Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) with a New Pathogenic Variant in TNFRSF1A Gene in a Family of the Adult Male with Renal AA Amyloidosis—Diagnostic and Therapeutic Challenge for Clinicians
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods of Molecular Analysis
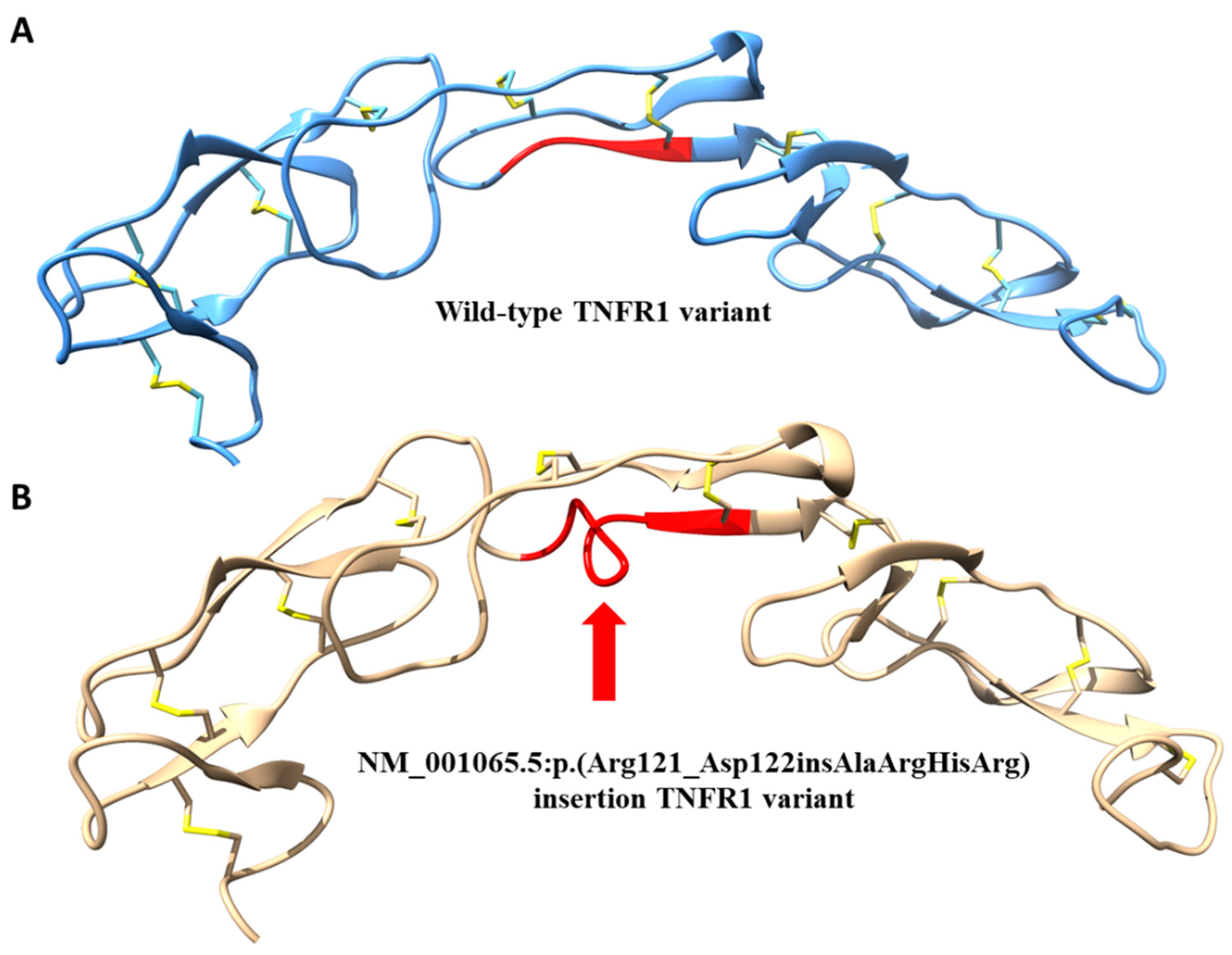
2.3. 3D Protein Modeling
3. Results
3.1. Patients
3.1.1. Patient 1—Proband
3.1.2. Remaining Patients
Patient 2
Patient 3
Patient 4
3.2. Genetic Results
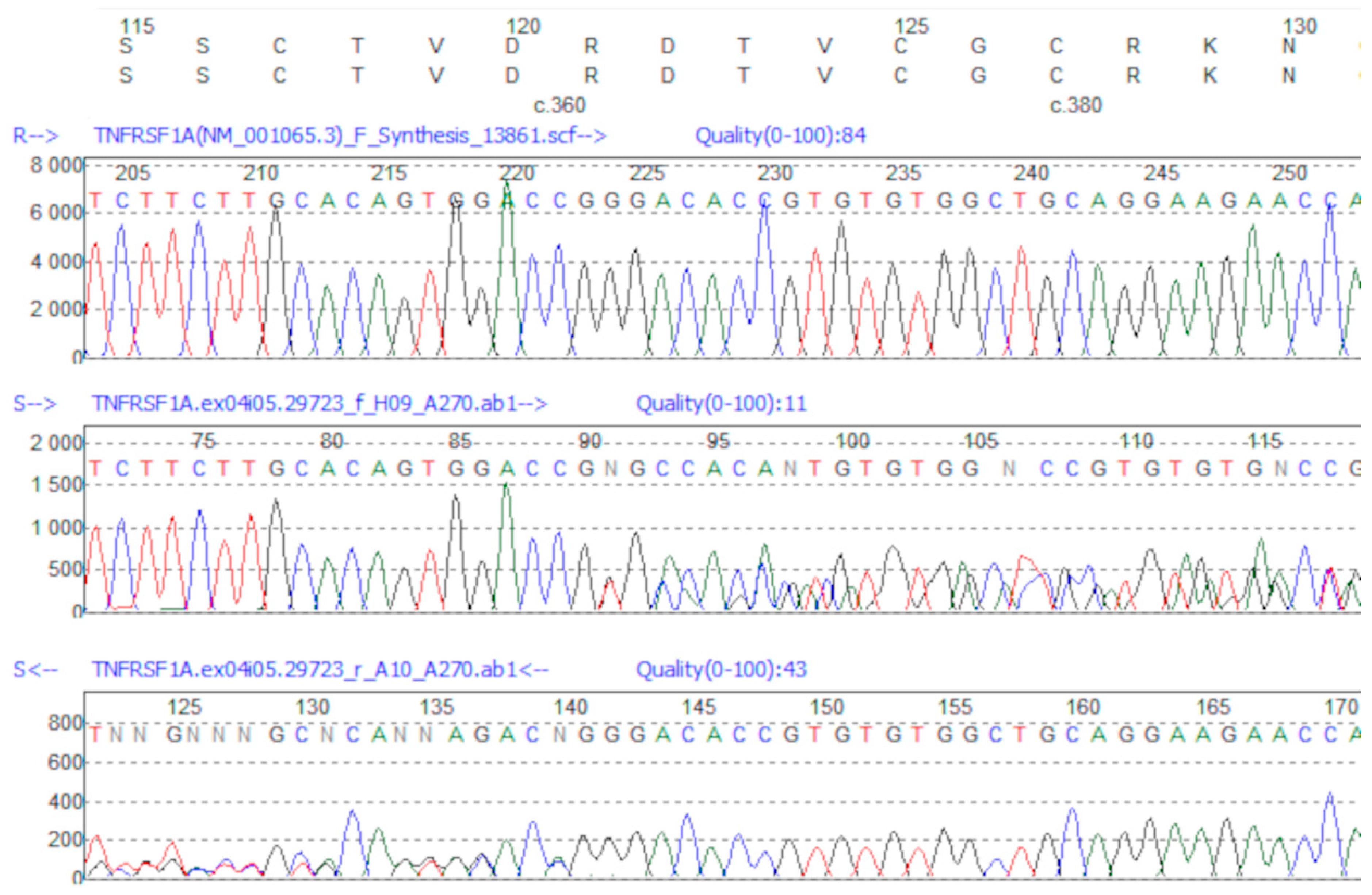
Genetic Variant Identification
3.3. Management
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDermott, M.F.; Aksentijevich, I.; Galon, J.; McDermott, E.M.; Ogunkolade, B.W.; Centola, M.; Mansfield, E.; Gadina, M.; Karenko, L.; Pettersson, T.; et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell 1999, 97, 133–144. [Google Scholar] [CrossRef]
- Hull, K.M.; Drewe, E.; Aksentijevich, I.; Singh, H.K.; Wong, K.; McDermott, E.M.; Dean, J.; Powell, R.J.; Kastner, D.L. The TNF receptor-associated periodic syndrome (TRAPS): Emerging concepts of an autoinflammatory disorder. Medicine (Baltimore) 2002, 81, 349–368. [Google Scholar] [CrossRef] [PubMed]
