Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature
Abstract
:1. Introduction
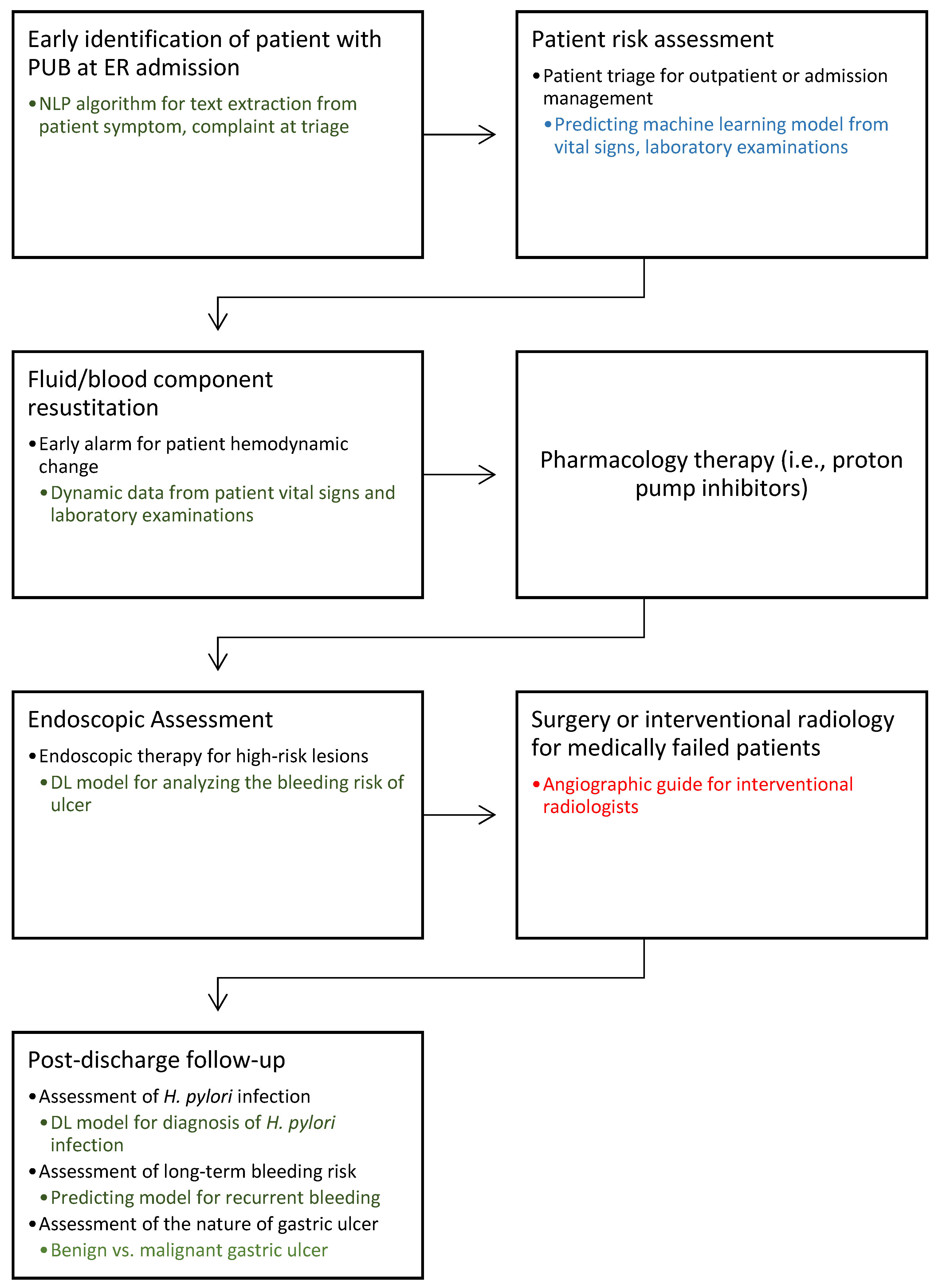
2. Application of AI in the Pre-Endoscopy Period for Patient Risk Assessment
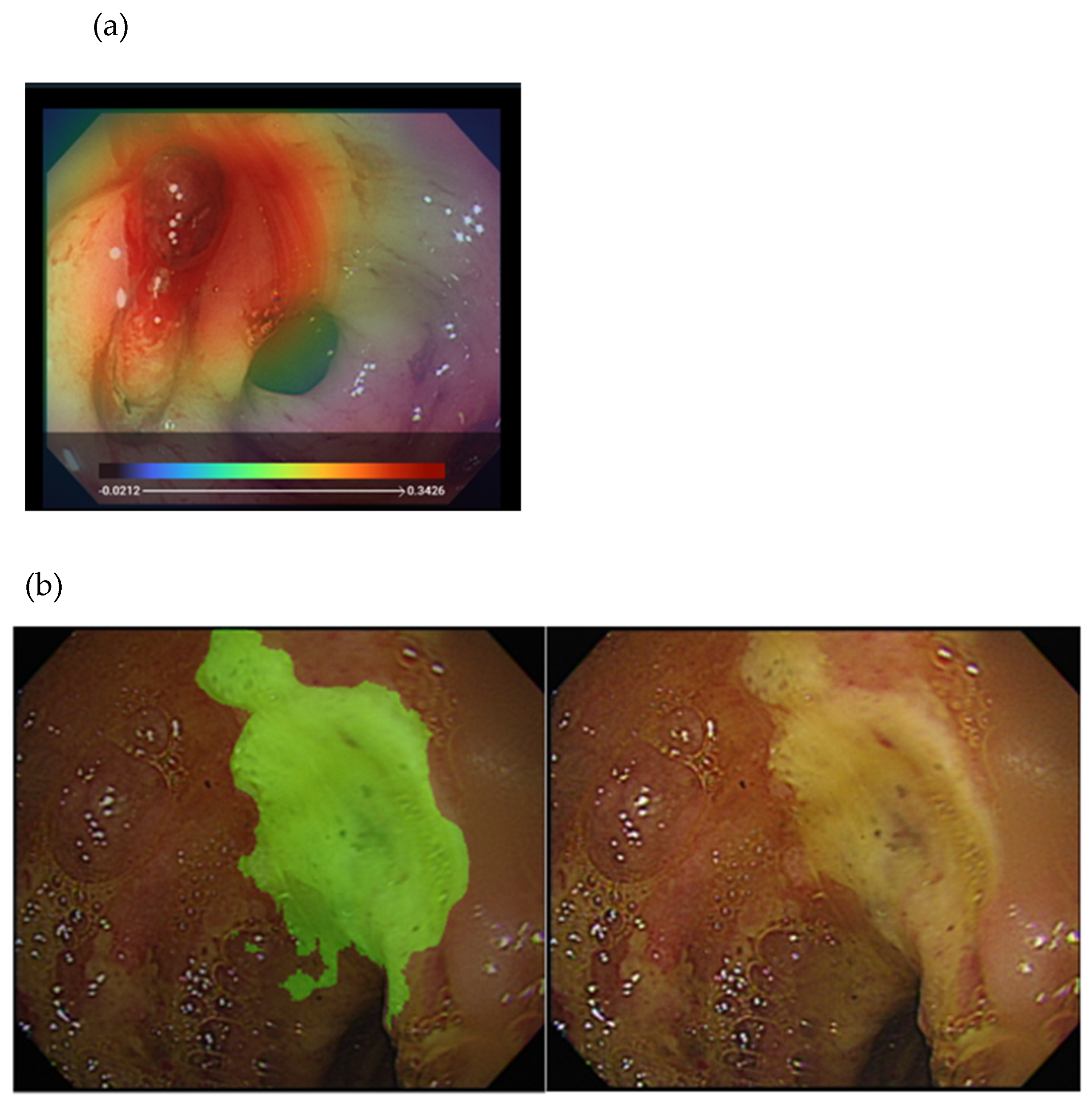
3. Application of AI during Endoscopy
4. Application of AI for Patient Care after a Bleeding Episode
5. Research Perspective on AI for PUB Management
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waddell, K.M.; Stanley, A.J.; Morris, A.J. Endoscopy for upper gastrointestinal bleeding: Where are we in 2017? Frontline Gastroenterol. 2017, 8, 94–97. [Google Scholar] [CrossRef] [Green Version]
- Penny, H.A.; Kurien, M.; Wong, E.; Ahmed, R.; Ejenavi, E.; Lau, M.; Romaya, C.; Gohar, F.; Dear, K.L.; Kapur, K.; et al. Changing trends in the UK management of upper GI bleeding: Is there evidence of reduced UK training experience? Frontline Gastroenterol. 2016, 7, 67–72. [Google Scholar] [CrossRef] [Green Version]
- Gralnek, I.M.; Dumonceau, J.M.; Kuipers, E.J.; Lanas, A.; Sanders, D.S.; Kurien, M.; Rotondano, G.; Hucl, T.; Dinis-Ribeiro, M.; Marmo, R.; et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015, 47, a1–a46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, L.H.S.; Sung, J.J.Y. Treatment of upper gastrointestinal bleeding in 2020: New techniques and outcomes. Dig. Endosc. 2021, 33, 83–94. [Google Scholar] [CrossRef]
- Shivaraju, A.; Patel, V.; Fonarow, G.C.; Xie, H.; Shroff, A.R.; Vidovich, M.I. Temporal trends in gastrointestinal bleeding associated with percutaneous coronary intervention: Analysis of the 1998–2006 Nationwide Inpatient Sample (NIS) database. Am. Heart J. 2011, 162, 1062–1068.e5. [Google Scholar] [CrossRef] [Green Version]
- Barkun, A.N.; Almadi, M.; Kuipers, E.J.; Laine, L.; Sung, J.; Tse, F.; Leontiadis, G.I.; Abraham, N.S.; Calvet, X.; Chan, F.K.L.; et al. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann. Intern. Med. 2019, 171, 805–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, J.J.; Chiu, P.W.; Chan, F.K.L.; Lau, J.Y.; Goh, K.L.; Ho, L.H.; Jung, H.Y.; Sollano, J.D.; Gotoda, T.; Reddy, N.; et al. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: An update 2018. Gut 2018, 67, 1757–1768. [Google Scholar] [CrossRef] [PubMed]
- El Hajjar, A.; Rey, J.F. Artificial intelligence in gastrointestinal endoscopy: General overview. Chin. Med. J. 2020, 133, 326–334. [Google Scholar] [CrossRef]
