Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
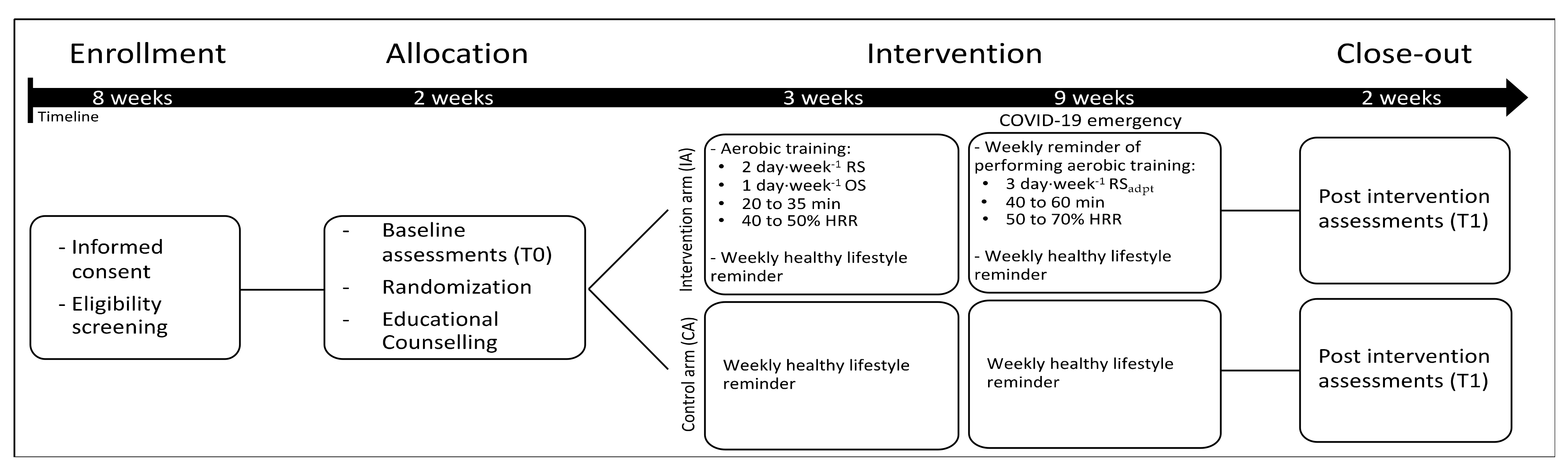
2.2. Study Design
2.3. Lifestyle Intervention
2.4. Assessments
2.4.1. Anthropometrics and Body Composition
2.4.2. Dietary Habits and Physical Activity Level
2.4.3. Cardiorespiratory Fitness
2.4.4. Cardiovascular Parameters
2.4.5. Metabolic, Hormonal, and Inflammatory Parameters
2.5. Statistical Analyses
3. Results
3.1. Changes in Anthropometric, Body Composition, Physical Activity Level, Dietary Habits, and Cardiorespiratory Fitness
3.2. Changes in Cardiovascular Parameters
3.3. Changes in Metabolic, Hormonal, and Inflammatory Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ortenzi, F.; Albanese, E.; Fadda, M. A Transdisciplinary Analysis of COVID-19 in Italy: The Most Affected Country in Europe. Int. J. Env. Res Public Health 2020, 17, 9488. [Google Scholar] [CrossRef] [PubMed]
- Oldani, C.; Vanni, G.; Buonomo, O.C. COVID-19 Unintended Effects on Breast Cancer in Italy after the Great Lockdown. Front. Public Health 2020, 8, 601748. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef]
- AIOM AIRTUM PASSI PASSI d’Argento And SIAPEC-IAP Working Group. I numeri del cancro in Italia 2019, 9th ed.; Intermedia: Brescia, Italy, 2019. [Google Scholar]
- Nardin, S.; Mora, E.; Varughese, F.M.; D’Avanzo, F.; Vachanaram, A.R.; Rossi, V.; Saggia, C.; Rubinelli, S.; Gennari, A. Breast Cancer Survivorship, Quality of Life, and Late Toxicities. Front. Oncol. 2020, 10, 864. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Russo, A.; Autelitano, M.; Bisanti, L. Metabolic syndrome and cancer risk. Eur. J. Cancer 2008, 44, 293–297. [Google Scholar] [CrossRef]
- Pasanisi, P.; Berrino, F.; De Petris, M.; Venturelli, E.; Mastroianni, A.; Panico, S. Metabolic syndrome as a prognostic factor for breast cancer recurrences. Int. J. Cancer 2006, 119, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Mills, R.C. Breast Cancer Survivors, Common Markers of Inflammation, and Exercise: A Narrative Review. Breast Cancer 2017, 11, 1178223417743976. [Google Scholar] [CrossRef]
- Harbeck, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast cancer. Nat. Rev. Dis. Primers 2019, 5, 66. [Google Scholar] [CrossRef]
- Biganzoli, L.; Cardoso, F.; Beishon, M.; Cameron, D.; Cataliotti, L.; Coles, C.E.; Delgado Bolton, R.C.; Trill, M.D.; Erdem, S.; Fjell, M.; et al. The requirements of a specialist breast centre. Breast 2020, 51, 65–84. [Google Scholar] [CrossRef]
- Irwin, M.L.; McTiernan, A.; Baumgartner, R.N.; Baumgartner, K.B.; Bernstein, L.; Gilliland, F.D.; Ballard-Barbash, R. Changes in body fat and weight after a breast cancer diagnosis: Influence of demographic, prognostic, and lifestyle factors. J. Clin. Oncol. 2005, 23, 774–782. [Google Scholar] [CrossRef]
- Dieli-Conwright, C.M.; Orozco, B.Z. Exercise after breast cancer treatment: Current perspectives. Breast Cancer Targets Ther. 2015, 7, 353–362. [Google Scholar] [CrossRef]
