Social Inequities in the Impact of COVID-19 Lockdown Measures on the Mental Health of a Large Sample of the Colombian Population (PSY-COVID Study)
Abstract
:1. Introduction
2. Materials and Methods
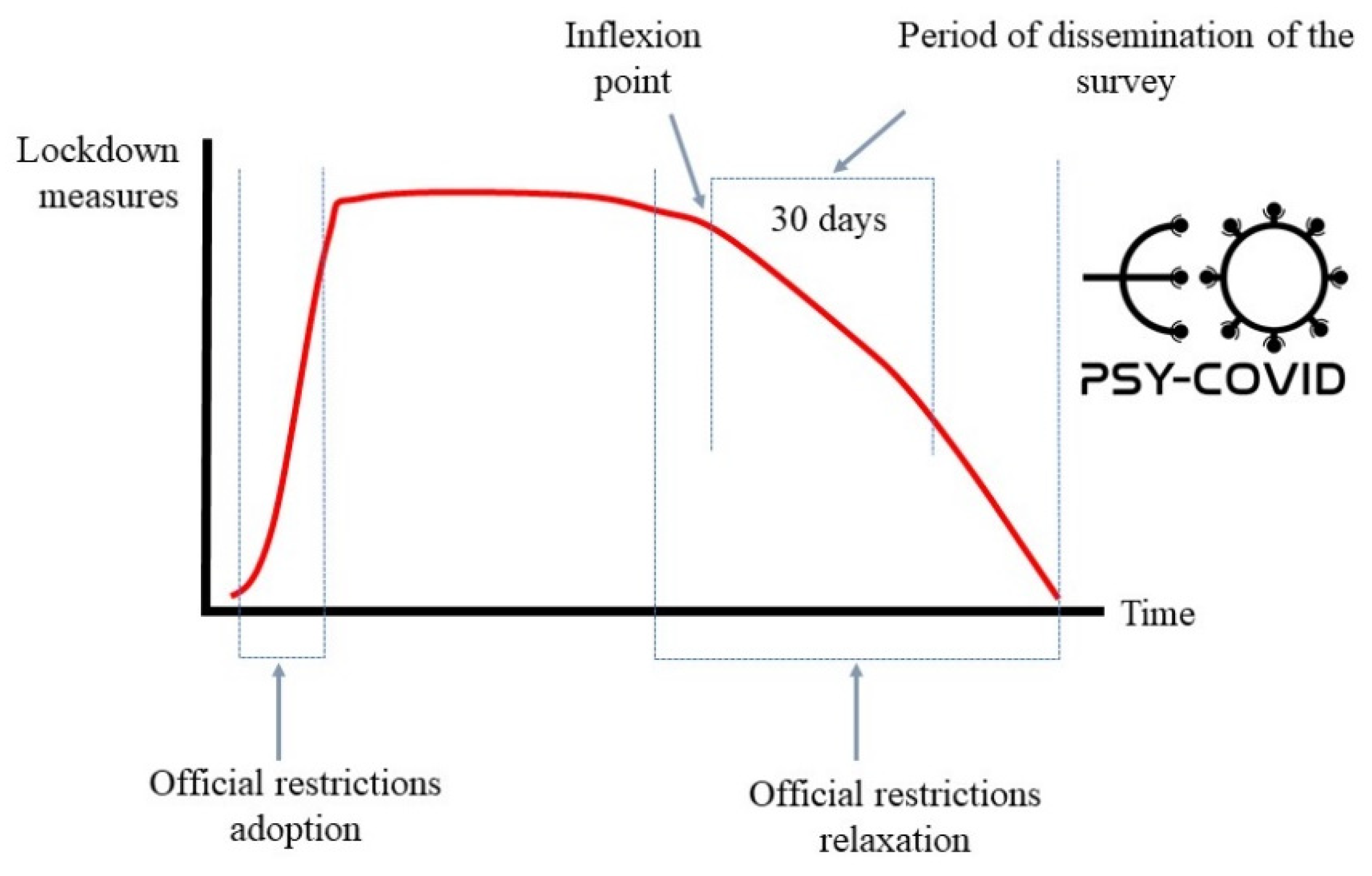
2.1. Study Design
2.2. Participants
2.3. Procedure
2.4. Measures
2.4.1. Socio-Demographic Characteristics
2.4.2. Mental Health Outcomes
2.5. Data Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Impact of COVID-19 Lockdown Measures on the Mental Health
3.2.1. Prevalence
3.2.2. Social Determinants of Health
Gender
Age Group
Income Level
Work Status
Education Level
Ethnic Group
Area of Residence
Region
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Planchuelo-Gómez, Á.; Odriozola-González, P.; Irurtia, M.J.; de Luis-García, R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020, 277, 842–849. [Google Scholar] [CrossRef]
- World Health Organization WHO. WHO Coronavirus Disease (COVID-19). Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 11 January 2021).