- Laine, L.; Barkun, A.N.; Saltzman, J.R.; Martel, M.; Leontiadis, G.I. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am. J. Gastroenterol. 2021, 116, 899–917. [Google Scholar] [CrossRef]
- Shung, D.; Tsay, C.; Laine, L.; Chang, D.; Li, F.; Thomas, P.; Partridge, C.; Simonov, M.; Hsiao, A.; Tay, J.K.; et al. Early identification of patients with acute gastrointestinal bleeding using natural language processing and decision rules. J. Gastroenterol. Hepatol. 2021, 36, 1590–1597. [Google Scholar] [CrossRef]
- Stanley, A.J.; Ashley, D.; Dalton, H.R.; Mowat, C.; Gaya, D.R.; Thompson, E.; Warshow, U.; Groome, M.; Cahill, A.; Benson, G.; et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: Multicentre validation and prospective evaluation. Lancet 2009, 373, 42–47. [Google Scholar] [CrossRef]
- Rockall, T.A.; Logan, R.F.; Devlin, H.B.; Northfield, T.C. Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996, 38, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Choi, J.; Shin, W.C. AIMS65 scoring system is comparable to Glasgow-Blatchford score or Rockall score for prediction of clinical outcomes for non-variceal upper gastrointestinal bleeding. BMC Gastroenterol. 2019, 19, 136. [Google Scholar] [CrossRef] [Green Version]
- Robertson, M.; Majumdar, A.; Boyapati, R.; Chung, W.; Worland, T.; Terbah, R.; Wei, J.; Lontos, S.; Angus, P.; Vaughan, R. Risk stratification in acute upper GI bleeding: Comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc. 2016, 83, 1151–1160. [Google Scholar] [CrossRef]
- Hyett, B.H.; Abougergi, M.S.; Charpentier, J.P.; Kumar, N.L.; Brozovic, S.; Claggett, B.L.; Travis, A.C.; Saltzman, J.R. The AIMS65 score compared with the Glasgow-Blatchford score in predicting outcomes in upper GI bleeding. Gastrointest Endosc. 2013, 77, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Shung, D.; Simonov, M.; Gentry, M.; Au, B.; Laine, L. Machine Learning to Predict Outcomes in Patients with Acute Gastrointestinal Bleeding: A Systematic Review. Dig. Dis. Sci. 2019, 64, 2078–2087. [Google Scholar] [CrossRef]
- Seo, D.W.; Yi, H.; Park, B.; Kim, Y.J.; Jung, D.H.; Woo, I.; Sohn, C.H.; Ko, B.S.; Kim, N.; Kim, W.Y. Prediction of Adverse Events in Stable Non-Variceal Gastrointestinal Bleeding Using Machine Learning. J. Clin. Med. 2020, 9, 2603. [Google Scholar] [CrossRef]
- Shung, D.L.; Au, B.; Taylor, R.A.; Tay, J.K.; Laursen, S.B.; Stanley, A.J.; Dalton, H.R.; Ngu, J.; Schultz, M.; Laine, L. Validation of a Machine Learning Model That Outperforms Clinical Risk Scoring Systems for Upper Gastrointestinal Bleeding. Gastroenterology 2020, 158, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Levi, R.; Carli, F.; Arevalo, A.R.; Altinel, Y.; Stein, D.J.; Naldini, M.M.; Grassi, F.; Zanoni, A.; Finkelstein, S.; Vieira, S.M.; et al. Artificial intelligence-based prediction of transfusion in the intensive care unit in patients with gastrointestinal bleeding. BMJ Health Care Inform. 2021, 28, e100245. [Google Scholar] [CrossRef]
- Forrest, J.A.; Finlayson, N.D.; Shearman, D.J. Endoscopy in gastrointestinal bleeding. Lancet 1974, 2, 394–397. [Google Scholar] [CrossRef]
- Yen, H.H.; Yang, C.W.; Su, W.W.; Soon, M.S.; Wu, S.S.; Lin, H.J. Oral versus intravenous proton pump inhibitors in preventing re-bleeding for patients with peptic ulcer bleeding after successful endoscopic therapy. BMC Gastroenterol. 2012, 12, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, H.H.; Yang, C.W.; Su, P.Y.; Su, W.W.; Soon, M.S. Use of hemostatic forceps as a preoperative rescue therapy for bleeding peptic ulcers. Surg. Laparosc. Endosc. Percutan. Tech. 2011, 21, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Brullet, E.; Garcia-Iglesias, P.; Calvet, X.; Papo, M.; Planella, M.; Pardo, A.; Junquera, F.; Montoliu, S.; Ballester, R.; Martinez-Bauer, E.; et al. Endoscopist’s Judgment Is as Useful as Risk Scores for Predicting Outcome in Peptic Ulcer Bleeding: A Multicenter Study. J. Clin. Med. 2020, 9, 408. [Google Scholar] [CrossRef] [Green Version]
- Laine, L.; Freeman, M.; Cohen, H. Lack of uniformity in evaluation of endoscopic prognostic features of bleeding ulcers. Gastrointest. Endosc. 1994, 40, 411–417. [Google Scholar] [CrossRef]
- Mondardini, A.; Barletti, C.; Rocca, G.; Garripoli, A.; Sambataro, A.; Perotto, C.; Repici, A.; Ferrari, A. Non-variceal upper gastrointestinal bleeding and Forrest’s classification: Diagnostic agreement between endoscopists from the same area. Endoscopy 1998, 30, 508–512. [Google Scholar] [CrossRef]
