo Ciccozzi, and Vincenzo Denaro. 2021. "Epidemiology of Posterior Cruciate Ligament Reconstructions in Italy: A 15-Year Study" Journal of Clinical Medicine 10, no. 3: 499. https://doi.org/10.3390/jcm10030499
APA StyleLongo, U. G., Viganò, M., Candela, V., de Girolamo, L., Cella, E., Thiebat, G., Salvatore, G., Ciccozzi, M., & Denaro, V. (2021). Epidemiology of Posterior Cruciate Ligament Reconstructions in Italy: A 15-Year Study. Journal of Clinical Medicine, 10(3), 499. https://doi.org/10.3390/jcm10030499








