Effects of COVID-19 Lockdown on Weight, Body Composition, and Behavior of Children, Adolescents, and Young Adults with Prader–Willi Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropometric Parameters and Body Composition
2.3. Hormonal Parameters, Lipoproteins and Carbohydrate Metabolism
2.4. The Questionnaire
2.5. Statistical Analysis
3. Results
3.1. Anthropometric Parameters and Body Composition
3.2. Hormonal Parameters, Lipoproteins, and Carbohydrate Metabolism
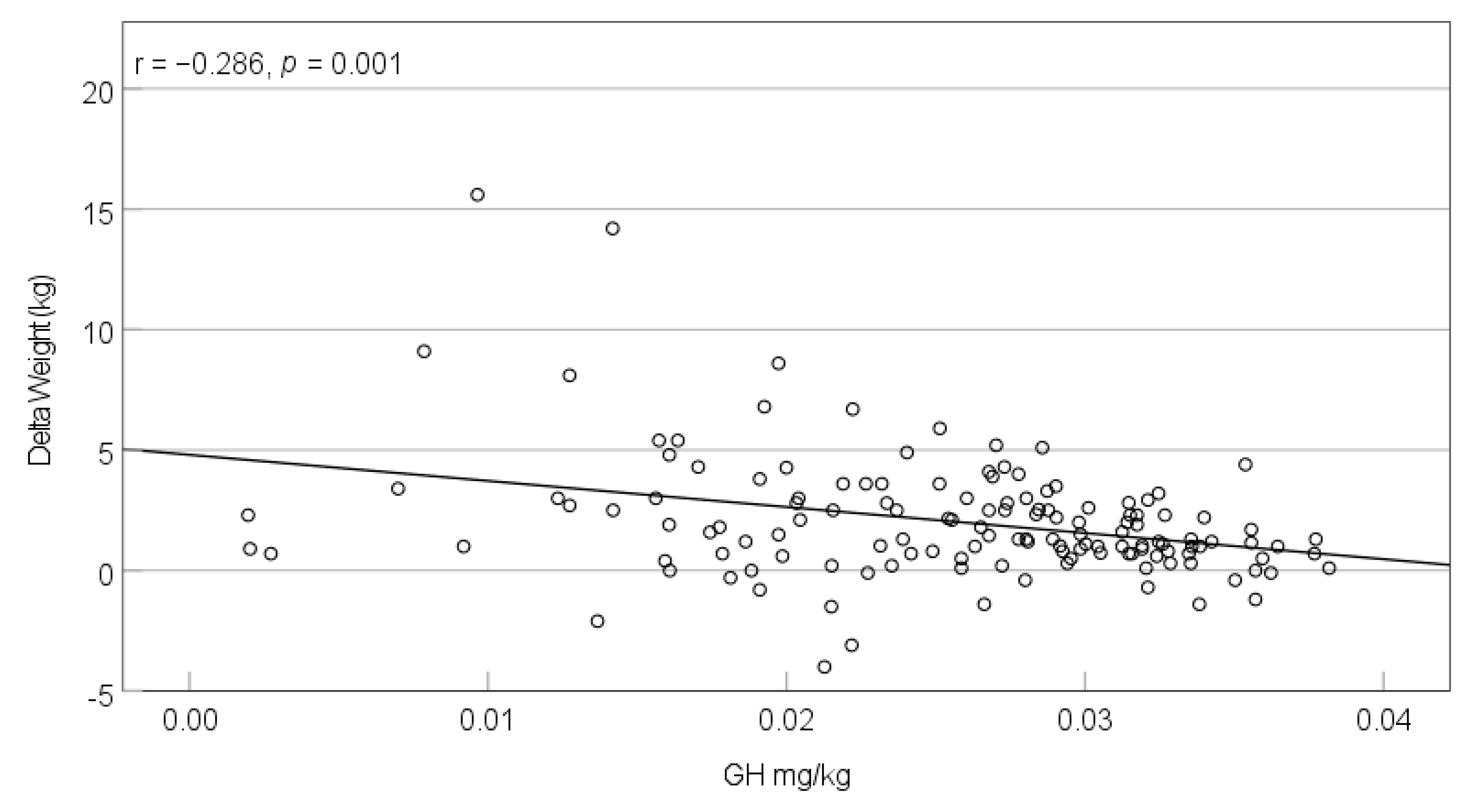
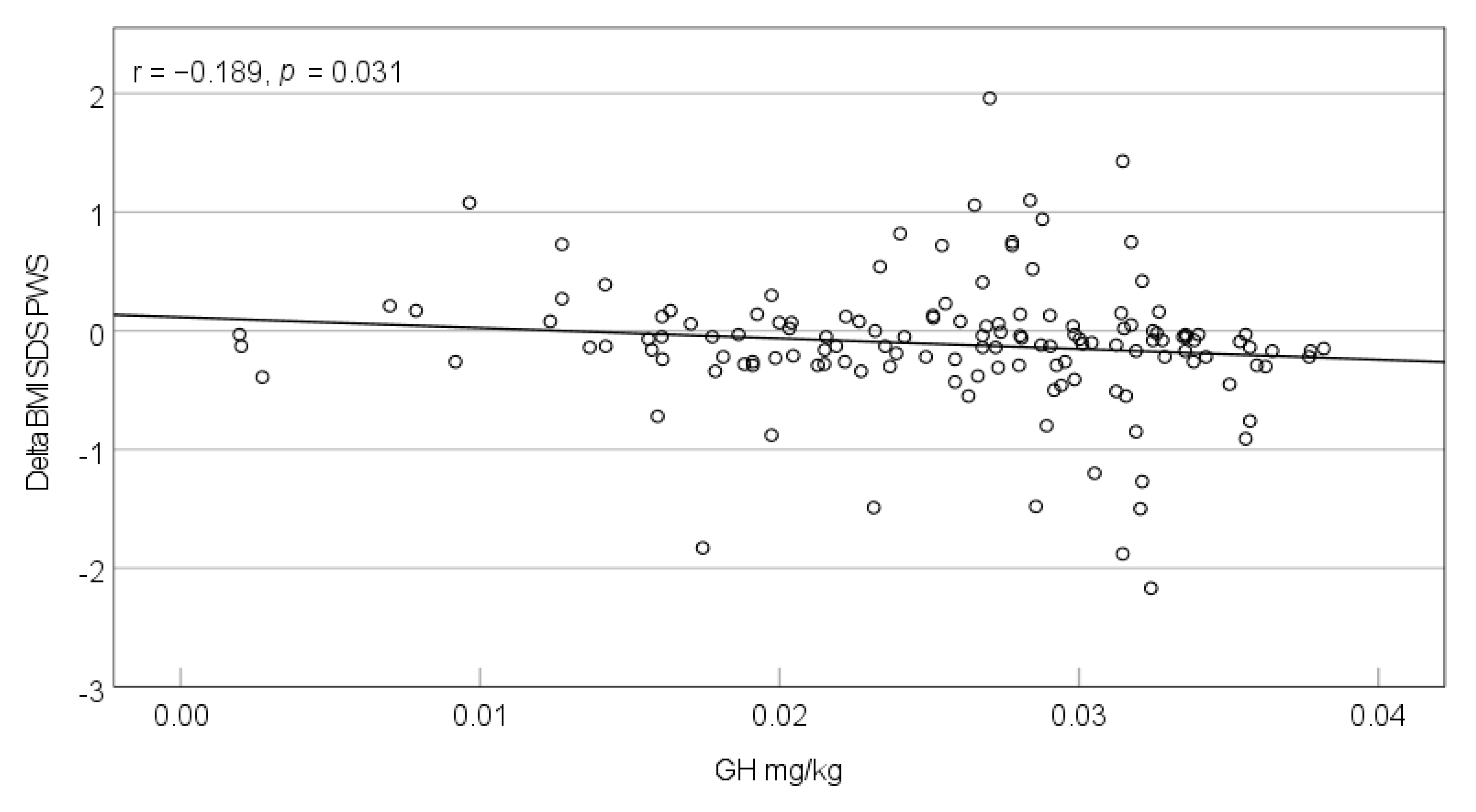
3.3. Growth Hormone Therapy and the Development of Weight/BMI/LBM
3.4. The Questionnaire
3.4.1. Living Environment
3.4.2. Care and Therapies during COVID-19 Lockdown
3.4.3. Behavior Changes during COVID-19 Lockdown
3.5. Multiple Regression Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Butler, M.G.; Miller, J.L.; Forster, J.L. Prader-Willi Syndrome—Clinical Genetics, Diagnosis and Treatment Approaches: An Update. Curr. Pediatr. Rev. 2019, 15, 207–244. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, S.B.; Schwartz, S.; Miller, J.L.; Driscoll, D.J. Prader-Willi syndrome. Genet. Med. 2012, 14, 10–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crinò, A.; Fintini, D.; Bocchini, S.; Grugni, G. Obesity