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Pedrosa, A.L.; Bitencourt, L.; Fróes, A.C.F.; Cazumbá, M.L.B.; Campos, R.G.B.; de Brito, S.B.C.S.; e Silva, A.C.S. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front. Psychol. 2020, 11, 566212. [Google Scholar] [CrossRef]
- Last, J.M. A Dictionary of Epidemiology; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Solar, O.; Irwin, A. Social determinants, political contexts and civil society action: A historical perspective on the Commission on Social Determinants of Health. Health Promot. J. Austr. 2006, 17, 180–5185. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Jain, R.; Singh, H.P. Epidemiological models of SARS-CoV-2 (COVID-19) to control the transmission based on current evidence: A systematic review. Preprints 2020, 2020070262. [Google Scholar]
- Marmot, M. The influence of income on health: Views of an epidemiologist. Health Aff. 2002, 21, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, R.; Marmot, M. Social Determinant of Health. J. Public Health Policy 2009. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Ren, X.; Huang, W.; Pan, H.; Huang, T.; Wang, X.; Ma, Y. Mental health during the covid-19 outbreak in china: A meta-analysis. Psychiatr. Q. 2020, 91, 1033–1045. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Gammon, J.; Hunt, J.; Musselwhite, C. The stigmatization of source isolation: A literature review. J. Res. Nurs. 2019, 24, 677–693. [Google Scholar] [CrossRef] [Green Version]
- Morgan, D.J.; Diekema, D.J.; Sepkowitz, K.; Perencevich, E.N. Adverse outcomes associated with contact precautions: A review of the literature. Am. J. Infect. Control. 2009, 37, 85–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, A.; Pillai, D.R.; Lu, M.; Doolan, C.; Leal, J.; Kim, J.; Hollis, A. Impact of isolation precautions on quality of life: A meta-analysis. J. Hosp. Infect. 2020, 105, 35–42. [Google Scholar] [CrossRef]
- Abad, C.; Fearday, A.; Safdar, N. Adverse effects of isolation in hospitalised patients: A systematic review. J. Hosp. Infect. 2010, 76, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Barratt, R.; Shaban, R.; Moyle, W. Patient experience of source isolation: Lessons for clinical practice. Contemp. Nurse 2011, 39, 180–193. [Google Scholar] [CrossRef]
- Purssell, E.; Gould, D.; Chudleigh, J. Impact of isolation on hospitalised patients who are infectious: Systematic review with meta-analysis. BMJ Open 2020, 10, e030371. [Google Scholar] [CrossRef]
- Hossain, M.D.; Sultana, A.; Purohit, N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol. Health 2016, 42, e2020038. [Google Scholar] [CrossRef]
- Jeong, H.; Woo-Yim, H.; Song, Y.J.; Ki, M.; Min, J.A.; Cho, J.; Chae, J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Alzueta, E.; Perrin, P.; Baker, F.C.; Caffarra, S.; Ramos-Usuga, D.; Yuksel, D.; Arango-Lasprilla, J.C. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 2020, 77, 556–570. [Google Scholar] [CrossRef] [PubMed]
- Li, L.Z.; Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020, 291, 113267. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Sutin, A.R.; Robinson, E. Depression reported by US adults in 2017–2018 and March and April 2020. J. Affect. Disord. 2020, 278, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Goularte, J.F.; Serafim, S.D.; Colombo, R.; Hogg, B.; Caldieraro, M.A.; Rosa, A.R. COVID-19 and mental health in brazil: Psychiatric symptoms in the general population. J. Psychiatr. Res. 2020, 132, 32–37. [Google Scholar] [CrossRef]
