Old and New Challenges in Uveitis Associated with Behçet’s Disease
Abstract
1. Introduction
2. Methodology and Literature Search
3. Epidemiology of Uveitis Associated with Behçet’s Disease
4. Prognosis of Behçet’s Disease Uveitis over Time
5. Diagnosis of Uveitis Associated with Behçet’s Disease
5.1. Diagnosis of Systemic Behçet’s Disease
5.2. Diagnosis of Uveitis Associated with Behçet’s Disease
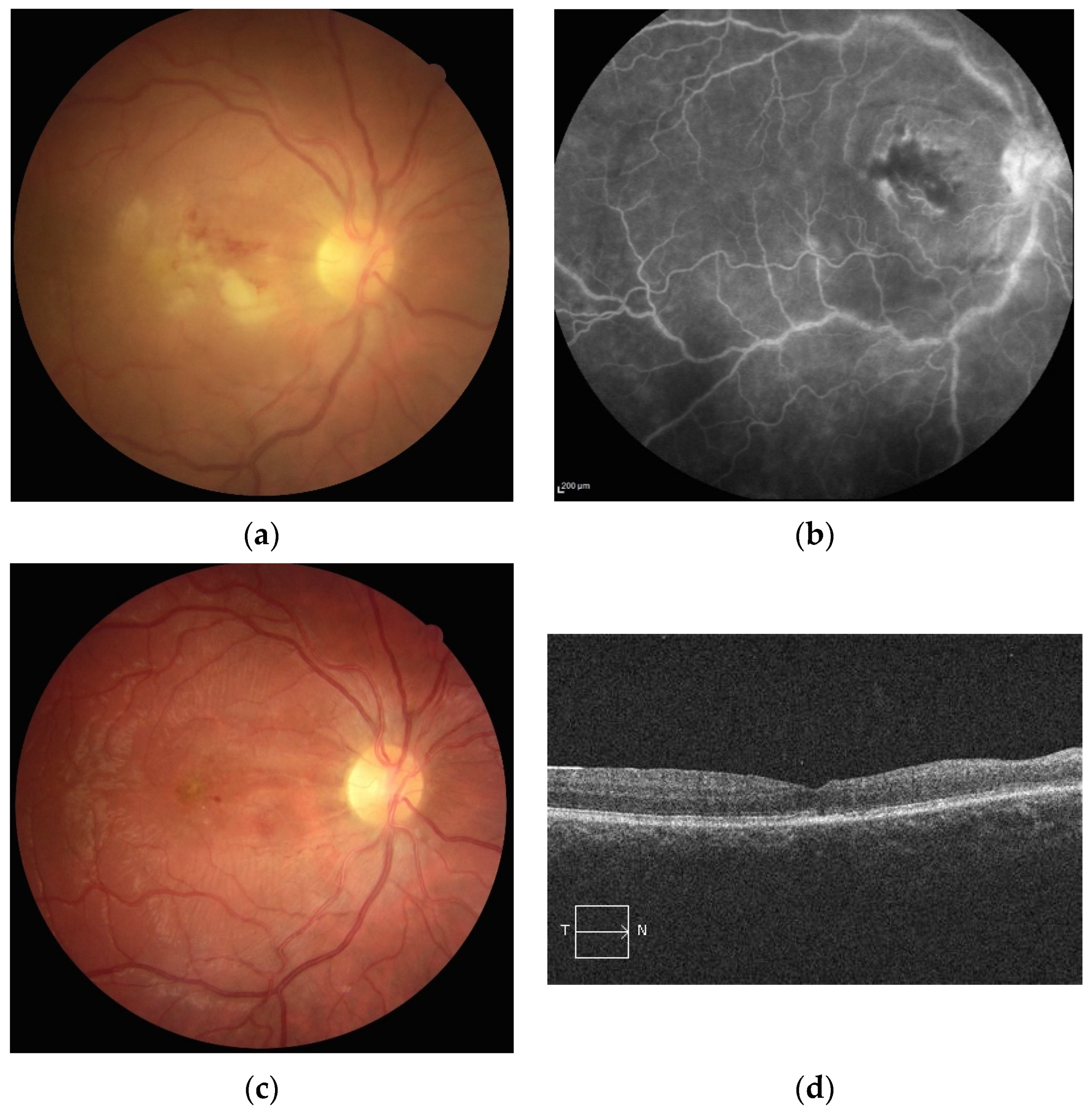
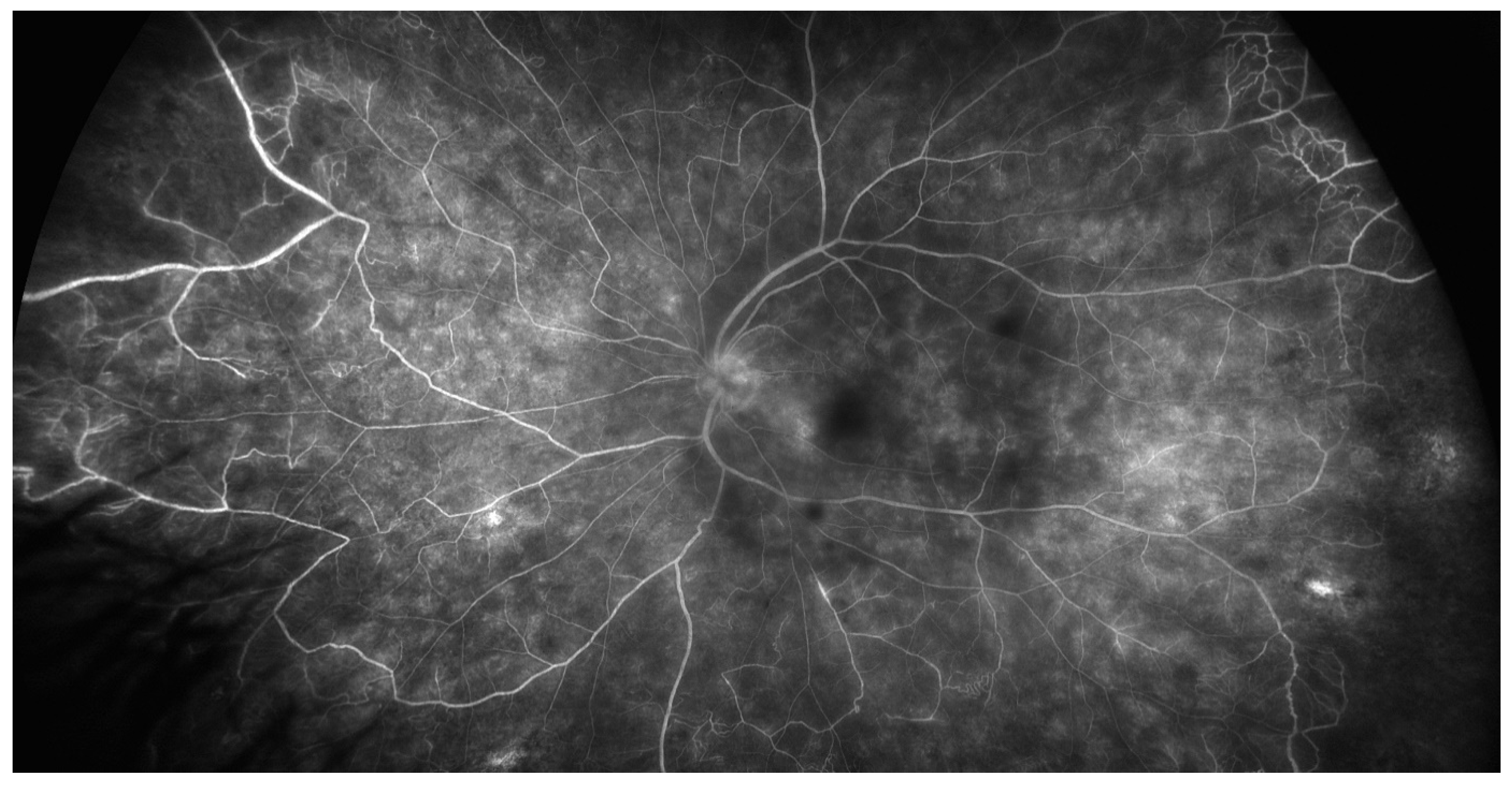
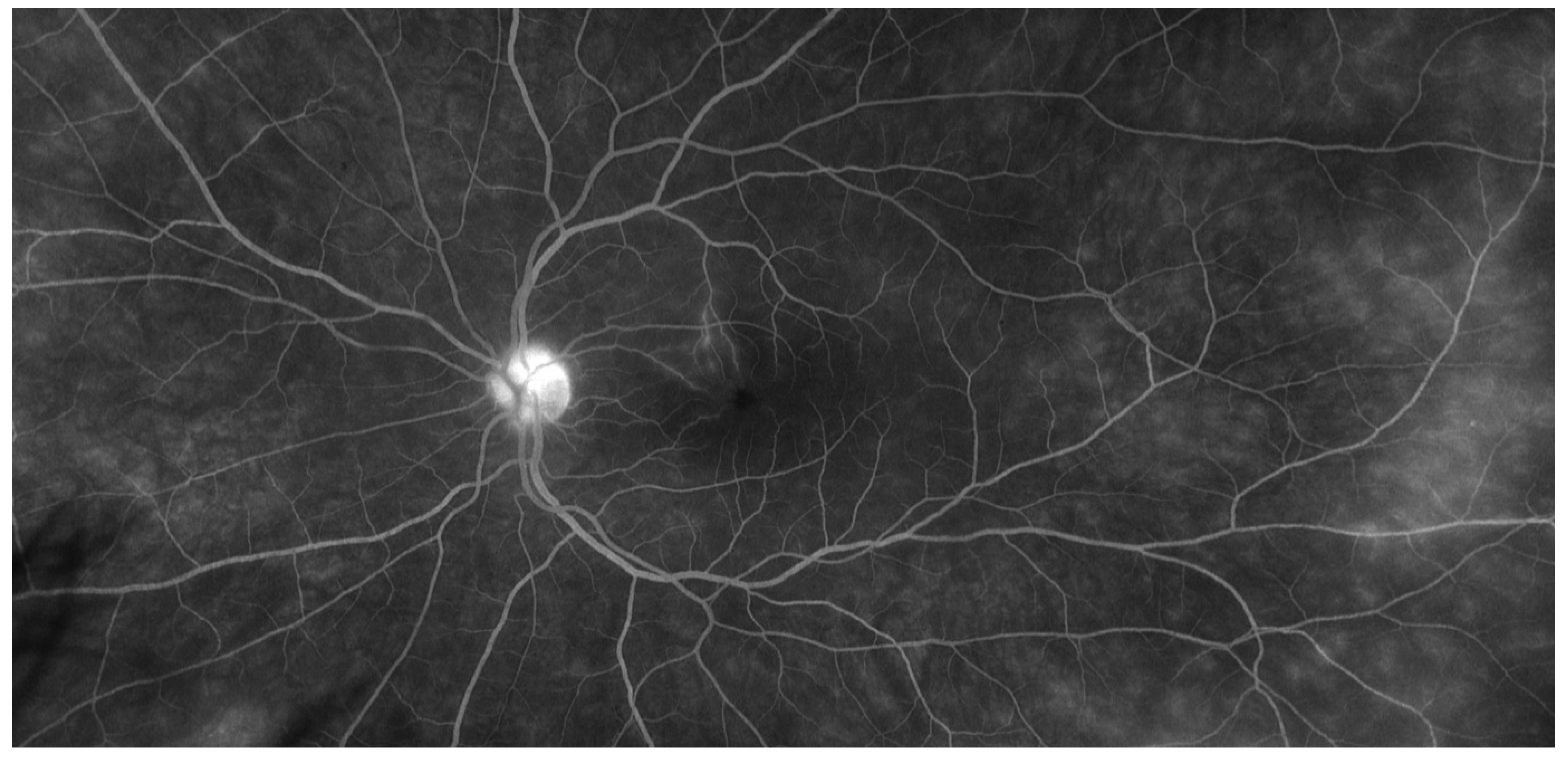
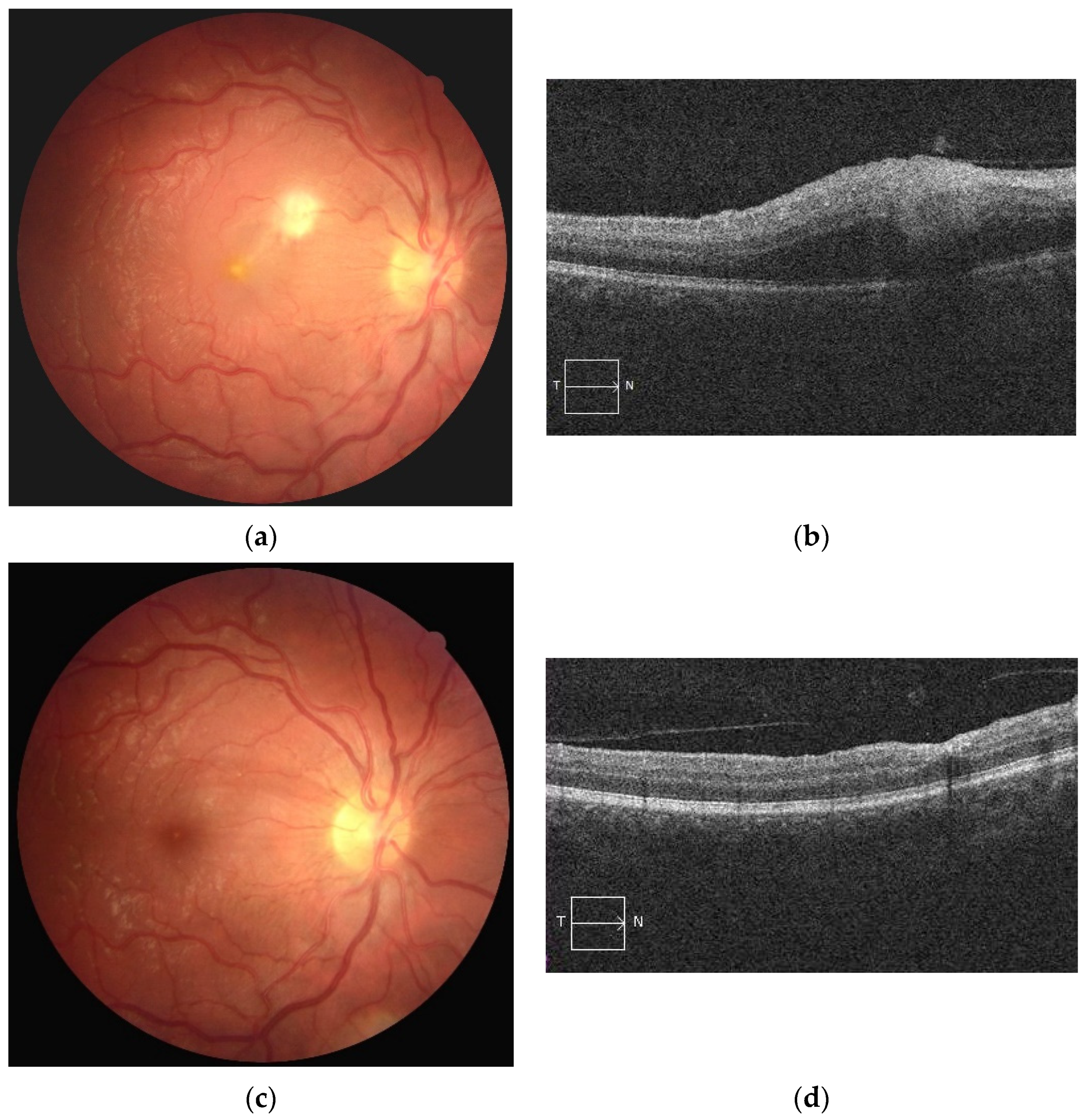
5.2.1. Clinical Characteristics and Investigations
5.2.2. Strategy for Definite and Earlier Diagnosis of Behçet’s Disease Uveitis
6. Treatment Modalities and Perspectives
6.1. Treatment Aims
6.2. Conventional Immunosuppressants
6.3. Interferons
6.4. Anti-TNFα Agents
6.5. Peri or Intraocular Treatment
6.6. Retinal Laser Photocoagulation
6.7. BD Uveitis Management Recommendations
6.8. Biologics beyond Anti-TNFα Agents
6.8.1. Anti-Interleukin-6 Agents
6.8.2. Anti-Interleukin-1 Agents
6.8.3. Anti-Interleukin-17 Agents
6.8.4. Anti-Interleukin-12/23 Agents
6.8.5. Other Biologics
6.8.6. Targeted Synthetic Disease-Modifying Antirheumatic Drugs
Anti-Janus Kinase
Apremilast
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Evereklioglu, C. Current concepts in the etiology and treatment of Behcet disease. Surv. Ophthalmol. 2005, 50, 297–350. [Google Scholar] [CrossRef]
- Wechsler, B.; Du-Boutin, L.T. Interferons and Behcet’s disease. Rev. Med. Interne 2002, 23, 495s–499s. [Google Scholar] [CrossRef]
- Cassoux, N.; Fardeau, C.; Lehoang, P. Ocular manifestations of Behcet’s disease. Ann. Med. Interne 1999, 150, 529–534. [Google Scholar]
- Sakane, T.; Takeno, M.; Suzuki, N.; Inaba, G. Behçet’s disease. N. Engl. J. Med. 1999, 341, 1284–1291. [Google Scholar] [CrossRef]
- Mahr, A.; Maldini, C. Epidemiology of Behçet’s disease. Rev. Med. Interne 2014, 35, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, B.; Du-Boutin, L.T.; Amoura, Z. Behcet’s disease. Rev. Prat. 2005, 55, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Kone-Paut, I.; Barete, S.; Bodaghi, B.; Deiva, K.; Desbois, A.C.; Galeotti, C.; Gaudric, J.; Kaplanski, G.; Mahr, A.; Noel, N.; et al. French recommendations for the management of Behçet’s disease. Orphanet J. Rare Dis. 2021, 16, 352. [Google Scholar] [CrossRef] [PubMed]
- Koné-Paut, I. Behçet’s disease in children, an overview. Pediatr. Rheumatol. Online J. 2016, 14, 10. [Google Scholar] [CrossRef]
- Mamo, J.G. The rate of visual loss in Behçet’s disease. Arch. Ophthalmol. 1970, 84, 451–452. [Google Scholar] [CrossRef] [PubMed]
- Tugal-Tutkun, I.; Onal, S.; Altan-Yaycioglu, R.; Huseyin Altunbas, H.; Urgancioglu, M. Uveitis in Behçet disease: An analysis of 880 patients. Am. J. Ophthalmol. 2004, 138, 373–380. [Google Scholar] [CrossRef]
- Cingu, A.K.; Onal, S.; Urgancioglu, M.; Tugal-Tutkun, I. Comparison of presenting features and three-year disease course in Turkish patients with Behçet uveitis who presented in the early 1990s and the early 2000s. Ocul. Immunol. Inflamm. 2012, 20, 423–428. [Google Scholar] [CrossRef]
- Desbois, A.C.; Terrada, C.; Cacoub, P.; Bodaghi, B.; Saadoun, D. Ocular manifestations in Behçet’s disease. Rev. Med. Interne 2018, 39, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Hatemi, G.; Christensen, R.; Bang, D.; Bodaghi, B.; Celik, A.F.; Fortune, F.; Gaudric, J.; Gul, A.; Kötter, I.; Leccese, P.; et al. 2018 update of the EULAR recommendations for the management of Behçet’s syndrome. Ann. Rheum. Dis. 2018, 77, 808–818. [Google Scholar] [CrossRef]
- Alpsoy, E.; Donmez, L.; Bacanli, A.; Apaydin, C.; Butun, B. Review of the chronology of clinical manifestations in 60 patients with Behçet’s disease. Dermatology 2003, 207, 354–356. [Google Scholar] [CrossRef]
- Criteria for diagnosis of Behcet’s disease. International Study Group for Behcet’s Disease. Lancet 1990, 335, 1078–1080. [Google Scholar]
- Lee, S. Diagnostic criteria of Behçet’s disease: Problems and suggestions. Yonsei Med. J. 1997, 38, 365–369. [Google Scholar] [CrossRef]
- The International Criteria for Behçet’s Disease (ICBD): A collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 338–347. [CrossRef]
- Khairallah, M.; Accorinti, M.; Muccioli, C.; Kahloun, R.; Kempen, J.H. Epidemiology of Behçet disease. Ocul. Immunol. Inflamm. 2012, 20, 324–335. [Google Scholar] [CrossRef] [PubMed]
- Tugal-Tutkun, I.; Gupta, V.; Cunningham, E.T. Differential diagnosis of Behçet Uveitis. Ocul. Immunol. Inflamm. 2013, 21, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Oray, M.; Onal, S.; Bayraktar, S.; Izgi, B.; Tugal-Tutkun, I. Nonglaucomatous localized retinal nerve fiber layer defects in Behçet uveitis. Am. J. Ophthalmol. 2015, 159, 475–481.e471. [Google Scholar] [CrossRef] [PubMed]
- Keino, H.; Okada, A.A.; Watanabe, T.; Taki, W. Long-term efficacy of infliximab on background vascular leakage in patients with Behçet’s disease. Eye 2014, 28, 1100–1106. [Google Scholar] [CrossRef]
- Tugal-Tutkun, I.; Ozdal, P.C.; Oray, M.; Onal, S. Review for Diagnostics of the Year: Multimodal Imaging in Behçet Uveitis. Ocul. Immunol. Inflamm. 2017, 25, 7–19. [Google Scholar] [CrossRef]
