Applications of Wearable Technology in a Real-Life Setting in People with Knee Osteoarthritis: A Systematic Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Questions
2.2. Eligibility Criteria
2.3. Information Sources and Search
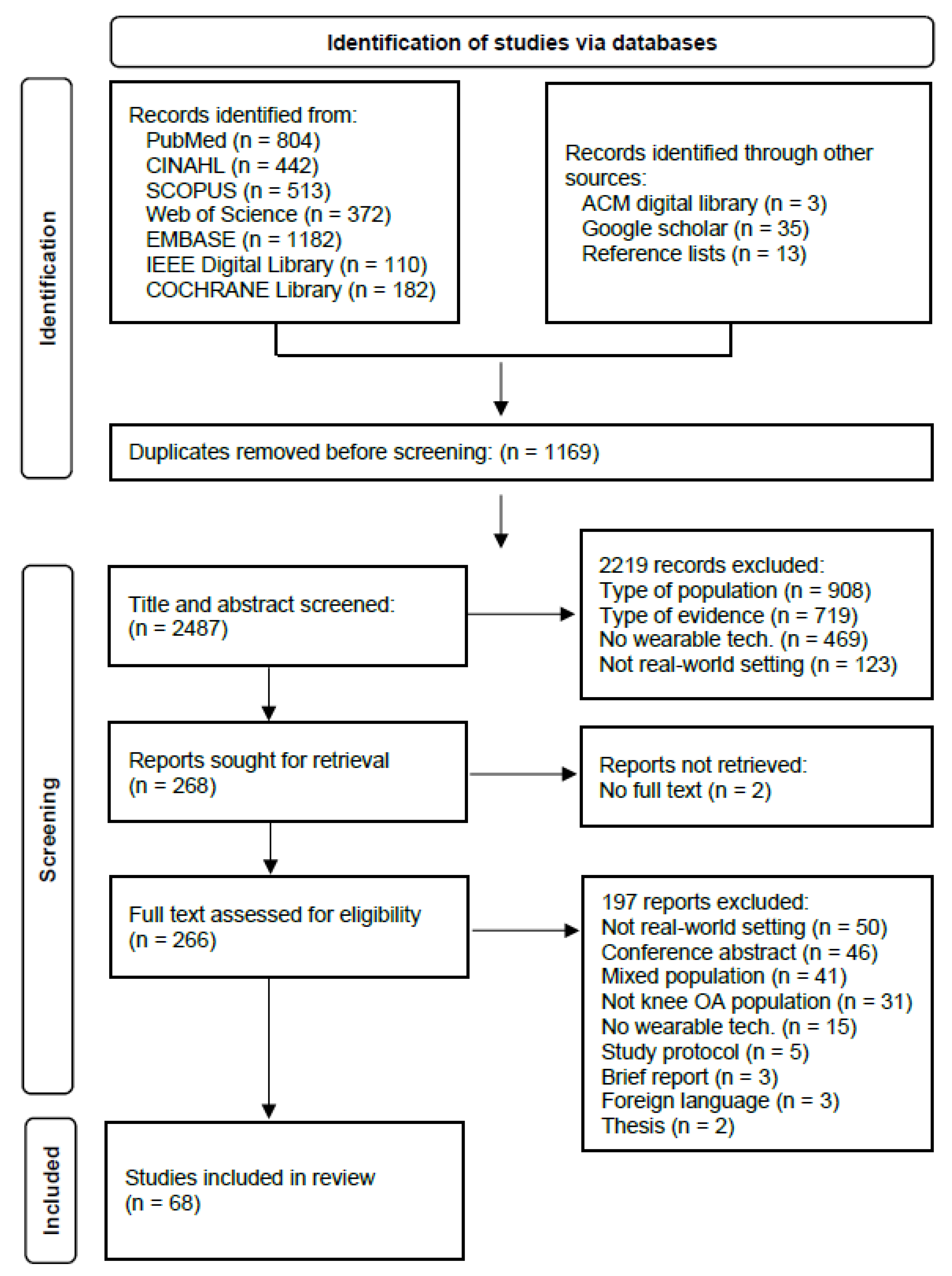
2.4. Study Selection
2.5. Data Extraction
2.6. Data Synthesis
3. Results
3.1. General Study and Population Details
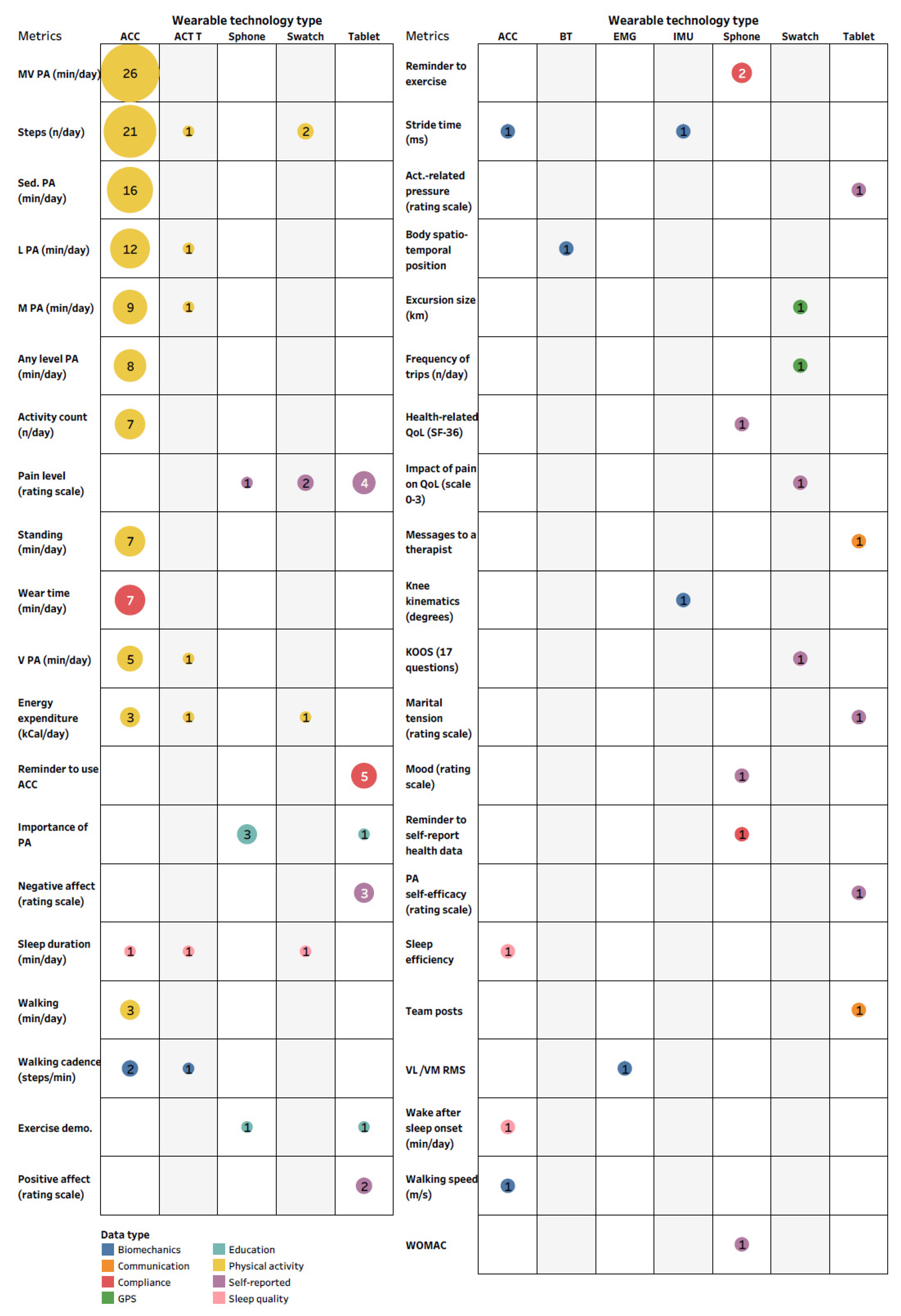
3.2. Wearable Technology
3.3. Applications of Wearable Technology
3.4. Facilitators and Barriers to Feasibility of Using Wearable Technology
4. Discussion
4.1. Applications of Wearable Technology in Knee OA
4.2. Facilitators and Barriers to Feasibility of Using Wearable Technology in a Real-World Setting
4.3. Recommendations for Future Research
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bijlsma, J.W.; Berenbaum, F.; Lafeber, F.P. Osteoarthritis: An update with relevance for clinical practice. Lancet 2011, 377, 2115–2126. [Google Scholar] [CrossRef]
