Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
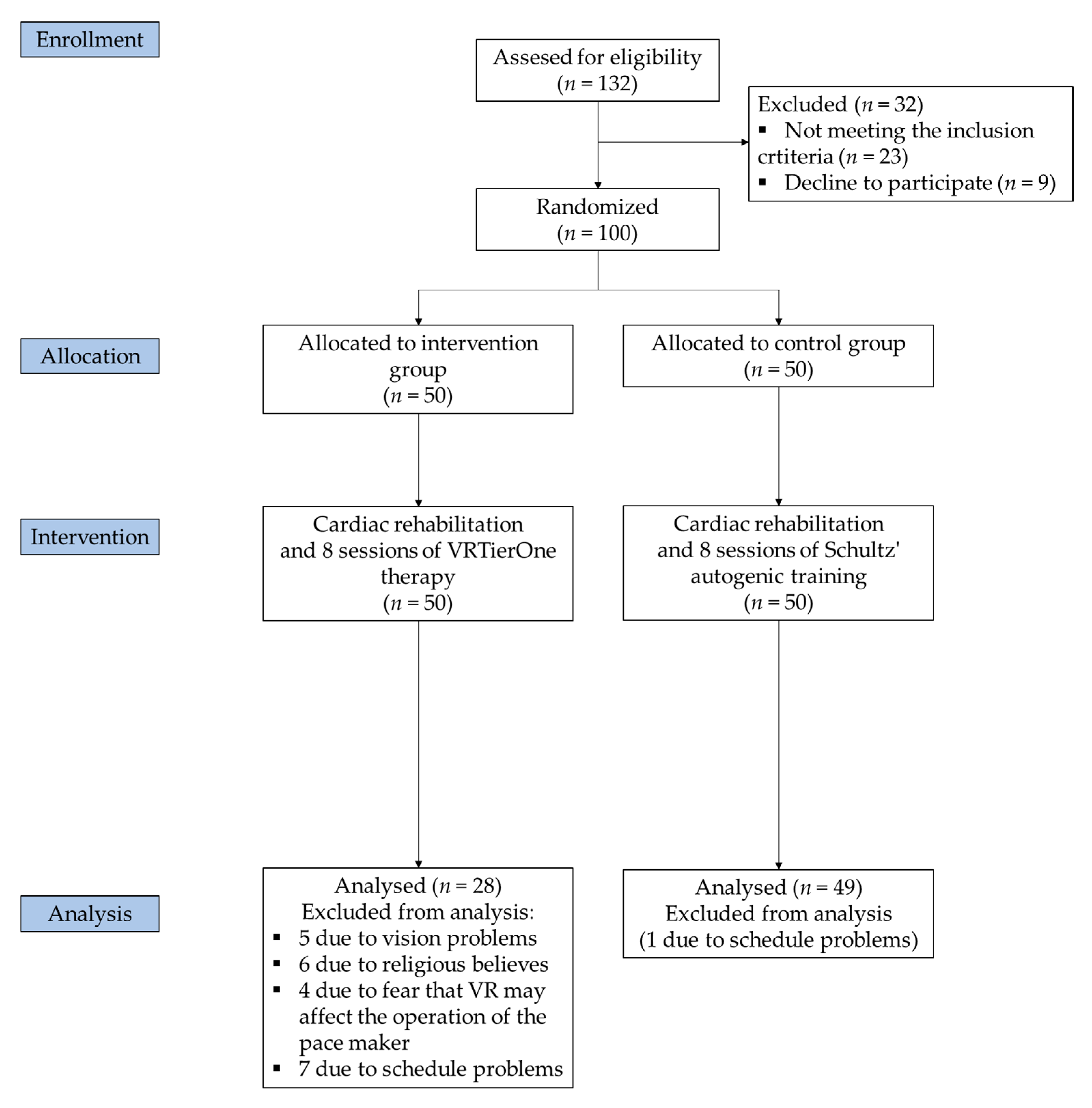
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Outcome Measures
2.5. Data Analysis
3. Results
3.1. Participants and Characteristics
3.2. Assessment of Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chowdhury, M.E.; Khandakar, A.; Alzoubi, K.; Mansoor, S.; Tahir, A.M.; Reaz, M.B.I.; Al-Emadi, N. Real-Time Smart-Digital Stethoscope System for Heart Diseases Monitoring. Sensors 2019, 19, 2781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raič, M. Depression and Heart Diseases: Leading Health Problems. Psychiatr. Danub. 2017, 29, 770–777. [Google Scholar] [PubMed]
- Rodwin, B.A.; Spruill, T.M.; Ladapo, J.A. Economics of Psychosocial Factors in Patients with Cardiovascular Disease. Prog. Cardiovasc. Dis. 2013, 55, 563–573. [Google Scholar] [CrossRef] [PubMed]
- May, H.T.; Horne, B.D.; Knight, S.; Knowlton, K.U.; Bair, T.L.; Lappé, D.L.; Le, V.T.; Muhlestein, J.B. The association of depression at any time to the risk of death following coronary artery disease diagnosis. Eur. Heart J. Qual. Care Clin. Outcomes 2017, 3, 296–302. [Google Scholar] [CrossRef] [Green Version]
- Lichtman, J.H.; Froelicher, E.S.; Blumenthal, J.A.; Carney, R.M.; Doering, L.V.; Frasure-Smith, N.; Freedland, K.E.; Jaffe, A.S.; Leifheit-Limson, E.C.; Sheps, D.S.; et al. Depression as a Risk Factor for Poor Prognosis Among Patients With Acute Coronary Syndrome: Systematic Review and Recommendations: A Scientific Statement from the American Heart Association. Circulation 2014, 129, 1350–1369. [Google Scholar] [CrossRef] [Green Version]
- Halaris, A. Comorbidity between depression and cardiovascular disease. Int. Angiol. 2009, 28, 92–99. [Google Scholar]
- Van Dijk, M.R.; Utens, E.M.W.J.; Dulfer, K.; A Al-Qezweny, M.N.; Van Geuns, R.-J.; Daemen, J.; Van Domburg, R.T. Depression and anxiety symptoms as predictors of mortality in PCI patients at 10 years of follow-up. Eur. J. Prev. Cardiol. 2016, 23, 552–558. [Google Scholar] [CrossRef]
- Pizzi, C.; Santarella, L.; Manfrini, O.; Chiavaroli, M.; Agushi, E.; Cordioli, E.; Costa, G.M.; Bugiardini, R. [Ischemic heart disease and depression: An underestimated clinical association]. G. Ital. Cardiol. 2013, 14, 526–537. [Google Scholar]
- Sokoreli, I.; De Vries, J.J.G.; Pauws, S.; Steyerberg, E.W. Depression and anxiety as predictors of mortality among heart failure patients: Systematic review and meta-analysis. Heart Fail. Rev. 2016, 21, 49–63. [Google Scholar] [CrossRef]
- Figueredo, V.M. The Time Has Come for Physicians to Take Notice: The Impact of Psychosocial Stressors on the Heart. Am. J. Med. 2009, 122, 704–712. [Google Scholar] [CrossRef] [Green Version]