- Khan, K.S.; Mamun, M.A.; Griffiths, M.D.; Ullah, I. The Mental health impact of the COVID-19 pandemic across different cohorts. Int. J. Ment. Health Addict. 2020, 9, 1–7. [Google Scholar] [CrossRef]
- Salerno, J.P.; Williams, N.D.; Gattamorta, K.A. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychol. Trauma 2020, 12 (Suppl. S1), S239–S242. [Google Scholar] [CrossRef]
- Wood, L.J.; Davies, A.P.; Khan, Z. COVID-19 precautions: Easier said than done when patients are homeless. Med. J. Aust. 2020, 212, 384.e1. [Google Scholar] [CrossRef] [Green Version]
- Ministerio de Salud y Protección Social. Encuesta Nacional de Salud Mental; Ministerio de Salud y Protección Social: Bogotá, Colombia, 2015. Available online: http://www.odc.gov.co/Portals/1/publicaciones/pdf/consumo/estudios/nacionales/CO031102015-salud_mental_tomoI.pdf (accessed on 15 January 2021).
- Benjamins, M.R.; Silva, A.; Saliyed, N.S.; de Maio, F.G. Comparison of all-cause mortality rates and inequities between black and white populations across the 30 most populous US cities. JAMA Netw. Open 2021, 4, e2032086. [Google Scholar] [CrossRef]
- Jahromi, A.H.; Hamidianjahromi, A. Why african americans are a potential target for COVID-19 infection in the United States. J. Med. Internet Res. 2020, 22, e19934. [Google Scholar] [CrossRef]
- Marí-Dell’Olmo, M.; Gotsens, M.; Pasarín, M.I.; Rodríguez-Sanz, M.; Artazcoz, L.; García de Olalla, P.; Rius, C.; Borrell, C. Socioeconomic inequalities in COVID-19 in a European urban area: Two waves, two patterns. Int. J. Environ. Res. Public Health 2021, 18, 1256. [Google Scholar] [CrossRef]
- Golsdtein, J.R.; Atherwood, S. Improved measurement of racial/ethnic disparities in COVID-19 mortality in the United States. MedRxiv 2020. [Google Scholar] [CrossRef]
- Horton, R. COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Cifuentes, M.P.; Rodríguez-Villamizar, L.A.; Rojas-Botero, M.L.; Álvarez-Moreno, C.; Fernández-Niño, J.A. Socioeconomic inequalities associated with mortality for COVID-19 in Colombia: A cohort nation-wide study. Medrxiv 2020. [Google Scholar] [CrossRef]
- Calderón-Larrañaga, A.; Vetrano, D.L.; Rizzuto, D.; Bellander, T.; Fratiglioni, L.; Dekhtyar, S. High excess mortality in areas with young and socially vulnerable populations during the COVID-19 outbreak in Stockholm Region, Sweden. BMJ Glob. Health 2020, 5, e003595. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Calderón-Villarreal, A.; Bojorquez, I.; Hernández, C.V.; Schriger, D.L.; Hirashima, E.T. Excess out-of-hospital mortality and declining oxygen saturation: The sentinel role of emergency medical services data in the COVID-19 crisis in Tijuana, Mexico. Ann. Emerg. Med. 2020, 76, 413–426. [Google Scholar] [CrossRef] [PubMed]
- Cediel-Sánchez, D.V.; Sánchez-Guerrero, D.E. Coeficiente de Gini Para Bogotá y Región; Alcaldía Mayor de Bogotá: Bogotá, Colombia, 2016. Available online: http://www.sdp.gov.co/sites/default/files/8._coeficiente_de_gini_para_bogota_y_region.pdf (accessed on 15 January 2021).