- Oliveria, S.A.; Felson, D.; Reed, J.I.; Cirillo, P.A.; Walker, A.M. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995, 38, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Alhambra, D.; Judge, A.; Javaid, M.; Cooper, C.; Diez-Perez, A.; Arden, N.K. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: Influences of age, gender and osteoarthritis affecting other joints. Ann. Rheum. Dis. 2013, 73, 1659–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salmon, J.; Rat, A.; Sellam, J.; Michel, M.; Eschard, J.; Guillemin, F.; Jolly, D.; Fautrel, B. Economic impact of lower-limb osteoarthritis worldwide: A systematic review of cost-of-illness studies. Osteoarthr. Cartil. 2016, 24, 1500–1508. [Google Scholar] [CrossRef] [Green Version]
- Hunter, D.J.; Schofield, D.; Callander, E. The individual and socioeconomic impact of osteoarthritis. Nat. Rev. Rheumatol. 2014, 10, 437–441. [Google Scholar] [CrossRef]
- Cui, A.; Li, H.; Wang, D.; Zhong, J.; Chen, Y.; Lu, H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine 2020, 29–30, 100587. [Google Scholar] [CrossRef]
- NHS. GP_APPT_Publication_May_2020. 30 Jun 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/may-2020# (accessed on 22 November 2021).
