Displacement of the Greater Tuberosity in Humeral Head Fractures Does Not only Depend on Rotator Cuff Status
Abstract
:1. Introduction
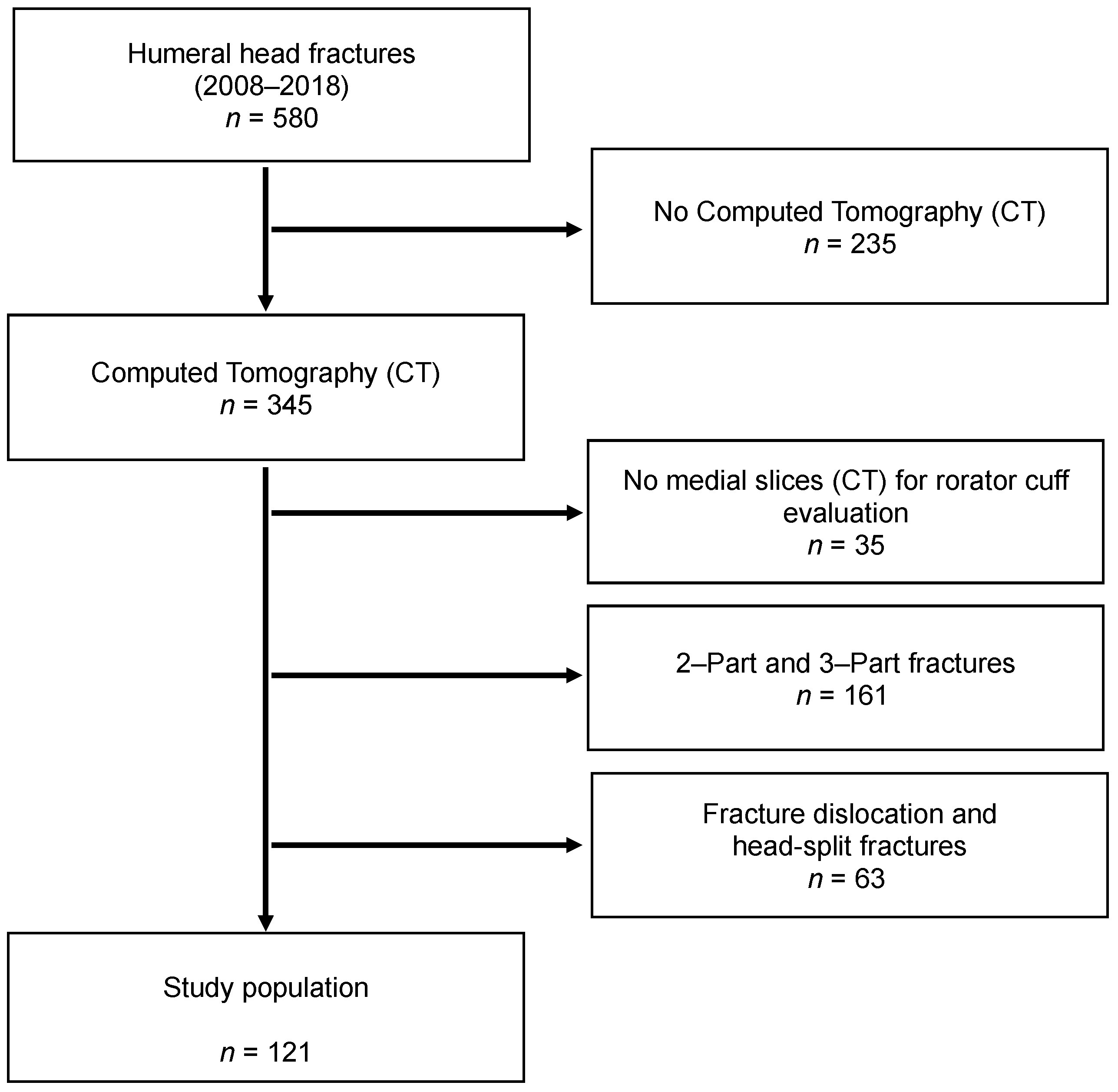
2. Materials and Methods
2.1. Radiological Evaluation
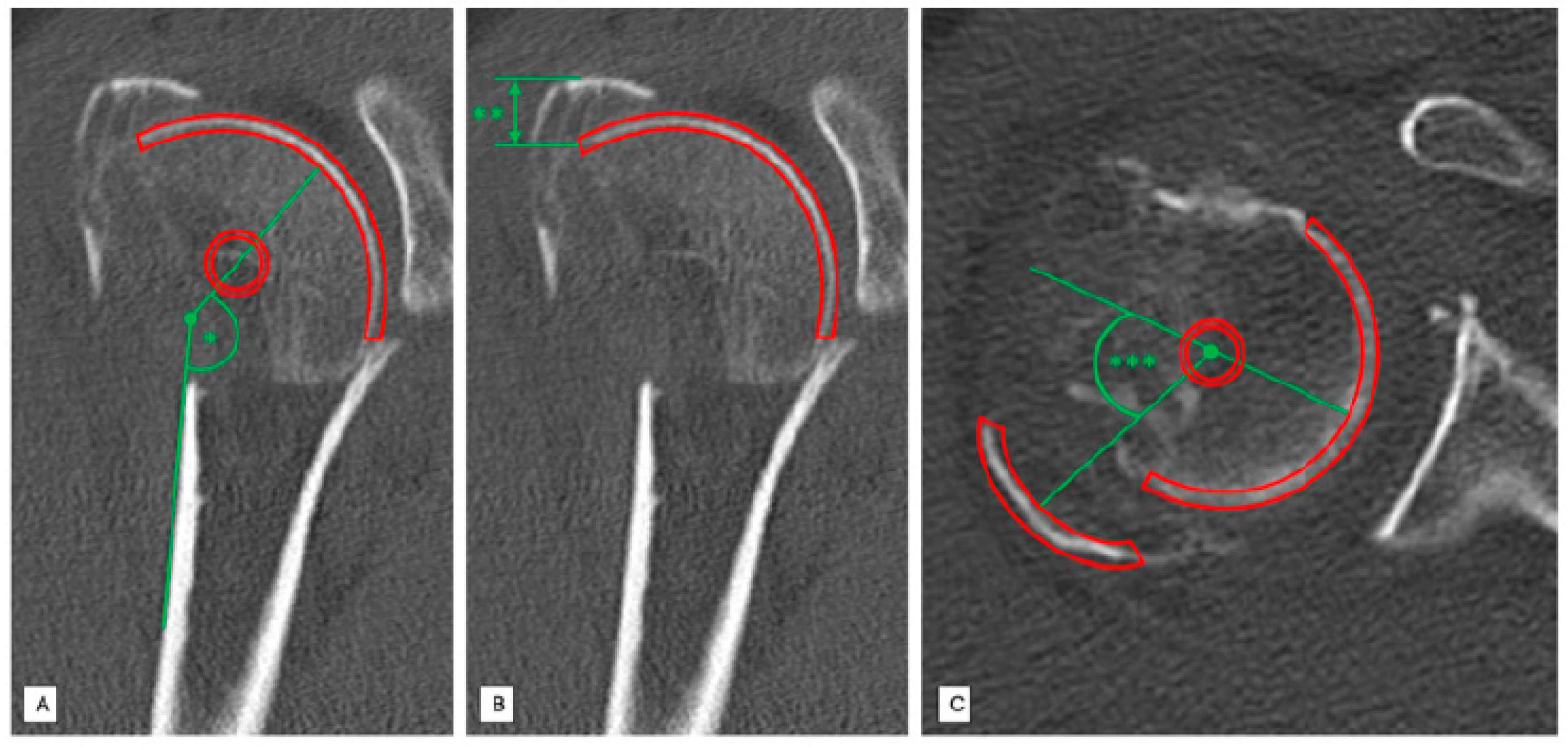
2.2. Head-Shaft Angle (HSA)
2.3. Position Determination of the Greater Tuberosity in the Vertical Plane (Cranial Displacement)
2.4. Position Determination of the Greater Tuberosity in the Horizontal Plane (Dorsal Displacement)
2.5. Classification of Fatty Degeneration of Rotator Cuff
2.6. Statistical Analysis
3. Results
3.1. Cranial Displacement of the Greater Tuberosity
3.2. Dorsal Displacement of the Greater Tuberosity
4. Discussion
- −
- In non-varus four-part humeral head fractures, cranial and dorsal displacement of the greater tuberosity depends on the status of the posterosuperior rotator cuff.