- Schmidt, M.E.; Wiskemann, J.; Armbrust, P.; Schneeweiss, A.; Ulrich, C.M.; Steindorf, K. Effects of resistance exercise on fatigue and quality of life in breast cancer patients undergoing adjuvant chemotherapy: A randomized controlled trial. Int. J. Cancer 2015, 137, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Meneses-Echávez, J.F.; Correa-Bautista, J.E.; González-Jiménez, E.; Schmidt Río-Valle, J.; Elkins, M.R.; Lobelo, F.; Ramírez-Vélez, R. The Effect of Exercise Training on Mediators of Inflammation in Breast Cancer Survivors: A Systematic Review with Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2016, 25, 1009–1017. [Google Scholar] [CrossRef]
- De Cicco, P.; Catani, M.V.; Gasperi, V.; Sibilano, M.; Quaglietta, M.; Savini, I. Nutrition and Breast Cancer: A Literature Review on Prevention, Treatment and Recurrence. Nutrients 2019, 11, 1514. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L.; Doyle, C.; Demark-Wahnefried, W.; Meyerhardt, J.; Courneya, K.S.; Schwartz, A.L.; Bandera, E.V.; Hamilton, K.K.; Grant, B.; McCullough, M.; et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J. Clin. 2012, 62, 243–274. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, K.H.; Courneya, K.S.; Matthews, C.; Demark-Wahnefried, W.; Galvão, D.A.; Pinto, B.M.; Irwin, M.L.; Wolin, K.Y.; Segal, R.J.; Lucia, A.; et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med. Sci. Sports Exerc. 2010, 42, 1409–1426. [Google Scholar] [CrossRef]
- Grazioli, E.; Dimauro, I.; Mercatelli, N.; Wang, G.; Pitsiladis, Y.; Di Luigi, L.; Caporossi, D. Physical activity in the prevention of human diseases: Role of epigenetic modifications. BMC Genom. 2017, 18, 802. [Google Scholar] [CrossRef] [PubMed]
- Berrino, F.; Villarini, A.; Traina, A.; Bonanni, B.; Panico, S.; Mano, M.P.; Mercandino, A.; Galasso, R.; Barbero, M.; Simeoni, M.; et al. Metabolic syndrome and breast cancer prognosis. Breast Cancer Res. Treat. 2014, 147, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Bruno, E.; Gargano, G.; Villarini, A.; Traina, A.; Johansson, H.; Mano, M.P.; Santucci De Magistris, M.; Simeoni, M.; Consolaro, E.; Mercandino, A.; et al. Adherence to WCRF/AICR cancer prevention recommendations and metabolic syndrome in breast cancer patients. Int. J. Cancer 2016, 138, 237–244. [Google Scholar] [CrossRef]
- Van den Brink, W.; van Bilsen, J.; Salic, K.; Hoevenaars, F.P.M.; Verschuren, L.; Kleemann, R.; Bouwman, J.; Ronnett, G.V.; van Ommen, B.; Wopereis, S. Current and Future Nutritional Strategies to Modulate Inflammatory Dynamics in Metabolic Disorders. Front. Nutr. 2019, 6, 129. [Google Scholar] [CrossRef] [PubMed]
- Hojman, P.; Gehl, J.; Christensen, J.F.; Pedersen, B.K. Molecular Mechanisms Linking Exercise to Cancer Prevention and Treatment. Cell Metab. 2018, 27, 10–21. [Google Scholar] [CrossRef]
- Hojman, P. Exercise protects from cancer through regulation of immune function and inflammation. Biochem. Soc. Trans. 2017, 45, 905–911. [Google Scholar] [CrossRef]
- Seiler, A.; Chen, M.A.; Brown, R.L.; Fagundes, C.P. Obesity, Dietary Factors, Nutrition, and Breast Cancer Risk. Curr. Breast Cancer Rep. 2018, 10, 14–27. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. 3rd Export Report. 2018. Available online: https://www.wcrf.org/wp-content/uploads/2021/02/Summary-of-Third-Expert-Report-2018.pdf (accessed on 10 May 2021).