- Kobsar, D.; Masood, Z.; Khan, H.; Khalil, N.; Kiwan, M.Y.; Ridd, S.; Tobis, M. Wearable Inertial Sensors for Gait Analysis in Adults with Osteoarthritis—A Scoping Review. Sensors 2020, 20, 7143. [Google Scholar] [CrossRef]
- Small, S.R.; Bullock, G.S.; Khalid, S.; Barker, K.; Trivella, M.; Price, A.J. Current clinical utilisation of wearable motion sensors for the assessment of outcome following knee arthroplasty: A scoping review. BMJ Open 2019, 9, e033832. [Google Scholar] [CrossRef] [Green Version]
- Kirk, S. The Wearables Revolution: Is Standardization a Help or a Hindrance?: Mainstream technology or just a passing phase? IEEE Consum. Electron. Mag. 2014, 3, 45–50. [Google Scholar] [CrossRef]
- Fogel, A.L.; Kvedar, J.C. Artificial intelligence powers digital medicine. NPJ Digit. Med. 2018, 1, 5. [Google Scholar] [CrossRef]
- Matthew-Maich, N.; Harris, L.; Ploeg, J.; Markle-Reid, M.; Valaitis, R.; Ibrahim, S.; Gafni, A.; Isaacs, S. Designing, Implementing, and Evaluating Mobile Health Technologies for Managing Chronic Conditions in Older Adults: A Scoping Review. JMIR mHealth uHealth 2016, 4, e29. [Google Scholar] [CrossRef]
- Sliepen, M.; Lipperts, M.; Tjur, M.; Mechlenburg, I. Use of accelerometer-based activity monitoring in orthopaedics: Benefits, impact and practical considerations. EFORT Open Rev. 2019, 4, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Kvedar, J.; Coye, M.J.; Everett, W. Connected Health: A Review of Technologies And Strategies To Improve Patient Care With Telemedicine And Telehealth. Health Aff. 2014, 33, 194–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sliepen, M.; Brandes, M.; Rosenbaum, D. Current Physical Activity Monitors in Hip and Knee Osteoarthritis: A Review. Arthritis Rheum. 2017, 69, 1460–1466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, K.D.; Lo, G.; Abbate, L.M.; Floegel, T.A.; Lindquist, J.H.; Coffman, C.; Oddone, E.Z.; Taylor, S.S.; Hall, K. Composite measures of physical activity and pain associate better with functional assessments than pain alone in knee osteoarthritis. Clin. Rheumatol. 2019, 38, 2241–2247. [Google Scholar] [CrossRef]
- Bartholdy, C.; Bliddal, H.; Henriksen, M. Effectiveness of text messages for decreasing inactive behaviour in patients with knee osteoarthritis: A pilot randomised controlled study. Pilot Feasibility Stud. 2019, 5, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Chang, A.H.; Lee, J.; Song, J.; Price, L.L.; Lee, A.C.; Reid, K.F.; Fielding, R.A.; Driban, J.B.; Harvey, W.C.; Wang, C. Association between Pre-intervention Physical Activity Level and Treatment Response to Exercise Therapy in Persons with Knee Osteoarthritis—An Exploratory Study. ACR Open Rheumatol. 2019, 1, 104–112. [Google Scholar] [CrossRef] [Green Version]
- Chmelo, E.; Nicklas, B.; Davis, C.; Miller, G.D.; Legault, C.; Messier, S. Physical Activity and Physical Function in Older Adults With Knee Osteoarthritis. J. Phys. Act. Health 2013, 10, 777–783. [Google Scholar] [CrossRef]
- Daugaard, R.; Tjur, M.; Sliepen, M.; Lipperts, M.; Grimm, B.; Mechlenburg, I. Are patients with knee osteoarthritis and patients with knee joint replacement as physically active as healthy persons? J. Orthop. Transl. 2018, 14, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Dessery, Y.; Belzile, L.; Turmel, S.; Doré, J.; Diallo, B.; Corbeil, P. Modulation of Physical Activity to Optimize Pain Sensation following an Intra-Articular Corticosteroid Injection in Patients with Knee Osteoarthritis. Sci. World J. 2014, 2014, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Maio, S.; Keller, J.; Job, V.; Felsenberg, D.; Ertel, W.; Schwarzer, R.; Knoll, N. Health Demands Moderate the Link Between Willpower Beliefs and Physical Activity in Patients with Knee Osteoarthritis. Int. J. Behav. Med. 2020, 27, 406–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Draper, D.; Klyve, D.; Ortiz, R.; Best, T.M. Effect of low-intensity long-duration ultrasound on the symptomatic relief of knee osteoarthritis: A randomized, placebo-controlled double-blind study. J. Orthop. Surg. Res. 2018, 13, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Fary, R.E.; Carroll, G.J.; Briffa, T.G.; Briffa, N.K. The effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: Results of a double-blind, randomized, placebo-controlled, repeated-measures trial. Arthritis Rheum. 2011, 63, 1333–1342. [Google Scholar] [CrossRef] [Green Version]
- Fawole, H.O.; Dell’Isola, A.; Steultjens, M.P.; Riskowski, J.L.; Chastin, S.F.M. Temporal associations between physical activity, mental activity and fatigue dimensions in knee osteoarthritis: An exploratory intensive longitudinal study. Fatigue Biomed. Health Behav. 2020, 8, 32–48. [Google Scholar] [CrossRef]
