Proximal Aortic Dilatation and Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot: Is There a Relationship? A Cardiac Magnetic Resonance Imaging Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
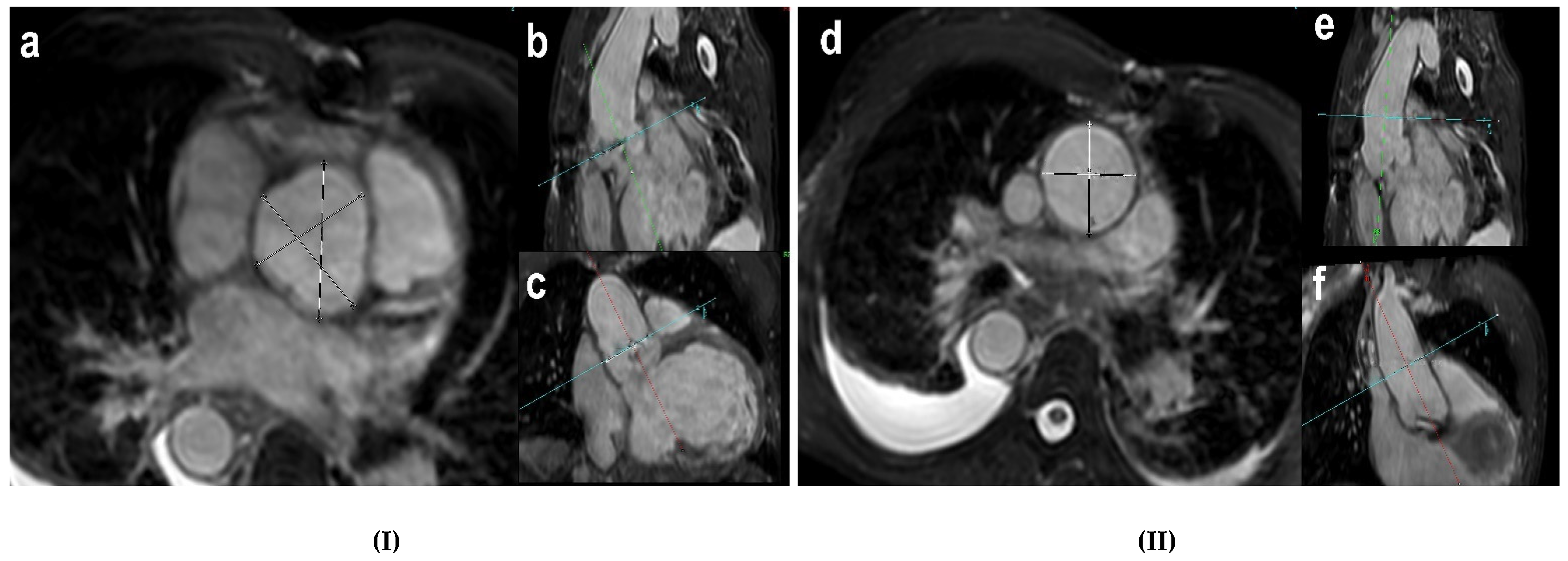
2.3. Cardiac Magnetic Resonance Imaging
2.4. Definition of Proximal Aortic Dilatation
2.5. Statistical Analysis
3. Results
3.1. Prevalence of Proximal Aortic Dilatation and Aortic Valve Regurgitation
3.2. Patients’ Characteristics
3.3. Surgical Reinterventions
3.4. Factors Associated with Proximal Aortic Dilatation
4. Discussion
4.1. Aortic Dilatation: Definition, Prevalence, and Level of Measurement
4.2. Factors Associated with Proximal Aortic Dilatation
4.3. Predictors of Proximal Aortic Dilatation
4.3.1. PVR
4.3.2. Aortic Valve Disease
4.4. Surgical Reinterventions
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lillehei, C.W.; Cohen, M.; Warden, H.E.; Read, R.C.; Aust, J.B.; DeWall, R.A.; Varco, R.L. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot, and pulmonary atresia defects: Report of first ten cases. Ann. Surg. 1955, 142, 418–442. [Google Scholar] [CrossRef]
- Cedars, A.; Benjamin, L.; Vyhmeister, R.; Harris, K.; Bradley, E.A.; Wadia, S.; Awad, A.J.; Novak, E. Contemporary hospitalization rate among adults with complex congenital heart disease. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 334–343. [Google Scholar] [CrossRef]
- Baumgartner, H.; Bonhoeffer, P.; De Groot, N.M.S.; De Haan, F.; Deanfield, J.E.; Galie, N.; Gatzoulis, M.A.; Gohlke-Baerwolf, C.; Kaemmerer, H.; Kilner, P.; et al. The Task Force on the Management of Grown-Up Congenital Heart Disease of the European Society of Cardiology (ESC): ESC Guidelines for the management of grown-up congenital heart disease. Eur. Heart J. 2010, 31, 2915–2957. [Google Scholar]
- Cuypers, J.A.A.E.; Menting, M.E.; Konings, E.E.M.; Opić, P.; Utens, E.M.W.; Helbing, W.A.; Witsenburg, M.; Van den Bosch, A.E.; Ouhlous, M.; van Domburg, R.T.; et al. Unnatural history of tetralogy of Fallot: Prospective follow-up of 40 years after surgical correction. Circulation 2014, 130, 1944–1953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egbe, A.C.; Crestanello, J.; Miranda, W.R.; Connolly, H.M. Thoracic aortic dissection in tetralogy of Fallot: A review of the National Inpatient Sample Database. J. Am. Heart Assoc. 2019, 8, e011943. [Google Scholar] [CrossRef] [Green Version]