- Mazurek, J.; Kiper, P.; Cieślik, B.; Rutkowski, S.; Mehlich, K.; Turolla, A.; Szczepańska-Gieracha, J. Virtual reality in medicine: A brief overview and future research directions. Hum. Mov. 2019, 20, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Decker, V.; Valenti, M.; Montoya, V.; Sikorskii, A.; Given, C.W.; Given, B.A. Maximizing New Technologies to Treat Depression. Issues Ment. Heath. Nurs. 2018, 40, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Park, M.J.; Kim, D.J.; Lee, U.; Na, E.J.; Jeon, H.J. A Literature Overview of Virtual Reality (VR) in Treatment of Psychiatric Disorders: Recent Advances and Limitations. Front. Psychiatry 2019, 10, 505. [Google Scholar] [CrossRef]
- Cieślik, B.; Mazurek, J.; Rutkowski, S.; Kiper, P.; Turolla, A.; Szczepańska-Gieracha, J. Virtual reality in psychiatric disorders: A systematic review of reviews. Complement. Ther. Med. 2020, 52, 102480. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska-Gieracha, J.; Cieślik, B.; Rutkowski, S.; Kiper, P.; Turolla, A. What can virtual reality offer to stroke patients? A narrative review of the literature. Neurorehabilitation 2020, 47, 109–120. [Google Scholar] [CrossRef]
- Silva, J.N.; Southworth, M.; Raptis, C.; Silva, J. Emerging Applications of Virtual Reality in Cardiovascular Medicine. JACC Basic Transl. Sci. 2018, 3, 420–430. [Google Scholar] [CrossRef]
- Rutkowski, S.; Kiper, P.; Cacciante, L.; Cieślik, B.; Mazurek, J.; Turolla, A.; Szczepańska-Gieracha, J. Use of virtual reality-based training in different fields of rehabilitation: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00121. [Google Scholar] [CrossRef]
- García-Bravo, S.; Cuesta-Gómez, A.; Campuzano-Ruiz, R.; López-Navas, M.J.; Domínguez-Paniagua, J.; Araújo-Narváez, A.; Barreñada-Copete, E.; García-Bravo, C.; Flórez-García, M.T.; Botas-Rodríguez, J.; et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil. Rehabil. 2021, 43, 448–457. [Google Scholar] [CrossRef]
- Bond, S.; Laddu, D.R.; Ozemek, C.; Lavie, C.J.; Arena, R. Exergaming and Virtual Reality for Health: Implications for Cardiac Rehabilitation. Curr. Probl. Cardiol. 2021, 46, 100472. [Google Scholar] [CrossRef]
- Vieira, Á.; Melo, C.; Machado, J.; Gabriel, J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: A randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2017, 13, 112–123. [Google Scholar] [CrossRef]
- Chuang, T.-Y.; Sung, W.-H.; Chang, H.-A.; Wang, R.-Y. Effect of a Virtual Reality–Enhanced Exercise Protocol After Coronary Artery Bypass Grafting. Phys. Ther. 2006, 86, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska-Gieracha, J.; Jóźwik, S.; Cieślik, B.; Mazurek, J.; Gajda, R. Immersive Virtual Reality Therapy As a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2021. [Google Scholar] [CrossRef]
