Differences in the Buccal Bone Marrow Distance of ≤0.8 mm in the Mandible of Patients Undergoing Sagittal Split Ramus Osteotomy among the Different Skeletal Patterns: A Retrospective Study
Abstract
:1. Introduction
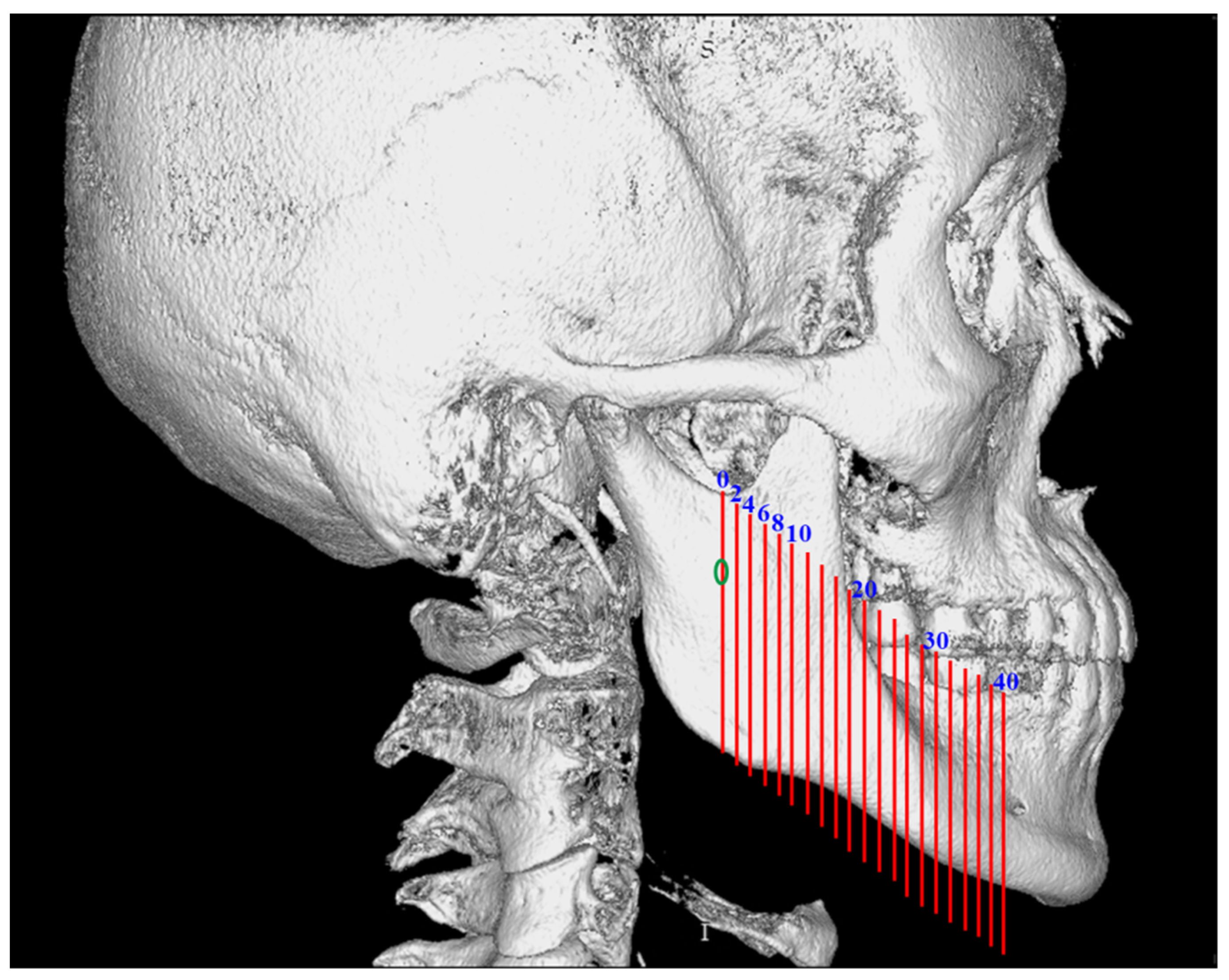
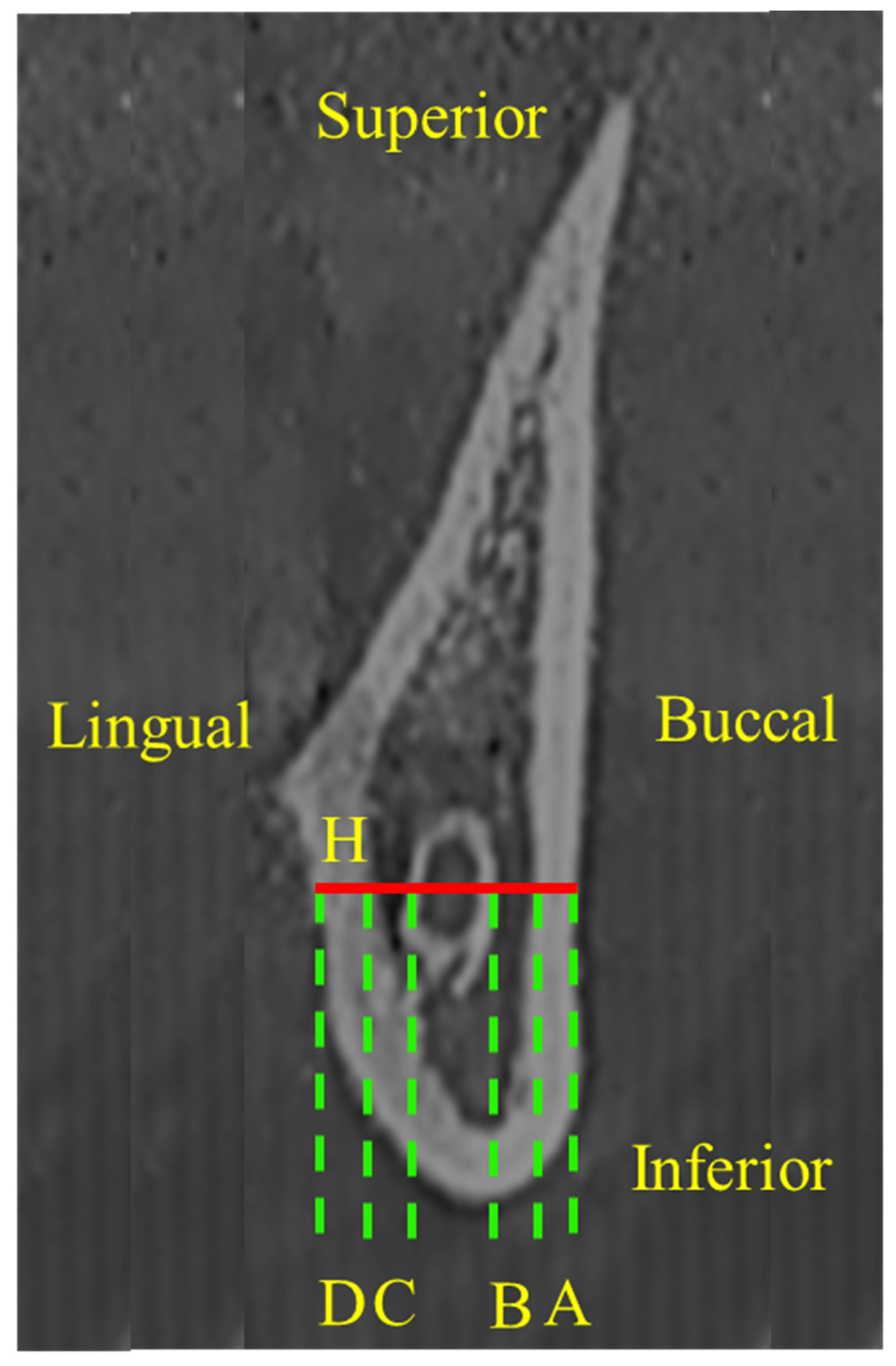
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SSRO | Sagittal Split Ramus Osteotomy |
| CBCT | Cone-Beam Computed Tomography |
References
- Steenen, S.A.; Becking, A.G. Bad Splits in Bilateral Sagittal Split Osteotomy: Systematic Review of Fracture Patterns. Int. J. Oral Maxillofac. Surg. 2016, 45, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Kniha, K.; Peters, F.; Ayoub, N.; Goloborodko, E.; Hölzle, F.; Fritz, U.; Modabber, A. Fracture patterns after bilateral sagittal split osteotomy of the mandibular ramus according to the Obwegeser/Dal Pont and Hunsuck/Epker modifications. J. Craniomaxillofac. Surg. 2017, 45, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Cunha, G.; Oliveira, M.R.; Salmen, F.S.; Gabrielli, M.F.R.; Gabrielli, M.A.C. How does bone thickness affect the split pattern of sagittal ramus osteotomy? Int. J. Oral Maxillofac. Surg. 2020, 49, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Nagamine, T.; Kobayashi, T.; Michimi, N.; Nakajima, T.; Sasakura, H.; Hanada, K. Impairment of the inferior alveolar nerve after sagittal split osteotomy. J. Craniomaxillofac. Surg. 1989, 17, 271–278. [Google Scholar] [CrossRef]
- Ylikontiola, L.; Kinnunen, J.; Oikarinen, K. Factors affecting neurosensory disturbance after mandibular bilateral sagittal split osteotomy. J. Oral Maxillofac. Surg. 2000, 58, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Zaroni, F.M.; Cavalcante, R.C.; João da Costa, D.; Kluppel, L.E.; Scariot, R.; Rebellato, N.L.B. Complications associated with orthognathic surgery: A retrospective study of 485 cases. J. Craniomaxillofac. Surg. 2019, 47, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, R.; Nakamura, A.; Ohno, K.; Michi, K. Relationship of the Mandibular Canal to the Lateral Cortex of the Mandibular Ramus as a Factor in the Development of Neurosensory Disturbance After Bilateral Sagittal Split Osteotomy. J. Oral Maxillofac. Surg. 2002, 60, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Kalabalik, F.; Akçay, H.; Tatar, B. Morphometric analysis of mandibular corpus relevance to sagittal split osteotomy: Comparison of dentoskeletal Class I and Class III patients. J. Stomatol. Oral Maxillofac. Surg. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Westmark, A.; Bystedt, H.; Konow, L. Inferior alveolar nerve function after sagittal split osteotomy of the mandible: Correlation with degree of intraoperative nerve encounter and other variables in 496 operations. Br. J. Oral Maxillofac. Surg. 1998, 36, 429–433. [Google Scholar] [CrossRef]
- Lemke, R.R.; Rugh, J.D.; Van Sickels, J.; Bays, R.A.; Clark, G.M. Neurosensory differences after wire and rigid fixation in patients with mandibular advancement. J. Oral Maxillofac. Surg. 2000, 58, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, K.; Ueki, K.; Takatsuka, S.; Yamamoto, E. Trigemial nerve hypesthesia after sagittal split osteotomy in setback cases: Correlation of postoperative computed tomography and long-term trigeminal somatosensory evoked potentials. J. Oral Maxillofac. Surg. 2003, 61, 898–903. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; de Carvalho Machado, V.; Gjelvold, B. A morphometric analysis of the mandibular canal by cone beam computed tomography and its relevance to the sagittal split ramus osteotomy. Oral Maxillofac. Surg. 2016, 20, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Karas, N.D.; Boyd, S.B.; Sinn, D.P. Recovery of neurosensory function following orthognathic surgery. J. Oral Maxillofac. Surg. 1990, 48, 124–134. [Google Scholar] [CrossRef]
- Huang, C.Y.; Liao, Y.F. Anatomical position of the mandibular canal in relation to the buccal cortical bone in Chinese patients with different dentofacial relationships. J. Formos. Med. Assoc. 2016, 115, 981–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, C.S.; Syu, J.J.; Ko, E.W.; Chen, Y.R. Quantitative Evaluation of Cortical Bone Thickness in Mandibular Prognathic Patients With Neurosensory Disturbance After Bilateral Sagittal Split Osteotomy. J. Oral Maxillofac. Surg. 2013, 71, e1–e10. [Google Scholar] [CrossRef] [PubMed]

| Total Participant by Gender: 60 Female and 30 Male |
|---|
| Total participant by skeletal pattern: |
| 30 Class I (21 female; 9 male) |
| 30 Class II (24 female; 6 male) |
| 30 Class III (15 female; 15 male) |