- Aksentijevich, I.; Galon, J.; Soares, M.; Mansfield, E.; Hull, K.; Oh, H.H.; Goldbach-Mansky, R.; Dean, J.; Athreya, B.; Reginato, A.J.; et al. The tumor-necrosis-factor receptor-associated periodic syndrome: New mutations in TNFRSF1A, ancestral origins, genotype-phenotype studies, and evidence for further genetic heterogeneity of periodic fevers. Am. J. Hum. Genet. 2001, 69, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Toro, J.R.; Aksentijevich, I.; Hull, K.; Dean, J.; Kastner, D.L. Tumor necrosis factor receptor-associated periodic syndrome: A novel syndrome with cutaneous manifestations. Arch. Dermatol. 2000, 136, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Lachmann, H.J.; Papa, R.; Gerhold, K.; Obici, L.; Touitou, I.; Cantarini, L.; Frenkel, J.; Anton, J.; Kone-Paut, I.; Cattalini, M.; et al. The phenotype of TNF receptor-associated autoinflammatory syndrome (TRAPS) at presentation: A series of 158 cases from the Eurofever/EUROTRAPS international registry. Ann. Rheum. Dis. 2014, 73, 2160–2167. [Google Scholar] [CrossRef]
- Cudrici, C.; Deuitch, N.; Aksentijevich, I. Revisiting TNF Receptor-Associated Periodic Syndrome (TRAPS): Current Perspectives. Int. J. Mol. Sci. 2020, 21, 3263. [Google Scholar] [CrossRef]
- Brunger, A.F.; Nienhuis, H.L.A.; Bijzet, J.; Hazenberg, B.P.C. Causes of AA amyloidosis: A systematic review. Amyloid 2020, 27, 1–12. [Google Scholar] [CrossRef]
