Impact of Post-Procedural Change in Left Ventricle Systolic Function on Survival after Percutaneous Edge-to-Edge Mitral Valve Repair
Abstract
:1. Introduction
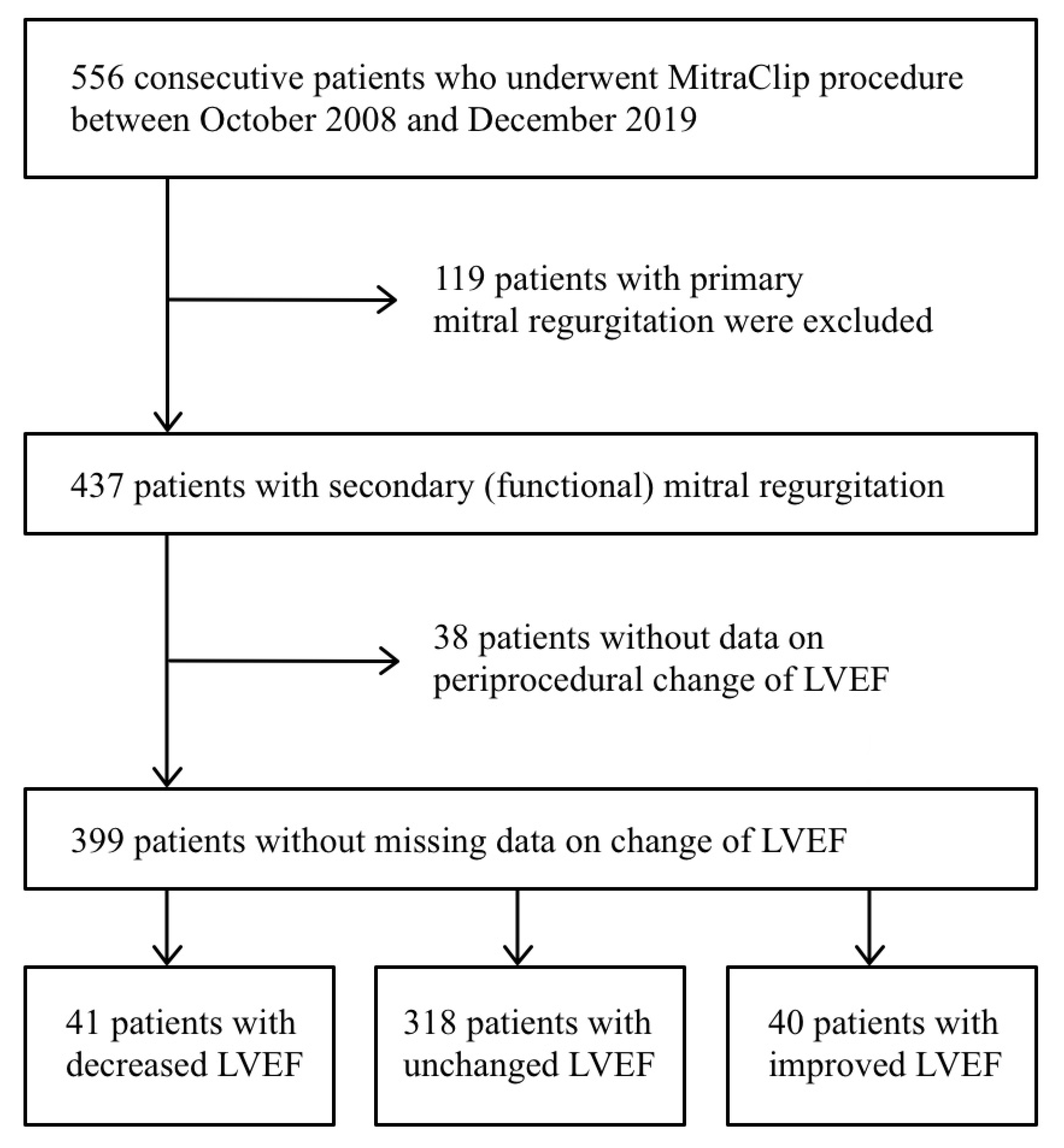
2. Materials and Methods
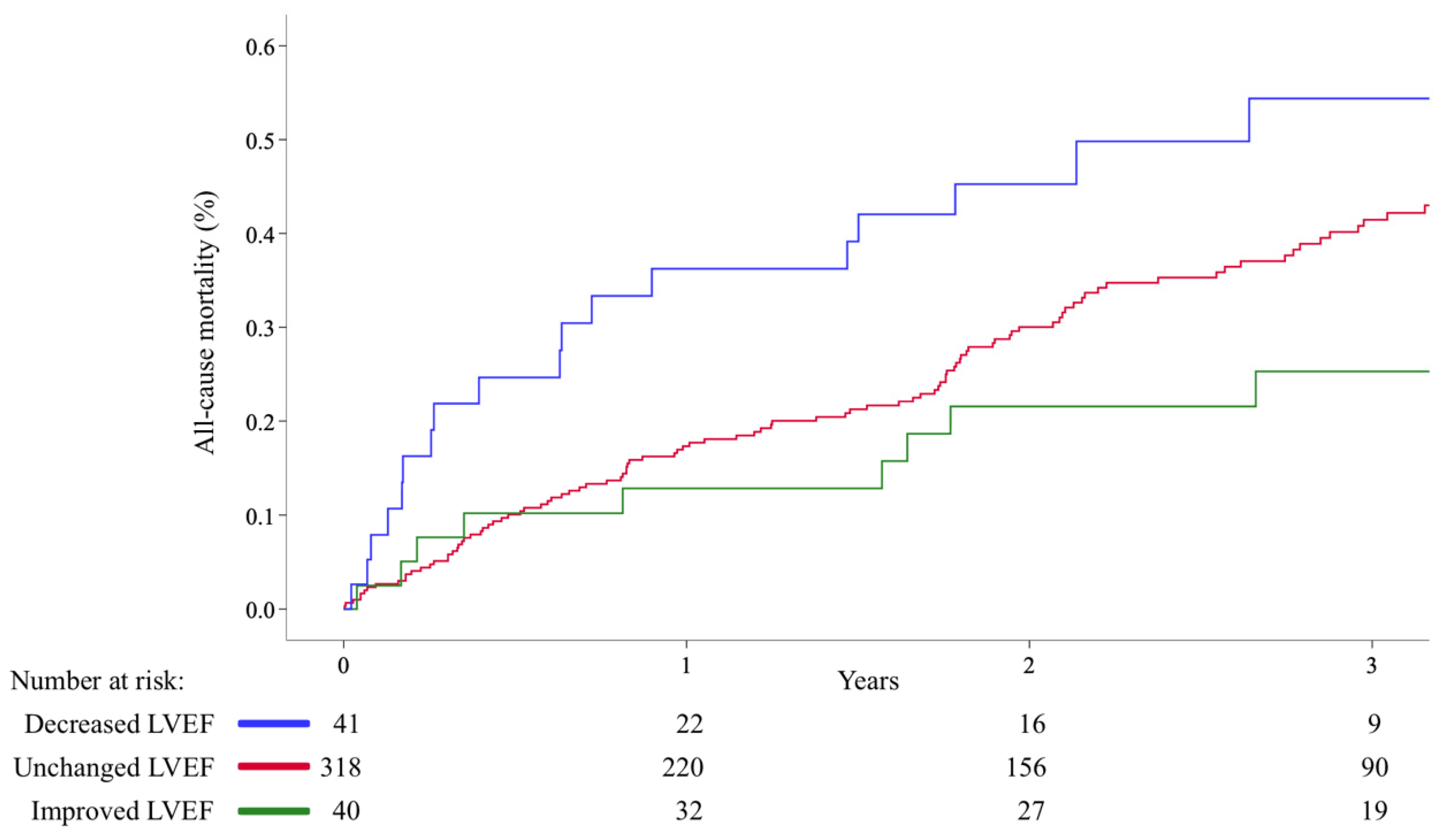
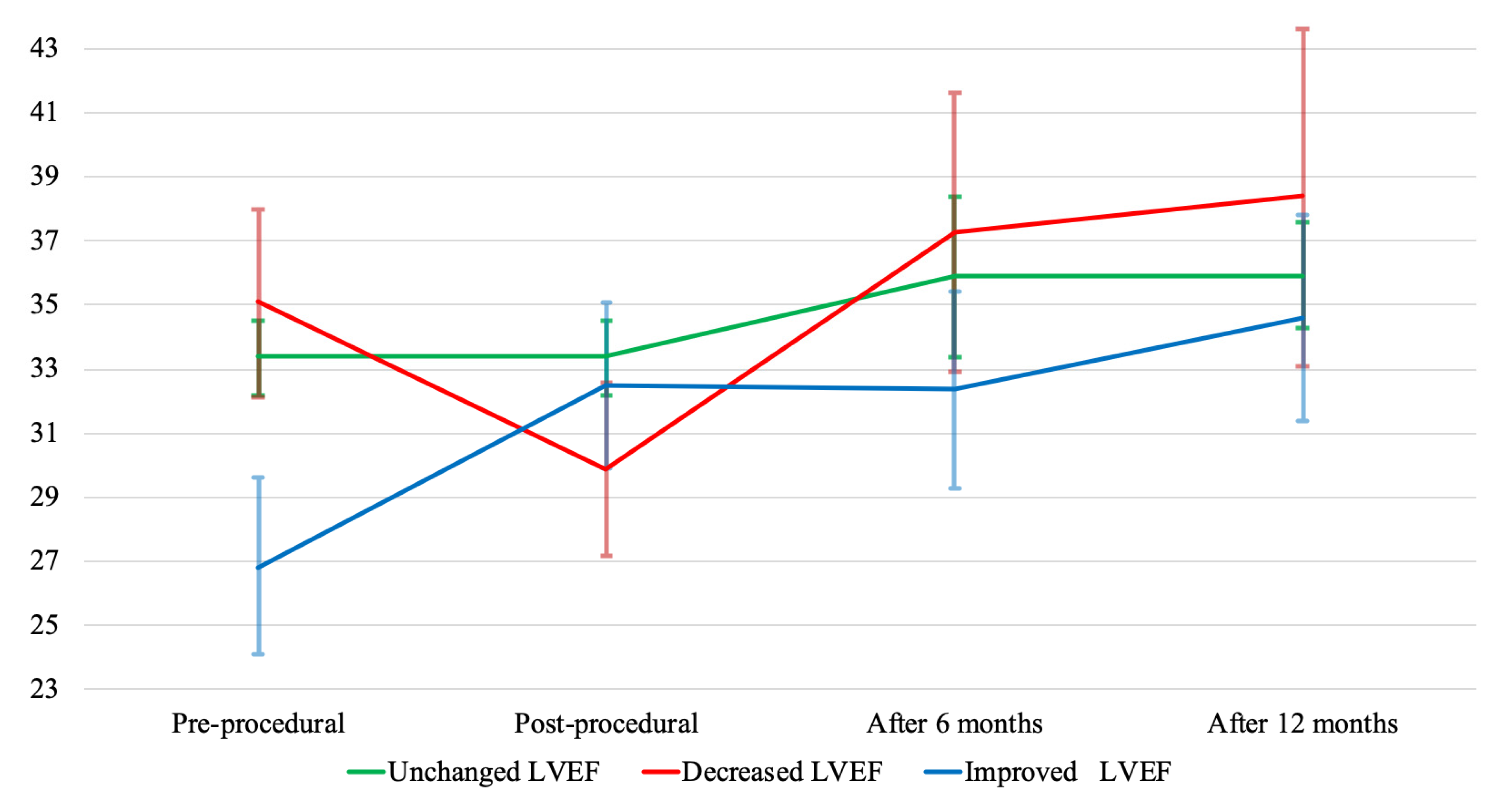
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations and Acronyms
| CI | confidence interval |
| eGFR | estimated glomerular filtration rate |
| GRASP | the Getting Reduction of mitrAl inSufficiency by Percutaneous clip implantation registry |
| HR | hazard ratio |
| IQR | interquartile range |
| LVEDD | left ventricle end-diastolic diameter |
| LVEF | left ventricle ejection fraction |
| MR | mitral regurgitation |
| NYHA | New York Heart Association |
| SD | standard deviation |
References
- Ross, J. Afterload mismatch in aortic and mitral valve disease: Implications for surgical therapy. J. Am. Coll. Cardiol. 1985, 5, 811–826. [Google Scholar] [CrossRef] [Green Version]
- Melisurgo, G.; Ajello, S.; Pappalardo, F.; Guidotti, A.; Agricola, E.; Kawaguchi, M.; Latib, A.; Covello, R.D.; Denti, P.; Zangrillo, A.; et al. Afterload Mismatch After MitraClip Insertion for Functional Mitral Regurgitation. Am. J. Cardiol. 2014, 113, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
- Jogani, S.; Van de Heyning, C.; Paelinck, B.P.; De Bock, D.; Mertens, P.; Heidbuchel, H.; Claeys, M.J. Afterload Mismatch After MitraClip Implantation: Intraoperative Assessment and Prognostic Implications. J. Invasive Cardiol 2020, 32, 88–93. [Google Scholar] [PubMed]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef] [Green Version]