- Gilbert, A.L.; Lee, J.; Ehrlich-Jones, L.; Semanik, P.A.; Song, J.; Pellegrini, C.A.; Pt, D.P.; Dunlop, D.D.; Chang, R.W. A randomized trial of a motivational interviewing intervention to increase lifestyle physical activity and improve self-reported function in adults with arthritis. Semin. Arthritis Rheum. 2017, 47, 732–740. [Google Scholar] [CrossRef]
- Kahn, T.L.; Schwarzkopf, R. Do Total Knee Arthroplasty Patients Have a Higher Activity Level Compared to Patients with Osteoarthritis? Geriatr. Orthop. Surg. Rehabil. 2016, 7, 142–147. [Google Scholar] [CrossRef]
- Lee, J.; Chang, R.W.; Ehrlich-Jones, L.; Kwoh, C.K.; Nevitt, M.; Semanik, P.A.; Sharma, L.; Sohn, M.-W.; Song, J.; Dunlop, D.D. Sedentary Behavior and Physical Function: Objective Evidence from the Osteoarthritis Initiative. Arthritis Rheum. 2014, 67, 366–373. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Song, J.; Hootman, J.M.; Semanik, P.A.; Chang, R.W.; Sharma, L.; Van Horn, L.; Bathon, J.M.; Eaton, C.; Hochberg, M.C.; et al. Obesity and other modifiable factors for physical inactivity measured by accelerometer in adults with knee osteoarthritis. Arthritis Rheum. 2012, 65, 53–61. [Google Scholar] [CrossRef]
- Madzia, A.; Agrawal, C.; Jarit, P.; Petterson, S.; Plancher, K.; Ortiz, R. Sustained Acoustic Medicine Combined with A Diclofenac Ultrasound Coupling Patch for the Rapid Symptomatic Relief of Knee Osteoarthritis: Multi-Site Clinical Efficacy Study. Open Orthop. J. 2020, 14, 176–185. [Google Scholar] [CrossRef]
- Maly, M.R.; Acker, S.M.; Totterman, S.; Tamez-Peña, J.; Stratford, P.W.; Callaghan, J.P.; Adachi, J.D.; Beattie, K.A. Knee adduction moment relates to medial femoral and tibial cartilage morphology in clinical knee osteoarthritis. J. Biomech. 2015, 48, 3495–3501. [Google Scholar] [CrossRef]
- Mardini, M.T.; Nerella, S.; Kheirkhahan, M.; Ranka, S.; Fillingim, R.B.; Hu, Y.; Corbett, D.B.; Cenko, E.; Weber, E.; Rashidi, P.; et al. The Temporal Relationship Between Ecological Pain and Life-Space Mobility in Older Adults with Knee Osteoarthritis: A Smartwatch-Based Demonstration Study. JMIR mHealth uHealth 2021, 9, e19609. [Google Scholar] [CrossRef] [PubMed]
- Martire, L.M.; Wilson, S.J.; Small, B.J.; Conley, Y.P.; Janicki, P.K.; Sliwinski, M.J. COMT and OPRM1 genotype associations with daily knee pain variability and activity induced pain. Scand. J. Pain 2016, 10, 6–12. [Google Scholar] [CrossRef] [Green Version]
- Nelligan, R.K.; Hinman, R.S.; Teo, P.L.; Bennell, K.L. Exploring Attitudes and Experiences of People with Knee Osteoarthritis Toward a Self-Directed eHealth Intervention to Support Exercise: Qualitative Study. JMIR Rehabil. Assist. Technol. 2020, 7, e18860. [Google Scholar] [CrossRef] [PubMed]
- Parkes, M.J.; Jones, R.K.; Carter, S.C.; Liu, A.; Callaghan, M.J.; Felson, D. Change in pain and its relation to change in activity in osteoarthritis. Osteoarthr. Cartil. Open 2020, 2, 100063. [Google Scholar] [CrossRef]
- Robbins, S.M.; Jones, G.R.; Birmingham, T.B.; Maly, M.R. Quantity and Quality of Physical Activity Are Influenced by Outdoor Temperature in People with Knee Osteoarthritis. Physiother. Can. 2013, 65, 248–254. [Google Scholar] [CrossRef] [Green Version]
- Semanik, P.; Lee, J.; Manheim, L.; DiPietro, L.; Dunlop, D.; Chang, R.W. Relationship between accelerometer-based measures of physical activity and the Yale Physical Activity Survey in adults with arthritis. Arthritis Rheum. 2011, 63, 1766–1772. [Google Scholar] [CrossRef]
- Song, J.; Hochberg, M.C.; Chang, R.W.; Hootman, J.M.; Manheim, L.M.; Lee, J.; Semanik, P.A.; Sharma, L.; Dunlop, R.D. Os-teoarthritis Initiative Investigators Racial and ethnic differences in physical activity guidelines attainment among people at high risk of or having knee osteoarthritis. Arthritis Rheum. 2012, 65, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Song, J.; Semanik, P.; Sharma, L.; Chang, R.W.; Hochberg, M.C.; Mysiw, W.J.; Bathon, J.M.; Eaton, C.; Jackson, R.; Kwoh, C.K.; et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: Data from the osteoarthritis initiative. Arthritis Rheum. 2010, 62, 1724–1732. [Google Scholar] [CrossRef]
- Thoma, L.; Dunlop, D.; Song, J.; Lee, J.; Tudor-Locke, C.; Aguiar, E.J.; Master, H.; Christiansen, M.B.; White, D.K. Are Older Adults with Symptomatic Knee Osteoarthritis Less Active Than the General Population? Analysis From the Osteoarthritis Initiative and the National Health and Nutrition Examination Survey. Arthritis Rheum. 2018, 70, 1448–1454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomkins-Lane, C.; Norden, J.; Sinha, A.; Hu, R.; Smuck, M. Digital biomarkers of spine and musculoskeletal disease from accelerometers: Defining phenotypes of free-living physical activity in knee osteoarthritis and lumbar spinal stenosis. Spine J. 2018, 19, 15–23. [Google Scholar] [CrossRef]