- Hannan, A.L.; Hing, W.; Simas, V.; Climstein, M.; Coombes, J.S.; Jayasinghe, R.; Byrnes, J.; Furness, J. High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: A systematic review and meta-analysis. Open Access J. Sports Med. 2018, ume 9, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Rutkowski, S.; Szczegielniak, J.; Szczepańska-Gieracha, J. Evaluation of The Efficacy of Immersive Virtual Reality Therapy as a Method Supporting Pulmonary Rehabilitation: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 352. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska-Gieracha, J.; Cieślik, B.; Serweta, A.; Klajs, K. Virtual Therapeutic Garden: A Promising Method Supporting the Treatment of Depressive Symptoms in Late-Life: A Randomized Pilot Study. J. Clin. Med. 2021, 10, 1942. [Google Scholar] [CrossRef]
- Smarr, K.L.; Keefer, A.L. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionna. Arthritis Rheum. 2011, 63, S454–S466. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Plopa, M.; Makarowski, R. The Perception of Stress Questionnaire. Manual; Vizja Press and IT: Warsaw, Poland, 2010; ISBN 978-83-61086-79-6. [Google Scholar]
- McMahon, S.R.; Ades, P.A.; Thompson, P.D. The role of cardiac rehabilitation in patients with heart disease. Trends Cardiovasc. Med. 2017, 27, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska-Gieracha, J.; Morka, J.; Kowalska, J.; Kustrzycki, W.; Rymaszewska, J. The role of depressive and anxiety symptoms in the evaluation of cardiac rehabilitation efficacy after coronary artery bypass grafting surgery. Eur. J. Cardio-Thorac. Surg. 2012, 42, e108–e114. [Google Scholar] [CrossRef] [Green Version]
- Kustrzycki, W.; Rymaszewska, J.; Malcher, K.; Szczepanska-Gieracha, J.; Biecek, P. Risk factors of depressive and anxiety symptoms 8 years after coronary artery bypass grafting. Eur. J. Cardio-Thorac. Surg. 2011, 41, 302–306. [Google Scholar] [CrossRef] [Green Version]
- Tulloch, H.; Heenan, A.; Cupper, L.; Pelletier, R.; O’Farrell, P.; Pipe, A. Depression and Anxiety Screening and Triage Protocol for Cardiac Rehabilitation Programs. J. Cardiopulm. Rehabil. Prev. 2018, 38, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, J.A.; Sherwood, A.; Smith, P.J.; Watkins, L.; Mabe, S.; Kraus, W.E.; Ingle, K.; Miller, P.; Hinderliter, A. Enhancing Cardiac Rehabilitation with Stress Management Training. Circulation 2016, 133, 1341–1350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albus, C.; Herrmann-Lingen, C.; Jensen, K.; Hackbusch, M.; Münch, N.; Kuncewicz, C.; Grilli, M.; