The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
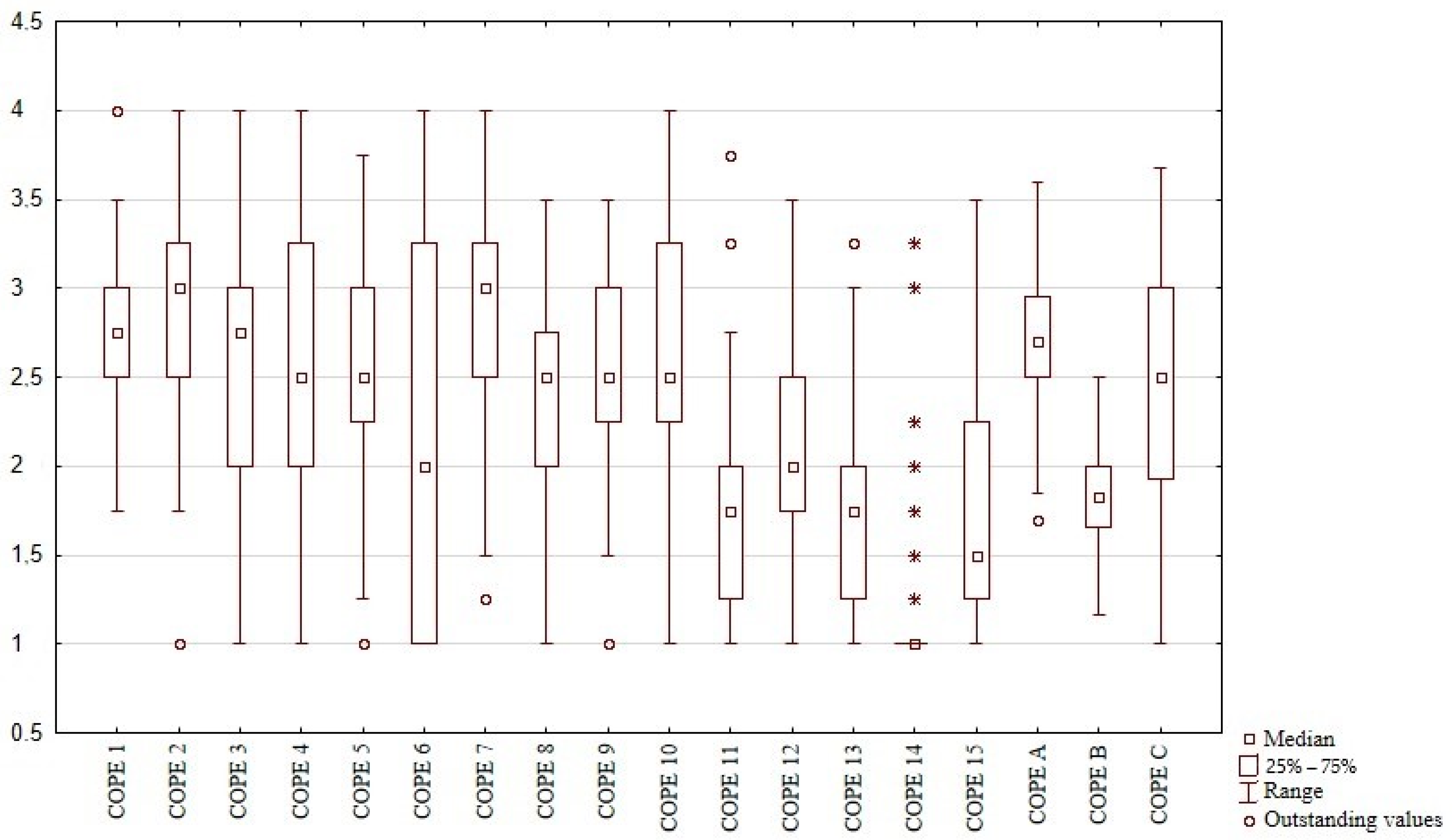
3. Results
3.1. Initial Assessment
3.1.1. Measures of Stress and MS-Related Variables
3.1.2. Measures of Stress and Other Factors
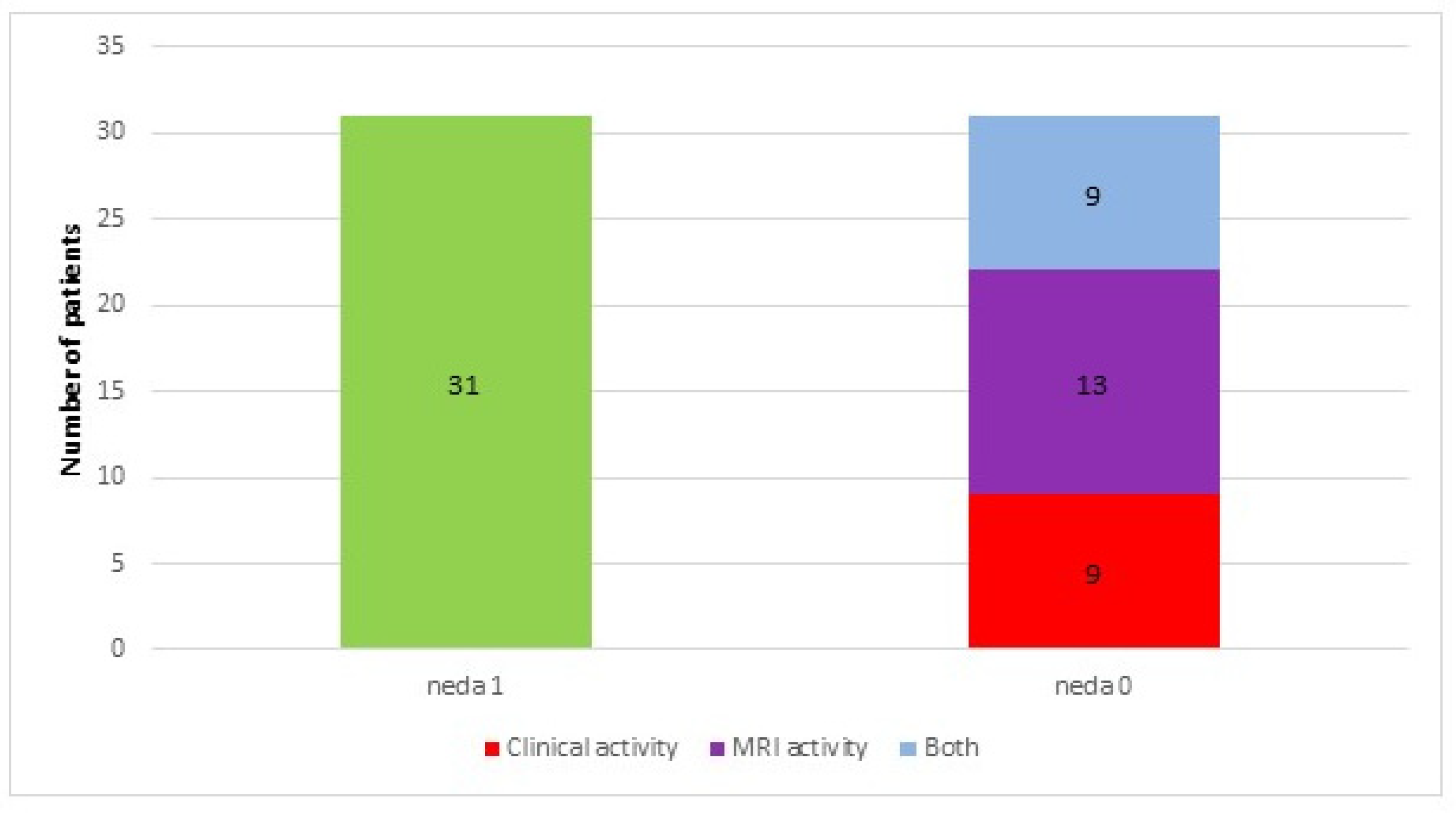
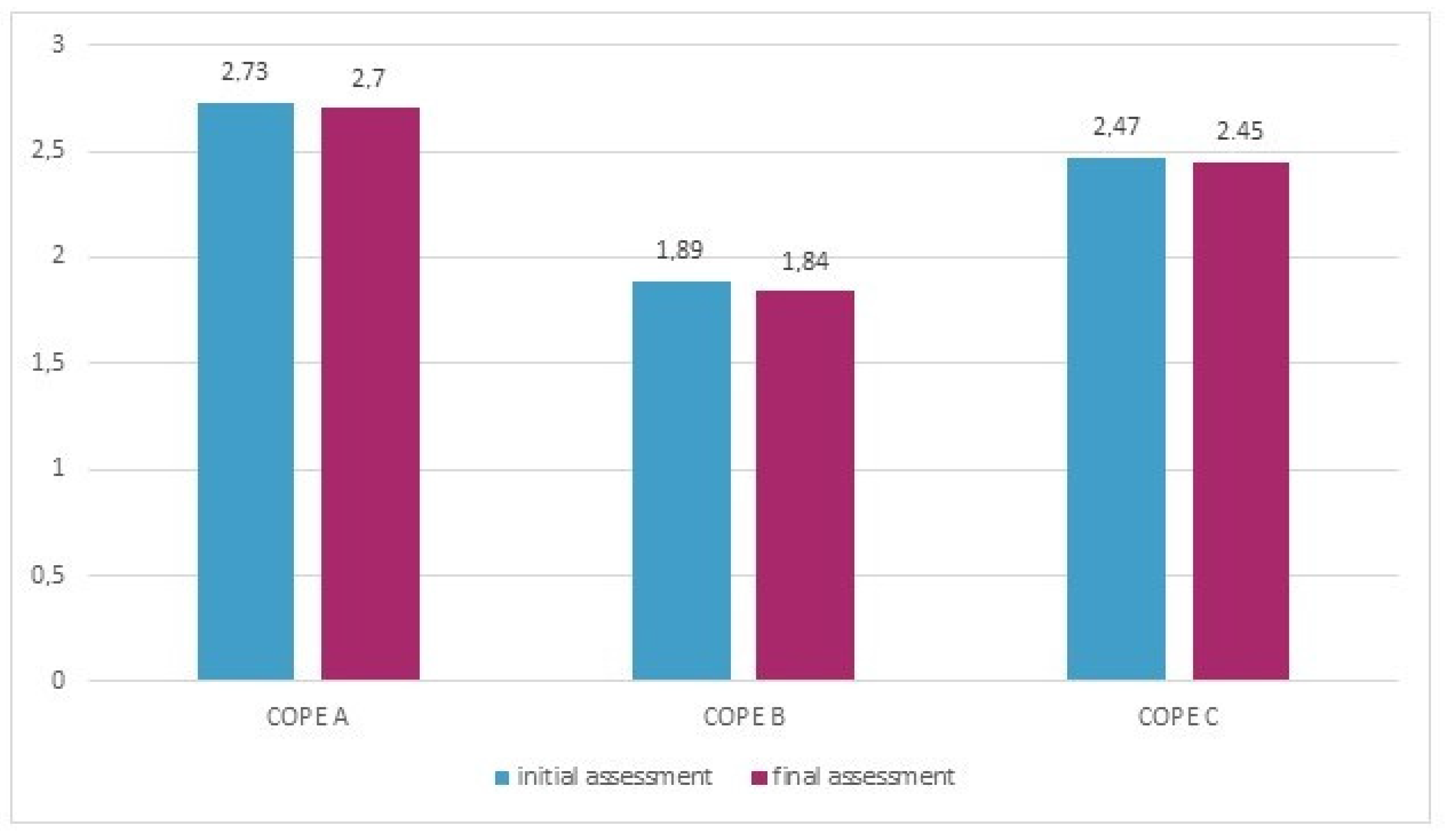
3.2. Assessment after a Year of Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- The Perceived Stress Scale (PSS-10) [15] consists of 10 items concerning the subjective perception of problems, situations and behaviors over the preceding four weeks. The score for each item ranges from 0 (never) to 4 (very often). The total score is the sum of responses to particular items, with a range of 0–40. The higher the score, the greater the level of perceived stress. The interpretation of the results is based on a 10-degree sten scale: scores within stens from 1–4 correspond with a low level of stress, within 5–6 to moderate and within 7–10 to a high level of stress [17]. The internal consistency of the Polish version of the PSS-10 reached a Cronbach’s alpha of 0.86 [17].
- The DS14 questionnaire [16] includes 14 items divided into two subscales (7 items each): negative affectivity (NEG) and social inhibition (SI). The score for each item ranges from 0 (false) to 4 (true). A result ≥10 in both subscales is used to categorize individuals as having a Type-D personality [17]. The internal consistency of the Polish version of the DS14 reached a Cronbach’s alpha of 0.86 for negative affectivity (NA) and 0.84 for social inhibition (SI) [17].
- 1. Active coping;2. Planning;3. Seeking social support for instrumental reasons4. Seeking social support for emotional reasons;5. Suppression of competing activities;6. Turning to religion;7. Positive reinterpretation and growth;8. Restraint coping;9. Acceptance;10. Focus on and venting of emotions;11. Denial;12. Mental disengagement;13. Behavioral disengagement;14. Alcohol–drug disengagement;15. Humor.General categories of coping strategies:
- -
- COPE A—active coping—this category consists of strategies 1, 2, 5, 7 and 8;
- -
- COPE B—avoidant behavior—this category consists of strategies 9, 11, 12, 13, 14 and 15;
- -
- COPE C—emotion-focused and seeking support—this category consists of strategies 3, 4, 6 and 10.
References
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Thompson, A.J.; Wolinsky, J.S.; Banwell, B.; Barkhof, F.; Bebo, B.; Calabresi, P.A.; et al. Defining the clinical course of multiple sclerosis. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Artemiadis, A.K.; Anagnostouli, M.C.; Alexopoulos, E.C. Stress as a risk factor for multiple sclerosis onset or relapse: A systematic review. Neuroepidemiology 2011, 36, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Benito-León, J. Stress and multiple sclerosis: What’s new? Neuroepidemiology 2011, 36, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Zänkert, S.; Bellingrath, S.; Wüst, S.; Kudielka, B.M. HPA axis responses to psychological challenge linking stress and disease: What do we know on sources of intra- and interindividual variability? Psychoneuroendocrinology 2019, 105, 86–97. [Google Scholar] [CrossRef]
- Kern, S.; Ziemssen, T. Brain–immune communication psychoneuroimmunology of multiple sclerosis. Mult. Scler. J. 2008, 14, 6–21. [Google Scholar] [CrossRef]
- Heesen, C.; Mohr, D.C.; Huitinga, I.; Then Bergh, F.; Gaab, J.; Otte, C.; Gold, S.M. Stress regulation in multiple sclerosis-Current issues and concepts. Mult. Scler. J. 2007, 13, 143–148. [Google Scholar] [CrossRef]
- Neustein, J.; Rymaszewska, J. Psychological consequences of multiple sclerosis and assistance possibilities. Physiother. Q. 2017, 25, 8–12. [Google Scholar] [CrossRef]
- Fisher, P.L.; Salmon, P.; Heffer-Rahn, P.; Huntley, C.; Reilly, J.; Cherry, M.G. Predictors of emotional distress in people with multiple sclerosis: A systematic review of prospective studies. J. Affect. Disord. 2020, 276, 752–764. [Google Scholar] [CrossRef]
- Briones-Buixassa, L.; Milà, R.; Ma Aragonès, J.; Bufill, E.; Olaya, B.; Arrufat, F.X. Stress and multiple sclerosis: A systematic review considering potential moderating and mediating factors and methods of assessing stress. Health Psychol. Open 2015, 2, 2055102915612271. [Google Scholar] [CrossRef]
- Carver, C.; Scheier, M.; Weintraub, J. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Lazarus, R.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Polman, C.; Reingold, S.; Banwell, B.; Clanet, M.; Cohen, J.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Medelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Folstein, M.; Folstein, S.; McHugh, P. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermrlstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Denollet, J. Type D personality: A potential risk factor refined. J. Psychosom. Res. 2000, 49, 255–266. [Google Scholar] [CrossRef]
- Juczynski, Z.; Oginska-Bulik, N. Narzędzia Pomiaru Stresu i Radzenia Sobie Ze Stresem; Pracownia Testów Psychologicznych: Warsaw, Poland, 2009. [Google Scholar]
- Kurtzke, J. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Roxburgh, R.; Seaman, S.; Masterman, T.; Hensiek, A.; Sawcer, S.; Vukusic, S.; Achiti, I.; Confavreux, C.; Coustans, M.; le Page, E.; et al. Multiple Sclerosis Severity Score. Using disability and disease duration to rate disease severity. Neurology 2005, 64, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Giovannoni, G.; Turner, B.; Gnanapavan, S.; Offiah, C.; Schmierer, K.; Marta, M. Is it time to target no evident disease activity (NEDA) in multiple sclerosis? Mult. Scler. Relat. Disord. 2015, 4, 329–333. [Google Scholar] [CrossRef]
- Scheffer, M.; Becker, J.; de Azeredo, L.A.; Grassi-Oliveira, R.; de Almeida, R.M.M. Subjective and physiological stress measurement in a multiple sclerosis sample and the relation with executive functions performance. J. Neural Transm. 2019, 126, 613–622. [Google Scholar] [CrossRef]
- Pritchard, M.; Elison-Bowers, P.; Birdsall, B. Impact of integrative restoration (iRest) meditation on perceived stress levels in multiple sclerosis and cancer outpatients. Stress Health 2010, 26, 233–237. [Google Scholar] [CrossRef]
- Sanaeinasab, H.; Saffari, M.; Hashempour, M.; Karimi Zarchi, A.A.; Alghamdi, W.A.; Koenig, H.G. Effect of a transactional model education program on coping effectiveness in women with multiple sclerosis. Brain Behav. 2017, 7, e00810. [Google Scholar] [CrossRef] [PubMed]
- Lamis, D.A.; Hirsch, J.K.; Pugh, K.C.; Topciu, R.; Nsamenang, S.A.; Goodman, A.; Duberstein, P.R. Perceived cognitive deficits and depressive symptoms in patients with multiple sclerosis: Perceived stress and sleep quality as mediators. Mult. Scler. Relat. Disord. 2018, 25, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Artemiadis, A.K.; Vervainioti, A.A.; Alexopoulos, E.C.; Rombos, A.; Anagnostouli, M.C.; Darviri, C. Stress management and multiple sclerosis: A randomized controlled trial. Arch. Clin. Neuropsychol. 2012, 27, 406–416. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Senders, A.; Bourdette, D.; Hanes, D.; Yadav, V.; Shinto, L. Perceived Stress in Multiple Sclerosis: The Potential Role of Mindfulness in Health and Well-Being. J. Evid.-Based Complement. Altern. Med. 2014, 19, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.C.; Roesch, S.; Fortmann, A.; Carnethon, M.R.; Penedo, F.J.; Perreira, K.; Birnbaum-Weitzman, O.; Wassertheil-Smoller, D.; Castaneda, S.; Talavera, G.; et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the HCHS/SOL Sociocultural Ancillary Study Linda. Psychosom. Med. 2014, 76, 468–475. [Google Scholar] [CrossRef]
- Lee, A.M.; Wong, J.G.W.S.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, N.M.; Wong, P.C.; Tsang, K.W.T.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, P.; Carpinelli, L.; Savarese, G. Perceived stress and bruxism in university students. BMC Res. Notes 2016, 9, 514. [Google Scholar] [CrossRef]
- Garber, M.C.; Huston, S.A.; Breese, C.R. Sources of stress in a pharmacy student population. Curr. Pharm. Teach. Learn. 2019, 11, 329–337. [Google Scholar] [CrossRef]
- Mills, S.D.; Azizoddin, D.; Racaza, G.Z.; Wallace, D.J.; Weisman, M.H.; Nicassio, P.M. The psychometric properties of the Perceived Stress Scale-10 among patients with systemic lupus erythematosus. Lupus 2017, 26, 1218–1223. [Google Scholar] [CrossRef]