management in Prader-Willi syndrome: Current perspectives. Diabetes Metab. Syndr. Obes. 2018, 11, 579–593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coupaye, M.; Tauber, M.; Cuisset, L.; Laurier, V.; Bieth, E.; Lacorte, J.M.; Oppert, J.M.; Clément, K.; Poitou, C. Effect of Genotype and Previous GH Treatment on Adiposity in Adults With Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2016, 101, 4895–5903. [Google Scholar] [CrossRef] [PubMed]
- Reus, L.; Zwarts, M.; van Vlimmeren, L.A.; Willemsen, M.A.; Otten, B.J.; van der Sanden, M.W.N. Motor problems in Prader-Willi syndrome: A systematic review on body composition and neuromuscular functioning. Neurosci. Biobehav. Rev. 2011, 35, 956–969. [Google Scholar] [CrossRef] [Green Version]
- Heksch, R.; Kamboj, M.; Anglin, K.; Obrynba, K. Review of Prader-Willi syndrome: The endocrine approach. Transl. Pediatr. 2017, 6, 274–285. [Google Scholar] [CrossRef] [Green Version]
- Emerick, J.E.; Vogt, K.S. Endocrine manifestations and management of Prader-Willi syndrome. Int. J. Pediatr. Endocrinol. 2013, 2013, 14. [Google Scholar] [CrossRef] [Green Version]