- Ideguchi, H.; Suda, A.; Takeno, M.; Ueda, A.; Ohno, S.; Ishigatsubo, Y. Behçet disease: Evolution of clinical manifestations. Medicine 2011, 90, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Mishima, S.; Masuda, K.; Izawa, Y.; Mochizuki, M.; Namba, K. The eighth Frederick H. Verhoeff Lecture. presented by saiichi mishima, MD Behcet’s disease in Japan: Ophthalmologic aspects. Trans. Am. Ophthalmol. Soc. 1979, 77, 225–279. [Google Scholar] [PubMed]
- Deuter, C.M.; Kotter, I.; Wallace, G.R.; Murray, P.I.; Stubiger, N.; Zierhut, M. Behcet’s disease: Ocular effects and treatment. Prog. Retin. Eye Res. 2008, 27, 111–136. [Google Scholar] [CrossRef]
- Tugal-Tutkun, I.; Onal, S.; Stanford, M.; Akman, M.; Twisk, J.W.R.; Boers, M.; Oray, M.; Özdal, P.; Kadayifcilar, S.; Amer, R.; et al. An Algorithm for the Diagnosis of Behçet Disease Uveitis in Adults. Ocul. Immunol. Inflamm. 2020, 1–10. [Google Scholar] [CrossRef]
- Kido, A.; Uji, A.; Morooka, S.; Kuroda, Y.; Arichika, S.; Akagi, T.; Tsujikawa, A. Outer Plexiform Layer Elevations as a Marker for Prior Ocular Attacks in Patients With Behcet’s Disease. Investig. Ophtalmol. Vis. Sci. 2018, 59, 2828–2832. [Google Scholar] [CrossRef] [PubMed]
- Shirahama, S.; Kaburaki, T.; Nakahara, H.; Tanaka, R.; Komae, K.; Fujino, Y.; Kawashima, H.; Aihara, M. Association between subfoveal choroidal thickness and leakage site on fluorescein angiography in Behçet’s uveitis. Sci. Rep. 2019, 9, 8612. [Google Scholar] [CrossRef] [PubMed]
- Onal, S.; Uludag, G.; Oray, M.; Mengi, E.; Herbort, C.P.; Akman, M.; Metin, M.M.; Koc Akbay, A.; Tugal-Tutkun, I. Quantitative analysis of structural alterations in the choroid of patients with active Behçet Uveitis. Retina 2018, 38, 828–840. [Google Scholar] [CrossRef]
- Accorinti, M.; Gilardi, M.; De Geronimo, D.; Iannetti, L.; Giannini, D.; Parravano, M. Optical Coherence Tomography Angiography Findings in Active and Inactive Ocular Behçet Disease. Ocul. Immunol. Inflamm. 2020, 28, 589–600. [Google Scholar] [CrossRef]
- Khairallah, M.; Abroug, N.; Khochtali, S.; Mahmoud, A.; Jelliti, B.; Coscas, G.; Lupidi, M.; Kahloun, R.; Ben Yahia, S. Optical coherence tomography angiography in patients with Behçet Uveitis. Retina 2017, 37, 1678–1691. [Google Scholar] [CrossRef] [PubMed]
- Somkijrungroj, T.; Vongkulsiri, S.; Kongwattananon, W.; Chotcomwongse, P.; Luangpitakchumpol, S.; Jaisuekul, K. Assessment of Vascular Change Using Swept-Source Optical Coherence Tomography Angiography: A New Theory Explains Central Visual Loss in Behcet’s Disease. J. Ophtalmol. 2017, 2017, 2180723. [Google Scholar] [CrossRef] [PubMed]
- Abucham-Neto, J.Z.; Torricelli, A.A.M.; Lui, A.C.F.; Guimarães, S.N.; Nascimento, H.; Regatieri, C.V. Comparison between optical coherence tomography angiography and fluorescein angiography findings in retinal vasculitis. Int. J. Retin. Vitr. 2018, 4, 15. [Google Scholar] [CrossRef]
- Raafat, K.A.; Allam, R.; Medhat, B.M. optical coherence tomography angiography findings in patients with nonocular Behçet disease. Retina 2019, 39, 1607–1612. [Google Scholar] [CrossRef]
- Smid, L.M.; Vermeer, K.A.; Missotten, T.; van Laar, J.A.M.; van Velthoven, M.E.J. Parafoveal Microvascular Alterations in Ocular and Non-Ocular Behçet’s Disease Evaluated With Optical Coherence Tomography Angiography. Investig. Ophtalmol. Vis. Sci. 2021, 62, 8. [Google Scholar] [CrossRef] [PubMed]
- Çömez, A.; Beyoğlu, A.; Karaküçük, Y. Quantitative analysis of retinal microcirculation in optical coherence tomography angiography in cases with Behçet’s disease without ocular involvement. Int. Ophthalmol. 2019, 39, 2213–2221. [Google Scholar] [CrossRef]
- Pei, M.; Zhao, C.; Gao, F.; Qu, Y.; Liang, A.; Xiao, J.; Zhang, M. Analysis of Parafoveal Microvascular Abnormalities in Behcet’s Uveitis Using Projection-Resolved Optical Coherence Tomographic Angiography. Ocul. Immunol. Inflamm. 2019, 1–6. [Google Scholar] [CrossRef]
- Karalezli, A.; Kaderli, S.T.; Sul, S.; Pektas, S.D. Preclinical ocular features in patients with Behçet’s disease detected by optical coherence tomography angiography. Eye 2020, 1–8. [Google Scholar] [CrossRef]
- Koca, S.; Onan, D.; Kalaycı, D.; Allı, N. Comparison of Optical Coherence Tomography Angiography Findings in Patients with Behçet’s Disease and Healthy Controls. Ocul. Immunol. Inflamm. 2020, 28, 806–813. [Google Scholar] [CrossRef]
- Leder, H.A.; Campbell, J.P.; Sepah, Y.J.; Gan, T.; Dunn, J.P.; Hatef, E.; Cho, B.; Ibrahim, M.; Bittencourt, M.; Channa, R.; et al. Ultra-wide-field retinal imaging in the management of non-infectious retinal vasculitis. J. Ophtalmic Inflamm. Infect. 2013, 3, 30. [Google Scholar] [CrossRef]
- Cunningham, E.T., Jr.; Munk, M.R.; Kiss, S.; Zierhut, M. Ultra-Wide-Field Imaging in Uveitis. Ocul. Immunol. Inflamm. 2019, 27, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Mesquida, M.; Llorenç, V.; Fontenla, J.R.; Navarro, M.J.; Adán, A. Use of ultra-wide-field retinal imaging in the management of active Behçet retinal vasculitis. Retina 2014, 34, 2121–2127. [Google Scholar] [CrossRef] [PubMed]
- Tugal-Tutkun, I.; Cingü, K.; Kir, N.; Yeniad, B.; Urgancioglu, M.; Gül, A. Use of laser flare-cell photometry to quantify intraocular inflammation in patients with Behçet uveitis. Graefe Arch. Clin. Exp. Ophtalmol. 2008, 246, 1169–1177. [Google Scholar] [CrossRef] [PubMed]
- Zierhut, M.; Abu El-Asrar, A.M.; Bodaghi, B.; Tugal-Tutkun, I. Therapy of ocular Behçet disease. Ocul. Immunol. Inflamm. 2014, 22, 64–76. [Google Scholar] [CrossRef]
- Touhami, S.; Diwo, E.; Sève, P.; Trad, S.; Bielefeld, P.; Sène, D.; Abad, S.; Brézin, A.; Quartier, P.; Koné Paut, I.; et al. Expert opinion on the use of biological therapy in non-infectious uveitis. Expert Opin. Biol. Ther. 2019, 19, 477–490. [Google Scholar] [CrossRef] [PubMed]
- Yazici, H.; Pazarli, H.; Barnes, C.G.; Tuzun, Y.; Ozyazgan, Y.; Silman, A.; Serdaroglu, S.; Oguz, V.; Yurdakul, S.; Lovatt, G.E.; et al. A controlled trial of azathioprine in Behcet’s syndrome. N. Engl. J. Med. 1990, 322, 281–285. [Google Scholar] [CrossRef]
- Masuda, K.; Nakajima, A.; Urayama, A.; Nakae, K.; Kogure, M.; Inaba, G. Double-masked trial of cyclosporin versus colchicine and long-term open study of cyclosporin in Behcet’s disease. Lancet 1989, 1, 1093–1096. [Google Scholar] [CrossRef]
- BenEzra, D.; Cohen, E.; Chajek, T.; Friedman, G.; Pizanti, S.; de Courten, C.; Harris, W. Evaluation of conventional therapy versus cyclosporine A in Behcet’s syndrome. Transpl. Proc. 1988, 20, 136–143. [Google Scholar]
- Ozyazgan, Y.; Yurdakul, S.; Yazici, H.; Tuzun, B.; Iscimen, A.; Tuzun, Y.; Aktunc, T.; Pazarli, H.; Hamuryudan, V.; Muftuoglu, A. Low dose cyclosporin A versus pulsed cyclophosphamide in Behcet’s syndrome: A single masked trial. Br. J. Ophthalmol. 1992, 76, 241–243. [Google Scholar] [CrossRef]
- Nussenblatt, R.B.; Palestine, A.G.; Chan, C.C.; Mochizuki, M.; Yancey, K. Effectiveness of cyclosporin therapy for Behcet’s disease. Arthritis Rheum. 1985, 28, 671–679. [Google Scholar] [CrossRef]
- Sullu, Y.; Oge, I.; Erkan, D.; Ariturk, N.; Mohajeri, F. Cyclosporin-A therapy in severe uveitis of Behcet’s disease. Acta Ophthalmol. Scand. 1998, 76, 96–99. [Google Scholar] [CrossRef]
- Hesselink, D.A.; Baarsma, G.S.; Kuijpers, R.W.; van Hagen, P.M. Experience with cyclosporine in endogenous uveitis posterior. Transpl. Proc. 2004, 36, 372s–377s. [Google Scholar] [CrossRef]
- Davatchi, F.; Shams, H.; Shahram, F.; Nadji, A.; Chams-Davatchi, C.; Sadeghi Abdollahi, B.; Faezi, T.; Akhlaghi, M.; Ashofteh, F. Methotrexate in ocular manifestations of Behcet’s disease: A longitudinal study up to 15 years. Int. J. Rheum. Dis. 2013, 16, 568–577. [Google Scholar] [CrossRef]
- Tugal-Tutkun, I.; Çakar Özdal, P. Behçet’s disease uveitis: Is there a need for new emerging drugs? Expert Opin. Emerg. Drugs 2020, 25, 531–547. [Google Scholar] [CrossRef]
- Feron, E.J.; Rothova, A.; van Hagen, P.M.; Baarsma, G.S.; Suttorp-Schulten, M.S. Interferon-alpha 2b for refractory ocular Behcet’s disease. Lancet 1994, 343, 1428. [Google Scholar] [CrossRef]
- Kotter, I.; Eckstein, A.K.; Stubiger, N.; Zierhut, M. Treatment of ocular symptoms of Behcet’s disease with interferon alpha 2a: A pilot study. Br. J. Ophthalmol. 1998, 82, 488–494. [Google Scholar] [CrossRef]
- Pivetti-Pezzi, P.; Accorinti, M.; Pirraglia, M.P.; Priori, R.; Valesini, G. Interferon alpha for ocular Behcet’s disease. Acta Ophthalmol. Scand. 1997, 75, 720–722. [Google Scholar] [CrossRef] [PubMed]
- Bodaghi, B.; Gendron, G.; Wechsler, B.; Terrada, C.; Cassoux, N.; Thi Huong, D.L.; Lemaitre, C.; Fradeau, C.; Lehoang, P.; Piette, J.C. Efficacy of interferon alpha in the treatment of refractory and sight threatening uveitis: A retrospective monocentric study of 45 patients. Br. J. Ophthalmol. 2007, 91, 335–339. [Google Scholar] [CrossRef]
- Guillaume-Czitrom, S.; Berger, C.; Pajot, C.; Bodaghi, B.; Wechsler, B.; Kone-Paut, I. Efficacy and safety of interferon-α in the treatment of corticodependent uveitis of paediatric Behcet’s disease. Rheumatology 2007, 46, 1570–1573. [Google Scholar] [CrossRef] [PubMed]
- Kotter, I.; Gunaydin, I.; Zierhut, M.; Stubiger, N. The use of interferon alpha in Behcet disease: Review of the literature. Semin. Arthritis Rheum. 2004, 33, 320–335. [Google Scholar] [CrossRef]
- Tugal-Tutkun, I.; Guney-Tefekli, E.; Urgancioglu, M. Results of interferon-alfa therapy in patients with Behcet uveitis. Graefe Arch. Clin. Exp. Ophtalmol. 2006, 244, 1692–1695. [Google Scholar] [CrossRef]
- Wechsler, B.; Bodaghi, B.; Huong, D.L.; Fardeau, C.; Amoura, Z.; Cassoux, N.; Piette, J.C.; LeHoang, P. Efficacy of interferon alfa-2a in severe and refractory uveitis associated with Behcet’s disease. Ocul. Immunol. Inflamm. 2000, 8, 293–301. [Google Scholar] [CrossRef]
- Alpsoy, E.; Durusoy, C.; Yilmaz, E.; Ozgurel, Y.; Ermis, O.; Yazar, S.; Basaran, E. Interferon alfa-2a in the treatment of Behçet disease: A randomized placebo-controlled and double-blind study. Arch Dermatol 2002, 138, 467–471. [Google Scholar] [CrossRef]
- Onal, S.; Kazokoglu, H.; Koc, A.; Akman, M.; Bavbek, T.; Direskeneli, H.; Yavuz, S. Long-term efficacy and safety of low-dose and dose-escalating interferon alfa-2a therapy in refractory Behçet uveitis. Arch. Ophthalmol. 2011, 129, 288–294. [Google Scholar] [CrossRef]
- Gueudry, J.; Wechsler, B.; Terrada, C.; Gendron, G.; Cassoux, N.; Fardeau, C.; Lehoang, P.; Piette, J.C.; Bodaghi, B. Long-term efficacy and safety of low-dose interferon alpha2a therapy in severe uveitis associated with Behçet disease. Am. J. Ophthalmol. 2008, 146, 837–844.e831. [Google Scholar] [CrossRef]
- Diwo, E.; Gueudry, J.; Saadoun, D.; Weschler, B.; LeHoang, P.; Bodaghi, B. Long-term Efficacy of Interferon in Severe Uveitis Associated with Behçet Disease. Ocul. Immunol. Inflamm. 2017, 25, 76–84. [Google Scholar] [CrossRef]
- Kotter, I.; Zierhut, M.; Eckstein, A.K.; Vonthein, R.; Ness, T.; Gunaydin, I.; Grimbacher, B.; Blaschke, S.; Meyer-Riemann, W.; Peter, H.H.; et al. Human recombinant interferon alfa-2a for the treatment of Behcet’s disease with sight threatening posterior or panuveitis. Br. J. Ophthalmol. 2003, 87, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Deuter, C.M.; Zierhut, M.; Möhle, A.; Vonthein, R.; Stöbiger, N.; Kötter, I. Long-term remission after cessation of interferon-α treatment in patients with severe uveitis due to Behçet’s disease. Arthritis Rheum. 2010, 62, 2796–2805. [Google Scholar] [CrossRef] [PubMed]
- Lightman, S.; Taylor, S.R.; Bunce, C.; Longhurst, H.; Lynn, W.; Moots, R.; Stanford, M.; Tomkins-Netzer, O.; Yang, D.; Calder, V.L.; et al. Pegylated interferon-α-2b reduces corticosteroid requirement in patients with Behçet’s disease with upregulation of circulating regulatory T cells and reduction of Th17. Ann. Rheum. Dis. 2015, 74, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Celiker, H.; Kazokoglu, H.; Direskeneli, H. Long-Term Efficacy of Pegylated Interferon Alpha-2b in Behçet’s Uveitis: A Small Case Series. Ocul. Immunol. Inflamm. 2019, 27, 15–22. [Google Scholar] [CrossRef]
- Bielefeld, P.; Devilliers, H.; Deschasse, C.; Saadoun, D.; Sève, P.; Muselier, A.; Creuzot-Garcher, C.; Besancenot, J.F.; Bron, A.M. Potential of Pegylated Interferon Alpha-2a in Behçet Uveitis: A Report of Five Cases. Ocul. Immunol. Inflamm. 2016, 24, 599–602. [Google Scholar] [CrossRef]
- Kötter, I.; Günaydin, I.; Treusch, M.; Zierhut, M.; Kanz, L.; Stübiger, N. The use of interferon-alpha in Behçet’s disease—Review of the literature and possible mechanisms of action. Adv. Exp. Med. Biol. 2003, 528, 503–509. [Google Scholar] [CrossRef]
- Uke, P.; Gorodkin, R.; Beare, N. Biologic therapy for Behçet’s uveitis: A systematic review. Br. J. Ophthalmol. 2020, 104, 1045–1051. [Google Scholar] [CrossRef]
- Leclercq, M.; Langlois, V.; Girszyn, N.; Le Besnerais, M.; Benhamou, Y.; Levesque, H.; Muraine, M.; Gueudry, J. Comparison of conventional immunosuppressive drugs versus anti-TNF-α agents in non-infectious non-anterior uveitis. J. Autoimmun. 2020, 113, 102481. [Google Scholar] [CrossRef] [PubMed]
- Sfikakis, P.P.; Theodossiadis, P.G.; Katsiari, C.G.; Kaklamanis, P.; Markomichelakis, N.N. Effect of infliximab on sight-threatening panuveitis in Behcet’s disease. Lancet 2001, 358, 295–296. [Google Scholar] [CrossRef]
- Yamada, Y.; Sugita, S.; Tanaka, H.; Kamoi, K.; Kawaguchi, T.; Mochizuki, M. Comparison of infliximab versus ciclosporin during the initial 6-month treatment period in Behçet disease. Br. J. Ophthalmol. 2010, 94, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Arida, A.; Fragiadaki, K.; Giavri, E.; Sfikakis, P.P. Anti-TNF Agents for Behcet’s Disease: Analysis of Published Data on 369 Patients. Semin Arthritis Rheum. 2011, 41, 61–70. [Google Scholar] [CrossRef]
- Markomichelakis, N.; Delicha, E.; Masselos, S.; Fragiadaki, K.; Kaklamanis, P.; Sfikakis, P.P. A single infliximab infusion vs corticosteroids for acute panuveitis attacks in Behcet’s disease: A comparative 4-week study. Rheumatology 2011, 50, 593–597. [Google Scholar] [CrossRef]
- Ozguler, Y.; Leccese, P.; Christensen, R.; Esatoglu, S.N.; Bang, D.; Bodaghi, B.; Çelik, A.F.; Fortune, F.; Gaudric, J.; Gul, A.; et al. Management of major organ involvement of Behçet’s syndrome: A systematic review for update of the EULAR recommendations. Rheumatology 2018, 57, 2200–2212. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Llopis, M.; Garcia-Delpech, S.; Salom, D.; Udaondo, P.; Hernandez-Garfella, M.; Bosch-Morell, F.; Quijada, A.; Romero, F.J. Adalimumab therapy for refractory uveitis: A pilot study. J. Ocul. Pharmacol. Ther. 2008, 24, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Callejas-Rubio, J.L.; Sanchez-Cano, D.; Serrano, J.L.; Ortego-Centeno, N. Adalimumab therapy for refractory uveitis: A pilot study. J. Ocul. Pharmacol. Ther. 2008, 24, 613–614; author reply 614. [Google Scholar] [CrossRef]
- Van Laar, J.A.; Missotten, T.; van Daele, P.L.; Jamnitski, A.; Baarsma, G.S.; van Hagen, P.M. Adalimumab: A new modality for Behcet’s disease? Ann. Rheum. Dis. 2007, 66, 565–566. [Google Scholar] [CrossRef]
- Bawazeer, A.; Raffa, L.H.; Nizamuddin, S.H. Clinical experience with adalimumab in the treatment of ocular Behcet disease. Ocul. Immunol. Inflamm. 2010, 18, 226–232. [Google Scholar] [CrossRef]
- Kunimi, K.; Usui, Y.; Asakage, M.; Maehara, C.; Tsubota, K.; Mitsuhashi, R.; Umazume, A.; Kezuka, T.; Sakai, J.I.; Goto, H. Anti-TNF-α Therapy for Refractory Uveitis Associated with Behçet’s Syndrome and Sarcoidosis: A Single Center Study of 131 Patients. Ocul. Immunol. Inflamm. 2020, 1–8. [Google Scholar] [CrossRef]
- Silvestri, E.; Bitossi, A.; Bettiol, A.; Emmi, G.; Urban, M.L.; Mattioli, I.; Di Scala, G.; Bacherini, D.; Lopalco, G.; Venerito, V.; et al. Adalimumab effectively controls both anterior and posterior noninfectious uveitis associated with systemic inflammatory diseases: Focus on Behçet’s syndrome. Inflammopharmacology 2020, 28, 711–718. [Google Scholar] [CrossRef]
- Jaffe, G.J.; Dick, A.D.; Brézin, A.P.; Nguyen, Q.D.; Thorne, J.E.; Kestelyn, P.; Barisani-Asenbauer, T.; Franco, P.; Heiligenhaus, A.; Scales, D.; et al. Adalimumab in Patients with Active Noninfectious Uveitis. N. Engl. J. Med. 2016, 375, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Merrill, P.T.; Jaffe, G.J.; Dick, A.D.; Kurup, S.K.; Sheppard, J.; Schlaen, A.; Pavesio, C.; Cimino, L.; Van Calster, J.; et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): A multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet 2016, 388, 1183–1192. [Google Scholar] [CrossRef]
- Hu, Y.; Huang, Z.; Yang, S.; Chen, X.; Su, W.; Liang, D. Effectiveness and Safety of Anti-Tumor Necrosis Factor-Alpha Agents Treatment in Behcets’ Disease-Associated Uveitis: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2020, 11, 941. [Google Scholar] [CrossRef] [PubMed]
- Vallet, H.; Seve, P.; Biard, L.; Baptiste Fraison, J.; Bielefeld, P.; Perard, L.; Bienvenu, B.; Abad, S.; Rigolet, A.; Deroux, A.; et al. Infliximab Versus Adalimumab in the Treatment of Refractory Inflammatory Uveitis: A Multicenter Study From the French Uveitis Network. Arthritis Rheumatol. 2016, 68, 1522–1530. [Google Scholar] [CrossRef] [PubMed]
- Vallet, H.; Riviere, S.; Sanna, A.; Deroux, A.; Moulis, G.; Addimanda, O.; Salvarani, C.; Lambert, M.; Bielefeld, P.; Seve, P.; et al. Efficacy of anti-TNF alpha in severe and/or refractory Behçet’s disease: Multicenter study of 124 patients. J. Autoimmun. 2015, 62, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Atienza-Mateo, B.; Martín-Varillas, J.L.; Calvo-Río, V.; Demetrio-Pablo, R.; Beltrán, E.; Sánchez-Bursón, J.; Mesquida, M.; Adan, A.; Hernández, M.V.; Hernández-Garfella, M.; et al. Comparative Study of Infliximab Versus Adalimumab in Refractory Uveitis due to Behçet’s Disease: National Multicenter Study of 177 Cases. Arthritis Rheumatol. 2019, 71, 2081–2089. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, C.; Sota, J.; Vitale, A.; Rigante, D.; Emmi, G.; Vannozzi, L.; Bacherini, D.; Lopalco, G.; Guerriero, S.; Gentileschi, S.; et al. Cumulative retention rate of adalimumab in patients with Behçet’s disease-related uveitis: A four-year follow-up study. Br. J. Ophthalmol. 2018, 102, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, C.; Sota, J.; Vitale, A.; Emmi, G.; Vannozzi, L.; Bacherini, D.; Lopalco, G.; Guerriero, S.; Venerito, V.; Orlando, I.; et al. Ten-Year Retention Rate of Infliximab in Patients with Behçet’s Disease-Related Uveitis. Ocul. Immunol. Inflamm. 2019, 27, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Horiguchi, N.; Kamoi, K.; Horie, S.; Iwasaki, Y.; Kurozumi-Karube, H.; Takase, H.; Ohno-Matsui, K. A 10-year follow-up of infliximab monotherapy for refractory uveitis in Behçet’s syndrome. Sci. Rep. 2020, 10, 22227. [Google Scholar] [CrossRef]
- Lee, J.; Koreishi, A.F.; Zumpf, K.B.; Minkus, C.L.; Goldstein, D.A. Success of Weekly Adalimumab in Refractory Ocular Inflammatory Disease. Ophthalmology 2020, 127, 1431–1433. [Google Scholar] [CrossRef]
- Liberman, P.; Berkenstock, M.K.; Burkholder, B.M.; Chaon, B.C.; Thorne, J.E. Escalation to Weekly Adalimumab for the Treatment of Ocular Inflammation. Ocul. Immunol. Inflamm. 2020, 1–5. [Google Scholar] [CrossRef]
- Gueudry, J.; LeHoang, P.; Bodaghi, B. Anti-tumor necrosis factor-α agents in noninfectious uveitis. Dev. Ophtalmol. 2012, 51, 63–78. [Google Scholar] [CrossRef]
- Miserocchi, E.; Modorati, G.; Pontikaki, I.; Meroni, P.L.; Gerloni, V. Long-term treatment with golimumab for severe uveitis. Ocul. Immunol. Inflamm. 2014, 22, 90–95. [Google Scholar] [CrossRef] [PubMed]
- William, M.; Faez, S.; Papaliodis, G.N.; Lobo, A.M. Golimumab for the treatment of refractory juvenile idiopathic arthritis-associated uveitis. J. Ophthalmic Inflamm. Infect. 2012, 2, 231–233. [Google Scholar] [CrossRef]
- Mesquida, M.; Victoria Hernandez, M.; Llorenc, V.; Pelegrin, L.; Espinosa, G.; Dick, A.D.; Adan, A. Behcet disease-associated uveitis successfully treated with golimumab. Ocul. Immunol. Inflamm. 2013, 21, 160–162. [Google Scholar] [CrossRef]
- Miserocchi, E.; Modorati, G.; Pontikaki, I.; Meroni, P.; Gerloni, V. Golimumab treatment for complicated uveitis. Clin. Exp. Rheumatol. 2013, 31, 320–321. [Google Scholar]
- Cordero-Coma, M.; Salom, D.; Diaz-Llopis, M.; Lopez-Prats, M.J.; Calleja, S. Golimumab for uveitis. Ophthalmology 2011, 118, 1892.e3–1892.e4. [Google Scholar] [CrossRef]
- Keane, J.; Gershon, S.; Wise, R.P.; Mirabile-Levens, E.; Kasznica, J.; Schwieterman, W.D.; Siegel, J.N.; Braun, M.M. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N. Engl. J. Med. 2001, 345, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Simsek, I.; Erdem, H.; Pay, S.; Sobaci, G.; Dinc, A. Optic neuritis occurring with anti-tumour necrosis factor alpha therapy. Ann. Rheum. Dis. 2007, 66, 1255–1258. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, E.T.; Zierhut, M. TNF inhibitors for uveitis: Balancing efficacy and safety. Ocul. Immunol. Inflamm. 2010, 18, 421–423. [Google Scholar] [CrossRef]
- Stubgen, J.P. Tumor necrosis factor-alpha antagonists and neuropathy. Muscle Nerve 2008, 37, 281–292. [Google Scholar] [CrossRef]
- Solomon, A.J.; Spain, R.I.; Kruer, M.C.; Bourdette, D. Inflammatory neurological disease in patients treated with tumor necrosis factor alpha inhibitors. Mult. Scler. J. 2011, 17, 1472–1487. [Google Scholar] [CrossRef]
- Bensouda-Grimaldi, L.; Mulleman, D.; Valat, J.P.; Autret-Leca, E. Adalimumab-associated multiple sclerosis. J. Rheumatol. 2007, 34, 239–240; discussion 240. [Google Scholar] [PubMed]
- Ding, T.; Ledingham, J.; Luqmani, R.; Westlake, S.; Hyrich, K.; Lunt, M.; Kiely, P.; Bukhari, M.; Abernethy, R.; Bosworth, A.; et al. BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies. Rheumatology 2010, 49, 2217–2219. [Google Scholar] [CrossRef]
- Pereira, R.; Lago, P.; Faria, R.; Torres, T. Safety of Anti-TNF Therapies in Immune-Mediated Inflammatory Diseases: Focus on Infections and Malignancy. Drug Dev. Res. 2015, 76, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Atzeni, F.; Gianturco, L.; Talotta, R.; Varisco, V.; Ditto, M.C.; Turiel, M.; Sarzi-Puttini, P. Investigating the potential side effects of anti-TNF therapy for rheumatoid arthritis: Cause for concern? Immunotherapy 2015, 7, 353–361. [Google Scholar] [CrossRef]
- Pascual-Salcedo, D.; Plasencia, C.; Ramiro, S.; Nuno, L.; Bonilla, G.; Nagore, D.; Ruiz Del Agua, A.; Martinez, A.; Aarden, L.; Martin-Mola, E.; et al. Influence of immunogenicity on the efficacy of long-term treatment with infliximab in rheumatoid arthritis. Rheumatology 2011, 50, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, C.; Alió, J.L. Local (topical and intraocular) therapy for ocular Adamantiades-Behçet’s disease. Curr. Opin. Ophtalmol. 2015, 26, 546–552. [Google Scholar] [CrossRef]
- Markomichelakis, N.; Delicha, E.; Masselos, S.; Sfikakis, P.P. Intravitreal infliximab for sight-threatening relapsing uveitis in Behçet disease: A pilot study in 15 patients. Am. J. Ophthalmol. 2012, 154, 534–541.e531. [Google Scholar] [CrossRef] [PubMed]
- Hamza, M.M.; Macky, T.A.; Sidky, M.K.; Ragab, G.; Soliman, M.M. Intravitreal infliximab in refractory uveitis in Behcet’s Disease: A Safety and Efficacy Clinical Study. Retina 2016, 36, 2399–2408. [Google Scholar] [CrossRef]
- Refaat, M.; Abdullatif, A.M.; Hamza, M.M.; Macky, T.A.; El-Agha, M.H.; Ragab, G.; Soliman, M.M. Monthly Intravitreal Infliximab in Behçet’s Disease Active Posterior Uveitis: A Long-Term Safety Study. Retina 2020. [Google Scholar] [CrossRef]
- Androudi, S.; Tsironi, E.; Kalogeropoulos, C.; Theodoridou, A.; Brazitikos, P. Intravitreal adalimumab for refractory uveitis-related macular edema. Ophthalmology 2010, 117, 1612–1616. [Google Scholar] [CrossRef] [PubMed]
- Hamam, R.N.; Barikian, A.W.; Antonios, R.S.; Abdulaal, M.R.; Alameddine, R.M.; El Mollayess, G.; Mansour, A.M. Intravitreal Adalimumab in Active Noninfectious Uveitis: A Pilot Study. Ocul. Immunol. Inflamm. 2016, 24, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Kheir, W.J.; Mehanna, C.J.; Abdul Fattah, M.; Al Ghadban, S.; El Sabban, M.; Mansour, A.M.; Hamam, R.N. Intravitreal Adalimumab for the Control of Breakthrough Intraocular Inflammation. Ocul. Immunol. Inflamm. 2018, 26, 1206–1211. [Google Scholar] [CrossRef]
- Manzano, R.P.; Peyman, G.A.; Carvounis, P.E.; Damico, F.M.; Aguiar, R.G.; Ioshimoto, G.L.; Ventura, D.F.; Cursino, S.T.; Takahashi, W. Toxicity of high-dose intravitreal adalimumab (humira) in the rabbit. J. Ocul. Pharmacol. Ther. 2011, 27, 327–331. [Google Scholar] [CrossRef]
- Manzano, R.P.; Peyman, G.A.; Carvounis, P.E.; Kivilcim, M.; Khan, P.; Chevez-Barrios, P.; Takahashi, W. Ocular toxicity of intravitreous adalimumab (Humira) in the rabbit. Graefes Arch. Clin. Exp. Ophthalmol. 2008, 246, 907–911. [Google Scholar] [CrossRef]
- Tsilimbaris, M.; Diakonis, V.F.; Naoumidi, I.; Charisis, S.; Kritikos, I.; Chatzithanasis, G.; Papadaki, T.; Plainis, S. Evaluation of potential retinal toxicity of adalimumab (Humira). Graefes Arch. Clin. Exp. Ophthalmol. 2009, 247, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.H.; Lee, C.S.; Lee, S.C. Efficacy and safety of intravitreal bevacizumab compared with intravitreal and posterior sub-tenon triamcinolone acetonide for treatment of uveitic cystoid macular edema. Retina 2011, 31, 111–118. [Google Scholar] [CrossRef]
- Hatemi, G.; Silman, A.; Bang, D.; Bodaghi, B.; Chamberlain, A.M.; Gul, A.; Houman, M.H.; Kötter, I.; Olivieri, I.; Salvarani, C.; et al. EULAR recommendations for the management of Behçet disease. Ann. Rheum. Dis. 2008, 67, 1656–1662. [Google Scholar] [CrossRef]
- Protocole National de Diagnostic et de Soins sur les Uvéites Chroniques Non Infectieuses de L’enfant et de L’adulte. Available online: https://www.has-sante.fr/upload/docs/application/pdf/2020-05/pnds_ucni.pdf (accessed on 28 February 2021).
- Martín-Varillas, J.L.; Calvo-Río, V.; Beltrán, E.; Sánchez-Bursón, J.; Mesquida, M.; Adán, A.; Hernandez, M.V.; Garfella, M.H.; Pascual, E.V.; Martínez-Costa, L.; et al. Successful Optimization of Adalimumab Therapy in Refractory Uveitis Due to Behçet’s Disease. Ophthalmology 2018, 125, 1444–1451. [Google Scholar] [CrossRef]
- Sepah, Y.J.; Sadiq, M.A.; Chu, D.S.; Dacey, M.; Gallemore, R.; Dayani, P.; Hanout, M.; Hassan, M.; Afridi, R.; Agarwal, A.; et al. Primary (Month-6) Outcomes of the STOP-Uveitis Study: Evaluating the Safety, Tolerability, and Efficacy of Tocilizumab in Patients With Noninfectious Uveitis. Am. J. Ophthalmol. 2017, 183, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Eser Ozturk, H.; Oray, M.; Tugal-Tutkun, I. Tocilizumab for the Treatment of Behçet Uveitis that Failed Interferon Alpha and Anti-Tumor Necrosis Factor-Alpha Therapy. Ocul. Immunol. Inflamm. 2018, 26, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Atienza-Mateo, B.; Calvo-Río, V.; Beltrán, E.; Martínez-Costa, L.; Valls-Pascual, E.; Hernández-Garfella, M.; Atanes, A.; Cordero-Coma, M.; Miquel Nolla, J.; Carrasco-Cubero, C.; et al. Anti-interleukin 6 receptor tocilizumab in refractory uveitis associated with Behçet’s disease: Multicentre retrospective study. Rheumatology 2018, 57, 856–864. [Google Scholar] [CrossRef]
- Akiyama, M.; Kaneko, Y.; Takeuchi, T. Effectiveness of tocilizumab in Behcet’s disease: A systematic literature review. Semin. Arthritis Rheum. 2020, 50, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Vegas-Revenga, N.; Calvo-Río, V.; Mesquida, M.; Adán, A.; Hernández, M.V.; Beltrán, E.; Valls Pascual, E.; Díaz-Valle, D.; Díaz-Cordovés, G.; Hernandez-Garfella, M.; et al. Anti-IL6-Receptor Tocilizumab in Refractory and Noninfectious Uveitic Cystoid Macular Edema: Multicenter Study of 25 Patients. Am. J. Ophthalmol. 2019, 200, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Choy, E.H.; De Benedetti, F.; Takeuchi, T.; Hashizume, M.; John, M.R.; Kishimoto, T. Translating IL-6 biology into effective treatments. Nat. Rev. Rheumatol. 2020, 16, 335–345. [Google Scholar] [CrossRef]
- Burmester, G.R.; Choy, E.; Kivitz, A.; Ogata, A.; Bao, M.; Nomura, A.; Lacey, S.; Pei, J.; Reiss, W.; Pethoe-Schramm, A.; et al. Low immunogenicity of tocilizumab in patients with rheumatoid arthritis. Ann. Rheum. Dis. 2017, 76, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Tugal-Tutkun, I.; Pavesio, C.; De Cordoue, A.; Bernard-Poenaru, O.; Gül, A. Use of Gevokizumab in Patients with Behçet’s Disease Uveitis: An International, Randomized, Double-Masked, Placebo-Controlled Study and Open-Label Extension Study. Ocul. Immunol. Inflamm. 2018, 26, 1023–1033. [Google Scholar] [CrossRef] [PubMed]
- Gül, A.; Tugal-Tutkun, I.; Dinarello, C.A.; Reznikov, L.; Esen, B.A.; Mirza, A.; Scannon, P.; Solinger, A. Interleukin-1β-regulating antibody XOMA 052 (gevokizumab) in the treatment of acute exacerbations of resistant uveitis of Behcet’s disease: An open-label pilot study. Ann. Rheum. Dis. 2012, 71, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Tugal-Tutkun, I.M.; Kadayifcilar, S.M.; Khairallah, M.M.; Lee, S.C.M.P.; Ozdal, P.; Özyazgan, Y.; Song, J.H.M.; Yu, H.G.M.P.; Lehner, V.P.; de Cordoue, A.M.; et al. Safety and Efficacy of Gevokizumab in Patients with Behçet’s Disease Uveitis: Results of an Exploratory Phase 2 Study. Ocul. Immunol. Inflamm. 2017, 25, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Cantarini, L.; Vitale, A.; Scalini, P.; Dinarello, C.A.; Rigante, D.; Franceschini, R.; Simonini, G.; Borsari, G.; Caso, F.; Lucherini, O.M.; et al. Anakinra treatment in drug-resistant Behcet’s disease: A case series. Clin. Rheumatol. 2015, 34, 1293–1301. [Google Scholar] [CrossRef]
- Emmi, G.; Talarico, R.; Lopalco, G.; Cimaz, R.; Cantini, F.; Viapiana, O.; Olivieri, I.; Goldoni, M.; Vitale, A.; Silvestri, E.; et al. Efficacy and safety profile of anti-interleukin-1 treatment in Behçet’s disease: A multicenter retrospective study. Clin. Rheumatol. 2016, 35, 1281–1286. [Google Scholar] [CrossRef]
- Fabiani, C.; Vitale, A.; Emmi, G.; Lopalco, G.; Vannozzi, L.; Guerriero, S.; Gentileschi, S.; Bacherini, D.; Franceschini, R.; Frediani, B.; et al. Interleukin (IL)-1 inhibition with anakinra and canakinumab in Behçet’s disease-related uveitis: A multicenter retrospective observational study. Clin. Rheumatol. 2017, 36, 191–197. [Google Scholar] [CrossRef]
- Sota, J.; Rigante, D.; Lopalco, G.; Frediani, B.; Franceschini, R.; Galeazzi, M.; Iannone, F.; Tosi, G.M.; Fabiani, C.; Cantarini, L. Biological therapies for the treatment of Behçet’s disease-related uveitis beyond TNF-alpha blockade: A narrative review. Rheumatol. Int. 2018, 38, 25–35. [Google Scholar] [CrossRef]
- Dick, A.D.; Tugal-Tutkun, I.; Foster, S.; Zierhut, M.; Melissa Liew, S.H.; Bezlyak, V.; Androudi, S. Secukinumab in the treatment of noninfectious uveitis: Results of three randomized, controlled clinical trials. Ophthalmology 2013, 120, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Hueber, W.; Patel, D.D.; Dryja, T.; Wright, A.M.; Koroleva, I.; Bruin, G.; Antoni, C.; Draelos, Z.; Gold, M.H.; Psoriasis Study, G.; et al. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci. Transl. Med. 2010, 2, 52ra72. [Google Scholar] [CrossRef]
- Letko, E.; Yeh, S.; Foster, C.S.; Pleyer, U.; Brigell, M.; Grosskreutz, C.L.; Group, A.A.S. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology 2015, 122, 939–948. [Google Scholar] [CrossRef]
- Fagni, F.; Bettiol, A.; Talarico, R.; Lopalco, G.; Silvestri, E.; Urban, M.L.; Russo, P.A.J.; Di Scala, G.; Emmi, G.; Prisco, D. Long-term effectiveness and safety of secukinumab for treatment of refractory mucosal and articular Behçet’s phenotype: A multicentre study. Ann. Rheum. Dis. 2020, 79, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Pepple, K.L.; Lin, P. Targeting Interleukin-23 in the Treatment of Noninfectious Uveitis. Ophthalmology 2018, 125, 1977–1983. [Google Scholar] [CrossRef] [PubMed]
- Guillo, L.; D’Amico, F.; Danese, S.; Peyrin-Biroulet, L. Ustekinumab for extra-intestinal manifestations of inflammatory bowel disease: A systematic literature review. J. Crohn Colitis 2020. [Google Scholar] [CrossRef]