- Trojan, D.; Arnold, D.; Shapiro, S.; Bar-Or, A.; Robinson, A.; Le Cruguel, J.; Narayanan, S.; Tartaglia, M.; Caramanos, Z.; Da Costa, D. Fatigue in post-poliomyelitis syndrome: Association with disease-related, behavioral, and psychosocial factors. PM&R 2009, 1, 442–449. [Google Scholar]
- Denollet, J.; Schiffer, A.A.; Spek, V. A general propensity to psychological distress affects cardiovascular outcomes: Evidence from research on the type D (distressed) personality profile. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 546–557. [Google Scholar] [CrossRef]
- Beutel, M.E.; Wiltink, J.; Till, Y.; Wild, P.S.; Münzel, T.; Ojeda, F.M.; Zeller, T.; Schnabel, R.B.; Lackner, K.; Blettner, M.; et al. Type D personality as a cardiovascular risk marker in the general population: Results from the gutenberg health study. Psychother. Psychosom. 2012, 81, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Jandackova, V.K.; Koenig, J.; Jarczok, M.N.; Fischer, J.E.; Thayer, J.F. Potential biological pathways linking Type-D personality and poor health: A cross-sectional investigation. PLoS ONE 2017, 12, e0176014. [Google Scholar] [CrossRef]
- Oginska-Bulik, N. Czy osobowość sprzyja etiopatogenezie chorób? Nowe kierunki badań-osobowość typu D. Now Psychol. 2006, 11, 69–79. [Google Scholar]
- Strober, L.B. Personality in multiple sclerosis (MS): Impact on health, psychological well-being, coping, and overall quality of life. Psychol. Health Med. 2017, 22, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Demirci, S.; Demirci, K.; Demirci, S. The effect of type D personality on quality of life in patients with multiple sclerosis. Noropsikiyatri Ars. 2017, 54, 272–276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lorefice, L.; Fenu, G.; Frau, J.; Coghe, G.; Marrosu, M.G.; Cocco, E. The burden of multiple sclerosis and patients’ coping strategies. BMJ Support. Palliat. Care 2018, 8, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Gazioglu, S.; Cakmak, V.A.; Ozkorumak, E.; Usta, N.C.; Ates, C.; Boz, C. Personality traits of patients with multiple sclerosis and their relationship with clinical characteristics. J. Nerv. Ment. Dis. 2014, 202, 408–411. [Google Scholar] [CrossRef]
- Goretti, B.; Portaccio, E.; Zipoli, V.; Razzolini, L.; Amato, M.P. Coping strategies, cognitive impairment, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol. Sci. 2010, 31, 227–230. [Google Scholar] [CrossRef]
- Nielsen-Prohl, J.; Saliger, J.; Güldenberg, V.; Breier, G.; Karbe, H. Stress-stimulated volitional coping competencies and depression in multiple sclerosis. J. Psychosom. Res. 2013, 74, 221–226. [Google Scholar] [CrossRef]
- Kroencke, D.C.; Denney, D.R. Stress and coping in multiple sclerosis: Exacerbation, remission and chronic subgroups. Mult. Scler. J. 1999, 5, 89–93. [Google Scholar] [CrossRef]
- Rätsep, T.; Kallasmaa, T.; Pulver, A.; Gross-Paju, K. Personality as a predictor of coping efforts in patients with multiple sclerosis. Mult. Scler. J. 2000, 6, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Gioia, M.C.; Cerasa, A.; Valentino, P.; Fera, F.; Nisticò, R.; Liguori, M.; Lanza, P.; Quattrone, A. Neurofunctional correlates of personality traits in relapsing-remitting multiple sclerosis: An fMRI study. Brain Cogn. 2009, 71, 320–327. [Google Scholar] [CrossRef]