- Uritani, D.; Kasza, J.; Campbell, P.K.; Metcalf, B.; Egerton, T. The association between psychological characteristics and physical activity levels in people with knee osteoarthritis: A cross-sectional analysis. BMC Musculoskelet. Disord. 2020, 21, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vårbakken, K.; Vårbakken, K.; Lorås, H.; Lorås, H.; Nilsson, K.G.; Nilsson, K.G.; Engdal, M.; Engdal, M.; Stensdotter, A.K.; Stensdotter, A.K.; et al. Relative difference among 27 functional measures in patients with knee osteoarthritis: An exploratory cross-sectional case-control study. BMC Musculoskelet. Disord. 2019, 20, 462. [Google Scholar] [CrossRef] [PubMed]
- White, D.K.; Lee, J.; Song, J.; Chang, R.W.; Dunlop, D. Potential Functional Benefit From Light Intensity Physical Activity in Knee Osteoarthritis. Am. J. Prev. Med. 2017, 53, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Zhaoyang, R.; Martire, L.M.; Darnall, B.D. Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain 2020, 161, 2603–2610. [Google Scholar] [CrossRef]
- Zhaoyang, R.; Martire, L.M.; Sliwinski, M.J. Morning self-efficacy predicts physical activity throughout the day in knee osteoarthritis. Health Psychol. 2017, 36, 568–576. [Google Scholar] [CrossRef]
- E Fary, R.; Briffa, N.K.; Briffa, T.G. Effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: Three case reports. Physiother. Theory Pract. 2009, 25, 21–29. [Google Scholar] [CrossRef]
- Alasfour, M.; Almarwani, M. The effect of innovative smartphone application on adherence to a home-based exercise programs for female older adults with knee osteoarthritis in Saudi Arabia: A randomized controlled trial. Disabil. Rehabil. 2020, 1–8. [Google Scholar] [CrossRef]
- Bagnato, G.L.; Miceli, G.; Marino, N.; Sciortino, D. Pulsed electromagnetic fields in knee osteoarthritis: A double blind, placebo-controlled, randomized clinical trial. Rheumatology 2015, 55, 755–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartholdy, C.; Christensen, R.; Kristensen, L.E.; Gudbergsen, H.; Bliddal, H.; Overgaard, A.; Rasmussen, M.U.; Henriksen, M. Association Between Weight Loss and Spontaneous Changes in Physical Inactivity in Overweight/Obese Individuals with Knee Osteoarthritis: An Eight-Week Prospective Cohort Study. Arthritis Rheum. 2019, 72, 397–404. [Google Scholar] [CrossRef] [Green Version]
- Bartholdy, C.; Skou, S.T.; Bliddal, H.; Henriksen, M. Changes in physical inactivity during supervised educational and exercise therapy in patients with knee osteoarthritis: A prospective cohort study. Knee 2020, 27, 1848–1856. [Google Scholar] [CrossRef] [PubMed]
- Beukenhorst, A.L.; Howells, K.; Cook, L.; McBeth, J.; O’Neill, T.W.; Parkes, M.J.; Sanders, C.; Sergeant, J.C.; Weihrich, K.S.; Dixon, W.G. Engagement and Participant Experiences With Consumer Smartwatches for Health Research: Longitudinal, Observational Feasibility Study. JMIR mHealth uHealth 2020, 8, e14368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burrows, N.J.; Barry, B.K.; Sturnieks, D.L.; Booth, J.; Jones, M.D. The Relationship Between Daily Physical Activity and Pain in Individuals with Knee Osteoarthritis. Pain Med. 2020, 21, 2481–2495. [Google Scholar] [CrossRef]
- Clermont, C.A.; Barden, J.M. Accelerometer-based determination of gait variability in older adults with knee osteoarthritis. Gait Posture 2016, 50, 126–130. [Google Scholar] [CrossRef]
- Clynes, M.A.; Parsons, C.; Edwards, M.H.; Tobias, J.H.; Deere, K.; Cooper, C.; Dennison, E.M. A diagnosis of knee osteoarthritis does not predict physical activity 2 years later in older adults: Findings from the Hertfordshire Cohort Study. Rheumatol. Int. 2019, 39, 1405–1411. [Google Scholar] [CrossRef] [Green Version]
- Collins, J.E.; Yang, H.Y.; Trentadue, T.P.; Gong, Y.; Losina, E. Validation of the Fitbit Charge 2 compared to the ActiGraph GT3X+ in older adults with knee osteoarthritis in free-living conditions. PLoS ONE 2019, 14, e0211231. [Google Scholar] [CrossRef]
- Farr, J.N.; Going, S.B.; Lohman, T.G.; Rankin, L.L.; Kasle, S.; Cornett, M.; Cussler, E.C. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum. 2008, 59, 1229–1236. [Google Scholar] [CrossRef] [Green Version]
- Fawole, H.; Felson, D.; Frey-Law, L.; Jafarzadeh, S.; Dell’Isola, A.; Steultjens, M.; Nevitt, M.; Lewis, C.; Riskowski, J.; Chastin, S. Is the association between physical activity and fatigue mediated by physical function or depressive symptoms in symptomatic knee osteoarthritis? The Multicenter Osteoarthritis Study. Scand. J. Rheumatol. 2021, 50, 372–380. [Google Scholar] [CrossRef]
- Focht, B.C.; Garver, M.J.; Devor, S.T.; Dials, J.; Lucas, A.R.; Emery, C.F.; Hackshaw, K.V.; Rejeski, W.J. Group-mediated Physical Activity Promotion and Mobility in Sedentary Patients with Knee Osteoarthritis: Results from the IMPACT-Pilot Trial. J. Rheumatol. 2014, 41, 2068–2077. [Google Scholar] [CrossRef] [PubMed]