| Participants with buccal bone marrow distance ≤ 0.8 mm |
| by gender (%): 45 female (75%); 18 male (60%) |
| by skeletal pattern (%): |
| Class I (17 female, 81%; 4 male, 44%) |
| Class II (16 female, 67%; 4 male, 67%) |
| Class III (12 female, 73%; 10 male, 67%) |
| Variables | A | p Value | B | p Value | A + B | p Value | |
|---|---|---|---|---|---|---|---|
| (Mean ± SD, mm) | (Mean ± SD, mm) | (Mean ± SD, mm) | |||||
| 0 mm | Class I | 2.47 ± 0.58 | 0.415 | 2.29 ± 1.42 | 0.252 | 4.75 ± 1.43 | 0.129 |
| Class II | 2.61 ± 0.68 | 2.35 ± 1.38 | 4.96 ± 1.28 | ||||
| Class III | 2.50 ± 0.61 | 1.97 ± 1.17 | 4.47 ± 1.21 | ||||
| 2 mm | Class I | 2.62 ± 0.46 | 0.512 | 2.12 ± 1.38 | 0.297 | 4.73 ± 1.43 | 0.201 |
| Class II | 2.73 ± 0.66 | 2.19 ± 1.28 | 4.92 ± 1.25 | ||||
| Class III | 2.65 ± 0.51 | 1.85 ± 1.14 | 4.50 ± 1.17 | ||||
| 4 mm | Class I | 2.62 ± 0.62 | 0.56 | 1.78 ± 1.44 | 0.28 | 4.39 ± 1.44 | 0.115 |
| Class II | 2.71 ± 0.73 | 2.11 ± 1.28 | 4.82 ± 1.31 | ||||
| Class III | 2.57 ± 0.69 | 1.76 ± 1.33 | 4.34 ± 1.36 | ||||
| 6 mm | Class I | 2.54 ± 0.53 | 0.339 | 1.72 ± 1.29 | 0.019 * | 4.26 ± 1.41 | 0.007 * |
| Class II | 2.66 ± 0.60 | 2.14 ± 1.21 | Class II > III | 4.81 ± 1.35 | Class II > III | ||
| Class III | 2.52 ± 0.55 | 1.50 ± 1.27 | 4.02 ± 1.37 | ||||
| 8 mm | Class I | 2.85 ± 0.70 | 0.131 | 1.77 ± 1.40 | 0.003 * | 4.61 ± 1.45 | <0.001 * |
| Class II | 2.96 ± 0.70 | 2.44 ± 1.31 | Class II > I | 5.39 ± 1.45 | Class II > I | ||
| Class III | 2.70 ± 0.71 | 1.63 ± 1.43 | Class II > III | 4.33 ± 1.49 | Class II > III | ||
| 10 mm | Class I | 2.90 ± 0.53 | 0.022 * | 1.73 ± 1.37 | 0.001 * | 4.62 ± 1.51 | <0.001 * |
| Class II | 3.02 ± 0.54 | Class II > III | 2.56 ± 1.32 | Class II > I | 5.58 ± 1.49 | Class II > I | |
| Class III | 2.71 ± 0.74 | 1.68 ± 1.42 | Class II > III | 4.39 ± 1.66 | Class II > III | ||
| 12 mm | Class I | 3.10 ± 0.70 | 0.455 | 2.08 ± 1.54 | <0.001 * | 5.18 ± 1.64 | <0.001 * |
| Class II | 3.08 ± 0.67 | 3.11 ± 1.39 | Class II > I | 6.19 ± 1.49 | Class II > I | ||
| Class III | 2.94 ± 0.81 | 1.83 ± 1.60 | Class II > III | 4.78 ± 1.77 | Class II > III | ||
| 14 mm | Class I | 3.12 ± 0.64 | 0.052 | 2.36 ± 1.59 | <0.001 * | 5.48 ± 1.59 | <0.001 * |
| Class II | 3.12 ± 0.62 | 3.26 ± 1.38 | Class II > I | 6.32 ± 1.32 | Class II > I | ||