- Yen, H.-H.; Wu, P.-Y.; Su, P.-Y.; Yang, C.-W.; Chen, Y.-Y.; Chen, M.-F.; Lin, W.-C.; Tsai, C.-L.; Lin, K.-P. Performance Comparison of the Deep Learning and the Human Endoscopist for Bleeding Peptic Ulcer Disease. J. Med. Biol. Eng. 2021, 41, 504–513. [Google Scholar] [CrossRef]
- Deshmukh, F.; Merchant, S.S. Explainable Machine Learning Model for Predicting GI Bleed Mortality in the Intensive Care Unit. Am. J. Gastroenterol. 2020, 115, 1657–1668. [Google Scholar] [CrossRef] [PubMed]
- Tan, Q.; Ma, A.J.; Deng, H.; Wong, V.W.; Tse, Y.K.; Yip, T.C.; Wong, G.L.; Ching, J.Y.; Chan, F.K.; Yuen, P.C. A Hybrid Residual Network and Long Short-Term Memory Method for Peptic Ulcer Bleeding Mortality Prediction. AMIA Annu. Symp. Proc. 2018, 2018, 998–1007. [Google Scholar]
- Tan, Q.; Ye, M.; Ma, A.J.; Yip, T.C.; Wong, G.L.; Yuen, P.C. Importance-aware personalized learning for early risk prediction using static and dynamic health data. J. Am. Med. Inform. Assoc. 2021, 28, 713–726. [Google Scholar] [CrossRef]
- Mohan, B.P.; Khan, S.R.; Kassab, L.L.; Ponnada, S.; Mohy-Ud-Din, N.; Chandan, S.; Dulai, P.S.; Kochhar, G.S. Convolutional neural networks in the computer-aided diagnosis of Helicobacter pylori infection and non-causal comparison to physician endoscopists: A systematic review with meta-analysis. Ann. Gastroenterol. 2021, 34, 20–25. [Google Scholar] [CrossRef]
- Wong, G.L.; Ma, A.J.; Deng, H.; Ching, J.Y.; Wong, V.W.; Tse, Y.K.; Yip, T.C.; Lau, L.H.; Liu, H.H.; Leung, C.M.; et al. Machine learning model to predict recurrent ulcer bleeding in patients with history of idiopathic gastroduodenal ulcer bleeding. Aliment. Pharmacol. Ther. 2019, 49, 912–918. [Google Scholar] [CrossRef]
- Wong, G.L.H.; Lau, L.H.S.; Ching, J.Y.L.; Tse, Y.K.; Ling, R.H.Y.; Wong, V.W.S.; Chiu, P.W.Y.; Lau, J.Y.W.; Chan, F.K.L. Prevention of recurrent idiopathic gastroduodenal ulcer bleeding: A double-blind, randomised trial. Gut 2020, 69, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Chi, T. Biopsy in emergency gastroscopy does not increase the risk of rebleeding in patients with Forrest I acute nonvariceal upper gastrointestinal bleeding combined with suspected malignant gastric ulcer: A multicenter retrospective cohort study. BMC Gastroenterol. 2021, 21, 250. [Google Scholar] [CrossRef]
- Klang, E.; Barash, Y.; Levartovsky, A.; Barkin Lederer, N.; Lahat, A. Differentiation Between Malignant and Benign Endoscopic Images of Gastric Ulcers Using Deep Learning. Clin. Exp. Gastroenterol. 2021, 14, 155–162. [Google Scholar] [CrossRef]