- Enriquez-Sarano, M.; Akins, C.W.; Vahanian, A. Mitral regurgitation. Lancet 2009, 373, 1382–1394. [Google Scholar] [CrossRef]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Muñoz, D.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, R.; Silverio, A.; Baldi, C.; Di Maio, M.; Prota, C.; Radano, I.; Rey, J.; Herrmann, E.; Citro, R.; Piscione, F.; et al. Transcatheter Repair of Functional Mitral Regurgitation in Heart Failure Patients—A Meta-Analysis of 23 Studies on MitraClip Implantation. Circ. J. 2018, 82, 2800–2810. [Google Scholar] [CrossRef] [Green Version]
- Takagi, H.; Ando, T.; Umemoto, T.; ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. A review of comparative studies of MitraClip versus surgical repair for mitral regurgitation. Int. J. Cardiol. 2017, 228, 289–294. [Google Scholar] [CrossRef]
- Essandoh, M.K. Afterload Mismatch After MitraClip Implantation: The Potential Impact of Pharmacologic Support. J. Cardiothorac. Vasc. Anesthesia 2017, 31, 702–706. [Google Scholar] [CrossRef]
- Freixa, X.; Hernández, M.; Farrero, M.; Sitges, M.; Jiménez, G.; Regueiro, A.; Fita, G.; Tatjer, I.; Andrea, R.; Martín-Yuste, V.; et al. Levosimendan as an adjunctive therapy to MitraClip implantation in patients with severe mitral regurgitation and left ventricular dysfunction. Int. J. Cardiol. 2016, 202, 517–518. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Kraft, C.D.; Levine, R.A.; Nihoyannopoulos, P.; Otto, C.M.; Quinones, M.A.; Rakowski, H.; et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and doppler echocardiography. J. Am. Soc. Echocardiogr. 2003, 16, 777–802. [Google Scholar] [CrossRef]
- Grasso, C.; Baldus, S. The MitraClip transcatheter mitral valve repair system. EuroIntervention 2015, 14, W45–W46. [Google Scholar] [CrossRef]
- Stone, G.W.; Adams, D.H.; Abraham, W.T.; Kappetein, A.P.; Généreux, P.; Vranckx, P.; Mehran, R.; Kuck, K.-H.; Leon, M.B.; Piazza, N.; et al. Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: Part 2: Endpoint definitionsA consensus document from the Mitral Valve Academic Research Consortium. Eur. Heart J. 2015, 36, 1878–1891. [Google Scholar] [CrossRef]
- Siegel, R.J.; Biner, S.; Rafique, A.M.; Rinaldi, M.; Lim, S.; Fail, P.; Hermiller, J.; Smalling, R.; Whitlow, P.L.; Herrmann, H.C.; et al. The Acute Hemodynamic Effects of MitraClip Therapy. J. Am. Coll. Cardiol. 2011, 57, 1658–1665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azzalini, L.; Millán, X.; Khan, R.; Couture, P.; Ducharme, A.; Basmadjian, A.; Bonan, R.; Asgar, A.W. Impact of left ventricular function on clinical outcomes of functional mitral regurgitation patients undergoing transcatheter mitral valve repair. Catheter. Cardiovasc. Interv. 2016, 88, 1124–1133. [Google Scholar] [CrossRef]
- Cimino, S.; Maestrini, V.; Cantisani, D.; Petronilli, V.; Filomena, D.; Mancone, M.; Sardella, G.; Fedele, F.; Lancellotti, P.; Agati, L. 2D/3D echocardiographic determinants of left ventricular reverse remodelling after MitraClip implantation. Eur. Hear. J.-Cardiovasc. Imaging 2018, 20, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, H.J.; Heijer, M.C.D.; Paelinck, B.P.; Debonnaire, P.; Vanderheyden, M.; Van De Heyning, C.M.; De Bock, D.; Coussement, P.; Saad, G.; Ferdinande, B.; et al. Left ventricular remodelling patterns after MitraClip implantation in patients with severe mitral valve regurgitation: Mechanistic insights and prognostic implications. Eur. Hear. J.-Cardiovasc. Imaging 2018, 20, 307–313. [Google Scholar] [CrossRef]
- Velu, J.F.; Baan, J., Jr.; de Bruin-Bon, H.A.C.M.; van Mourik, M.S.; Nassif, M.; Koch, K.T.; Vis, M.M.; van den Brink, R.B.; Boekholdt, S.M.; Piek, J.J.; et al. Can stress echocardiography identify patients who will benefit from percutaneous mitral valve repair? Int. J. Cardiovasc. Imaging 2019, 35, 645–651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, R.; Haluska, B.; Leung, D.; Case, C.; Mundy, J.; Marwick, T.H. Functional and prognostic implications of left ventricular contractile reserve in patients with asymptomatic severe mitral regurgitation. Heart 2005, 91, 1407–1412. [Google Scholar] [CrossRef] [Green Version]
- Giannini, C.; D’Ascenzo, F.; Fiorelli, F.; Spontoni, P.; Swaans, M.J.; Velazquez, E.J.; Armeni, P.; Adamo, M.; De Carlo, M.; Petronio, A.S. A meta-analysis of MitraClip combined with medical therapy vs. medical therapy alone for treatment of mitral regurgitation in heart failure patients. ESC Heart Fail. 2018, 5, 1150–1158. [Google Scholar] [CrossRef]
- Orban, M.; Orban, M.; Lesevic, H.; Braun, D.; Deseive, S.; Sonne, C.; Hutterer, L.; Grebmer, C.; Khandoga, A.; Pache, J.; et al. Predictors for long-term survival after transcatheter edge-to-edge mitral valve repair. J. Interv. Cardiol. 2017, 30, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Foerst, J.; Cardenas, A.; Swank, G. Safety of MitraClip Implant in the Unstable Patient: Feasibility of Concomitant Left Ventricular Support Device. JACC Cardiovasc. Interv. 2016, 9, e71–e72. [Google Scholar] [CrossRef] [PubMed]
| Overall Series | Unchanged LVEF | Decreased LVEF | Improved LVEF | p-Value | |
|---|---|---|---|---|---|
| n | 399 | 318 | 41 | 40 | |
| Age (years) | 72.6 ± 8.9 | 72.7 ± 8.4 | 72.9 ± 11.8 | 71.9 ± 8.9 | 0.389 |
| Gender (male), n (%) | 239 (60) | 190 (60) | 23 (56) | 26 (65) | 0.711 |
| Diabetes, n (%) | 154 (39) | 133 (42) | 11 (27) | 10 (25) | 0.148 |
| Hypertension, n (%) | 317 (79) | 256 (81) | 30 (73) | 31 (78) | 0.522 |
| Previous CABG, n (%) | 84 (21) | 64 (20) | 8 (20) | 12 (30) | 0.341 |
| Atrial fibrillation, n (%) | 185 (46) | 141 (44) | 29 (71) | 15 (38) | 0.003 |
| eGFR (mL/min/1.73 m2) | 50.6 (35.6–66.8) | 50.1 (35.3–66.4) | 61.1 (36.4–71.1) | 53.5 (42.0–71.1) | 0.549 |
| ProBNP (pg/mL) | 709 (323–2324) | 674 (322–2446) | 787 (341–1894) | 1087 (320–2044) | 0.800 |
| EuroSCORE II | 6.2 (3.6–10.8) | 6.1 (3.6–10.8) | 6.1 (3.8–11.2) | 7.2 (3.3–11.3) | 0.759 |
| Ischemic MR, n (%) | 206 (52) | 161 (51) | 26 (63) | 19 (48) | 0.178 |
| ICD-pacemaker, n (%) | 100 (25) | 78 (25) | 41 (22) | 40 (33) | 0.487 |
| CRT-pacemaker, n (%) | 40 (10) | 31 (10) | 6 (15) | 3 (8) | 0.529 |
| NYHA II, n (%) | 55 (14) | 42 (13) | 5 (12) | 8 (20) | 0.478 |
| NYHA III, n (%) | 296 (74) | 241 (76) | 29 (71) | 26 (65) | 0.295 |
| NYHA IV, n (%) | 48 (12) | 35 (11) | 7 (17) | 6 (15) | 0.442 |
| LVEF (%) | 32.9 ± 10.6 | 33.4 ± 10.8 | 35.1 ± 9.3 | 26.8 ± 8.6 | <0.001 |
| MR grade III, n (%) | 117 (31) | 94 (32) | 9 (23) | 14 (36) | 0.435 |
| MR grade IV, n (%) | 255 (69) | 200 (68) | 30 (77) | 25 (64) | 0.435 |