- Chateau, T.; Angioi, K.; Peyrin-Biroulet, L. Two Cases of Successful Ustekinumab Treatment for Non-infectious Uveitis Associated With Crohn’s Disease. J. Crohn Colitis 2020, 14, 571. [Google Scholar] [CrossRef] [PubMed]
- Mugheddu, C.; Atzori, L.; Del Piano, M.; Lappi, A.; Pau, M.; Murgia, S.; Zucca, I.; Rongioletti, F. Successful ustekinumab treatment of noninfectious uveitis and concomitant severe psoriatic arthritis and plaque psoriasis. Dermatol. Ther. 2017, 30, e12527. [Google Scholar] [CrossRef] [PubMed]
- Mirouse, A.; Barete, S.; Desbois, A.C.; Comarmond, C.; Sène, D.; Domont, F.; Bodaghi, B.; Ferfar, Y.; Cacoub, P.; Saadoun, D. Long-Term Outcome of Ustekinumab Therapy for Behçet’s Disease. Arthritis Rheumatol. 2019, 71, 1727–1732. [Google Scholar] [CrossRef]
- Mirouse, A.; Barete, S.; Monfort, J.B.; Resche-Rigon, M.; Bouyer, A.S.; Comarmond, C.; Sène, D.; Domont, F.; Ferfar, Y.; Cacoub, P.; et al. Ustekinumab for Behçet’s disease. J. Autoimmun. 2017, 82, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Davatchi, F.; Shams, H.; Rezaipoor, M.; Sadeghi-Abdollahi, B.; Shahram, F.; Nadji, A.; Chams-Davatchi, C.; Akhlaghi, M.; Faezi, T.; Naderi, N. Rituximab in intractable ocular lesions of Behcet’s disease; randomized single-blind control study (pilot study). Int. J. Rheum. Dis. 2010, 13, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, C.M.; Hale, G.; Waldman, H.; Jayne, D.R. Remission induction in Behçet’s disease following lymphocyte depletion by the anti-CD52 antibody CAMPATH 1-H. Rheumatology 2003, 42, 1539–1544. [Google Scholar] [CrossRef]
- Mohammad, A.J.; Smith, R.M.; Chow, Y.W.; Chaudhry, A.N.; Jayne, D.R.W. Alemtuzumab as Remission Induction Therapy in Behçet Disease: A 20-year Experience. J. Rheumatol. 2015, 42, 1906–1913. [Google Scholar] [CrossRef] [PubMed]
- Maciel, M.L.; Novello, M.; Neves, F.S. Short-term efficacy of abatacept in the treatment of refractory ocular and cutaneous Behçet’s disease. Rheumatol. Adv. Pract. 2017, 1, rkx004. [Google Scholar] [CrossRef]
- Buggage, R.R.; Levy-Clarke, G.; Sen, H.N.; Ursea, R.; Srivastava, S.K.; Suhler, E.B.; Altemare, C.; Velez, G.; Ragheb, J.; Chan, C.C.; et al. A double-masked, randomized study to investigate the safety and efficacy of daclizumab to treat the ocular complications related to Behçet’s disease. Ocul. Immunol. Inflamm. 2007, 15, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Daclizumab withdrawn from the market worldwide. Drug Ther. Bull. 2018, 56, 38. [CrossRef]
- Pleyer, U.; Algharably, E.A.; Feist, E.; Kreutz, R. Small molecules as therapy for uveitis: A selected perspective of new and developing agents. Expert Opin. Pharmacother. 2017, 18, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hou, Y.; Sun, L.; Li, C.; Li, L.; Zhao, Y.; Zeng, X.; Zhang, F.; Zheng, W. A pilot study of tofacitinib for refractory Behçet’s syndrome. Ann. Rheum. Dis. 2020, 79, 1517–1520. [Google Scholar] [CrossRef] [PubMed]
- Paley, M.A.; Karacal, H.; Rao, P.K.; Margolis, T.P.; Miner, J.J. Tofacitinib for refractory uveitis and scleritis. Am. J. Ophtalmol. Case Rep. 2019, 13, 53–55. [Google Scholar] [CrossRef]
- Bauermann, P.; Heiligenhaus, A.; Heinz, C. Effect of Janus Kinase Inhibitor Treatment on Anterior Uveitis and Associated Macular Edema in an Adult Patient with Juvenile Idiopathic Arthritis. Ocul. Immunol. Inflamm. 2019, 27, 1232–1234. [Google Scholar] [CrossRef]
- Miserocchi, E.; Giuffrè, C.; Cornalba, M.; Pontikaki, I.; Cimaz, R. JAK inhibitors in refractory juvenile idiopathic arthritis-associated uveitis. Clin. Rheumatol. 2020, 39, 847–851. [Google Scholar] [CrossRef]
- Hatemi, G.; Melikoglu, M.; Tunc, R.; Korkmaz, C.; Turgut Ozturk, B.; Mat, C.; Merkel, P.A.; Calamia, K.T.; Liu, Z.; Pineda, L.; et al. Apremilast for Behçet’s syndrome—A phase 2, placebo-controlled study. N. Engl. J. Med. 2015, 372, 1510–1518. [Google Scholar] [CrossRef] [PubMed]
- Hatemi, G.; Mahr, A.; Ishigatsubo, Y.; Song, Y.W.; Takeno, M.; Kim, D.; Melikoğlu, M.; Cheng, S.; McCue, S.; Paris, M.; et al. Trial of Apremilast for Oral Ulcers in Behçet’s Syndrome. N. Engl. J. Med. 2019, 381, 1918–1928. [Google Scholar] [CrossRef] [PubMed]
- Vieira, M.; Buffier, S.; Vautier, M.; Le Joncour, A.; Jamilloux, Y.; Gerfaud-Valentin, M.; Bouillet, L.; Lazaro, E.; Barete, S.; Misery, L.; et al. Apremilast in Refractory Behçet’s Syndrome: A Multicenter Observational Study. Front. Immunol. 2020, 11, 626792. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gueudry, J.; Leclercq, M.; Saadoun, D.; Bodaghi, B. Old and New Challenges in Uveitis Associated with Behçet’s Disease. J. Clin. Med. 2021, 10, 2318. https://doi.org/10.3390/jcm10112318
Gueudry J, Leclercq M, Saadoun D, Bodaghi B. Old and New Challenges in Uveitis Associated with Behçet’s Disease. Journal of Clinical Medicine. 2021; 10(11):2318. https://doi.org/10.3390/jcm10112318
Chicago/Turabian StyleGueudry, Julie, Mathilde Leclercq, David Saadoun, and Bahram Bodaghi. 2021. "Old and New Challenges in Uveitis Associated with Behçet’s Disease" Journal of Clinical Medicine 10, no. 11: 2318. https://doi.org/10.3390/jcm10112318
APA StyleGueudry, J., Leclercq, M., Saadoun, D., & Bodaghi, B. (2021). Old and New Challenges in Uveitis Associated with Behçet’s Disease. Journal of Clinical Medicine, 10(11), 2318. https://doi.org/10.3390/jcm10112318