- Butler, M.G. Prader-Willi Syndrome: Obesity due to Genomic Imprinting. Curr. Genom. 2011, 12, 204–215. [Google Scholar] [CrossRef]
- Butler, M.G.; Theodoro, M.F.; Bittel, D.C.; Donnelly, J.E. Energy expenditure and physical activity in Prader-Willi syndrome: Comparison with obese subjects. Am. J. Med. Genet. A 2007, 143A, 449–459. [Google Scholar] [CrossRef] [Green Version]
- Passone, C.G.B.; Franco, R.R.; Ito, S.S.; Trindade, E.; Polak, M.; Damiani, D.; Bernardo, W.M. Growth hormone treatment in Prader-Willi syndrome patients: Systematic review and meta-analysis. BMJ Paediatr. Open 2020, 4, e000630. [Google Scholar] [CrossRef]
- Goldstone, A.; Holland, A.J.; Hauffa, B.P.; Hokken-Koelega, A.C.; Tauber, M. Recommendations for the Diagnosis and Management of Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2008, 93, 4183–4197. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Bedford, J.; Enria, D.; Giesecke, J.; Heymann, D.L.; Ihekweazu, C.; Kobinger, G.; Lane, H.C.; Memish, Z.; Oh, M.D.; Sall, A.A.; et al. COVID-19: Towards controlling of a pandemic. Lancet 2020, 395, 1015–1018. [Google Scholar] [CrossRef]
- Sharma, A.; Metzger, D.L. Calculator: Prader-Willi Syndrome Z-Scores 0-18y. Available online: https://apps.cpeg-gcep.net/PWSZ_cpeg/ (accessed on 4 November 2020).