| LVEDD (mm) | 60.6 ± 10.8 | 60.2 ± 11.0 | 61.2 ± 9.6 | 61.9 ± 9.7 | 0.378 |
| LVESD (mm) | 47.1 ± 12.0 | 48.8 ± 12.2 | 47.7 ± 11.4 | 48.7 ± 11.5 | 0.710 |
| TAPSE (mm) | 18.0 ± 4.2 | 18.2 ± 4.2 | 17.2 ± 4.9 | 17.3 ± 3.4 | 0.190 |
| PASP (mmHg) | 47.0 ± 13.2 | 46.7 ± 12.9 | 47.9 ± 13.3 | 48.3 ± 16.2 | 0.716 |
| Left atrial area (cm2) | 27.8 ± 8.4 | 27.4 ± 8.1 | 30.1 ± 10.2 | 28.3 ± 9.1 | 0.343 |
| Variable | Univariate Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Gender (male) | 1.43 (1.02–2.01) | 0.038 | 1.62 (1.15–2.29) | 0.006 |
| NYHA Class III | 1.52 (0.87–2.65) | 0.144 | 1.26 (0.72–2.22) | 0.419 |
| NYHA Class IV | 4.18 (2.22–7.87) | <0.001 | 3.88 (2.05–7.37) | <0.001 |
| eGFR | 0.98 (0.98–0.99) | <0.001 | 0.98 (0.98–0.99) | <0.001 |
| LVEF decreased | 1.59 (0.98–2.56) | 0.062 | 2.05 (1.26–3.34) | 0.004 |
| LVEF improved | 0.53 (0.29–0.99) | 0.045 | 0.47 (0.24–0.91) | 0.024 |
| Unchanged LVEF | Decreased LVEF | Improved LVEF | p-Value | n (%) | |
|---|---|---|---|---|---|
| Pre-procedural LVEF, % | 33.4 ± 10.8 | 35.1 ± 9.3 | 26.8 ± 8.6 | <0.001 | 399 (100) |
| Post-procedural LVEF, % | 33.4 ± 10.8 | 29.9 ± 8.6 | 32.5 ± 8.1 | 0.251 | 399 (100) |
| LVEF after 6 months, % | 34.9 ± 10.4 | 37.3 ± 9.0 | 32.4 ± 7.8 | 0.287 | 235 (59) |
| LVEF after 12 months, % | 35.9 ± 10.6 | 38.4 ± 10.2 | 34.6 ± 7.4 | 0.558 | 199 (50) |
| Pre-procedural LVEDD, mm | 60.2 ± 11.0 | 61.2 ± 9.6 | 62.9 ± 9.7 | 0.378 | 357 (89) |
| LVEDD at 6 months, mm | 58.2 ± 9.4 | 56.1 ± 7.8 | 62.5 ± 10.2 | 0.084 | 229 (57) |