| Class III | 2.87 ± 0.63 | 2.20 ± 1.65 | Class II > III | 5.07 ± 1.94 | Class II > III | ||
| 16 mm | Class I | 3.11 ± 0.64 | 0.814 | 2.99 ± 1.71 | 0.001 * | 6.1 ± 1.72 | <0.001 * |
| Class II | 3.15 ± 0.71 | 3.64 ± 1.41 | Class II > III | 6.79 ± 1.34 | Class II > III | ||
| Class III | 3.06 ± 0.81 | 2.52 ± 1.73 | 5.58 ± 1.90 | ||||
| 18 mm | Class I | 3.22 ± 0.74 | 0.195 | 2.92 ± 1.59 | 0.006 * | 6.14 ± 1.65 | 0.006 * |
| Class II | 3.08 ± 0.58 | 3.64 ± 1.33 | Class II > III | 6.72 ± 1.28 | Class II > III | ||
| Class III | 3.01 ± 0.66 | 2.70 ± 1.99 | 5.71 ± 2.09 | ||||
| 20 mm | Class I | 3.17 ± 0.71 | 0.584 | 3.29 ± 1.42 | 0.026 * | 6.46 ± 1.56 | 0.114 |
| Class II | 3.08 ± 0.62 | 3.76 ± 1.30 | Class II > III | 6.83 ± 1.32 | |||
| Class III | 3.20 ± 0.74 | 3.00 ± 1.81 | 6.20 ± 2.02 | ||||
| 22 mm | Class I | 3.07 ± 0.68 | 0.456 | 3.07 ± 1.55 | 0.328 | 6.14 ± 1.58 | 0.157 |
| Class II | 3.21 ± 0.59 | 3.43 ± 1.20 | 6.63 ± 1.27 | ||||
| Class III | 3.09 ± 0.68 | 3.05 ± 1.84 | 6.14 ± 1.94 | ||||
| 24 mm | Class I | 3.14 ± 0.66 | 0.540 | 3.55 ± 1.46 | 0.600 | 6.69 ± 1.61 | 0.737 |
| Class II | 3.01 ± 0.64 | 3.63 ± 1.20 | 6.64 ± 1.13 | ||||
| Class III | 3.11 ± 0.67 | 3.36 ± 1.73 | 6.48 ± 1.85 | ||||
| 26 mm | Class I | 3.09 ± 0.79 | 0.984 | 3.18 ± 1.31 | 0.990 | 6.26 ± 1.45 | 0.996 |
| Class II | 3.07 ± 0.46 | 3.20 ± 1.29 | 6.27 ± 1.36 | ||||
| Class III | 3.07 ± 0.56 | 3.21 ± 1.66 | 6.29 ± 1.72 | ||||
| 28 mm | Class I | 3.06 ± 0.71 | 0.492 | 3.41 ± 1.20 | 0.220 | 6.47 ± 1.43 | 0.153 |
| Class II | 2.92 ± 0.60 | 3.11 ± 1.47 | 6.03 ± 1.43 | ||||
| Class III | 2.96 ± 0.71 | 3.57 ± 1.67 | 6.53 ± 1.70 | ||||
| 30 mm | Class I | 3.03 ± 0.72 | 0.295 | 3.19 ± 1.20 | 0.012 * | 6.23 ± 1.32 | 0.087 |
| Class II | 3.08 ± 0.55 | 2.73 ± 1.29 | Class III > II | 5.82 ± 1.39 | |||
| Class III | 2.91 ± 0.52 | 3.44 ± 1.41 | 6.36 ± 1.43 | ||||
| 32 mm | Class I | 3.02 ± 0.70 | 0.587 | 3.13 ± 1.20 | 0.096 | 6.15 ± 1.38 | 0.047 * |
| Class II | 2.89 ± 0.60 | 2.80 ± 1.62 | 5.70 ± 1.55 | Class III > II | |||
| Class III | 2.97 ± 0.72 | 3.40 ± 1.58 | 6.38 ± 1.54 | ||||
| 34 mm | Class I | 2.89 ± 0.64 | 0.403 | 2.95 ± 1.17 | 0.017 * | 5.84 ± 1.29 | 0.042 * |
| Class II | 3.03 ± 0.59 | 2.41 ± 1.33 | Class III > II | 5.43 ± 1.54 | Class III > II | ||
| Class III | 3.03 ± 0.63 | 3.08 ± 1.35 | 6.11 ± 1.40 | ||||