- Cho, B.J.; Bang, C.S.; Park, S.W.; Yang, Y.J.; Seo, S.I.; Lim, H.; Shin, W.G.; Hong, J.T.; Yoo, Y.T.; Hong, S.H.; et al. Automated classification of gastric neoplasms in endoscopic images using a convolutional neural network. Endoscopy 2019, 51, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Namikawa, K.; Hirasawa, T.; Nakano, K.; Ikenoyama, Y.; Ishioka, M.; Shiroma, S.; Tokai, Y.; Yoshimizu, S.; Horiuchi, Y.; Ishiyama, A.; et al. Artificial intelligence-based diagnostic system classifying gastric cancers and ulcers: Comparison between the original and newly developed systems. Endoscopy 2020, 52, 1077–1083. [Google Scholar] [CrossRef]
- Yoon, H.J.; Kim, S.; Kim, J.H.; Keum, J.S.; Oh, S.I.; Jo, J.; Chun, J.; Youn, Y.H.; Park, H.; Kwon, I.G.; et al. A Lesion-Based Convolutional Neural Network Improves Endoscopic Detection and Depth Prediction of Early Gastric Cancer. J. Clin. Med. 2019, 8, 1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, L.; Wang, J.; He, X.; Zhu, Y.; Jiang, X.; Chen, Y.; Wang, Y.; Huang, L.; Shang, R.; Dong, Z.; et al. Deep learning system compared with expert endoscopists in predicting early gastric cancer and its invasion depth and differentiation status (with videos). Gastrointest. Endosc. 2021, 21, S0016-5107. [Google Scholar] [CrossRef]
- Siau, K.; Hearnshaw, S.; Stanley, A.J.; Estcourt, L.; Rasheed, A.; Walden, A.; Thoufeeq, M.; Donnelly, M.; Drummond, R.; Veitch, A.M.; et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020, 11, 311–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, Y.; Barkun, A.N.; Martel, M.; REASON investigators. Adherence to guidelines: A national audit of the management of acute upper gastrointestinal bleeding. The REASON registry. Can. J. Gastroenterol. Hepatol. 2014, 28, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Thompson, W.H.; Wright, J.; Bissett, P.G.; Poldrack, R.A. Dataset decay and the problem of sequential analyses on open datasets. Elife 2020, 9, e53498. [Google Scholar] [CrossRef] [PubMed]
- Borgli, H.; Thambawita, V.; Smedsrud, P.H.; Hicks, S.; Jha, D.; Eskeland, S.L.; Randel, K.R.; Pogorelov, K.; Lux, M.; Nguyen, D.T.D.; et al. HyperKvasir, a comprehensive multi-class image and video dataset for gastrointestinal endoscopy. Sci. Data 2020, 7, 283. [Google Scholar] [CrossRef]