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. Cancer-related fatigue: ESMO Clinical Practice Guidelines for Diagnosis and Treatment. Ann. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Stefan, N.; Birkenfeld, A.L.; Schulze, M.B. Global pandemics interconnected-obesity, impaired metabolic health and COVID-19. Nat. Rev. Endocrinol. 2021, 17, 135–149. [Google Scholar] [CrossRef]
- Derosa, L.; Melenotte, C.; Griscelli, F.; Gachot, B.; Marabelle, A.; Kroemer, G.; Zitvogel, L. The immuno-oncological challenge of COVID-19. Nat. Cancer 2020, 1, 946–964. [Google Scholar] [CrossRef]
- Palaskas, N.L.; Koutroumpakis, E.; Deswal, A. COVID-19 and Cardiovascular Health among Patients with Cancer. Curr. Cardiol. Rep. 2020, 22, 171. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- American College of Sports Medicine; Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Gurgel, A.R.B.; Mingroni-Netto, P.; Farah, J.C.; de Brito, C.M.M.; Levin, A.S.; Brum, P.C. Determinants of Health and Physical Activity Levels among Breast Cancer Survivors during the COVID-19 Pandemic: A Cross-Sectional Study. Front. Physiol. 2021, 12, 624169. [Google Scholar] [CrossRef]
- Natalucci, V.; Villarini, M.; Emili, R.; Acito, M.; Vallorani, L.; Barbieri, E.; Villarini, A. Special Attention to Physical Activity in Breast Cancer Patients during the First Wave of COVID-19 Pandemic in Italy: The DianaWeb Cohort. J. Pers. Med. 2021, 11, 381. [Google Scholar] [CrossRef]
- Newton, R.U.; Hart, N.H.; Clay, T. Keeping Patients with Cancer Exercising in the Age of COVID-19. JCO Oncol. Pract. 2020, 16, 656–664. [Google Scholar] [CrossRef]
- Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur. J. Sport Sci. 2020, 1–22. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020, 87, 23–24. [Google Scholar] [CrossRef] [PubMed]
- Villarini, A.; Pasanisi, P.; Traina, A.; Mano, M.P.; Bonanni, B.; Panico, S.; Scipioni, C.; Galasso, R.; Paduos, A.; Simeoni, M.; et al. Lifestyle and breast cancer recurrences: The DIANA-5 trial. Tumori J. 2012, 98, 1–18. [Google Scholar] [CrossRef]
- Pistelli, M.; Natalucci, V.; Bastianelli, L.; Scortichini, L.; Agostinelli, V.; Merloni, F.; Savini, A.; Capecci, M.; Ceravolo, M.G.; Serrani, R.; et al. Assessing the impact of 12 months lifestyle interventions on breast cancer secondary prevention: A modeling approach. In In Proceedings of the San Antonio Breast Cancer Virtual Symposium, San Antonio, TX, USA , 7–10 December 2021; Volume 81, p. 4. [Google Scholar]
- Sternfeld, B.; Weltzien, E.; Quesenberry, C.P.; Castillo, A.L.; Kwan, M.; Slattery, M.L.; Caan, B.J. Physical Activity and Risk of Recurrence and mortality in breast cancer survivors: Findings from the LACE study. Cancer Epidemiol. Biomark. Prev. 2009, 18, 87–95. [Google Scholar] [CrossRef]
- Dieli-Conwright, C.M.; Lee, K.; Kiwata, J.L. Reducing the Risk of Breast Cancer Recurrence: An Evaluation of the Effects and Mechanisms of Diet and Exercise. Curr. Breast Cancer Rep. 2016, 8, 139–150. [Google Scholar] [CrossRef]
- Spencer, J.C.; Wheeler, S.B. A systematic review of Motivational Interviewing interventions in cancer patients and survivors. Patient Educ. Couns. 2016, 99, 1099–1105. [Google Scholar] [CrossRef]
- Ministero della Salute. Linee di Indirizzo Percorsi Nutrizionali Nei Pazienti Oncologici. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_2682_allegato.pdf (accessed on 10 May 2021).
- Ministero della Salute. Linee di Indirizzo Sull’attività Fisica per le Differenti Fasce D’età e con Riferimento a Situazioni Fisiologiche e Fisiopatologiche e a Sottogruppi Specifici di Popolazione. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_2828_allegato.pdf (accessed on 10 May 2021).