- Völgyi, E.; Tylavsky, F.A.; Lyytikäinen, A.; Suominen, H.; Alén, M.; Cheng, S. Assessing body composition with DXA and bioimpedance: Effects of obesity, physical activity, and age. Obesity 2008, 16, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis--part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Franckle, R.; Adler, R.; Davison, K. Accelerated Weight Gain Among Children During Summer Versus School Year and Related Racial/Ethnic Disparities: A Systematic Review. Prev. Chronic Dis. 2014, 11, E101. [Google Scholar] [CrossRef] [Green Version]
- Weaver, R.G.; Beets, M.W.; Brazendale, K.; Brusseau, T.A. Summer Weight Gain and Fitness Loss: Causes and Potential Solutions. Am. J. Lifestyle Med. 2018, 13, 116–128. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; Von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Lancet Child & Adolescent Health. Pandemic school closures: Risks and opportunities. Lancet Child Adolesc. Health 2020, 4, 341. [Google Scholar] [CrossRef]
- Fisher, B.G.; Acerini, C.L. Understanding the growth hormone therapy adherence paradigm: A systematic review. Horm. Res. Paediatr. 2013, 79, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Giavoli, C.; Profka, E.; Giancola, N.; Rodari, G.; Giacchetti, F.; Ferrante, E.; Arosio, M.; Mantovani, G. Growth hormone therapy at the time of Covid-19 pandemic: Adherence and drug supply issues. Eur. J. Endocrinol. 2020, 183, L13–L15. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, L.; Barone, B.; Morra, S.; Celentano, G.; Rocca, R.L.; Capece, M.; Morgera, V.; Turco, C.; Caputo, V.F.; Spena, G.; et al. Hypogonadism in Patients with Prader Willi Syndrome: A Narrative Review. Int. J. Mol. Sci. 2021, 22, 1993. [Google Scholar] [CrossRef]
- Morales, J.S.; Valenzuela, P.L.; Pareja-Galeano, H.; Rincón-Castanedo, C.; Rubin, D.A.; Lucia, A. Physical exercise and Prader-Willi syndrome: A systematic review. Clin. Endocrinol. 2019, 90, 649–661. [Google Scholar] [CrossRef] [Green Version]
- Eiholzer, U.; Nordmann, Y.; l’Allemand, D.; Schlumpf, M.; Schmid, S.; Kromeyer-Hauschild, K. Improving body composition and physical activity in Prader-Willi Syndrome. J. Pediatr. 2003, 142, 73–78. [Google Scholar] [CrossRef] [Green Version]
- Rubin, D.A.; Duran, A.; Haqq, A.M.; Gertz, E.R.; Dumont-Driscoll, M. Changes in cardiometabolic markers in children with Prader-Willi syndrome and nonsyndromic obesity following participation in a home-based physical activity intervention. Pediatr. Obes. 2018, 13, 734–743. [Google Scholar] [CrossRef]
- Rubin, D.A.; Wilson, K.S.; Castner, D.M.; Dumont-Driscoll, M.C. Changes in Health-Related Outcomes in Youth With Obesity in Response to a Home-Based Parent-Led Physical Activity Program. J. Adolesc. Health 2019, 65, 323–330. [Google Scholar] [CrossRef] [Green Version]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–11. [Google Scholar] [CrossRef]
- Guan, H.; Okely, A.D.; Aguilar-Farias, N.; Cruz, B.D.P.; Draper, C.E.; El Hamdouchi, A.; Florindo, A.A.; Jáuregui, A.; Katzmarzyk, P.T.; Kontsevaya, A.; et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc. Health 2020, 4, 416–418. [Google Scholar] [CrossRef]
