Addition of Bone Marrow Aspirate Concentrate Resulted in High Rate of Healing and Good Functional Outcomes in the Treatment of Clavicle Fracture Nonunion: A Retrospective Case Series
Abstract
1. Introduction
2. Methods
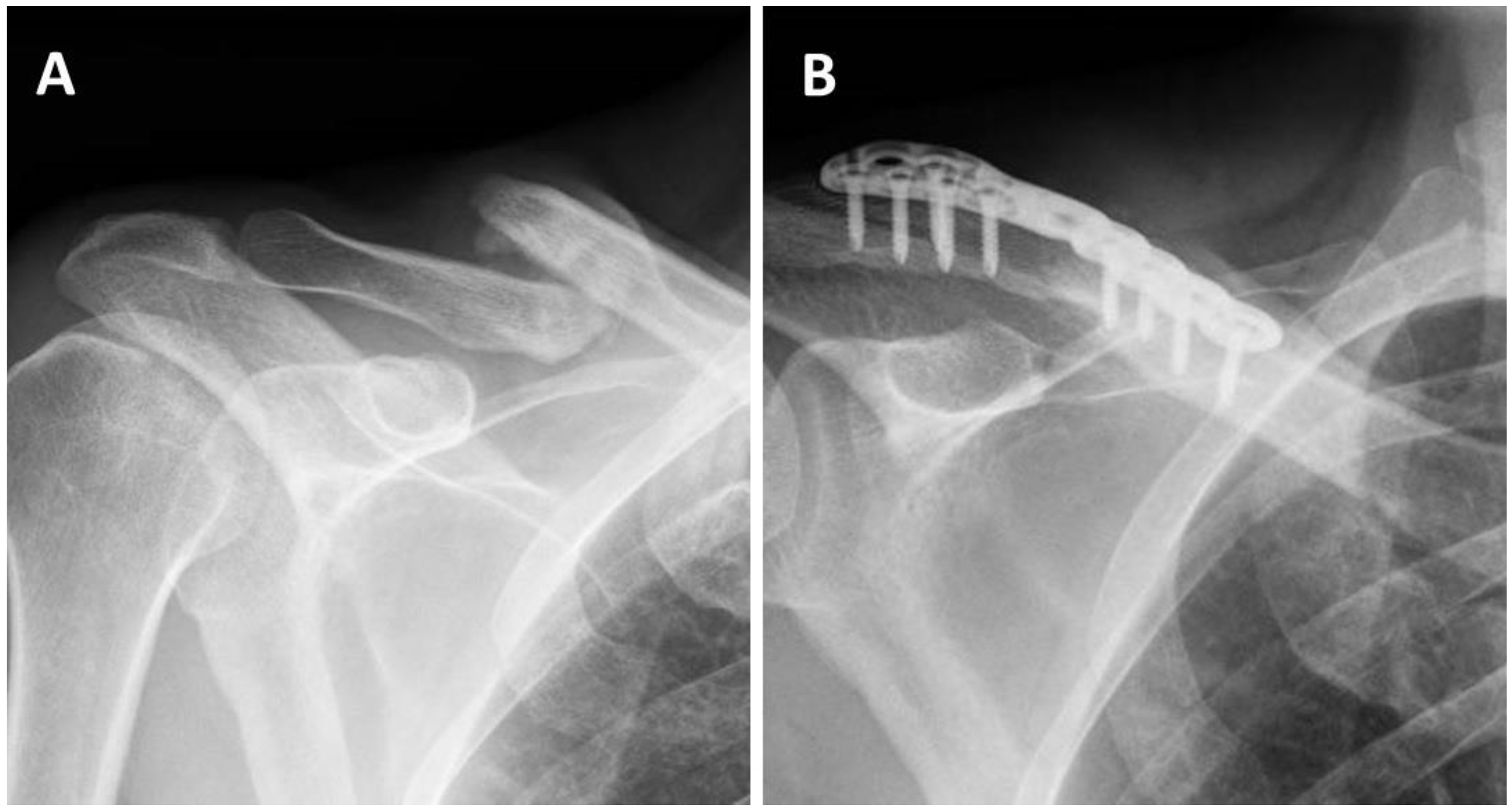
2.1. Surgical Technique
2.2. Clinical Outcome
2.3. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Robinson, C.M. Fractures of the clavicle in the adult: Epidemiology and Classification. J. Bone Jt. Surg. 1998, 80, 476–484. [Google Scholar] [CrossRef]
- Nordqvist, A.; Petersson, C. The incidence of fractures of the clavicle. Clin. Orthop. Relat. Res. 1994, 300, 127–132. [Google Scholar] [CrossRef]
- Court-Brown, C.M.; Caesar, B. Epidemiology of adult fractures: A review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.; Longworth, A.; Amirfeyz, R.; Fox, R.; Bannister, G. The functional outcome of the fractured clavicle. Arch. Orthop. Trauma Surg. 2009, 129, 1557–1564. [Google Scholar] [CrossRef] [PubMed]
- Smekal, V.; Oberladstaetter, J.; Struve, P.; Krappinger, D. Shaft fractures of the clavicle: Current concepts. Arch. Orthop. Trauma Surg. 2009, 129, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, R.; Waterman, B.; Padalecki, J.; Robertson, W. Management of distal clavicle fractures. J. Am. Acad. Orthop. Surg. 2011, 19, 392–401. [Google Scholar] [CrossRef]
- Wick, M.; Müller, E.J.; Kollig, E.; Muhr, G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch. Orthop. Trauma Surg. 2001, 121, 207–211. [Google Scholar] [CrossRef]
- Fuglesang, H.F.S.; Flugsrud, G.B.; Randsborg, P.H.; Stavem, K.; Utvåg, S.E. Radiological and functional outcomes 2.7 years following conservatively treated completely displaced midshaft clavicle fractures. Arch. Orthop. Trauma Surg. 2016, 136, 17–25. [Google Scholar] [CrossRef]
- Nowak, J.; Mallmin, H.; Larsson, S. The aetiology and epidemiology of clavicular fractures: A prospective study during a two-year period in Uppsala, Sweden. Injury 2000, 31, 353–358. [Google Scholar] [CrossRef]
- Zlowodzki, M.; Zelle, B.A.; Cole, P.A.; Jeray, K.; McKee, M.D. Treatment of acute midshaft clavicle fractures: Systematic review of 2144 fractures. On behalf of the Evidence-Based Orthopaedic Trauma Working Group. J. Orthop. Trauma 2005, 19, 504–507. [Google Scholar] [CrossRef]
- Virtanen, K.J.; Remes, V.; Pajarinen, J.; Savolainen, V.; Björkenheim, J.M.; Paavola, M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: A randomized clinical trial. J. Bone Jt. Surg.-Ser. A 2012, 94, 1546–1553. [Google Scholar] [CrossRef]
- Wiesel, B.; Nagda, S.; Mehta, S.; Churchill, R. Management of Midshaft Clavicle Fractures in Adults. J. Am. Acad. Orthop. Surg. 2018, 26, e468–e476. [Google Scholar] [CrossRef]
- Robinson, M.M.; Court-Brown, C.M.; McQueen, M.M.; Wakefield, A.E. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J. Bone Jt. Surg.-Ser. A 2004, 86, 1359–1365. [Google Scholar] [CrossRef]
- Davids, P.H.P.; Luitse, J.S.K.; Strating, R.P.; Van Der Hart, C.P. Operative treatment for delayed union and nonunion of midshaft clavicular fractures: AO reconstruction plate fixation and early mobilization. J. Trauma Acute Care Surg. 1996, 40, 985–986. [Google Scholar] [CrossRef]
- Neer, C.S. Nonunion of the clavicle. J. Am. Med. Assoc. 1960, 172, 1006–1011. [Google Scholar] [CrossRef]
- Wilkins, R.M.; Johnston, R.M. Ununited fractures of the clavicle. J. Bone Jt. Surg.-Ser. A 1983, 65, 773–778. [Google Scholar] [CrossRef]
- Manske, D.J.; Szabo, R.M. The operative treatment of mid-shaft clavicular non-unions. J. Bone Jt. Surg.-Ser. A 1985, 67, 1367–1371. [Google Scholar] [CrossRef]
- Jupiter, J.B.; Leffert, R.D. Non-union of the clavicle. Associated complications and surgical management. J. Bone Jt. Surg.-Ser. A 1987, 69, 753–760. [Google Scholar] [CrossRef]
- Der Tavitian, J.; Davison, J.N.S.; Dias, J.J. Clavicular fracture non-union surgical outcome and complications. Injury 2002, 33, 135–143. [Google Scholar] [CrossRef]
- Harrell, D.B.; Caradonna, E.; Mazzucco, L.; Gudenus, R.; Amann, B.; Prochazka, V.; Giannoudis, P.V.; Hendrich, C.; Jäger, M.; Krauspe, R.; et al. Non-hematopoietic essential functions of bone marrow cells: A review of scientific and clinical literature and rationale for treating bone defects. Orthop. Rev. (Pavia) 2015, 7, 5691. [Google Scholar] [CrossRef] [PubMed]
- Gianakos, A.L.; Sun, L.; Patel, J.N.; Adams, D.M.; Liporace, F.A. Clinical application of concentrated bone marrow aspirate in orthopaedics: A systematic review. World J. Orthop. 2017, 8, 491–506. [Google Scholar] [CrossRef] [PubMed]
- Faraud, A.; Bonnevialle, N.; Allavena, C.; Nouaille Degorce, H.; Bonnevialle, P.; Mansat, P. Outcomes from surgical treatment of middle-third clavicle fractures non-union in adults: A series of 21cases. Orthop. Traumatol. Surg. Res. 2014, 100, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.K.; Chiang, C.C.; Su, Y.U.P.; Feng, C.K.; Chiu, F.Y.; Liu, C.L.; Chen, T.H. Role of autologous bone graft in the surgical treatment of atrophic nonunion of midshaft clavicular fractures. Orthopedics 2012, 35, e197–e201. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.K.; Chiang, C.C.; Hung, S.H.; Su, Y.P.; Chiu, F.Y.; Liu, C.L.; Chen, T.H. The role of autologous bone graft in surgical treatment of hypertrophic nonunion of midshaft clavicle fractures. J. Chin. Med. Assoc. 2012, 75, 216–220. [Google Scholar] [CrossRef][Green Version]
- Leighton, R.; Watson, J.T.; Giannoudis, P.; Papakostidis, C.; Harrison, A.; Steen, R.G. Healing of fracture nonunions treated with low-intensity pulsed ultrasound (LIPUS): A systematic review and meta-analysis. Injury 2017, 48, 1339–1347. [Google Scholar] [CrossRef]
- Romano, C.L.; Romano, D.; Logoluso, N. Low-intensity pulsed ultrasound for the treatment of bone delayed union or nonunion: A review. Ultrasound Med. Biol. 2009, 35, 529–536. [Google Scholar] [CrossRef]
- Moya, D.; Ramón, S.; Schaden, W.; Wang, C.J.; Guiloff, L.; Cheng, J.H. The Role of Extracorporeal Shockwave Treatment in Musculoskeletal Disorders. J. Bone Jt. Surg. Am. 2018, 100, 251–263. [Google Scholar] [CrossRef]