- Garland, D.; Holt, P.; Harrington, J.T.; Caldwell, J.; Zizic, T.; Cholewczynski, J. A 3-month, randomized, double-blind, placebo-controlled study to evaluate the safety and efficacy of a highly optimized, capacitively coupled, pulsed electrical stimulator in patients with osteoarthritis of the knee. Osteoarthr. Cartil. 2007, 15, 630–637. [Google Scholar] [CrossRef] [Green Version]
- Garver, M.J.; Focht, B.C.; Dials, J.; Rose, M.; Lucas, A.R.; Devor, S.T.; Emery, C.F.; Hackshaw, K.V.; Rejeski, W.J. Weight Status and Differences in Mobility Performance, Pain Symptoms, and Physical Activity in Older, Knee Osteoarthritis Patients. Arthritis 2014, 2014, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Howe, T.; Rafferty, D. Quadriceps activity and physical activity profiles over long durations in patients with osteoarthritis of the knee and controls. J. Electromyogr. Kinesiol. 2009, 19, e78–e83. [Google Scholar] [CrossRef]
- Jeong, J.N.; Kim, S.H.; Park, K.N. Relationship between objectively measured lifestyle factors and health factors in patients with knee osteoarthritis: The STROBE Study. Medicine 2019, 98, e16060. [Google Scholar] [CrossRef]
- Kearey, P.; Popple, A.; Warren, J.; Davis, T.; Bellamy, N. for the LOBRAS Study Group Improvement in condition-specific and generic quality of life outcomes in patients with knee osteoarthritis following single-injection Synvisc: Results from the LOBRAS study. Curr. Med. Res. Opin. 2016, 33, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Li, L.C.; Feehan, L.M.; Xie, H.; Lu, N.; Shaw, C.D.; Gromala, D.; Zhu, S.; Aviña-Zubieta, J.A.; Hoens, A.M.; Koehn, C.; et al. Effects of a 12-Week Multifaceted Wearable-Based Program for People with Knee Osteoarthritis: Randomized Controlled Trial. JMIR mHealth uHealth 2020, 8, e19116. [Google Scholar] [CrossRef] [PubMed]
- Li, L.C.; Sayre, E.C.; Xie, H.; Clayton, C.; Feehan, L.M. A Community-Based Physical Activity Counselling Program for People With Knee Osteoarthritis: Feasibility and Preliminary Efficacy of the Track-OA Study. JMIR mHealth uHealth 2017, 5, e86. [Google Scholar] [CrossRef]
- Liu, S.-H.; Driban, J.; Eaton, C.; McAlindon, T.E.; Harrold, L.R.; Lapane, K.L. Objectively Measured Physical Activity and Symptoms Change in Knee Osteoarthritis. Am. J. Med. 2016, 129, 497–505.e1. [Google Scholar] [CrossRef] [Green Version]
- Lo, G.H.; McAlindon, T.E.; Hawker, G.A.; Driban, J.B.; Price, L.L.; Song, J.; Eaton, C.B.; Hochberg, M.C.; Jackson, R.D.; Kwoh, C.K.; et al. Symptom assessment in knee osteoarthritis needs to account for physical activity level. Arthritis Rheumatol. 2015, 67, 2897–2904. [Google Scholar] [CrossRef] [Green Version]
- Maly, M.R.; Robbins, S.M.; Stratford, P.W.; Birmingham, T.B.; Callaghan, J.P. Cumulative knee adductor load distinguishes between healthy and osteoarthritic knees–A proof of principle study. Gait Posture 2013, 37, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Martire, L.M.; Stephens, M.A.; Mogle, J.; Schulz, R.; Brach, J.; Keefe, F.J. Daily spousal influence on physical activity in knee osteoarthritis. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2013, 45, 213–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCarthy, I.; Hodgins, D.; Mor, A.; Elbaz, A.; Segal, G. Analysis of knee flexion characteristics and how they alter with the onset of knee osteoarthritis: A case control study. BMC Musculoskelet. Disord. 2013, 14, 169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mecklenburg, G.; Smittenaar, P.; Erhart-Hledik, J.C.; A Perez, D.; Hunter, S. Effects of a 12-Week Digital Care Program for Chronic Knee Pain on Pain, Mobility, and Surgery Risk: Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e156. [Google Scholar] [CrossRef] [Green Version]
- Michishita, R.; Shono, N.; Kasahara, T.; Katoku, M.; Tsuruta, T. The possible influence of osteoarthritis of the knee on the accumulation of coronary risk factors in postmenopausal obese women. Obes. Res. Clin. Pract. 2008, 2, 29–34. [Google Scholar] [CrossRef]
- Mündermann, A.; King, K.B.; Smith, R.L.; Andriacchi, T.P. Change in serum COMP concentration due to ambulatory load is not related to knee OA Status. J. Orthop. Res. 2009, 27, 1408–1413. [Google Scholar] [CrossRef]
- Palmer, S.; Domaille, M.; Cramp, F.; Walsh, N.; Pollock, J.; Kirwan, J.; Johnson, M.I. Transcutaneous Electrical Nerve Stimulation as an Adjunct to Education and Exercise for Knee Osteoarthritis: A Randomized Controlled Trial. Arthritis Rheum. 2014, 66, 387–394. [Google Scholar] [CrossRef]
- Parmelee, P.A.; Cox, B.S.; DeCaro, J.; Keefe, F.J.; Smith, D.M. Racial/ethnic differences in sleep quality among older adults with osteoarthritis. Sleep Health 2017, 3, 163–169. [Google Scholar] [CrossRef]
- Pipitone, N.; Scott, D.L. Magnetic Pulse Treatment for Knee Osteoarthritis: A Randomised, Double-Blind, Placebo-Controlled Study. Curr. Med. Res. Opin. 2001, 17, 190–196. [Google Scholar] [CrossRef]