- Villarini, A.; Villarini, M.; Gargano, G.; Moretti, M.; Berrino, F. DianaWeb: A demonstration project to improve breast cancer prognosis through lifestyles. Epidemiol. E Prev. 2015, 39, 402–405. [Google Scholar]
- Gianfredi, V.; Nucci, D.; Balzarini, M.; Acito, M.; Moretti, M.; Villarini, A.; Villarini, M. E-Coaching: The DianaWeb study to prevent breast cancer recurrences. Clin. Ter. 2020, 170, e59–e65. [Google Scholar] [PubMed]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.W.; Eves, N.D.; Haykowsky, M.; Joy, A.A.; Douglas, P.S. Cardiorespiratory exercise testing in clinical oncology research: Systematic review and practice recommendations. Lancet Oncol. 2008, 9, 757–765. [Google Scholar] [CrossRef]
- Ferri Marini, C.; Correale, L.; Carnevale Pellino, V.; Federici, A.; Vandoni, M.; Lucertini, F. Assessing Maximal Oxygen Uptake: Creating Personalized Incremental Exercise Protocols Simply and Quickly. Strength Cond. J. 2021, 43, 86–92. [Google Scholar] [CrossRef]
- Gellish, R.L.; Goslin, B.R.; Olson, R.E.; McDonald, A.; Russi, G.D.; Moudgil, V.K. Longitudinal modeling of the relationship between age and maximal heart rate. Med. Sci. Sports Exerc. 2007, 39, 822–829. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J.-Cardiovasc. Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Malik, M. Heart Rate Variability. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef]
- Thygesen, K.; Mair, J.; Giannitsis, E.; Mueller, C.; Lindahl, B.; Blankenberg, S.; Huber, K.; Plebani, M.; Biasucci, L.M.; Tubaro, M.; et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur. Heart J. 2012, 33, 2252–2257. [Google Scholar] [CrossRef]
- Bondar, R.J.; Mead, D.C. Evaluation of glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides in the hexokinase method for determining glucose in serum. Clin. Chem. 1974, 20, 586–590. [Google Scholar] [CrossRef]
- Roeschlau, P.; Bernt, E.; Gruber, W. Enzymatic determination of total cholesterol in serum. Z Klin. Chem. Klin. Biochem. 1974, 12, 226. [Google Scholar]
- Bonora, E.; Targher, G.; Alberiche, M.; Bonadonna, R.C.; Saggiani, F.; Zenere, M.B.; Monauni, T.; Muggeo, M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: Studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 2000, 23, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Gerhard, I.; Runnebaum, B. Hormone load tests in the first half of pregnancy–A diagnostic and therapeutic approach. Biol. Res. Pregnancy Perinatol. 1984, 5, 157–173. [Google Scholar] [PubMed]
- Newman, J.D.; Handelsman, D.J. Challenges to the measurement of oestradiol: Comments on an endocrine society position statement. Clin. Biochem. Rev. 2014, 35, 75–79. [Google Scholar] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Elsevier Science: Amsterdam, The Netherlands, 1988. [Google Scholar]
- Kang, D.W.; Lee, J.; Suh, S.H.; Ligibel, J.; Courneya, K.S.; Jeon, J.Y. Effects of Exercise on Insulin, IGF Axis, Adipocytokines, and Inflammatory Markers in Breast Cancer Survivors: A Systematic Review and Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2017, 26, 355–365. [Google Scholar] [CrossRef]
- Arnett, D.K.; Khera, A.; Blumenthal, R.S. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Part 1, Lifestyle and Behavioral Factors. JAMA Cardiol. 2019, 4, 1043–1044. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Reis, R.S.; Salvo, D.; Ogilvie, D.; Lambert, E.V.; Goenka, S.; Brownson, R.C.; Committee, L.P.A.S.E. Scaling up physical activity interventions worldwide: Stepping up to larger and smarter approaches to get people moving. Lancet 2016, 388, 1337–1348. [Google Scholar] [CrossRef]