- Nolte, P.A.; van der Krans, A.; Patka, P.; Janssen, I.M.; Ryaby, J.P.; Albers, G.R. Low-intensity pulsed ultrasound in the treatment of nonunions. J. Trauma 2001, 51, 693–703. [Google Scholar] [CrossRef]
- Martetschläger, F.; Gaskill, T.R.; Millett, P.J. Management of clavicle nonunion and malunion. J. Shoulder Elb. Surg. 2013, 22, 862–868. [Google Scholar] [CrossRef]
- Schnetzke, M.; Morbitzer, C.; Aytac, S.; Erhardt, M.; Frank, C.; Muenzberg, M.; Studier-Fischer, S.; Helbig, L.; Suda, A.J.; Gruetzner, P.A.; et al. Additional bone graft accelerates healing of clavicle non-unions and improves long-term results after 8.9 years: A retrospective study. J. Orthop. Surg. Res. 2015, 10, 2. [Google Scholar] [CrossRef]
- Rollo, G.; Vicenti, G.; Rotini, R.; Abate, A.; Colella, A.; D’Arienzo, A.; Carrozzo, M.; Moretti, B. Clavicle aseptic nonunion: Is there a place for cortical allogenic strut graft? Injury 2017, 48, S60–S65. [Google Scholar] [CrossRef]
- Nikiforidis, P.; Babis, G.C.; Vayanos, E.D. Treatment of pseudarthrosis of the clavicle by bone plate with screw fixation and autologous spongiosa graft. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1996, 82, 82. [Google Scholar]
- Wentz, S.; Eberhardt, C.; Leonhard, T. Reconstruction plate fixation with bone graft for mid-shaft clavicular non-union in semi-professional athletes. J. Orthop. Sci. 1999, 4, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Shamshery, P.; Gupta, V.; Trikha, V.; Varshney, M.K.; Kumar, A. Locking compression plate in long standing clavicular nonunions with poor bone stock. J. Trauma-Inj. Infect. Crit. Care 2008, 64, 439–441. [Google Scholar] [CrossRef] [PubMed]
- Ebraheim, N.A.; Mekhail, A.O.; Darwich, M. Open reduction and internal fixation with bone grafting of clavicular nonunion. J. Trauma-Inj. Infect. Crit. Care 1997, 42, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Mestha, P.; Tavakkolizadeh, A.; Sinha, J. Clavicle midshaft fracture non-union treated surgically, with bone grafting or demineralised bone matrix: A comparative outcome analysis. Inj. Extra 2011, 42, 120. [Google Scholar] [CrossRef]
- Muller, M.E.; Thomas, R.J. Treatment of non-union in fractures of long bones. Clin. Orthop. Relat. Res. 1979, 138, 141–153. [Google Scholar]
- Dimitriou, R.; Mataliotakis, G.I.; Angoules, A.G.; Kanakaris, N.K.; Giannoudis, P.V. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: A systematic review. Injury 2011, 42, S3–S15. [Google Scholar] [CrossRef]
- Garnavos, C.; Mouzopoulos, G.; Morakis, E. Fixed intramedullary nailing and percutaneous autologous concentrated bone-marrow grafting can promote bone healing in humeral-shaft fractures with delayed union. Injury 2010, 6, 563–567. [Google Scholar] [CrossRef]
- Hernigou, P.; Guissou, I.; Homma, Y.; Poignard, A.; Chevallier, N.; Rouard, H.; Flouzat Lachaniette, C.H. Percutaneous injection of bone marrow mesenchymal stem cells for ankle non-unions decreases complications in patients with diabetes. Int. Orthop. 2015, 39, 1639–1643. [Google Scholar] [CrossRef]
- Woltz, S.; Sengab, A.; Krijnen, P.; Schipper, I.B. Does clavicular shortening after nonoperative treatment of midshaft fractures affect shoulder function? A systematic review. Arch. Orthop. Trauma Surg. 2017, 137, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
| Nonunion after Conservative Treatment (n = 14) | Nonunion after Surgical Treatment (n = 7) | Total (n = 21) | |
|---|---|---|---|
| Age (years) (SD) 1 | 45 (14) | 35 (5.4) | 41.8 (12.7) |
| Gender, Male (%) | 10 (71) | 5 (71) | 15 (71) |
| Smoking (%) | 6 (43) | 3 (43) | 9 (43) |
| Distal clavicle fracture (%) | 2 (14) | 1 (14) | 3 (14) |
| Follow-up (months) (SD) 1 | 34.4 (15.5) | 39.4 (26.3) | 36.1 (19.2) |
| Nonunion after Conservative Treatment (n = 14) | Nonunion after Surgical Treatment (n = 7) | Total (n = 21) | |
|---|---|---|---|
| Nonunion (%) | 1 (7.1) | 0 (0) | 1 (4.8) |
| Time to union * (Months) (SD) 1 | 3.9 (2.33) | 5.7 (3.82) | 4.5 (2.96) |
| Nonunion after Conservative Treatment * (n = 13) | Nonunion after Surgical Treatment (n = 7) | Total (n = 20) | |
|---|---|---|---|
| Shoulder VAS (SD) 1 | 3.7 (3.66) | 2 (2.52) | 3.1 (3.34) |
| SSV (SD) 1 | 71.9 (29.41) | 78.6 (16.76) | 74.3 (25.41) |
| QDASH (SD) 1 | 25.2 (25.18) | 19.9 (18.06) | 23.3 (22.59) |
| Donor site VAS | 0 | 0 | 0 |
| Donor site complications | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benshabat, D.; Factor, S.; Maman, E.; Khoury, A.; Krespi, R.; Ashkenazi, I.; Chechik, O.; Dolkart, O. Addition of Bone Marrow Aspirate Concentrate Resulted in High Rate of Healing and Good Functional Outcomes in the Treatment of Clavicle Fracture Nonunion: A Retrospective Case Series. J. Clin. Med. 2021, 10, 4749. https://doi.org/10.3390/jcm10204749
Benshabat D, Factor S, Maman E, Khoury A, Krespi R, Ashkenazi I, Chechik O, Dolkart O. Addition of Bone Marrow Aspirate Concentrate Resulted in High Rate of Healing and Good Functional Outcomes in the Treatment of Clavicle Fracture Nonunion: A Retrospective Case Series. Journal of Clinical Medicine. 2021; 10(20):4749. https://doi.org/10.3390/jcm10204749
Chicago/Turabian StyleBenshabat, Dvir, Shai Factor, Eran Maman, Amal Khoury, Raphael Krespi, Itay Ashkenazi, Ofir Chechik, and Oleg Dolkart. 2021. "Addition of Bone Marrow Aspirate Concentrate Resulted in High Rate of Healing and Good Functional Outcomes in the Treatment of Clavicle Fracture Nonunion: A Retrospective Case Series" Journal of Clinical Medicine 10, no. 20: 4749. https://doi.org/10.3390/jcm10204749
APA StyleBenshabat, D., Factor, S., Maman, E., Khoury, A., Krespi, R., Ashkenazi, I., Chechik, O., & Dolkart, O. (2021). Addition of Bone Marrow Aspirate Concentrate Resulted in High Rate of Healing and Good Functional Outcomes in the Treatment of Clavicle Fracture Nonunion: A Retrospective Case Series. Journal of Clinical Medicine, 10(20), 4749. https://doi.org/10.3390/jcm10204749