- The World Bank. PovcalNet: An Online Analysis Tool for Global Poverty Monitoring; The World Bank: Washington, DC, USA, 2020. Available online: http://iresearch.worldbank.org/PovcalNet/home.aspx (accessed on 5 January 2021).
- Johns Hopkins Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 5 January 2021).
- Panamerican Health Organization. Reportes de Situación COVID-19 Colombia. 2021. Available online: https://www.paho.org/es/reportes-situacion-covid-19-colombia (accessed on 5 January 2021).
- Lowy Institute. COVID Performance Index. Deconstructing Pandemic Responses. 2021. Available online: https://interactives.lowyinstitute.org/features/covid-performance/ (accessed on 5 January 2021).
- Cano-Vindel, A.; Muñoz-Navarro, R.; Medrano, L.A.; Ruiz-Rodríguez, P.; González-Blanch, C.; Gómez-Castillo, M.D.; Capafons, A.; Chacón, F.; Santolaya, F. A computerized version of the Patient Health Questionnaire-4 as an ultra-brief screening tool to detect emotional disorders in primary care. J. Affect. Disord. 2018, 234, 247–255. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Sanabria-Mazo, J.P.; Gómez-Acosta, A.; Castro-Muñoz, J.A.; Rojas, Y.F.; Soler, A.F.; Luciano, J.V.; Sanz, A. Psychometric properties of the online version of the Patient Health Questionnaire-4 in a large Colombian sample: Results from the PSY-COVID study. OSF Prepr. 2021. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Stolk, R.P.; Löwe, B.; Rief, W.; White, P.D.; Rosmalen, J.G. How to assess common somatic symptoms in large-scale studies: A systematic review of questionnaires. J. Psychosom. Res. 2013, 74, 459–468. [Google Scholar] [CrossRef]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H.; et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 2021, 279, 462–472. [Google Scholar] [CrossRef]
- Caballero, C.; De Luque, J.G.; Campo, A. Social capital and psychological distress during Colombian coronavirus disease lockdown. J. Community Psychol. 2020, 49, 691–702. [Google Scholar] [CrossRef]
- Rivillas-García, J.C.; Murad-Rivera, R.; Marcela-Sánchez, S.; Rivera-Montero, D.; Calderón-Jaramillo, M.; Castaño, L.M.; Royo, M. Respuesta social a las medidas del gobierno para controlar el nuevo coronavirus durante la etapa temprana en Colombia, 8-20 de abril de 2020. Asoc. Profamilia 2020. [Google Scholar] [CrossRef]
- Departamento Administrativo Nacional de Estadística. Encuesta Pulso Social: Salud Mental en Colombia: Una Aproximación Desde las Estadísticas Oficiales en el Contexto de Pandemia; Departamento Administrativo Nacional de Estadística: Bogotá, Colombia, 2020. Available online: https://www.dane.gov.co/files/webinar/presentacion-webinar-salud-mental-en-colombia-21-10-2020.pdf (accessed on 5 January 2021).
- Sanabria-Mazo, J.P.; Useche-Aldana, B.; Ochoa, P.P.; Rojas-Gualdrón, D.F.; Sanz, A. Impacto de la pandemia de COVID-19 en la salud mental en Colombia; Editorial CES: Medellín, Colombia.
- Yao, H.; Chen, J.H.; Xu, Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet 2020, 7, e21. [Google Scholar] [CrossRef]
- Ehrenfeld, M.; Tincani, A.; Andreoli, L.; Cattalini, M.; Greenbaum, A.; Kanduc, D.; Alijotas-Reig, J.; Zinserling, V.; Semenova, N.; Amital, H.; et al. COVID-19 and autoimmunity. Autoimmun. Rev. 2020, 19, 102597. [Google Scholar] [CrossRef]
- Mendenhall, E. The COVID-19 syndemic is not global: Context matters. Lancet 2020, 396, 1731. [Google Scholar] [CrossRef]
| Variables, n (%) | Sample (n = 18,061) |
|---|---|
| Gender | |
| Female | 13,491 (74.7) |
| Male | 4495 (24.9) |
| Non-binary | 75 (0.4) |
| Age group | |
| Young adults (18–29 years) | 7739 (42.9) |
| Middle aged adults (30–59 years) | 9421 (52.1) |
| Older adults (≥60 years) | 901 (5.0) |
| Income level | |
| Low | 5173 (28.6) |
| Medium | 11,186 (61.9) |
| High | 1702 (9.5) |
| Work status | |
| Student | 3511 (19.5) |
| Informal workers | 2149 (11.9) |
| Formal workers | 8208 (45.5) |
| Unpaid workers | 515 (2.9) |
| Unemployed | 3024 (16.8) |
| Retired | 627 (3.4) |
| Education level | |
| No studies | 18 (0.1) |
| Primary | 322 (1.8) |
| Secondary | 1536 (8.5) |
| University | 16,185 (89.6) |
| Ethnic group | |
| Gypsy | 26 (0.1) |
| Afrodescendant | 953 (5.3) |
| Indigenous | 578 (3.2) |
| None of the above | 16,443 (91.4) |
| Area of residence | |
| Urban | 16,527 (91.8) |
| Rural | 1473 (8.2) |
| Region | |
| Amazon | 285 (1.6) |
| Andean | 9347 (51.9) |
| Caribbean | 1395 (7.8) |
| Orinoco | 557 (3.1) |
| Pacific | 6420 (35.6) |
| Variables, n (%) | Depression (PHQ-2) | Anxiety (GAD-2) | Somatization (SSQ-5) |
|---|---|---|---|
| Gender | |||
| Female | 36.0 | 30.7 | 35.0 |
| Male | 31.6 | 24.7 | 19.5 |
| Non-binary | 56.0 | 40.0 | 41.3 |
| Age group | |||
| Young adults (18–29 years) | 48.0 | 37.3 | 40.1 |
| Middle aged adults (30–59 years) | 26.0 | 23.7 | 25.8 |
| Older adults (≥60 years) | 17.4 | 17.9 | 10.5 |
| Income level | |||
| Low | 46.1 | 36.2 | 35.5 |
| Medium | 31.4 | 26.9 | 30.4 |
| High | 25.2 | 23.6 | 22.7 |
| Work status | |||
| Student | 46.0 | 35.6 | 37.8 |
| Informal workers | 30.7 | 26.6 | 27.5 |
| Formal workers | 32.4 | 27.9 | 30.5 |
| Unpaid workers | 36.7 | 30.3 | 28.2 |
| Unemployed | 34.1 | 28.7 | 30.8 |
| Retired | 23.8 | 21.5 | 18.7 |
| Education level | |||
| No studies | 38.9 | 44.4 | 50.0 |
| Primary | 37.3 | 33.2 | 25.8 |
| Secondary | 41.9 | 34.1 | 24.9 |
| University | 34.3 | 28.7 | 31.8 |
| Ethnic group | |||
| Gypsy | 50.0 | 34.6 | 23.1 |
| Afrodescendant | 38.1 | 30.9 | 27.6 |
| Indigenous | 37.5 | 31.5 | 27.9 |
| None of the above | 34.7 | 29.0 | 31.5 |
| Area of residence | |||
| Urban | 35.2 | 29.4 | 31.6 |
| Rural | 32.5 | 27.0 | 25.5 |
| Region | |||
| Amazon | 35.8 | 29.1 | 34.4 |
| Andean | 32.2 | 28.2 | 31.4 |
| Caribbean | 34.0 | 27.1 | 31.8 |
| Orinoco | 38.2 | 30.9 | 32.0 |
| Pacific | 39.0 | 31.0 | 30.6 |
| Variables | Depression (PHQ-2) | Anxiety (GAD-2) | Somatization (SSQ-5) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | PR (95% CI) | aPR (95% CI) | PR (95% CI) | aPR (95% CI) | |
| Gender | ||||||
| Female | 1.22 (1.13–1.31) | 1.17 (1.08–1.26) | 1.35 (1.25–1.46) | 1.21 (1.15–1.28) | 2.22 (2.04–2.41) | 1.71 (1.60–1.82) |
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-binary | 2.76 (1.74–4.37) | 2.5 (1.54–4.06) | 2.04 (1.28–3.25) | 1.42 (1.06–1.90) | 2.90 (1.82–4.62) | 2.12 (1.61–2.78) |
| Age group | ||||||
| Young adults (18–29 years) | 4.37 (3.66–5.22) | 3.56 (2.93–4.31) | 2.73 (2.29–3.26) | 1.84 (1.58–2.14) | 5.67 (4.56–7.05) | 3.07 (2.52–3.74) |
| Middle aged adults (30–59 years) | 1.67 (1.39–1.99) | 1.55 (1.28–1.88) | 1.43 (1.20–1.71) | 1.25 (1.08–1.46) | 2.95 (2.38–3.67) | 2.13 (1.75–2.59) |
| Older adults (≥ 60 years) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Income level | ||||||
| Low | 2.54 (2.25–2.87) | 1.76 (1.54–2.00) | 1.84 (1.62–2.08) | 1.23 (1.12–1.35) | 1.87 (1.65–2.12) | 1.26 (1.15–1.39) |
| Medium | 1.36 (1.21–1.53) | 1.15 (1.02–1.30) | 1.19 (1.05–1.34) | 1.03 (0.94–1.12) | 1.49 (1.32–1.68) | 1.19 (1.09–1.30) |
| High | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Work status | ||||||
| Student | 1.92 (1.72–2.15) | 1.48 (1.31–1.67) | 2.01 (1.64–2.46) | 1.21 (1.03–1.42) | 2.65 (2.14–3.28) | 1.30 (1.10–1.54) |
| Informal workers | 1.00 | 1.00 | 1.32 (1.07–1.64) | 1.02 (0.87–1.21) | 1.65 (1.32–2.06) | 1.08 (0.91–1.29) |
| Formal workers | 1.08 (0.97–1.20) | 1.12 (1.00–1.24) | 1.41 (1.16–1.71) | 1.09 (0.93–1.27) | 1.91 (1.56–2.35) | 1.16 (0.98–1.36) |
| Unpaid workers | 1.31 (1.07–1.60) | 1.33 (1.08–1.64) | 1.58 (1.21–2.07) | 1.16 (0.95–1.41) | 1.71 (1.29–2.26) | 1.11 (0.90–1.36) |
| Unemployed | 1.17 (1.04–1.32) | 1.03 (0.91–1.17) | 1.46 (1.19–1.80) | 1.02 (0.87–1.21) | 1.94 (1.56–2.40) | 1.11 (0.94–1.32) |
| Retired | 0.70 (0.57–0.86) | 1.05 (0.84–1.31) | 1.00 | 1.00 | 1.00 | 1.00 |
| Education level | ||||||
| No studies | 1.00 | 1.00 | 1.99 (0.78–5.04) | 1.36 (0.82–2.25) | 3.01 (1.19–7.64) | 1.85 (1.19–2.89) |
| Primary | 0.93 (0.35–2.47) | 1.59 (0.59–4.33) | 1.24 (0.98–1.56) | 1.22 (1.04–1.44) | 1.05 (0.79–1.38) | 1.18 (0.96–1.44) |
| Secondary | 1.13 (0.44–2.93) | 1.61 (0.60–4.28) | 1.29 (1.15–1.44) | 1.16 (1.07–1.25) | 1.00 | 1.00 |
| University | 0.82 (0.32–2.12) | 1.23 (0.46–3.27) | 1.00 | 1.00 | 1.41 (1.25–1.59) | 1.23 (1.12–1.34) |
| Ethnic group | ||||||
| Gypsy | 1.89 (0.87–4.07) | 2.05 (0.90–4.67) | 1.30 (0.58–2.91) | 1.22 (0.73–2.04) | 0.79 (0.31–1.98) | 1.06 (0.54–2.08) |
| Afrodescendant | 1.16 (1.01–1.33) | 1.03 (0.89–1.18) | 1.09 (0.95–1.26) | 1.01 (0.92–1.12) | 1.00 | 1.00 |
| Indigenous | 1.13 (0.96–1.35) | 1.03 (0.86–1.23) | 1.13 (0.94–1.35) | 1.07 (0.95–1.20) | 1.01 (0.80–1.28) | 1.05 (0.89–1.23) |
| None of the above | 1.00 | 1.00 | 1.00 | 1.00 | 1.20 (1.04–1.39) | 1.16 (1.05–1.29) |
| Area of residence | ||||||
| Urban | 1.13 (1.01–1.26) | 1.23 (1.09–1.39) | 1.13 (1.01–1.27) | 1.12 (1.03–1.22) | 1.35 (1.20–1.53) | 1.23 (1.13–1.34) |
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Region | ||||||
| Amazon | 1.00 | 1.00 | 1.11 (0.83–1.46) | 1.03 (0.84–1.25) | 1.19 (0.93–1.53) | 1.08 (0.92–1.26) |
| Andean | 0.85 (0.67–1.09) | 1.03 (0.80–1.34) | 1.06 (0.93–1.20) | 1.08 (0.98–1.18) | 1.04 (0.97–1.11) | 1.02 (0.97–1.07) |
| Caribbean | 0.92 (0.71–1.21) | 1.05 (0.79–1.39) | 1.00 | 1.00 | 1.06 (0.93–1.20) | 1.01 (0.93–1.10) |
| Orinoco | 1.11 (0.83–1.49) | 1.33 (0.97–1.81) | 1.20 (0.97–1.49) | 1.16 (1.01–1.35) | 1.07 (0.89–1.29) | 1.07 (0.95–1.21) |
| Pacific | 1.15 (0.90–1.47) | 1.25 (0.96–1.61) | 1.21 (1.06–1.37) | 1.13 (1.03–1.24) | 1.00 | 1.00 |
| Main Recommendations |
|---|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanabria-Mazo, J.P.; Useche-Aldana, B.; Ochoa, P.P.; Rojas-Gualdrón, D.F.; Mateo-Canedo, C.; Carmona-Cervelló, M.; Crespo-Puig, N.; Selva-Olid, C.; Muro, A.; Méndez-Ulrich, J.L.; et al. Social Inequities in the Impact of COVID-19 Lockdown Measures on the Mental Health of a Large Sample of the Colombian Population (PSY-COVID Study). J. Clin. Med. 2021, 10, 5297. https://doi.org/10.3390/jcm10225297
Sanabria-Mazo JP, Useche-Aldana B, Ochoa PP, Rojas-Gualdrón DF, Mateo-Canedo C, Carmona-Cervelló M, Crespo-Puig N, Selva-Olid C, Muro A, Méndez-Ulrich JL, et al. Social Inequities in the Impact of COVID-19 Lockdown Measures on the Mental Health of a Large Sample of the Colombian Population (PSY-COVID Study). Journal of Clinical Medicine. 2021; 10(22):5297. https://doi.org/10.3390/jcm10225297
Chicago/Turabian StyleSanabria-Mazo, Juan P., Bernardo Useche-Aldana, Pedro P. Ochoa, Diego F. Rojas-Gualdrón, Corel Mateo-Canedo, Meritxell Carmona-Cervelló, Neus Crespo-Puig, Clara Selva-Olid, Anna Muro, Jorge L. Méndez-Ulrich, and et al. 2021. "Social Inequities in the Impact of COVID-19 Lockdown Measures on the Mental Health of a Large Sample of the Colombian Population (PSY-COVID Study)" Journal of Clinical Medicine 10, no. 22: 5297. https://doi.org/10.3390/jcm10225297
APA StyleSanabria-Mazo, J. P., Useche-Aldana, B., Ochoa, P. P., Rojas-Gualdrón, D. F., Mateo-Canedo, C., Carmona-Cervelló, M., Crespo-Puig, N., Selva-Olid, C., Muro, A., Méndez-Ulrich, J. L., Feliu-Soler, A., Luciano, J. V., & Sanz, A. (2021). Social Inequities in the Impact of COVID-19 Lockdown Measures on the Mental Health of a Large Sample of the Colombian Population (PSY-COVID Study). Journal of Clinical Medicine, 10(22), 5297. https://doi.org/10.3390/jcm10225297