- Lashinger, L.M.; Rossi, E.L.; Hursting, S.D. Obesity and resistance to cancer chemotherapy: Interacting roles of inflammation and metabolic dysregulation. Clin. Pharmacol. Ther. 2014, 96, 458–463. [Google Scholar] [CrossRef]
- Irwin, M.L. Weight loss interventions and breast cancer survival: The time is now. J. Clin. Oncol. 2014, 32, 2197–2199. [Google Scholar] [CrossRef]
- Holick, C.N.; Newcomb, P.A.; Trentham-Dietz, A.; Titus-Ernstoff, L.; Bersch, A.J.; Stampfer, M.J.; Baron, J.A.; Egan, K.M.; Willett, W.C. Physical activity and survival after diagnosis of invasive breast cancer. Cancer Epidemiol. Biomark. Prev. 2008, 17, 379–386. [Google Scholar] [CrossRef]
- Biamonte, E.; Pegoraro, F.; Carrone, F.; Facchi, I.; Favacchio, G.; Lania, A.G.; Mazziotti, G.; Mirani, M. Weight change and glycemic control in type 2 diabetes patients during COVID-19 pandemic: The lockdown effect. Endocrine 2021, 72, 604–610. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Turati, F.; Carioli, G.; Bravi, F.; Ferraroni, M.; Serraino, D.; Montella, M.; Giacosa, A.; Toffolutti, F.; Negri, E.; Levi, F.; et al. Mediterranean Diet and Breast Cancer Risk. Nutrients 2018, 10, 326. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Schwedhelm, C.; Galbete, C.; Hoffmann, G. Adherence to Mediterranean Diet and Risk of Cancer: An Updated Systematic Review and Meta-Analysis. Nutrients 2017, 9, 1063. [Google Scholar] [CrossRef] [PubMed]
- Courneya, K.S.; Mackey, J.R.; Bell, G.J.; Jones, L.W.; Field, C.J.; Fairey, A.S. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: Cardiopulmonary and quality of life outcomes. J. Clin. Oncol. 2003, 21, 1660–1668. [Google Scholar] [CrossRef]
- Daley, A.J.; Crank, H.; Saxton, J.M.; Mutrie, N.; Coleman, R.; Roalfe, A. Randomized trial of exercise therapy in women treated for breast cancer. J. Clin. Oncol. 2007, 25, 1713–1721. [Google Scholar] [CrossRef] [PubMed]
- Vincent, F.; Labourey, J.L.; Leobon, S.; Antonini, M.T.; Lavau-Denes, S.; Tubiana-Mathieu, N. Effects of a home-based walking training program on cardiorespiratory fitness in breast cancer patients receiving adjuvant chemotherapy: A pilot study. Eur. J. Phys. Rehabil. Med. 2013, 49, 319–329. [Google Scholar]
- Ligibel, J.A.; Partridge, A.; Giobbie-Hurder, A.; Campbell, N.; Shockro, L.; Salinardi, T.; Salinardri, T.; Winer, E.P. Physical and psychological outcomes among women in a telephone-based exercise intervention during adjuvant therapy for early stage breast cancer. J. Women’s Health 2010, 19, 1553–1559. [Google Scholar] [CrossRef]
- Scott, E.; Daley, A.J.; Doll, H.; Woodroofe, N.; Coleman, R.E.; Mutrie, N.; Crank, H.; Powers, H.J.; Saxton, J.M. Effects of an exercise and hypocaloric healthy eating program on biomarkers associated with long-term prognosis after early-stage breast cancer: A randomized controlled trial. Cancer Causes Control 2013, 24, 181–191. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Ganesan, T.B. Sedentarism and chronic disease risk in COVID 19 lockdown-a scoping review. Scott. Med. J. 2021, 66, 3–10. [Google Scholar] [CrossRef]
- Jones, L.W.; Courneya, K.S.; Mackey, J.R.; Muss, H.B.; Pituskin, E.N.; Scott, J.M.; Hornsby, W.E.; Coan, A.D.; Herndon, J.E.; Douglas, P.S.; et al. Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J. Clin. Oncol. 2012, 30, 2530–2537. [Google Scholar] [CrossRef]
- Jones, L.W.; Eves, N.D.; Haykowsky, M.; Freedland, S.J.; Mackey, J.R. Exercise intolerance in cancer and the role of exercise therapy to reverse dysfunction. Lancet Oncol. 2009, 10, 598–605. [Google Scholar] [CrossRef]
- Koelwyn, G.J.; Khouri, M.; Mackey, J.R.; Douglas, P.S.; Jones, L.W. Running on empty: Cardiovascular reserve capacity and late effects of therapy in cancer survivorship. J. Clin. Oncol. 2012, 30, 4458–4461. [Google Scholar] [CrossRef]