- −
- In varus displaced humeral head fractures, no correlation between displacement of the greater tuberosity and the condition of the posterosuperior rotator cuff could be detected.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Neer, C.S. Displaced proximal humeral fractures: Part, I. Classification and evaluation, 1970. Clin. Orthop. Relat. Res. 2006, 442, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Codman, E. Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Shoulder Thomas Todd 1934, 45, 612–616. [Google Scholar]
- Yamamoto, A.; Takagishi, K.; Osawa, T.; Yanagawa, T.; Nakajima, D.; Shitara, H.; Kobayashi, T. Prevalence and risk factors of a rotator cuff tear in the general population. J. Shoulder Elb. Surg. 2010, 19, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Sher, J.S.; Uribe, J.W.; Posada, A.; Murphy, B.J.; Zlatkin, M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J. Bone Jt. Surg. Am. Vol. 1995, 77, 10–15. [Google Scholar] [CrossRef] [Green Version]
- Milgrom, C.; Schaffler, M.; Gilbert, S.; van Holsbeeck, M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J. Bone Jt. Surg. Br. Vol. 1995, 77, 296–298. [Google Scholar] [CrossRef] [Green Version]
- Scheibel, M. Humeral head fracture and cuff. Unfallchirurg 2011, 114, 1075–1078, 1081–1082. [Google Scholar] [CrossRef]
- Bahrs, C.; Rolauffs, B.; Stuby, F.; Dietz, K.; Weise, K.; Helwig, P. Effect of Proximal Humeral Fractures on the Age-Specific Prevalence of Rotator Cuff Tears. J. Trauma Inj. Infect. Crit. Care 2010, 69, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994, 304, 78–83. [Google Scholar]
- Thomazeau, H.; Duval, J.M.; Darnault, P.; Dréano, T. Anatomical relationships and scapular attachments of the supraspinatus muscle. Surg. Radiol. Anat. 1996, 18, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Bahrs, C.; Lingenfelter, E.; Fischer, F.; Walters, E.M.; Schnabel, M. Mechanism of injury and morphology of the greater tuberosity fracture. J. Shoulder Elb. Surg. 2006, 15, 140–147. [Google Scholar] [CrossRef]
- Barry, J.J.; Lansdown, D.A.; Cheung, S.; Feeley, B.T.; Ma, C.B. The relationship between tear severity, fatty infiltration, and muscle atrophy in the supraspinatus. J. Shoulder Elb. Surg. 2013, 22, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Bahrs, C.; Bauer, M.; Blumenstock, G.; Eingartner, C.; Bahrs, S.D.; Tepass, A.; Weise, K.; Rolauffs, B. The complexity of proximal humeral fractures is age and gender specific. J. Orthop. Sci. 2013, 18, 465–470. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Ditsios, K.; Middleton, W.D.; Hildebolt, C.F.; Galatz, L.M.; Teefey, S.A. The Demographic and Morphological Features of Rotator Cuff Disease. A Comparison of Asymptomatic and Symptomatic Shoulders. J. Bone Jt. Surg. Am. Vol. 2006, 88, 1699–1704. [Google Scholar] [CrossRef]
- Robinson, C.M.; Stirling, P.H.; Goudie, E.B.; MacDonald, D.J.; Strelzow, J.A. Complications and Long-Term Outcomes of Open Reduction and Plate Fixation of Proximal Humeral Fractures. J. Bone Jt. Surg. Am. Vol. 2019, 101, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, B.; Weishaupt, D.; Zanetti, M.; Hodler, J.; Gerber, C. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb. Surg. 1999, 8, 599–605. [Google Scholar] [CrossRef]
- Nardo, L.; Karampinos, D.C.; Lansdown, D.A.; Carballido-Gamio, J.; Lee, S.; Maroldi, R.; Ma, C.B.; Link, T.M.; Krug, R. Quantitative assessment of fat infiltration in the rotator cuff muscles using water-fat MRI. J. Magn. Reson. Imaging 2013, 39, 1178–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frich, L.H.; Fernandes, L.R.; Schrøder, H.D.; Hejbøl, E.K.; Nielsen, P.V.; Jørgensen, P.H.; Stensballe, A.; Lambertsen, K.L. The inflammatory response of the supraspinatus muscle in rotator cuff tear conditions. J. Shoulder Elb. Surg. 2021, 30, e261–e275. [Google Scholar] [CrossRef] [PubMed]




| Fracture Type | Number of Fragments | ||
|---|---|---|---|
| 2 | 3 | 4 | |
| I | |||
| II | anatomical neck | ||
| III | surgical neck | ||
| IV | greater tuberosity | ||
| V | lesser tuberosity | ||
| VI | anterior or posterior luxation | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klute, L.; Pfeifer, C.; Weiss, I.; Mayr, A.; Alt, V.; Kerschbaum, M. Displacement of the Greater Tuberosity in Humeral Head Fractures Does Not only Depend on Rotator Cuff Status. J. Clin. Med. 2021, 10, 4136. https://doi.org/10.3390/jcm10184136
Klute L, Pfeifer C, Weiss I, Mayr A, Alt V, Kerschbaum M. Displacement of the Greater Tuberosity in Humeral Head Fractures Does Not only Depend on Rotator Cuff Status. Journal of Clinical Medicine. 2021; 10(18):4136. https://doi.org/10.3390/jcm10184136
Chicago/Turabian StyleKlute, Lisa, Christian Pfeifer, Isabella Weiss, Agnes Mayr, Volker Alt, and Maximilian Kerschbaum. 2021. "Displacement of the Greater Tuberosity in Humeral Head Fractures Does Not only Depend on Rotator Cuff Status" Journal of Clinical Medicine 10, no. 18: 4136. https://doi.org/10.3390/jcm10184136
APA StyleKlute, L., Pfeifer, C., Weiss, I., Mayr, A., Alt, V., & Kerschbaum, M. (2021). Displacement of the Greater Tuberosity in Humeral Head Fractures Does Not only Depend on Rotator Cuff Status. Journal of Clinical Medicine, 10(18), 4136. https://doi.org/10.3390/jcm10184136