- Mosbah, H.; Coupaye, M.; Jacques, F.; Tauber, M.; Clément, K.; Oppert, J.-M.; Poitou, C. Effects of the COVID-19 pandemic and lockdown on the mental and physical health of adults with Prader-Willi syndrome. Orphanet J. Rare Dis. 2021, 16, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Irizarry, K.A.; Mager, D.R.; Triador, L.; Muehlbauer, M.J.; Haqq, A.M.; Freemark, M. Hormonal and metabolic effects of carbohydrate restriction in children with Prader-Willi syndrome. Clin. Endocrinol. 2019, 90, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Grugni, G.; Cicolini, S.; Caroli, D.; Tamini, S.; Sartorio, A. Changes of Body Weight and Body Composition in Obese Patients with Prader–Willi Syndrome at 3 and 6 Years of Follow-Up: A Retrospective Cohort Study. J. Clin. Med. 2020, 9, 3596. [Google Scholar] [CrossRef] [PubMed]
- Carrel, A.L.; Myers, S.E.; Whitman, B.Y.; Allen, D.B. Growth hormone improves body composition, fat utilization, physical strength and agility, and growth in Prader-Willi syndrome: A controlled study. J. Pediatr. 1999, 134, 215–221. [Google Scholar] [CrossRef]
- l’Allemand, D.; Eiholzer, U.; Schlumpf, M.; Steinert, H.; Riesen, W. Cardiovascular risk factors improve during 3 years of growth hormone therapy in Prader-Willi syndrome. Eur. J. Pediatr. 2000, 159, 835–842. [Google Scholar] [CrossRef]
- Kim, S.-H.; Park, M.-J. Effects of growth hormone on glucose metabolism and insulin resistance in human. Ann. Pediatr. Endocrinol. Metab. 2017, 22, 145–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Groot, C.J.; Bernert, C.P.; Coupaye, M.; Clement, K.; Paschou, S.A.; Charmandari, E.; Kanaka-Gantenbein, C.; Wabitsch, M.; Buddingh, E.P.; Nieuwenhuijsen, B.; et al. Clinical management of patients with genetic obesity during COVID-19 pandemic: Position paper of the ESE Growth & Genetic Obesity COVID-19 Study Group and Rare Endo-ERN main thematic group on Growth and Obesity. Endocrine 2021, 71, 653–662. [Google Scholar]
- Meade, C.; Martin, R.; McCrann, A.; Lyons, J.; Meehan, J.; Hoey, H.; Roche, E. Prader-Willi Syndrome in children: Quality of life and caregiver burden. Acta Paediatr. 2020, 110, 1665–1670. [Google Scholar] [CrossRef]
- Wieting, J.; Eberlein, C.; Bleich, S.; Frieling, H.; Deest, M. Behavioural change in Prader-Willi syndrome during COVID-19 pandemic. J. Intellect. Disabil. Res. 2021, 65, 609–616. [Google Scholar] [CrossRef]
- Feighan, S.-M.; Hughes, M.; Maunder, K.; Roche, E.; Gallagher, L. A profile of mental health and behaviour in Prader-Willi syndrome. J. Intellect. Disabil. Res. 2019, 64, 158–169. [Google Scholar] [CrossRef]
| <2 Years | 2–6 Years | 7–10 Years | 11–17 Years | ≥18 Years | |
|---|---|---|---|---|---|
| Sample size (n) | 10 | 59 | 38 | 46 | 27 |
| Mean age in years (range) | 1.38 (0.94–1.96) | 4.07 (2.02–6.94) | 8.92 (7.05–10.95) | 14.33 (11.26–17.99) | 23.38 (18.49–33.55) |
| Females (%) | 10 (100%) | 31 (52.5%) | 19 (50%) | 23 (50%) | 12 (44.4%) |
| Median interval between assessments (months) | 5 | 6 | 6.5 | 7 | 9 |
| n GH therapy pre-lockdown (%) | 5 (50%) | 55 (93.2%) | 37 (97.4%) | 34 (73.9%) | 2 (7.4%) |
| n GH therapy intra-lockdown (%) | 10 (100%) | 56 (94.9%) | 38 (100%) | 34 (73.9%) | 2 (7.4%) |
| <2 Years | 2–6 Years | 7–10 Years | 11–17 Years | ≥18 Years | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | ||