- Jones, L.W.; Haykowsky, M.; Peddle, C.J.; Joy, A.A.; Pituskin, E.N.; Tkachuk, L.M.; Courneya, K.S.; Slamon, D.J.; Mackey, J.R. Cardiovascular risk profile of patients with HER2/neu-positive breast cancer treated with anthracycline-taxane-containing adjuvant chemotherapy and/or trastuzumab. Cancer Epidemiol. Biomark. Prev. 2007, 16, 1026–1031. [Google Scholar] [CrossRef]
- Jones, L.W.; Haykowsky, M.; Pituskin, E.N.; Jendzjowsky, N.G.; Tomczak, C.R.; Haennel, R.G.; Mackey, J.R. Cardiovascular reserve and risk profile of postmenopausal women after chemoendocrine therapy for hormone receptor–positive operable breast cancer. Oncologist 2007, 12, 1156–1164. [Google Scholar] [CrossRef]
- Upshaw, J.N.; Finkelman, B.; Hubbard, R.A.; Smith, A.M.; Narayan, H.K.; Arndt, L.; Domchek, S.; DeMichele, A.; Fox, K.; Shah, P.; et al. Comprehensive Assessment of Changes in Left Ventricular Diastolic Function With Contemporary Breast Cancer Therapy. JACC Cardiovasc. Imaging 2020, 13, 198–210. [Google Scholar] [CrossRef]
- Kloter, E.; Barrueto, K.; Klein, S.D.; Scholkmann, F.; Wolf, U. Heart Rate Variability as a Prognostic Factor for Cancer Survival-A Systematic Review. Front. Physiol. 2018, 9, 623. [Google Scholar] [CrossRef]
- Kangas, P.; Tikkakoski, A.; Uitto, M.; Viik, J.; Bouquin, H.; Niemelä, O.; Mustonen, J.; Pörsti, I. Metabolic syndrome is associated with decreased heart rate variability in a sex-dependent manner: A comparison between 252 men and 249 women. Clin. Physiol. Funct. Imaging 2019, 39, 160–167. [Google Scholar] [CrossRef]
- Thayer, J.F.; Ahs, F.; Fredrikson, M.; Sollers, J.J.; Wager, T.D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Lampert, R.; Bremner, J.D.; Su, S.; Miller, A.; Lee, F.; Cheema, F.; Goldberg, J.; Vaccarino, V. Decreased heart rate variability is associated with higher levels of inflammation in middle-aged men. Am. Heart J. 2008, 156, 759.e1–759.e7. [Google Scholar] [CrossRef]
- Lima-Silva, A.E.; Bertuzzi, R.; Dalquano, E.; Nogueira, M.; Casarini, D.; Kiss, M.A.; Ugrinowitsch, C.; Pires, F.O. Influence of high- and low-carbohydrate diet following glycogen-depleting exercise on heart rate variability and plasma catecholamines. Appl. Physiol. Nutr. Metab. 2010, 35, 541–547. [Google Scholar] [CrossRef]
- Toohey, K.; Pumpa, K.; McKune, A.; Cooke, J.; Welvaert, M.; Northey, J.; Quinlan, C.; Semple, S. The impact of high-intensity interval training exercise on breast cancer survivors: A pilot study to explore fitness, cardiac regulation and biomarkers of the stress systems. BMC Cancer 2020, 20, 787. [Google Scholar] [CrossRef]
- Fairey, A.S.; Courneya, K.S.; Field, C.J.; Bell, G.J.; Jones, L.W.; Mackey, J.R. Effects of exercise training on fasting insulin, insulin resistance, insulin-like growth factors, and insulin-like growth factor binding proteins in postmenopausal breast cancer survivors: A randomized controlled trial. Cancer Epidemiol. Biomark. Prev. 2003, 12, 721–727. [Google Scholar]
- Schmitz, K.H.; Holtzman, J.; Courneya, K.S.; Mâsse, L.C.; Duval, S.; Kane, R. Controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1588–1595. [Google Scholar] [CrossRef]
- Dittus, K.L.; Harvey, J.R.; Bunn, J.Y.; Kokinda, N.D.; Wilson, K.M.; Priest, J.; Pratley, R.E. Impact of a behaviorally-based weight loss intervention on parameters of insulin resistance in breast cancer survivors. BMC Cancer 2018, 18, 351. [Google Scholar] [CrossRef]
- Barchitta, M.; Maugeri, A.; Magnano San Lio, R.; Quattrocchi, A.; Degrassi, F.; Catalano, F.; Basile, G.; Agodi, A. The Effects of Diet and Dietary Interventions on the Quality of Life among Breast Cancer Survivors: A Cross-Sectional Analysis and a Systematic Review of Experimental Studies. Cancers 2020, 12, 322. [Google Scholar] [CrossRef] [PubMed]