- Robbins, S.M.; Birmingham, T.B.; Callaghan, J.P.; Jones, G.R.; Chesworth, B.M.; Maly, M.R. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Rheum. 2011, 63, 991–997. [Google Scholar] [CrossRef]
- Skrepnik, N.; Spitzer, A.; Altman, R.; Hoekstra, J.; Stewart, J.; Toselli, R.; Jerome, G.; Iversen, M. Assessing the Impact of a Novel Smartphone Application Compared with Standard Follow-Up on Mobility of Patients With Knee Osteoarthritis Following Treatment With Hylan G-F 20: A Randomized Controlled Trial. JMIR mHealth uHealth 2017, 5, e64. [Google Scholar] [CrossRef] [Green Version]
- Sliepen, M.; Mauricio, E.; Lipperts, M.; Grimm, B.; Rosenbaum, D. Objective assessment of physical activity and sedentary behaviour in knee osteoarthritis patients—Beyond daily steps and total sedentary time. BMC Musculoskelet. Disord. 2018, 19, 64. [Google Scholar] [CrossRef] [Green Version]
- Sultan, A.A.; Samuel, L.; Bhave, A. Utilization and outcomes of neuromuscular electric stimulation in patients with knee osteoarthritis: A retrospective analysis. Ann. Transl. Med. 2019, 7, S246. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.R.; Vincent, H.K. Concentric and Eccentric Resistance Training Comparison on Physical Function and Functional Pain Outcomes in Knee Osteoarthritis: A Randomized Controlled Trial. J. Phys. Med. Rehabil. 2020, 99, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Zhaoyang, R.; Martire, L.M. Daily Sedentary Behavior Predicts Pain and Affect in Knee Arthritis. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2019, 53, 642–651. [Google Scholar] [CrossRef]
- Callahan, L.F.; Cleveland, R.J.; Allen, K.D.; Golightly, Y. Racial/Ethnic, Socioeconomic, and Geographic Disparities in the Epidemiology of Knee and Hip Osteoarthritis. Rheum. Dis. Clin. N. Am. 2021, 47, 1–20. [Google Scholar] [CrossRef]
- Ometov, A.; Shubina, V.; Klus, L.; Skibińska, J.; Saafi, S.; Pascacio, P.; Flueratoru, L.; Gaibor, D.Q.; Chukhno, N.; Chukhno, O.; et al. A Survey on Wearable Technology: History, State-of-the-Art and Current Challenges. Comput. Netw. 2021, 193, 108074. [Google Scholar] [CrossRef]
- Lundgren-Nilsson, Å.; Dencker, A.; Palstam, A.; Person, G.; Horton, M.C.; Escorpizo, R.; Küçükdeveci, A.A.; Kutlay, S.; Elhan, A.H.; Stucki, G.; et al. Patient-reported outcome measures in osteoarthritis: A systematic search and review of their use and psychometric properties. RMD Open 2018, 4, e000715. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, A.; Conway, R.; Meagher, D.; Ólaighin, G. Direct measurement of human movement by accelerometry. Med. Eng. Phys. 2008, 30, 1364–1386. [Google Scholar] [CrossRef] [PubMed]
- Finucane, A.M.; O’Donnell, H.; Lugton, J.; Gibson-Watt, T.; Swenson, C.; Pagliari, C. Digital health interventions in palliative care: A systematic meta-review. NPJ Digit. Med. 2021, 4, 64. [Google Scholar] [CrossRef]
- Manini, T.M.; Mendoza, T.; Battula, M.; Davoudi, A.; Kheirkhahan, M.; Young, M.E.; Weber, E.; Fillingim, R.B.; Rashidi, P. Perception of Older Adults Toward Smartwatch Technology for Assessing Pain and Related Patient-Reported Outcomes: Pilot Study. JMIR mHealth uHealth 2019, 7, e10044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slater, H.; Dear, B.F.; Merolli, M.; Li, L.C.; Briggs, A.M. Use of eHealth technologies to enable the implementation of musculoskeletal Models of Care: Evidence and practice. Best Pract. Res. Clin. Rheumatol. 2016, 30, 483–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, C.; Li, H.; Yang, T.; Deng, Z.-H.; Yang, Y.; Zhang, Y.; Ding, X.; Lei, G.-H. Effectiveness of continuous and pulsed ultrasound for the management of knee osteoarthritis: A systematic review and network meta-analysis. Osteoarthr. Cartil. 2014, 22, 1090–1099. [Google Scholar] [CrossRef] [Green Version]
- Wu, Z.; Ding, X.; Lei, G.; Zeng, C.; Wei, J.; Li, J.; Li, H.; Yang, T.; Cui, Y.; Xiong, Y.; et al. Efficacy and safety of the pulsed electromagnetic field in osteoarthritis: A meta-analysis. BMJ Open 2018, 8, e022879. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Hagen, K.B.; Bijlsma, J.W.J.; Andreassen, O.; Christensen, P.; Conaghan, P.; Doherty, M.; Geenen, R.; Hammond, A.; Kjeken, I.; et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann. Rheum. Dis. 2013, 72, 1125–1135. [Google Scholar] [CrossRef] [Green Version]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [Green Version]
- Pagliari, C.; Sloan, D.; Gregor, P.; Sullivan, F.; Detmer, D.; Kahan, J.P.; Oortwijn, W.; MacGillivray, S. What Is eHealth (4): A Scoping Exercise to Map the Field. J. Med. Internet Res. 2005, 7, e9. [Google Scholar] [CrossRef]
- Bothun, D. The Wearable Life 2.0: Connected Living in a Wearable World. 2016. Available online: https://www.pwc.se/sv/pdf-reports/the-wearable-life-2-0.pdf (accessed on 25 November 2021).