- Sarihan, I.; Caliskan, Y.; Mirioglu, S.; Ozluk, Y.; Senates, B.; Seyahi, N.; Basturk, T.; Yildiz, A.; Kilicaslan, I.; Sever, M.S. Amyloid A Amyloidosis After Renal Transplantation: An Important Cause of Mortality. Transplantation 2020, 104, 1703–1711. [Google Scholar] [CrossRef]
- Ter Haar, N.; Lachmann, H.; Ozen, S.; Woo, P.; Uziel, Y.; Modesto, C.; Kone-Paut, I.; Cantarini, L.; Insalaco, A.; Neven, B.; et al. Treatment of autoinflammatory diseases: Results from the Eurofever Registry and a literature review. Ann. Rheum. Dis. 2013, 72, 678–685. [Google Scholar] [CrossRef]
- Ozen, S.; Demir, S. Monogenic Periodic Fever Syndromes: Treatment Options for the Pediatric Patient. Paediatr. Drugs 2017, 19, 303–311. [Google Scholar] [CrossRef]
- Li, H.; Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 2010, 26, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Bousfiha, A.; Jeddane, L.; Al-Herz, W.; Ailal, F.; Casanova, J.L.; Chatila, T.; Conley, M.E.; Cunningham-Rundles, C.; Etzioni, A.; Franco, J.L.; et al. The 2015 IUIS Phenotypic Classification for Primary Immunodeficiencies. J. Clin. Immunol. 2015, 35, 727–738. [Google Scholar] [CrossRef] [PubMed]
- 1000Genomes. Available online: http://www.l000genomes.org (accessed on 19 October 2016).
- Exome Variant Server. Available online: http://evs.gs.washington.edu/EVS (accessed on 19 October 2016).
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Sali, A.; Blundell, T.L. Comparative protein modelling by satisfaction of spatial restraints. J. Mol. Biol. 1993, 234, 779–815. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.Y.; Sali, A. Statistical potential for assessment and prediction of protein structures. Protein Sci. 2006, 15, 2507–2524. [Google Scholar] [CrossRef]
- Greco, E.; Aita, A.; Galozzi, P.; Gava, A.; Sfriso, P.; Negm, O.H.; Tighe, P.; Caso, F.; Navaglia, F.; Dazzo, E.; et al. The novel S59P mutation in the TNFRSF1A gene identified in an adult onset TNF receptor associated periodic syndrome (TRAPS) constitutively activates NF-kappaB pathway. Arthritis Res. Ther. 2015, 17, 93. [Google Scholar] [CrossRef]
- Tsuji, S.; Matsuzaki, H.; Iseki, M.; Nagasu, A.; Hirano, H.; Ishihara, K.; Ueda, N.; Honda, Y.; Horiuchi, T.; Nishikomori, R.; et al. Functional analysis of a novel G87V TNFRSF1A mutation in patients with TNF receptor-associated periodic syndrome. Clin. Exp. Immunol. 2019, 198, 416–429. [Google Scholar] [CrossRef]
- Federici, S.; Sormani, M.P.; Ozen, S.; Lachmann, H.J.; Amaryan, G.; Woo, P.; Kone-Paut, I.; Dewarrat, N.; Cantarini, L.; Insalaco, A.; et al. Evidence-based provisional clinical classification criteria for autoinflammatory periodic fevers. Ann. Rheum. Dis. 2015, 74, 799–805. [Google Scholar] [CrossRef]
- Gattorno, M.; Hofer, M.; Federici, S.; Vanoni, F.; Bovis, F.; Aksentijevich, I.; Anton, J.; Arostegui, J.I.; Barron, K.; Ben-Cherit, E.; et al. Classification criteria for autoinflammatory recurrent fevers. Ann. Rheum. Dis. 2019, 78, 1025–1032. [Google Scholar] [CrossRef]
- Federici, S.; Vanoni, F.; Ben-Chetrit, E.; Cantarini, L.; Frenkel, J.; Goldbach-Mansky, R.; Gul, A.; Hoffman, H.; Kone-Paut, I.; Kuemmerle-Deschner, J.; et al. An International Delphi Survey for the Definition of New Classification Criteria for Familial Mediterranean Fever, Mevalonate Kinase Deficiency, TNF Receptor-associated Periodic Fever Syndromes, and Cryopyrin-associated Periodic Syndrome. J. Rheumatol. 2019, 46, 429–436. [Google Scholar] [CrossRef]
- Rowczenio, D.M.; Lachmann, H.J. How to prescribe a genetic test for the diagnosis of autoinflammatory diseases? Presse Med. 2019, 48, e49. [Google Scholar] [CrossRef] [PubMed]
- Rigante, D.; Frediani, B.; Cantarini, L. A Comprehensive Overview of the Hereditary Periodic Fever Syndromes. Clin. Rev. Allergy Immunol. 2018, 54, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Drewe, E.; McDermott, E.M.; Powell, R.J. Treatment of the nephrotic syndrome with etanercept in patients with the tumor necrosis factor receptor-associated periodic syndrome. N. Engl. J. Med. 2000, 343, 1044–1045. [Google Scholar] [CrossRef] [PubMed]