- Van Kruijsdijk, R.C.; van der Wall, E.; Visseren, F.L. Obesity and cancer: The role of dysfunctional adipose tissue. Cancer Epidemiol. Biomark. Prev. 2009, 18, 2569–2578. [Google Scholar] [CrossRef]
- Pierce, B.L.; Ballard-Barbash, R.; Bernstein, L.; Baumgartner, R.N.; Neuhouser, M.L.; Wener, M.H.; Baumgartner, K.B.; Gilliland, F.D.; Sorensen, B.E.; McTiernan, A.; et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J. Clin. Oncol. 2009, 27, 3437–3444. [Google Scholar] [CrossRef]
- Olefsky, J.M.; Glass, C.K. Macrophages, inflammation, and insulin resistance. Annu. Rev. Physiol. 2010, 72, 219–246. [Google Scholar] [CrossRef]
- Kabat, G.C.; Kim, M.Y.; Lee, J.S.; Ho, G.Y.; Going, S.B.; Beebe-Dimmer, J.; Manson, J.E.; Chlebowski, R.T.; Rohan, T.E. Metabolic Obesity Phenotypes and Risk of Breast Cancer in Postmenopausal Women. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1730–1735. [Google Scholar] [CrossRef]
- Kerr, J.; Anderson, C.; Lippman, S.M. Physical activity, sedentary behaviour, diet, and cancer: An update and emerging new evidence. Lancet Oncol. 2017, 18, e457–e471. [Google Scholar] [CrossRef]
- Asegaonkar, S.B.; Asegaonkar, B.N.; Takalkar, U.V.; Advani, S.; Thorat, A.P. C-Reactive Protein and Breast Cancer: New Insights from Old Molecule. Int. J. Breast Cancer 2015, 2015, 145647. [Google Scholar] [CrossRef]
- Michigan, A.; Johnson, T.V.; Master, V.A. Review of the relationship between C-reactive protein and exercise. Mol. Diagn. Ther. 2011, 15, 265–275. [Google Scholar] [CrossRef]
- Frydenberg, H.; Thune, I.; Lofterød, T.; Mortensen, E.S.; Eggen, A.E.; Risberg, T.; Wist, E.A.; Flote, V.G.; Furberg, A.S.; Wilsgaard, T.; et al. Pre-diagnostic high-sensitive C-reactive protein and breast cancer risk, recurrence, and survival. Breast Cancer Res. Treat. 2016, 155, 345–354. [Google Scholar] [CrossRef]
- Bourdillon, N.; Yazdani, S.; Schmitt, L.; Millet, G.P. Effects of COVID-19 lockdown on heart rate variability. PLoS ONE 2020, 15, e0242303. [Google Scholar] [CrossRef] [PubMed]
- Raymond, E.; Thieblemont, C.; Alran, S.; Faivre, S. Impact of the COVID-19 Outbreak on the Management of Patients with Cancer. Target Oncol. 2020, 15, 249–259. [Google Scholar] [CrossRef]
- Curigliano, G. How to Guarantee the Best of Care to Patients with Cancer during the COVID-19 Epidemic: The Italian Experience. Oncologist 2020, 25, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Grazioli, E.; Cerulli, C.; Dimauro, I.; Moretti, E.; Murri, A.; Parisi, A. New Strategy of Home-Based Exercise during Pandemic COVID-19 in Breast Cancer Patients: A Case Study. Sustainability 2020, 12, 6940. [Google Scholar] [CrossRef]
| n | % | ||
|---|---|---|---|
| Disease Stage | |||
| 0 | 6 | 20 | |
| I | 15 | 50 | |
| II | 9 | 30 | |
| III | - | - | |
| Menopausal Status | |||
| Postmenopausal | 18 | 64.3 | |
| Surgery Type | |||
| Mastectomy | 3 | 10.0 | |
| Quadrantectomy | 26 | 87.7 | |
| Lumpectomy | 1 | 3.3 | |
| Treatment in Addition to Surgery | |||
| Only radiation | 2 | 6.7 | |
| Only chemotherapy | 13 | 43.3 | |
| Radiation and chemotherapy | 4 | 13.3 | |
| None | 11 | 36.7 | |
| Current Endocrine Therapy | |||
| None | 6 | 20.0 | |
| Tamoxifen | 8 | 26.7 | |
| Aromatase inhibitor | 16 | 53.3 | |
| T0 | T1 | Statistics | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p-Value | ES | %Δ | |
| Weight (kg) | 67.1 ± 11.6 | 66.3 ± 10.9 | 0.091 | 0.33 | −1.2% |
| BMI (kg/m2) | 26.0 ± 5.0 | 25.5 ± 4.7 | 0.035 | 0.41 | −1.7% |
| Waist circumference (cm) | 84.4 ± 12.1 | 84.6 ± 10.7 | 0.842 | 0.04 | +0.2% |
| Fat mass (%) | 31.1 ± 6.3 | 30.7 ± 5.9 | 0.408 | 0.16 | −1.3% |
| VO2max (mL·min−1·kg−1) | 30.5 ± 5.8 | 33.4 ± 6.8 | <0.001 | 0.91 | +9.6% |