- Lynch, S.G.; Kroencke, D.C.; Denney, D.R. The relationship between disability and depression in multiple sclerosis: The role of uncertainty, coping, and hope. Mult. Scler. J. 2001, 7, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.F.; Tennant, C.C.; Sharrock, M.; Hodgkinson, S.; Dunn, S.M.; Pollard, J.M. Relationship between stress and relapse in multiple sclerosis: Part II. Direct and indirect relationships. Mult. Scler. J. 2006, 12, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.E.; Foley, F.W.; Rao, S.M.; Bernardin, L.J.; Lee, H.; Genderson, M.W. Stress and course of disease in multiple sclerosis. Behav. Med. 1999, 25, 110–116. [Google Scholar] [CrossRef]
- Nowaczyk, N.; Cierpialkowska, L. Psychological profiles of patients with multiple sclerosis based on Hobfoll’s conservation of resources theory. Health Psychol. Rep. 2016, 4, 332–339. [Google Scholar] [CrossRef]
- Lode, K.; Bru, E.; Klevan, G.; Myhr, K.M.; Nyland, H.; Larsen, J.P. Coping with multiple sclerosis: A 5-year follow-up study. Acta Neurol. Scand. 2010, 122, 336–342. [Google Scholar] [CrossRef]
- Buljevac, D.; Hop, W.C.J.; Reedeker, W.; Janssens, A.C.J.W.; Van Doorn, P.A.; Hintzen, R.Q. Self reported stressful life events and exacerbations in multiple sclerosis: Prospective study. BMJ 2003, 327, 646. [Google Scholar] [CrossRef][Green Version]
- Abdollahpour, I.; Nedjat, S.; Mansournia, M.A.; Eckert, S.; Weinstock-Guttman, B. Stress-full life events and multiple sclerosis: A population-based incident case-control study. Mult. Scler. Relat. Disord. 2018, 26, 168–172. [Google Scholar] [CrossRef]
- Mohr, D.C.; Hart, S.L.; Julian, L.; Cox, D.; Pelletier, D. Association between stressful life events and exacerbation in multiple sclerosis: A meta-analysis. Br. Med. J. 2004, 328, 731–733. [Google Scholar] [CrossRef] [PubMed]
- Mitsonis, C.I.; Zervas, I.M.; Mitropoulos, P.A.; Dimopoulos, N.P.; Soldatos, C.R.; Potagas, C.M.; Sfagos, C.A. The impact of stressful life events on risk of relapse in women with multiple sclerosis: A prospective study. Eur. Psychiatry 2008, 23, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.F.; Tennant, C.C.; Sharrock, M.; Hodgkinson, S.; Dunn, S.M.; Pollard, J.D. Relationship between stress and relapse in multiple sclerosis: Part I. Important features. Mult. Scler. J. 2006, 12, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, R.; Fontanillas, L.; Salmaggi, A.; La Mantia, L.; Milanese, C. Stressful life events and multiple sclerosis: A retrospective study. Ital. J. Neurol. Sci. 1998, 19, 259–260. [Google Scholar] [CrossRef]
- Liu, X.J.; Ye, H.X.; Li, W.P.; Dai, R.; Chen, D.; Jin, M. Relationship between psychosocial factors and onset of multiple sclerosis. Eur. Neurol. 2009, 62, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Kern, S.; Schrempf, W.; Schneider, H.; Schultheiß, T.; Reichmann, H.; Ziemssen, T. Neurological disability, psychological distress, and health-related quality of life in MS patients within the first three years after diagnosis. Mult. Scler. J. 2009, 15, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Riise, T.; Mohr, D.C.; Munger, K.L.; Rich-Edwards, J.W.; Kawachi, I.; Ascherio, A. Stress and the risk of multiple sclerosis. Neurology 2011, 76, 1866–1871. [Google Scholar] [CrossRef]
- Gasperini, C.; Grasso, M.G.; Fiorelli, M.; Millefiorini, E.; Morino, S.; Anzini, A.; Colleluori, A.; Salvetti, M.; Buttinelli, C.; Pozzilli, C. A controlled study of potential risk factors preceding exacerbation in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1995, 59, 303–305. [Google Scholar] [CrossRef][Green Version]
- Oveisgharan, S.; Hosseini, S.; Arbabi, M.; Nafissi, S. Stress differentially predicts multiple sclerosis relapses. Neurol. Asia 2014, 19, 53–58. [Google Scholar]