| Height (m) | Pre | 0.67 | 0.08 | 0.005 | 0.96 | 0.12 | <0.001 | 1.29 | 0.10 | <0.001 | 1.55 | 0.12 | <0.001 | 1.67 | 0.12 | NS |
| Post | 0.77 | 0.06 | 1.00 | 0.12 | 1.33 | 0.10 | 1.57 | 0.11 | 1.67 | 0.11 | ||||||
| Height SDSPWS | Pre | 0.15 | 0.69 | 0.028 | 0.60 | 0.96 | NS | 0.61 | 0.60 | NS | 1.19 | 0.93 | <0.001 | |||
| Post | 0.72 | 0.93 | 0.57 | 1.01 | 0.66 | 0.61 | 1.28 | 0.91 | ||||||||
| Weight (kg) | Pre | 6.93 | 1.17 | 0.005 | 14.52 | 5.15 | <0.001 | 30.93 | 9.09 | <0.001 | 54.92 | 18.00 | <0.001 | 69.07 | 9.75 | NS |
| Post | 9.04 | 1.52 | 16.32 | 5.91 | 33.17 | 9.99 | 57.52 | 19.72 | 67.87 | 11.92 | ||||||
| Weight SDSPWS | Pre | 0.12 | 0.70 | NS | −0.73 | 0.79 | NS | −0.78 | 0.73 | 0.044 | −0.71 | 0.90 | NS | |||
| Post | −0.15 | 0.83 | −0.81 | 0.80 | −0.82 | 0.77 | −0.75 | 0.94 | ||||||||
| BMI (kg/m2) | Pre | 15.30 | 1.31 | NS | 15.51 | 2.09 | NS | 18.35 | 3.76 | NS | 22.38 | 5.23 | NS | 24.75 | 3.07 | NS |
| Post | 15.15 | 1.66 | 15.88 | 2.55 | 18.45 | 3.68 | 22.77 | 5.99 | 24.20 | 3.30 | ||||||
| BMI SDSPWS | Pre | −0.30 | 1.25 | 0.037 | −1.15 | 0.73 | NS | −1.24 | 0.67 | 0.007 | −1.36 | 0.65 | NS | |||
| Post | −1.08 | 1.29 | −1.21 | 0.77 | −1.32 | 0.65 | −1.39 | 0.71 | ||||||||
| LBM (kg) | Pre | 13.72 | 3.17 | <0.001 | 21.97 | 4.58 | <0.001 | 35.58 | 8.89 | <0.001 | 44.94 | 7.93 | NS | |||
| Post | 15.11 | 3.49 | 23.43 | 5.41 | 37.24 | 9.99 | 43.26 | 9.56 | ||||||||
| Fat Mass (%) | Pre | 17.43 | 7.51 | NS | 26.62 | 7.89 | NS | 32.01 | 8.68 | NS | 36.14 | 7.40 | NS | |||
| Post | 17.02 | 9.07 | 26.75 | 7.41 | 32.27 | 8.73 | 35.21 | 6.62 | ||||||||
| <2 Years | 2–6 Years | 7–10 Years | 11–17 Years | ≥18 Years | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | ||
| IGF-1 (µg/L) | Pre | 46.97 | 29.42 | 0.008 | 115.17 | 58.46 | <0.001 | 233.25 | 74.29 | 0.022 | 307.19 | 109.17 | NS | 146.63 | 46.46 | NS |
| Post | 81.73 | 41.63 | 147.61 | 59.31 | 264.11 | 108.65 | 319.13 | 118.17 | 148.63 | 71.97 | ||||||
| IGFBP-3 (mg/L) | Pre | 2.56 | 0.85 | 0.008 | 4.09 | 1.11 | <0.001 | 5.51 | 1.00 | <0.001 | 6.70 | 1.41 | 0.001 | 5.65 | 1.27 | NS |
| Post | 4.13 | 1.18 | 5.01 | 1.16 | 9.01 | 16.39 | 7.41 | 1.72 | 5.88 | 1.19 | ||||||
| Total cholesterol (mg/dL) | Pre | 139.22 | 31.91 | NS | 163.56 | 28.79 | NS | 157.92 | 27.14 | NS | 155.52 | 29.45 | NS | 158.50 | 37.06 | NS |
| Post | 150.22 | 17.35 | 167.81 | 27.55 | 164.22 | 21.15 | 156.82 | 27.03 | 159.42 | 37.34 | ||||||
| Triglycerides (mg/dL) | Pre | 73.56 | 17.07 | NS | 76.83 | 30.09 | 0.047 | 62.39 | 20.74 | NS | 77.57 | 37.99 | 0.050 | 88.19 | 54.66 | NS |
| Post | 67.89 | 20.76 | 69.97 | 20.52 | 66.42 | 25.62 | 95.45 | 78.58 | 84.85 | 44.61 | ||||||
| HDL (mg/dL) | Pre | 39.81 | 9.02 | NS | 49.82 | 11.00 | <0.001 | 58.23 | 15.12 | 0.008 | 53.14 | 11.11 | NS | 52.05 | 14.24 | NS |
| Post | 45.60 | 8.23 | 55.38 | 9.62 | 63.19 | 11.93 | 53.07 | 11.77 | 52.45 | 12.16 | ||||||
| LDL (mg/dL) | Pre | 84.78 | 25.92 | NS | 98.80 | 26.99 | NS | 87.25 | 20.54 | NS | 88.00 | 23.97 | NS | 90.96 | 31.75 | NS |
| Post | 91.11 | 14.13 | 98.58 | 25.90 | 87.72 | 19.86 | 87.05 | 23.75 | 90.92 | 32.47 | ||||||