| PAL (MET-min/week) | 647 ± 547 | 1043 ± 564 | <0.001 | 1.03 | +61.2% |
| Adherence to Mediterranean diet (Mediet Score DianaWeB) | 6.9 ± 2.3 | 8.8 ± 2.2 | <0.001 | 1.07 | +28.0% |
| T0 | T1 | Statistics | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p-Value | ES | %Δ | |
| Echocardiography | |||||
| Ejection Fraction (%) | 60.8 ± 4.4 | 62.6 ± 4.1 | 0.550 | 0.12 | +3.1% |
| e’ (cm/s) | 11.6 ± 3.3 | 12.0 ± 3.8 | 0.459 | 0.15 | +3.4% |
| LVEDV/BSA | 47.6 ± 8.7 | 48.5 ± 8.9 | 0.015 | 0.52 | +1.8% |
| LVESV/BSA | 18.4 ± 3.5 | 21.1 ± 11.9 | 0.119 | 0.32 | +14.6% |
| LAESV/BSA | 31.7 ± 7.8 | 31.0 ± 9.2 | 0.350 | 0.19 | −2.0% |
| GLS (%) | −20.1 ± 2.4 | −20.2 ± 2.3 | 0.569 | 0.12 | +0.6% |
| 24 h-Holter monitoring | |||||
| Mean HR (bpm) | 76.6 ± 7.8 | 73.7 ± 8.3 | 0.003 | 0.66 | −3.8% |
| Supraventricular extrasystole (%) | 0.04 ± 0.1 | 0.08 ± 0.28 | 0.380 | 0.18 | +136.9% |
| Ventricular extrasystole (%) | 0.01 ± 0.03 | 0.02 ± 0.07 | 0.450 | 0.15 | +115.4% |
| pNN50 (%) | 5.44 ± 5.49 | 8.03 ± 10.26 | 0.358 | 0.19 | +47.7% |
| ASDNN/5 min (ms) | 50.6 ± 14.4 | 55.3 ± 16.7 | 0.032 | 0.47 | +9.2% |
| RMSSD | 25.12 ± 9.92 | 26.64 ± 11.65 | 0.570 | 0.11 | +6.0% |
| VLF (ms2) | 1598 ± 967 | 1881 ± 963 | 0.118 | 0.32 | +17.7% |
| LF (ms2) | 589 ± 391 | 732 ± 542 | 0.014 | 0.53 | +24.3% |
| HF (ms2) | 157 ± 128 | 225 ± 241 | 0.197 | 0.27 | +43.1% |
| Total power (ms2) | 2627 ± 1393 | 3034 ± 1669 | 0.035 | 0.42 | +15.5% |
| T0 | T1 | Statistics | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p-Value | ES | %Δ | |
| Glycemia (mg/dL) | 100.8 ± 11.4 | 91.7 ± 11.0 | <0.001 | 1.15 | −9.1% |
| Insulin (microU/mL) | 7.92 ± 4.68 | 6.49 ± 3.94 | 0.018 | 0.47 | −18.1% |
| HOMA Index | 2.07 ± 1.54 | 1.53 ± 1.11 | 0.005 | 0.57 | −26.1% |
| Triglycerides (mg/dL) | 102.8 ± 43.7 | 93.3 ± 43.7 | 0.091 | 0.32 | −9.3% |
| HDL (mg/dL) | 62.3 ± 15.9 | 60.8 ± 13.5 | 0.242 | 0.22 | −2.5% |
| LDL (mg/dL) | 137.7 ± 29.9 | 126.1 ± 28.3 | <0.001 | 0.77 | −8.4% |
| Total cholesterol (mg/dL) | 217.7 ± 39.3 | 208.5 ± 37.3 | 0.029 | 0.43 | −4.3% |
| Progesterone (ng/mL) | 0.52 ± 0.40 | 0.50 ± 0.21 | 0.750 | 0.06 | −4.0% |
| Testosterone (ng/mL) | 0.34 ± 0.27 | 0.24 ± 0.20 | 0.003 | 0.60 | −28.9% |
| hs-CRP (mg/L) | 2.18 ± 2.14 | 1.75 ± 1.74 | 0.027 | 0.43 | −19.9% |
| hs-Troponin (ng/L) | 3.07 ± 1.14 | 2.73 ± 2.72 | 0.479 | 0.13 | −11.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Natalucci, V.; Marini, C.F.; Flori, M.; Pietropaolo, F.; Lucertini, F.; Annibalini, G.; Vallorani, L.; Sisti, D.; Saltarelli, R.; Villarini, A.; et al. Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. J. Clin. Med. 2021, 10, 2678. https://doi.org/10.3390/jcm10122678
Natalucci V, Marini CF, Flori M, Pietropaolo F, Lucertini F, Annibalini G, Vallorani L, Sisti D, Saltarelli R, Villarini A, et al. Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. Journal of Clinical Medicine. 2021; 10(12):2678. https://doi.org/10.3390/jcm10122678
Chicago/Turabian StyleNatalucci, Valentina, Carlo Ferri Marini, Marco Flori, Francesca Pietropaolo, Francesco Lucertini, Giosuè Annibalini, Luciana Vallorani, Davide Sisti, Roberta Saltarelli, Anna Villarini, and et al. 2021. "Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown" Journal of Clinical Medicine 10, no. 12: 2678. https://doi.org/10.3390/jcm10122678
APA StyleNatalucci, V., Marini, C. F., Flori, M., Pietropaolo, F., Lucertini, F., Annibalini, G., Vallorani, L., Sisti, D., Saltarelli, R., Villarini, A., Monaldi, S., Barocci, S., Catalano, V., Rocchi, M. B. L., Benelli, P., Stocchi, V., Barbieri, E., & Emili, R. (2021). Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. Journal of Clinical Medicine, 10(12), 2678. https://doi.org/10.3390/jcm10122678