| 36 mm | Class I | 3.07 ± 0.73 | 0.607 | 2.64 ± 1.21 | 0.005 * | 5.72 ± 1.36 | 0.020 * |
| Class II | 3.00 ± 0.71 | 2.30 ± 1.55 | Class III > II | 5.30 ± 1.59 | Class III > II | ||
| Class III | 2.94 ± 0.75 | 3.17 ± 1.38 | 6.11 ± 1.42 | ||||
| 38 mm | Class I | 2.85 ± 0.52 | 0.166 | 2.41 ± 1.25 | 0.357 | 5.26 ± 1.32 | 0.242 |
| Class II | 3.08 ± 0.60 | 2.27 ± 1.35 | 5.35 ± 1.57 | ||||
| Class III | 3.00 ± 0.62 | 2.67 ± 1.37 | 5.68 ± 1.32 | ||||
| 40 mm | Class I | 3.17 ± 0.77 | 0.073 | 1.98 ± 1.16 | 0.014 * | 5.15 ± 1.37 | 0.122 |
| Class II | 2.77 ± 0.65 | 2.39 ± 1.77 | Class III > I | 5.15 ± 1.70 | |||
| Class III | 2.89 ± 0.81 | 2.77 ± 1.44 | 5.67 ± 1.36 |
| Variables | C | p Value | D | p Value | H | p Value | |
|---|---|---|---|---|---|---|---|
| (Mean ± SD, mm) | (Mean ± SD, mm) | (Mean ± SD, mm) | |||||
| 0 mm | Class I | 0.06 ± 0.30 | 0.114 | 1.14 ± 0.57 | 0.195 | 9.79 ± 1.61 | 0.641 |
| Class II | 0.01 ± 0.06 | 0.97 ± 0.52 | 9.55 ± 1.37 | ||||
| Class III | 0.00 ± 0.00 | 1.05 ± 0.43 | 9.65 ± 1.31 | ||||
| 2 mm | Class I | 0.02 ± 0.12 | 0.368 | 1.28 ± 0.65 | 0.448 | 9.96 ± 1.50 | 0.735 |
| Class II | 0.03 ± 0.18 | 1.15 ± 0.56 | 9.79 ± 1.38 | ||||
| Class III | 0.00 ± 0.00 | 1.19 ± 0.46 | 9.78 ± 1.30 | ||||
| 4 mm | Class I | 0.14 ± 0.36 | 0.644 | 1.65 ± 0.71 | 0.580 | 10.08 ± 1.60 | 0.480 |
| Class II | 0.18 ± 0.42 | 1.59 ± 0.50 | 10.21 ± 1.44 | ||||
| Class III | 0.11 ± 0.34 | 1.53 ± 0.71 | 9.89 ± 1.27 | ||||
| 6 mm | Class I | 0.35 ± 0.57 | 0.239 | 1.83 ± 0.71 | 0.077 | 10.25 ± 1.66 | 0.116 |
| Class II | 0.19 ± 0.42 | 1.56 ± 0.60 | 10.38 ± 1.47 | ||||
| Class III | 0.29 ± 0.53 | 1.65 ± 0.65 | 9.84 ± 1.29 | ||||
| 8 mm | Class I | 0.41 ± 0.63 | 0.881 | 2.20 ± 0.96 | 0.004 * | 11.09 ± 1.68 | 0.364 |
| Class II | 0.42 ± 0.71 | 1.74 ± 0.56 | Class I > II | 11.25 ± 1.70 | |||
| Class III | 0.46 ± 0.67 | 2.08 ± 0.75 | Class III > II | 10.84 ± 1.44 | |||
| 10 mm | Class I | 0.64 ± 0.80 | 0.255 | 1.87 ± 0.67 | 0.005 * | 11.19 ± 1.78 | 0.140 |
| Class II | 0.41 ± 0.70 | 1.58 ± 0.56 | Class I > II | 11.42 ± 1.64 | |||
| Class III | 0.51 ± 0.78 | 1.95 ± 0.70 | Class III > II | 10.81 ± 1.65 | |||
| 12 mm | Class I | 0.69 ± 0.87 | 0.165 | 2.23 ± 0.99 | 0.006 * | 12.11 ± 1.90 | 0.515 |
| Class II | 0.42 ± 0.65 | 1.91 ± 0.62 | Class III > II | 12.28 ± 1.80 | |||