- Papa, R.; Lane, T.; Minden, K.; Touitou, I.; Cantarini, L.; Cattalini, M.; Obici, L.; Jansson, A.F.; Belot, A.; Frenkel, J.; et al. INSAID Variant Classification and Eurofever Criteria Guide Optimal Treatment Strategy in Patients with TRAPS: Data from the Eurofever Registry. J. Allergy Clin. Immunol. Pract. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ozen, S.; Kuemmerle-Deschner, J.B.; Cimaz, R.; Livneh, A.; Quartier, P.; Kone-Paut, I.; Zeft, A.; Spalding, S.; Gul, A.; Hentgen, V.; et al. International Retrospective Chart Review of Treatment Patterns in Severe Familial Mediterranean Fever, Tumor Necrosis Factor Receptor-Associated Periodic Syndrome, and Mevalonate Kinase Deficiency/Hyperimmunoglobulinemia D Syndrome. Arthritis Care Res. (Hoboken) 2017, 69, 578–586. [Google Scholar] [CrossRef]
- Gentileschi, S.; Rigante, D.; Vitale, A.; Sota, J.; Frediani, B.; Galeazzi, M.; Cantarini, L. Efficacy and safety of anakinra in tumor necrosis factor receptor-associated periodic syndrome (TRAPS) complicated by severe renal failure: A report after long-term follow-up and review of the literature. Clin. Rheumatol. 2017, 36, 1687–1690. [Google Scholar] [CrossRef]
- La Torre, F.; Caparello, M.C.; Cimaz, R. Canakinumab for the treatment of TNF-receptor associated periodic syndrome. Expert Rev. Clin. Immunol. 2017, 13, 513–523. [Google Scholar] [CrossRef]
- De Benedetti, F.; Gattorno, M.; Anton, J.; Ben-Chetrit, E.; Frenkel, J.; Hoffman, H.M.; Kone-Paut, I.; Lachmann, H.J.; Ozen, S.; Simon, A.; et al. Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes. N. Engl. J. Med. 2018, 378, 1908–1919. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zegarska, J.; Wiesik-Szewczyk, E.; Hryniewiecka, E.; Wolska-Kusnierz, B.; Soldacki, D.; Kacprzak, M.; Sobczynska-Tomaszewska, A.; Czerska, K.; Siedlecki, P.; Jahnz-Rozyk, K.; et al. Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) with a New Pathogenic Variant in TNFRSF1A Gene in a Family of the Adult Male with Renal AA Amyloidosis—Diagnostic and Therapeutic Challenge for Clinicians. J. Clin. Med. 2021, 10, 465. https://doi.org/10.3390/jcm10030465
Zegarska J, Wiesik-Szewczyk E, Hryniewiecka E, Wolska-Kusnierz B, Soldacki D, Kacprzak M, Sobczynska-Tomaszewska A, Czerska K, Siedlecki P, Jahnz-Rozyk K, et al. Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) with a New Pathogenic Variant in TNFRSF1A Gene in a Family of the Adult Male with Renal AA Amyloidosis—Diagnostic and Therapeutic Challenge for Clinicians. Journal of Clinical Medicine. 2021; 10(3):465. https://doi.org/10.3390/jcm10030465
Chicago/Turabian StyleZegarska, Jolanta, Ewa Wiesik-Szewczyk, Ewa Hryniewiecka, Beata Wolska-Kusnierz, Dariusz Soldacki, Magdalena Kacprzak, Agnieszka Sobczynska-Tomaszewska, Kamila Czerska, Pawel Siedlecki, Karina Jahnz-Rozyk, and et al. 2021. "Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) with a New Pathogenic Variant in TNFRSF1A Gene in a Family of the Adult Male with Renal AA Amyloidosis—Diagnostic and Therapeutic Challenge for Clinicians" Journal of Clinical Medicine 10, no. 3: 465. https://doi.org/10.3390/jcm10030465
APA StyleZegarska, J., Wiesik-Szewczyk, E., Hryniewiecka, E., Wolska-Kusnierz, B., Soldacki, D., Kacprzak, M., Sobczynska-Tomaszewska, A., Czerska, K., Siedlecki, P., Jahnz-Rozyk, K., Bernatowska, E., Zagozdzon, R., & Paczek, L. (2021). Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) with a New Pathogenic Variant in TNFRSF1A Gene in a Family of the Adult Male with Renal AA Amyloidosis—Diagnostic and Therapeutic Challenge for Clinicians. Journal of Clinical Medicine, 10(3), 465. https://doi.org/10.3390/jcm10030465