| Fasting glucose (mg/dL) | Pre | 82.33 | 3.24 | NS | 81.44 | 9.48 | NS | 88.00 | 7.43 | NS | 90.44 | 7.56 | NS | 88.81 | 7.12 | NS |
| Post | 80.78 | 8.71 | 85.63 | 12.44 | 89.31 | 8.43 | 91.76 | 7.90 | 96.40 | 32.63 | ||||||
| OGTT 30 min (mg/dL) | Pre | 127.60 | 17.57 | NS | 145.91 | 28.75 | NS | 152.47 | 31.19 | 0.035 | 155.14 | 23.70 | NS | 149.21 | 30.37 | NS |
| Post | 134.20 | 33.25 | 149.64 | 27.17 | 165.14 | 28.53 | 158.11 | 26.80 | 158.63 | 34.50 | ||||||
| OGTT 60 min (mg/dL) | Pre | 112.60 | 28.84 | NS | 126.77 | 26.58 | NS | 133.61 | 19.87 | NS | 142.66 | 30.74 | NS | 139.92 | 42.93 | 0.006 |
| Post | 124.60 | 43.33 | 129.88 | 31.62 | 137.11 | 32.15 | 148.82 | 36.65 | 157.17 | 41.88 | ||||||
| OGTT 120 min (mg/dL) | Pre | 111.60 | 32.76 | NS | 105.61 | 17.67 | 0.026 | 110.47 | 19.43 | 0.006 | 114.76 | 22.14 | NS | 111.76 | 20.44 | NS |
| Post | 109.60 | 21.42 | 111.50 | 19.35 | 121.31 | 20.99 | 123.55 | 31.46 | 121.67 | 32.13 | ||||||
| Insulin (pU/dL) | Pre | 1.89 | 1.08 | NS | 4.17 | 3.56 | NS | 6.59 | 2.71 | 0.042 | 11.61 | 5.59 | NS | 6.99 | 3.39 | 0.003 |
| Post | 2.42 | 1.70 | 4.24 | 3.05 | 7.79 | 3.79 | 15.34 | 19.21 | 5.12 | 1.76 | ||||||
| Vitamin D (nmol/L) | Pre | 92.75 | 66.40 | NS | 65.43 | 23.91 | <0.001 | 74.44 | 48.48 | NS | 66.59 | 29.19 | 0.004 | 75.50 | 23.99 | 0.001 |
| Post | 88.70 | 50.91 | 80.04 | 22.33 | 75.44 | 22.55 | 76.70 | 26.45 | 97.79 | 21.93 | ||||||
| <2 Years | 2–6 Years | 7–10 Years | 11–17 Years | ≥18 Years | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Less | Equal | More | p | Less | Equal | More | p | Less | Equal | More | p | Less | Equal | More | p | Less | Equal | More | p | |
| Intra-pre-lockdown | 2 | 6 | 0 | 0.500 | 3 | 35 | 20 | 0.000 | 6 | 12 | 20 | 0.011 | 6 | 13 | 27 | 0.000 | 5 | 8 | 14 | 0.064 |
| Post-intra-lockdown | 0 | 7 | 0 | 1.000 | 12 | 36 | 3 | 0.035 | 13 | 13 | 8 | 0.383 | 15 | 21 | 8 | 0.210 | 12 | 10 | 2 | 0.013 |
| Post-pre-lockdown | 2 | 5 | 0 | 0.500 | 3 | 41 | 7 | 0.344 | 2 | 16 | 16 | 0.001 | 6 | 18 | 20 | 0.011 | 4 | 9 | 11 | 0.118 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohr, A.K.; Laemmer, C.; Schulte, S.; Gohlke, B. Effects of COVID-19 Lockdown on Weight, Body Composition, and Behavior of Children, Adolescents, and Young Adults with Prader–Willi Syndrome. J. Clin. Med. 2021, 10, 4746. https://doi.org/10.3390/jcm10204746
Mohr AK, Laemmer C, Schulte S, Gohlke B. Effects of COVID-19 Lockdown on Weight, Body Composition, and Behavior of Children, Adolescents, and Young Adults with Prader–Willi Syndrome. Journal of Clinical Medicine. 2021; 10(20):4746. https://doi.org/10.3390/jcm10204746
Chicago/Turabian StyleMohr, Andrea Karoline, Constanze Laemmer, Sandra Schulte, and Bettina Gohlke. 2021. "Effects of COVID-19 Lockdown on Weight, Body Composition, and Behavior of Children, Adolescents, and Young Adults with Prader–Willi Syndrome" Journal of Clinical Medicine 10, no. 20: 4746. https://doi.org/10.3390/jcm10204746
APA StyleMohr, A. K., Laemmer, C., Schulte, S., & Gohlke, B. (2021). Effects of COVID-19 Lockdown on Weight, Body Composition, and Behavior of Children, Adolescents, and Young Adults with Prader–Willi Syndrome. Journal of Clinical Medicine, 10(20), 4746. https://doi.org/10.3390/jcm10204746