- Somer, E.; Golan, D.; Dishon, S.; Cuzin-Disegni, L.; Lavi, I.; Miller, A. Patients with multiple sclerosis in a war zone: Coping strategies associated with reduced risk for relapse. Mult. Scler. J. 2010, 16, 463–471. [Google Scholar] [CrossRef]
- Nisipeanu, P.; Korczyn, A. Psychological stress as risk factor for exacerbations in multiple sclerosis. Neurology 1993, 43, 1311–1312. [Google Scholar] [CrossRef] [PubMed]
- McCabe, M. A longitudinal study of coping strategies and quality of life among people with multiple sclerosis. J. Clin. Psychol. Med. Settings 2006, 13, 367–377. [Google Scholar] [CrossRef]
- Dennison, L.; Moss-Morris, R.; Chalder, T. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin. Psychol. Rev. 2009, 29, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Aikens, J.E.; Fischer, J.S.; Namey, M.; Rudick, R.A. A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. J. Behav. Med. 1997, 20, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Barlow, J.; Turner, A.; Edwards, R.; Gilchrist, M. A randomised controlled trial of lay-led self-management for people with multiple sclerosis. Patient Educ. Couns. 2009, 77, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Bombardier, C.; Cunniffe, M.; Wadhwani, R.; Gibbons, L.; Blake, K.; Kraft, G. The Efficacy of Telephone Counseling for Health Promotion in People With Multiple Sclerosis: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2008, 89, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Tesar, N.; Bandion, K.; Baumhackl, U. Efficacy of a neuropsychological training programme for patients with multiple sclerosis -A randomised controlled trial. Wien. Klin. Wochenschr. 2005, 117, 747–754. [Google Scholar] [CrossRef] [PubMed]
| Mean | SD | MIN | MAX | Median | |
|---|---|---|---|---|---|
| Disease duration (years) | 7.25 | 5.34 | 1 | 28 | 6 |
| Duration of treatment | 3.44 | 3.07 | 0.5 | 13 | 2.5 |
| EDSS | 2.05 | 5.4 | 1 | 6 | 2 |
| MSSS | 3.28 | 1.61 | 0.76 | 6.46 | 2.87 |
| Number | % | |
|---|---|---|
| Place of residence | ||
| Rural | 22 | 33.8 |
| Urban | 43 | 66.2 |
| Marital status | ||
| Single | 13 | 20 |
| Married | 40 | 61.5 |
| Divorced | 5 | 7.7 |
| Other | 7 | 10.8 |
| Level of education | ||
| Vocational | 5 | 7.7 |
| Secondary education | 24 | 36.9 |
| Higher education | 36 | 55.4 |
| Occupational status | ||
| Studying | 2 | 3 |
| Working | 52 | 80 |
| Unnemployed | 4 | 6.2 |
| Pension/retiremet | 7 | 10.8 |
| Mean | SD | MIN | MAX | Median | |
|---|---|---|---|---|---|
| PSS-10 | 16.9 | 6.7 | 3.0 | 28 | 17 |
| DS-14 NEG | 12.4 | 7.1 | 0 | 27 | 12 |
| DS-14 SI | 8.97 | 6.38 | 0 | 25 | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotas, R.; Nowakowska-Kotas, M.; Budrewicz, S.; Pokryszko-Dragan, A. The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. J. Clin. Med. 2021, 10, 3916. https://doi.org/10.3390/jcm10173916
Kotas R, Nowakowska-Kotas M, Budrewicz S, Pokryszko-Dragan A. The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. Journal of Clinical Medicine. 2021; 10(17):3916. https://doi.org/10.3390/jcm10173916
Chicago/Turabian StyleKotas, Roman, Marta Nowakowska-Kotas, Sławomir Budrewicz, and Anna Pokryszko-Dragan. 2021. "The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course" Journal of Clinical Medicine 10, no. 17: 3916. https://doi.org/10.3390/jcm10173916
APA StyleKotas, R., Nowakowska-Kotas, M., Budrewicz, S., & Pokryszko-Dragan, A. (2021). The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. Journal of Clinical Medicine, 10(17), 3916. https://doi.org/10.3390/jcm10173916