| LVEDD at 12 months, mm | 57.6 ± 10.2 | 53.5 ± 6.2 | 61.9 ± 7.7 | 0.012 | 189 (47) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hagnäs, M.J.; Grasso, C.; Di Salvo, M.E.; Caggegi, A.; Barbanti, M.; Scandura, S.; Milici, A.; Motta, G.; Bentivegna, A.; Sardone, A.; et al. Impact of Post-Procedural Change in Left Ventricle Systolic Function on Survival after Percutaneous Edge-to-Edge Mitral Valve Repair. J. Clin. Med. 2021, 10, 4748. https://doi.org/10.3390/jcm10204748
Hagnäs MJ, Grasso C, Di Salvo ME, Caggegi A, Barbanti M, Scandura S, Milici A, Motta G, Bentivegna A, Sardone A, et al. Impact of Post-Procedural Change in Left Ventricle Systolic Function on Survival after Percutaneous Edge-to-Edge Mitral Valve Repair. Journal of Clinical Medicine. 2021; 10(20):4748. https://doi.org/10.3390/jcm10204748
Chicago/Turabian StyleHagnäs, Magnus J., Carmelo Grasso, Maria Elena Di Salvo, Anna Caggegi, Marco Barbanti, Salvatore Scandura, Annalisa Milici, Gessica Motta, Agnese Bentivegna, Andrea Sardone, and et al. 2021. "Impact of Post-Procedural Change in Left Ventricle Systolic Function on Survival after Percutaneous Edge-to-Edge Mitral Valve Repair" Journal of Clinical Medicine 10, no. 20: 4748. https://doi.org/10.3390/jcm10204748
APA StyleHagnäs, M. J., Grasso, C., Di Salvo, M. E., Caggegi, A., Barbanti, M., Scandura, S., Milici, A., Motta, G., Bentivegna, A., Sardone, A., Capodicasa, L., Giuffrida, A., Biancari, F., Mäkikallio, T., Capodanno, D., & Tamburino, C. (2021). Impact of Post-Procedural Change in Left Ventricle Systolic Function on Survival after Percutaneous Edge-to-Edge Mitral Valve Repair. Journal of Clinical Medicine, 10(20), 4748. https://doi.org/10.3390/jcm10204748