| Class III | 0.65 ± 1.01 | 2.37 ± 0.74 | 11.90 ± 1.75 | ||||
| 14 mm | Class I | 0.71 ± 0.86 | 0.027 * | 1.88 ± 0.54 | 0.010 * | 12.12 ± 1.84 | 0.392 |
| Class II | 0.39 ± 0.70 | Class III > II | 1.69 ± 0.56 | Class III > II | 12.15 ± 1.64 | ||
| Class III | 0.83 ± 1.16 | 2.03 ± 0.67 | 11.74 ± 1.89 | ||||
| 16 mm | Class I | 0.56 ± 0.97 | 0.009 * | 2.20 ± 0.72 | 0.005 * | 12.64 ± 1.73 | 0.879 |
| Class II | 0.46 ± 0.77 | Class III > I | 1.92 ± 0.68 | Class III > II | 12.79 ± 1.64 | ||
| Class III | 1.02 ± 1.32 | Class III > II | 2.36 ± 0.82 | 12.76 ± 1.79 | |||
| 18 mm | Class I | 0.64 ± 0.73 | 0.010 * | 1.94 ± 0.51 | 0.305 | 12.61 ± 1.72 | 0.905 |
| Class II | 0.39 ± 0.73 | Class III > II | 1.81 ± 0.67 | Class III > II | 12.66 ± 1.59 | ||
| Class III | 0.91 ± 0.63 | 2.00 ± 0.67 | 12.52 ± 1.99 | ||||
| 20 mm | Class I | 0.42 ± 0.67 | 0.015 * | 2.35 ± 0.64 | 0.003 * | 13.05 ± 1.72 | 0.370 |
| Class II | 0.45 ± 0.71 | Class III > II | 1.95 ± 0.63 | Class I > II | 12.86 ± 1.57 | ||
| Class III | 0.83 ± 1.09 | 2.47 ± 1.17 | Class III > II | 13.33 ± 2.11 | |||
| 22 mm | Class I | 0.64 ± 1.01 | 0.007 * | 2.06 ± 0.58 | 0.654 | 12.68 ± 1.71 | 0.424 |
| Class II | 0.31 ± 0.57 | Class III > II | 2.01 ± 0.61 | 12.51 ± 1.65 | |||
| Class III | 0.90 ± 1.29 | 2.11 ± 0.71 | 12.95 ± 2.12 | ||||
| 24 mm | Class I | 0.35 ± 0.55 | 0.054 | 2.39 ± 0.67 | 0.125 | 13.00 ± 1.77 | 0.084 |
| Class II | 0.33 ± 0.62 | 2.20 ± 0.71 | 12.63 ± 1.55 | ||||
| Class III | 0.59 ± 0.79 | 2.53 ± 1.15 | 13.39 ± 2.20 | ||||
| 26 mm | Class I | 0.30 ± 0.60 | 0.006 * | 2.14 ± 0.63 | 0.990 | 12.49 ± 1.78 | 0.267 |
| Class II | 0.27 ± 0.52 | Class III > I | 2.13 ± 0.68 | 12.31 ± 1.52 | |||
| Class III | 0.71 ± 1.2 | Class III > II | 2.13 ± 0.57 | 12.84 ± 2.07 | |||
| 28 mm | Class I | 0.28 ± 0.46 | 0.087 | 2.42 ± 0.73 | 0.887 | 12.69 ± 1.91 | 0.173 |
| Class II | 0.51 ± 0.88 | 2.35 ± 0.63 | 12.46 ± 1.43 | ||||
| Class III | 0.57 ± 0.87 | 2.37 ± 0.80 | 13.09 ± 2.13 | ||||
| 30 mm | Class I | 0.37 ± 0.52 | 0.195 | 2.09 ± 0.63 | 0.018 * | 12.23 ± 1.78 | 0.909 |
| Class II | 0.58 ± 0.82 | 2.29 ± 0.76 | Class II > III | 12.32 ± 1.46 | |||
| Class III | 0.61 ± 0.94 | 1.93 ± 0.64 | 12.37 ± 1.95 | ||||
| 32 mm | Class I | 0.26 ± 0.46 | 0.001 * | 2.38 ± 0.76 | 0.254 | 12.26 ± 1.90 | 0.614 |