- Lee, C.; Coughlin, J.F. PERSPECTIVE: Older Adults’ Adoption of Technology: An Integrated Approach to Identifying Determinants and Barriers. J. Prod. Innov. Manag. 2014, 32, 747–759. [Google Scholar] [CrossRef]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.; Esculier, J.-F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 1–21. [Google Scholar] [CrossRef]
- Jones, A.; Silva, P.G.; Silva, A.C.; Colucci, M.; Tuffanin, A.; Jardim, J.R.; Natour, J. Impact of cane use on pain, function, general health and energy expenditure during gait in patients with knee osteoarthritis: A randomised controlled trial. Ann. Rheum. Dis. 2011, 71, 172–179. [Google Scholar] [CrossRef]
- Del Din, S.; Godfrey, A.; Galna, B.; Lord, S.; Rochester, L. Free-living gait characteristics in ageing and Parkinson’s disease: Impact of environment and ambulatory bout length. J. Neuroeng. Rehabil. 2016, 13, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Demeyer, H.; Burtin, C.; Van Remoortel, H.; Hornikx, M.; Langer, D.; Decramer, M.; Gosselink, R.; Janssens, W.; Troosters, T. Standardizing the Analysis of Physical Activity in Patients With COPD Following a Pulmonary Rehabilitation Program. Chest 2014, 146, 318–327. [Google Scholar] [CrossRef] [Green Version]
- Curcin, V.; Silva, P.A.; Guisado-Fernandez, E.; Loncar-Turukalo, T.; Zdravevski, E.; Da Silva, J.M.; Chouvarda, I.; Trajkovik, V. Literature on Wearable Technology for Connected Health: Scoping Review of Research Trends, Advances, and Barriers. J. Med. Internet Res. 2019, 21, e14017. [Google Scholar] [CrossRef]
- Shen, Z.; Spruit, M. A Systematic Review of Open Source Clinical Software on GitHub for Improving Software Reuse in Smart Healthcare. Appl. Sci. 2019, 9, 150. [Google Scholar] [CrossRef] [Green Version]
- Gurchiek, R.D.; Choquette, R.H.; Beynnon, B.D.; Slauterbeck, J.R.; Tourville, T.W.; Toth, M.J.; McGinnis, R.S. Open-Source Remote Gait Analysis: A Post-Surgery Patient Monitoring Application. Sci. Rep. 2019, 9, 17966. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Ahamed, N.U.; Kobsar, D.; Ferber, R. New considerations for collecting biomechanical data using wearable sensors: Number of level runs to define a stable running pattern with a single IMU. J. Biomech. 2019, 85, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, G.I.; Triantafyllou, A.I.; Roumpelakis, I.M.; Papagelopoulos, P.J.; Babis, G.C. Gait analysis methodology for the measurement of biomechanical parameters in total knee arthroplasties. A literature review. J. Orthop. 2018, 15, 181–185. [Google Scholar] [CrossRef]
- Guilak, F. Biomechanical factors in osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2011, 25, 815–823. [Google Scholar] [CrossRef] [Green Version]
- Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J.L. Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity. Sensors 2018, 18, 719. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Lu, W.; Narayanan, M.R.; Redmond, S.J.; Lovell, N.H. Low-power technologies for wearable telecare and telehealth systems: A review. Biomed. Eng. Lett. 2015, 5, 1–9. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Haeberle, H.; Ramanathan, D.; Cantrell, W.A.; Navarro, S.; Mont, M.A.; Bloomfield, M.; Patterson, B.M. Remote Patient Monitoring Using Mobile Health for Total Knee Arthroplasty: Validation of a Wearable and Machine Learning–Based Surveillance Platform. J. Arthroplast. 2019, 34, 2253–2259. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 2018, 63, 124–138. [Google Scholar] [CrossRef]
- Reddy, S.; Fox, J.; Purohit, M.P. Artificial intelligence-enabled healthcare delivery. J. R. Soc. Med. 2018, 112, 22–28. [Google Scholar] [CrossRef]
- Sun, H.; Zhang, Z.; Hu, R.Q.; Qian, Y. Wearable Communications in 5G: Challenges and Enabling Technologies. IEEE Veh. Technol. Mag. 2018, 13, 100–109. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cudejko, T.; Button, K.; Willott, J.; Al-Amri, M. Applications of Wearable Technology in a Real-Life Setting in People with Knee Osteoarthritis: A Systematic Scoping Review. J. Clin. Med. 2021, 10, 5645. https://doi.org/10.3390/jcm10235645
Cudejko T, Button K, Willott J, Al-Amri M. Applications of Wearable Technology in a Real-Life Setting in People with Knee Osteoarthritis: A Systematic Scoping Review. Journal of Clinical Medicine. 2021; 10(23):5645. https://doi.org/10.3390/jcm10235645
Chicago/Turabian StyleCudejko, Tomasz, Kate Button, Jake Willott, and Mohammad Al-Amri. 2021. "Applications of Wearable Technology in a Real-Life Setting in People with Knee Osteoarthritis: A Systematic Scoping Review" Journal of Clinical Medicine 10, no. 23: 5645. https://doi.org/10.3390/jcm10235645
APA StyleCudejko, T., Button, K., Willott, J., & Al-Amri, M. (2021). Applications of Wearable Technology in a Real-Life Setting in People with Knee Osteoarthritis: A Systematic Scoping Review. Journal of Clinical Medicine, 10(23), 5645. https://doi.org/10.3390/jcm10235645