- Vida, V.L.; Triglia, L.T.; Zanotto, L.; Zanotto, L.; Bertelli, F.; Padalino, M.; Sarris, G.; Protopapas, E.; Prospero, C.; Pizarro, C.; et al. Late management of the aortic root after repair of tetralogy of Fallot: A European multicentre study. J. Card. Surg. 2020, 35, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Kawel-Boehm, N.; Hetzel, S.J.; Ambale-Venkatesh, B.; Captur, G.; Francois, C.J.; Jerosch-Herold, M.; Salerno, M.; Teague, S.D.; Valsangiacomo-Buechel, E.; Van der Geest, R.J.; et al. Reference ranges (‘normal values’) for cardiovascular magnetic resonance (CMR) in adults and children: 2020 update. J. Cardiovasc. Magn. Reson. 2020, 22, 87. [Google Scholar] [CrossRef] [PubMed]
- Burman, E.D.; Keegan, J.; Kilner, P.J. Aortic root measurement by cardiovascular magnetic resonance: Specification of planes and lines of measurement and corresponding normal values. Circ. Cardiovasc. Imaging 2008, 1, 104–113. [Google Scholar] [CrossRef] [Green Version]
- Davis, A.E.; Lewandowski, A.J.; Holloway, C.J.; Ntusi, N.A.B.; Banerjee, R.; Nethononda, R.; Pitcher, A.; Francis, J.M.; Myerson, S.G.; Leeson, P.; et al. Observational study of regional aortic size referenced to body size: Production of a cardiovascular magnetic resonance nomogram. J. Cardiovasc. Magn. Reson. 2014, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Mongeon, F.P.; Gurvitz, M.Z.; Broberg, C.S.; Aboulhosn, J.; Opotowsky, A.R.; Kay, J.D.; Valente, A.M.; Earing, M.G.; Lui, G.K.; Fernandes, S.M.; et al. Aortic root dilatation in adults with surgically repaired tetralogy of Fallot: A multicenter cross-sectional study. Circulation 2013, 127, 172–179. [Google Scholar] [CrossRef] [Green Version]
- Chong, W.Y.; Wong, W.H.S.; Chiu, C.S.W.; Cheung, Y.F. Aortic root dilation and aortic elastic properties in children after repair of tetralogy of Fallot. Am. J. Cardiol. 2006, 97, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Cruz, C.; Pinho, T.; Madureira, A.J.; Dias, C.C.; Ramos, I.; Silva Cardoso, J.S.; Maciel, M.J. Is it important to assess the ascending aorta after tetralogy of Fallot repair? Rev. Port. Cardiol. (Engl. Ed.) 2018, 37, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Dodds III, G.A.; Warnes, C.A.; Danielson, G.K. Aortic valve replacement after repair of pulmonary atresia and ventricular septal defect or tetralogy of Fallot. J. Thorac. Cardiovasc. Surg. 1997, 113, 736–741. [Google Scholar] [CrossRef] [Green Version]
- Nagy, C.D.; Alejo, D.E.; Corretti, M.C.; Ravekes, W.J.; Crosson, J.E.; Spevak, P.J.; Ringel, R.; Carson, K.A.; Khalil, S.; Dietz, H.C.; et al. Tetralogy of Fallot and aortic root dilation: A long-term outlook. Pediatr. Cardiol. 2013, 34, 809–816. [Google Scholar] [CrossRef]
- Bonello, B.; Shore, D.F.; Uebing, A.; Diller, G.P.; Keegan, J.; Burman, E.D.; Shiina, Y.; Swan, L.; Pennell, D.J.; Kilner, P.J.; et al. Aortic dilatation in repaired tetralogy of Fallot. JACC Cardiovasc. Imaging 2018, 11, 150–152. [Google Scholar] [CrossRef]
- Kay, W.A.; Cook, S.C.; Daniels, C.J. Evaluation by MRA of aortic dilation late after repair of tetralogy of Fallot. Int. J. Cardiol. 2013, 167, 2922–2927. [Google Scholar] [CrossRef]
- Niwa, K.; Siu, S.C.; Webb, G.D.; Gatzoulis, M.A. Progressive aortic root dilatation in adults late after repair of tetralogy of Fallot. Circulation 2002, 106, 1374–1378. [Google Scholar] [CrossRef] [Green Version]
- Saiki, H.; Kojima, T.; Seki, M.; Masutani, S.; Senzaki, H. Marked disparity in mechanical wall properties between ascending and descending aorta in patients with tetralogy of Fallot. Eur. J. Cardiothorac. Surg. 2012, 41, 570–573. [Google Scholar] [CrossRef]
- Rathi, V.K.; Doyle, M.; Williams, R.B.; Yamrozik, J.; Shannon, R.P.; Biederman, R.W. Massive aortic aneurysm and dissection in repaired tetralogy of Fallot; diagnosis by cardiovascular magnetic resonance imaging. Int. J. Cardiol. 2005, 101, 169–170. [Google Scholar] [CrossRef]
- Kim, W.H.; Seo, J.W.; Kim, S.J.; Song, J.; Lee, J.; Na, C.Y. Aortic dissection late after repair of tetralogy of Fallot. Int. J. Cardiol. 2005, 101, 515–516. [Google Scholar] [CrossRef]
- Konstantinov, I.E.; Fricke, T.A.; d’Udekem, Y.; Robertson, T. Aortic dissection and rupture in adolescents after tetralogy of Fallot repair. J. Thorac. Cardiovasc. Surg. 2010, 140, e71–e73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijesekera, V.A.; Kiess, M.C.; Grewal, J.; Chow, R.; Raju, R.; Leipsic, J.A.; Barlow, A.J. Aortic dissection in a patient with a dilated aortic root following tetralogy of Fallot repair. Int. J. Cardiol. 2014, 174, 833–834. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.C.; Rocha, B.A.; Au, T.W.K.; Yung, T.C. Aortic dissection in a Chinese patient 31 years after surgical repair of tetralogy of Fallot. J. Cardiol. Cases 2020, 22, 174–176. [Google Scholar] [CrossRef] [PubMed]
- Capelli, H.; Ross, D.; Somerville, J. Aortic regurgitation in tetrad of Fallot and pulmonary atresia. Am. J. Cardiol. 1982, 49, 1979–1983. [Google Scholar] [CrossRef]
- Bhat, A.H.; Smith, C.J.; Hawker, R.E. Late aortic root dilatation in tetralogy of Fallot may be prevented by early repair in infancy. Pediatr. Cardiol. 2004, 25, 654–659. [Google Scholar] [CrossRef]
- Sim, H.T.; Kim, J.W.; Kim, S.H.; Park, S.J.; Jang, S.I.; Lee, C.H. Correlation between total repair timing and late aortic root dilatation in repaired tetralogy of Fallot. Pediatr. Cardiol. 2020, 41, 1501–1508. [Google Scholar] [CrossRef]
- Anderson, R.H.; Cook, A.; Brown, N.A.; Henderson, D.J.; Chaudhry, B.; Mohun, T. Development of the outflow tracts with reference to aortopulmonary windows and aortoventricular tunnels. Cardiol. Young 2010, 20 (Suppl. 3), 92–99. [Google Scholar] [CrossRef]
- Rao, B.N.S.; Anderson, R.C.; Edwards, J.E. Anatomic variations in the tetralogy of Fallot. Am. Heart J. 1971, 81, 361–371. [Google Scholar]
- Ordovas, K.G.; Keedy, A.; Naeger, D.M.; Kallianos, K.; Foster, E.; Liu, J.; Saloner, D.; Hope, M.D. Dilatation of the ascending aorta is associated with presence of aortic regurgitation in patients after repair of tetralogy of Fallot. Int. J. Cardiovasc. Imaging 2016, 32, 1265–1272. [Google Scholar] [CrossRef] [Green Version]
- Maselli, D.; De Paulis, R.; Scaffa, R.; Weltert, L.; Bellisario, A.; Salica, A.; Ricci, A. Sinotubular junction size affects aortic root geometry and aortic valve function in the aortic valve reimplantation procedure: An in vitro study using the Valsalva graft. Ann. Thorac. Surg. 2007, 84, 1214–1218. [Google Scholar] [CrossRef]
- Schäfers, H.-J. The 10 Commandments for Aortic Valve Repair; SAGE Publications Sage CA: Los Angeles, CA, USA, 2019. [Google Scholar]
- Marom, G.; Halevi, R.; Haj-Ali, R.; Rosenfeld, M.; Schäfers, H.-J.; Raanani, E. Numerical model of the aortic root and valve: Optimization of graft size and sinotubular junction to annulus ratio. J. Thorac. Cardiovasc. Surg. 2013, 146, 1227–1231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Nondilated SoV, n = 34 | Dilated SoV, n = 43 | Nondilated AAo, n = 58 | Dilated AAo, n = 19 | |
|---|---|---|---|---|
| Absolute inner diameter (mm) | 37.8 ± 5.0 | 41.3 ± 5.1 | 31.3 ± 4.4 | 40.9 ± 5.5 |
| Inner diameter indexed to BSA (mm/m2) | 19.3 ± 1.9 | 23.9 ± 2.8 | 16.8 ± 1.9 | 23.7 ± 2.8 |
| All Study Population | Nondilated SoV, n = 34 | Dilated SoV, n = 43 | p | Nondilated AAo, n = 58 | Dilated AAo, n = 19 | p | |
|---|---|---|---|---|---|---|---|
| Male, n (%) | 45 (58.4) | 18 (52.9) | 27 (62.8) | 0.486 | 33 (56.9) | 12 (63.2) | 0.790 |
| Age at CMR, y * | 28.8 ± 10.6 | 26 ±10.07 | 30.8 ± 10.66 | 0.024 | 26.5 ± 9.6 | 35.5 ± 10.7 | 0.002 |
| Age at corrective surgery, m * | 52.1 ± 48.2 | 36.8 ± 40.6 | 64.1 ± 50.7 | 0.004 | 39.9 ± 40.6 | 89 ± 51.7 | <0.001 |
| Correction during the 1st year of life, n (%) | 20 (26) | 14 (41.2) | 6 (14) | 0.009 | 20 (34.5) | 0 (0) | 0.002 |
| Palliative shunt, n (%) | 15 (19.5) | 4 (11.8) | 11 (25.6) | 0.156 | 7 (12.1) | 8 (42.1) | 0.008 |
| Palliative shunt duration, y * | 0.9 ± 2.3 | 0.73 ± 2.35 | 1.09 ± 2.29 | 0.156 | 0.6 ± 2 | 1.95 ± 2.89 | 0.005 |
| Residual_VSD, n (%) | 13 (16.9) | 5 (14.7) | 8 (18.6) | 0.764 | 6 (10.3) | 7 (36.8) | 0.013 |
| Residual VSD_duration, m * | 3.6 ± 10 | 1.79 ± 5.35 | 5.05 ± 12.33 | 0.560 | 1.37 ± 4.77 | 10.42 ± 16.76 | 0.005 |
| Right-sided aortic arch, n (%) | 23 (29.9) | 13 (38.2) | 10 (23.3) | 0.211 | 20 (34.5) | 3 (15.8) | 0.156 |
| AR moderate to severe, n (%) | 3 (3.9) | 0 (0) | 3 (7) | 0.251 | 0 (0) | 3 (15.8) | 0.013 |
| AR_fraction, % * | 5.4 ± 10.6 | 2.91 ± 4.4 | 7.2 ± 13.32 | 0.370 | 2.29 ± 3.88 | 14.7 ± 17.32 | <0.001 |
| AVR, n (%) | 3 (3.9) | 0 (0) | 3 (7) | 0.251 | 0 (0) | 3 (15.8) | 0.013 |
| Ascending aorta replacement, n (%) | 2 (2.6) | 0 (0) | 2 (4.7) | 0.500 | 0 (0) | 2 (10.5) | 0.058 |
| TAP, n (%) | 57 (74) | 25 (73.5) | 32 (74.4) | 1.000 | 41 (70.7) | 16 (84.2) | 0.387 |
| PR fraction, % * | 31.4 ± 17.2 | 29.94 ± 14.49 | 32.37 ± 19.23 | 0.355 | 30.17 ± 14.38 | 34.73 ± 24.14 | 0.151 |
| PVR, n (%) | 28 (36.4) | 8 (23.5) | 20 (46.5) | 0.056 | 14 (24.1) | 14 (73.7) | <0.001 |
| Arterial hypertension, n (%) | 3 (3.9) | 2 (5.9) | 1 (2.3) | 0.580 | 2 (3.4) | 1 (5.3) | 1.000 |
| SBP * (mmHg) | 116.4 ± 12.9 | 117.3 ± 13.3 | 115.5 ± 12.7 | 0.687 | 117.1 ± 12.9 | 113.8 ± 12.9 | 0.470 |
| DBP * (mmHg) | 71.6 ± 12.4 | 69.3 ± 12.2 | 73.4 ± 12.4 | 0.188 | 70.8 ± 11.6 | 74.1 ± 14.5 | 0.467 |
| NYHA >II, n (%) | 8 (10.4) | 0 | 8 (18.6) | 0.003 | 2 (3.4) | 6 (31.6) | 0.002 |
| Dilated SoV Group | Dilated AAo Group | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Male | 1.5 | 0.5–2 | 0.385 | 1.30 | 0.45–3.78 | 0.631 |
| Age at CMR | 1.05 | 1.00–1.10 | 0.044 | 1.08 | 1.03–1.14 | 0.003 |
| Age at corrective surgery | 1.01 | 1.00–1.03 | 0.019 | 1.02 | 1.01–1.03 | <0.001 |
| Correction during the 1st year of life | 0.23 | 0.08–0.70 | 0.009 | 0.05 | 0.00–0.89 | 0.030 |
| Palliative shunt | 2.58 | 0.74–8.98 | 0.137 | 0.19 | 0.06–1.63 | 0.047 |
| Palliative shunt duration | 1.07 | 0.87–1.32 | 0.502 | 1.24 | 1.01–1.53 | 0.043 |
| Residual_VSD | 1.33 | 0.39–4.49 | 0.651 | 5.06 | 1.44–17.79 | 0.012 |
| Residual VSD_duration | 1.04 | 0.98–1.11 | 0.186 | 1.09 | 1.02–1.16 | 0.008 |
| Right-sided aortic arch | 0.49 | 0.18–1.32 | 0.157 | 2.81 | 0.73–10.79 | 0.133 |
| AR moderate to severe | 0.16 | 0.009–3.36 | 0.991 | 3.38 | 0.89–6.92 | 0.013 |
| AR_fraction | 1.06 | 0.99–1.13 | 0.106 | 1.20 | 1.07– 1.34 | 0.002 |
| AVR | 0.16 | 0.009–3.36 | 0.991 | 3.38 | 0.89–6.92 | 0.003 |
| Ascending aorta replacement | 0.24 | 0.01–5.11 | 0.992 | 30.2 | 1.35–67.11 | 0.992 |
| TAP | 1.05 | 0.38–2.92 | 0.930 | 2.21 | 0.57–8.59 | 0.252 |
| PR fraction | 1.02 | 0.99–1.05 | 0.153 | 1.02 | 0.98–1.05 | 0.328 |
| PVR | 2.83 | 1.05–7.63 | 0.040 | 8.80 | 2.69–28.78 | <0.001 |
| Arterial hypertension | 0.38 | 0.03–4.39 | 0.439 | 1.56 | 0.13–18.18 | 0.725 |
| SBP | 0.99 | 0.96–1.03 | 0.561 | 0.98 | 0.94–1.02 | 0.352 |
| DBP | 1.03 | 0.99–1.07 | 0.160 | 1.02 | 0.98–1.07 | 0.319 |
| NYHA > II | 0.06 | 0.003–1.08 | 0.030 | 12.92 | 2.34–71.47 | 0.003 |
| Dilated SoV Group | Dilated AAo Group | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| AR fraction | - | - | - | 1.19 | 1.01–1.40 | 0.031 |
| PVR | - | - | - | 6.41 | 1.01–40.61 | 0.048 |
| Age at corrective surgery | 1.00 | 0.98–1.02 | 0.825 | 0.99 | 0.96–1.02 | 0.775 |
| Correction during the 1st year of life | 0.36 | 0.09–1.45 | 0.152 | 1.00 | - | - |
| Age at CMR | 1.01 | 0.94–1.09 | 0.694 | 0.93 | 0.81–1.06 | 0.310 |
| Shunt | - | - | - | 1.00 | - | - |
| Shunt duration | - | - | - | 1.42 | 0.91–2.21 | 0.115 |
| Residual VSD | - | - | - | 0.26 | 0.006–11.58 | 0.486 |
| VSD duration | - | - | - | 1.12 | 0.94–1.32 | 0.190 |
| NYHA > II | 2.10 | 0.84–5.23 | 0.109 | 0.91 | 0.49–1.68 | 0.779 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammed, A.F.A.; Frick, M.; Kerst, G.; Hatam, N.; Elgamal, M.-A.F.; Essa, K.M.; Hövels-Gürich, H.H.; Vazquez-Jimenez, J.F.; Zayat, R. Proximal Aortic Dilatation and Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot: Is There a Relationship? A Cardiac Magnetic Resonance Imaging Study. J. Clin. Med. 2021, 10, 5296. https://doi.org/10.3390/jcm10225296
Mohammed AFA, Frick M, Kerst G, Hatam N, Elgamal M-AF, Essa KM, Hövels-Gürich HH, Vazquez-Jimenez JF, Zayat R. Proximal Aortic Dilatation and Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot: Is There a Relationship? A Cardiac Magnetic Resonance Imaging Study. Journal of Clinical Medicine. 2021; 10(22):5296. https://doi.org/10.3390/jcm10225296
Chicago/Turabian StyleMohammed, Ahmed Farghal A., Michael Frick, Gunter Kerst, Nima Hatam, Mohamed-Adel F. Elgamal, Karam M. Essa, Hedwig H. Hövels-Gürich, Jaime F. Vazquez-Jimenez, and Rashad Zayat. 2021. "Proximal Aortic Dilatation and Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot: Is There a Relationship? A Cardiac Magnetic Resonance Imaging Study" Journal of Clinical Medicine 10, no. 22: 5296. https://doi.org/10.3390/jcm10225296
APA StyleMohammed, A. F. A., Frick, M., Kerst, G., Hatam, N., Elgamal, M.-A. F., Essa, K. M., Hövels-Gürich, H. H., Vazquez-Jimenez, J. F., & Zayat, R. (2021). Proximal Aortic Dilatation and Pulmonary Valve Replacement in Patients with Repaired Tetralogy of Fallot: Is There a Relationship? A Cardiac Magnetic Resonance Imaging Study. Journal of Clinical Medicine, 10(22), 5296. https://doi.org/10.3390/jcm10225296