| Class II | 0.87 ± 1.18 | Class II > I | 2.46 ± 0.83 | 12.52 ± 1.67 | |||
| Class III | 0.58 ± 0.88 | 2.22 ± 0.85 | 12.58 ± 2.06 | ||||
| 34 mm | Class I | 0.42 ± 0.61 | 0.001 * | 2.22 ± 0.63 | 0.002 * | 11.98 ± 1.61 | 0.338 |
| Class II | 0.98 ± 1.04 | Class II > I | 2.30 ± 0.63 | Class I > III | 12.39 ± 1.72 | ||
| Class III | 0.52 ± 0.70 | Class II > III | 1.90 ± 0.61 | Class II > III | 11.94 ± 1.92 | ||
| 36 mm | Class I | 0.36 ± 0.56 | <0.001 * | 2.5 ± 0.73 | 0.004 * | 11.99 ± 1.80 | 0.057 |
| Class II | 1.27 ± 1.33 | Class II > I | 2.63 ± 0.95 | Class I > III | 12.85 ± 2.00 | ||
| Class III | 0.37 ± 0.57 | Class II > III | 2.14 ± 0.66 | Class II > III | 12.11 ± 1.96 | ||
| 38 mm | Class I | 0.53 ± 0.66 | 0.002 * | 2.29 ± 0.68 | 0.004 * | 11.57 ± 1.60 | 0.131 |
| Class II | 1.18 ± 1.40 | Class II > I | 2.25 ± 0.88 | Class I > III | 12.44 ± 2.56 | ||
| Class III | 0.49 ± 0.69 | Class II > III | 1.87 ± 0.64 | 11.62 ± 1.94 | |||
| 40 mm | Class I | 0.55 ± 0.72 | 0.084 | 2.54 ± 0.79 | 0.089 | 11.79 ± 1.81 | 0.899 |
| Class II | 1.06 ± 1.42 | 2.26 ± 1.05 | 12.04 ± 2.73 | ||||
| Class III | 0.60 ± 0.79 | 2.21 ± 0.68 | 11.83 ± 1.97 |
| Total Sides: Female (2520 Sides); Male (1260 Sides) |
|---|
| Buccal bone marrow distance ≤ 0.8 mm (461 sides): |
| by gender (female > male): female (294 sided); male (167 sides) |
| by skeletal pattern (Class III > Class I > Class II) * |
| Class I (159 sides), Class II (104 sides), Class III (198 sides) |
| Buccal bone marrow distance ≤ 0.8 mm (mean value: mm): |
| by gender (female > male) **: female: 0.33 ± 0.30 mm; male: 0.25 ± 0.29 mm |
| by skeletal pattern (Class II > Class III) *** |
| Class I: 0.31 ± 0.31 mm; Class II: 0.37 ± 0.31 mm; Class III: 0.25 ± 0.27 mm |
| Variables | Class I | Class II | Class III | p Value | Significant | ||
|---|---|---|---|---|---|---|---|
| 0 mm | 13.33% | 15.00% | 16.67% | 0.877 | |||
| 2 mm | 18.33% | 15.00% | 18.33% | 0.856 | |||
| 4 mm | 28.33% | 16.67% | 30.00% | 0.185 | |||
| 6 mm | 26.67% | 15.00% | 35.00% | 0.041 * | Class III > II | ||
| 8 mm | 31.67% | 15.00% | 35.00% | 0.031 * | Class I > II, Class III > II | ||
| 10 mm | 31.67% | 10.00% | 30.00% | 0.008 * | Class I > II, Class III > II | ||
| 12 mm | 25.00% | 3.33% | 30.00% | 0.001 * | Class I > II, Class III > II | ||