- Garcia-Peraza-Herrera, L.C.; Everson, M.; Lovat, L.; Wang, H.P.; Wang, W.L.; Haidry, R.; Stoyanov, D.; Ourselin, S.; Vercauteren, T. Intrapapillary capillary loop classification in magnification endoscopy: Open dataset and baseline methodology. Int. J. Comput. Assist. Radiol. Surg. 2020, 15, 651–659. [Google Scholar] [CrossRef] [Green Version]
- Loffroy, R. Endoscopy-guided empiric arterial embolization for angiographically negative upper gastrointestinal bleeding: Use it without fear! Cardiovasc. Intervent. Radiol. 2013, 36, 867–868. [Google Scholar] [CrossRef]
- Yu, Q.; Funaki, B.; Navuluri, R.; Zangan, S.; Zhang, A.; Cao, D.; Leef, J.; Ahmed, O. Empiric Transcatheter Embolization for Acute Arterial Upper Gastrointestinal Bleeding: A Meta-Analysis. AJR Am. J. Roentgenol. 2021, 216, 880–893. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.H.; Lee, D.Y.; Cha, W.C.; Chung, M.J.; Lee, K.S.; Cho, B.H.; Choi, J.H. Automatic stenosis recognition from coronary angiography using convolutional neural networks. Comput. Methods Programs Biomed. 2021, 198, 105819. [Google Scholar] [CrossRef]
- Loffroy, R.; Falvo, N.; Nakai, M.; Pescatori, L.; Midulla, M.; Chevallier, O. When all else fails—Radiological management of severe gastrointestinal bleeding. Best Pract. Res. Clin. Gastroenterol. 2019, 42–43, 101612. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yen, H.-H.; Wu, P.-Y.; Chen, M.-F.; Lin, W.-C.; Tsai, C.-L.; Lin, K.-P. Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature. J. Clin. Med. 2021, 10, 3527. https://doi.org/10.3390/jcm10163527
Yen H-H, Wu P-Y, Chen M-F, Lin W-C, Tsai C-L, Lin K-P. Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature. Journal of Clinical Medicine. 2021; 10(16):3527. https://doi.org/10.3390/jcm10163527
Chicago/Turabian StyleYen, Hsu-Heng, Ping-Yu Wu, Mei-Fen Chen, Wen-Chen Lin, Cheng-Lun Tsai, and Kang-Ping Lin. 2021. "Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature" Journal of Clinical Medicine 10, no. 16: 3527. https://doi.org/10.3390/jcm10163527
APA StyleYen, H.-H., Wu, P.-Y., Chen, M.-F., Lin, W.-C., Tsai, C.-L., & Lin, K.-P. (2021). Current Status and Future Perspective of Artificial Intelligence in the Management of Peptic Ulcer Bleeding: A Review of Recent Literature. Journal of Clinical Medicine, 10(16), 3527. https://doi.org/10.3390/jcm10163527