| 14 mm | 21.67% | 3.33% | 23.33% | 0.004 * | Class I > II, Class III > II | ||
| 16 mm | 11.67% | 1.67% | 15.00% | 0.034 * | Class I > II, Class III > II | ||
| 18 mm | 8.33% | 1.67% | 18.33% | 0.007 * | Class III > II | ||
| 20 mm | 3.33% | 1.67% | 13.33% | 0.016 * | Class III > II | ||
| 22 mm | 3.33% | 1.67% | 15.00% | 0.006 * | |||
| 24 mm | 1.67% | 0.00% | 6.67% | 0.069 | |||
| 26 mm | 1.67% | 1.67% | 5.00% | 0.439 | |||
| 28 mm | 0.00% | 8.33% | 3.33% | 0.059 | |||
| 30 mm | 1.67% | 8.33% | 1.67% | 0.093 | |||
| 32 mm | 1.67% | 11.67% | 3.33% | 0.038 * | Class II > I | ||
| 34 mm | 1.67% | 11.67% | 3.33% | 0.038 * | Class II > I | ||
| 36 mm | 5.00% | 16.67% | 5.00% | 0.035 * | Class II > I, Class II > III | ||
| 38 mm | 11.67% | 6.67% | 10.00% | 0.635 | |||
| 40 mm | 18.33% | 6.67% | 11.67% | 0.147 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseng, Y.-C.; Liang, S.-W.; Chou, S.-T.; Chen, S.-C.; Pan, C.-Y.; Chen, C.-M. Differences in the Buccal Bone Marrow Distance of ≤0.8 mm in the Mandible of Patients Undergoing Sagittal Split Ramus Osteotomy among the Different Skeletal Patterns: A Retrospective Study. J. Clin. Med. 2021, 10, 5644. https://doi.org/10.3390/jcm10235644
Tseng Y-C, Liang S-W, Chou S-T, Chen S-C, Pan C-Y, Chen C-M. Differences in the Buccal Bone Marrow Distance of ≤0.8 mm in the Mandible of Patients Undergoing Sagittal Split Ramus Osteotomy among the Different Skeletal Patterns: A Retrospective Study. Journal of Clinical Medicine. 2021; 10(23):5644. https://doi.org/10.3390/jcm10235644
Chicago/Turabian StyleTseng, Yu-Chuan, Shih-Wei Liang, Szu-Ting Chou, Shih-Chieh Chen, Chin-Yun Pan, and Chun-Ming Chen. 2021. "Differences in the Buccal Bone Marrow Distance of ≤0.8 mm in the Mandible of Patients Undergoing Sagittal Split Ramus Osteotomy among the Different Skeletal Patterns: A Retrospective Study" Journal of Clinical Medicine 10, no. 23: 5644. https://doi.org/10.3390/jcm10235644
APA StyleTseng, Y.-C., Liang, S.-W., Chou, S.-T., Chen, S.-C., Pan, C.-Y., & Chen, C.-M. (2021). Differences in the Buccal Bone Marrow Distance of ≤0.8 mm in the Mandible of Patients Undergoing Sagittal Split Ramus Osteotomy among the Different Skeletal Patterns: A Retrospective Study. Journal of Clinical Medicine, 10(23), 5644. https://doi.org/10.3390/jcm10235644






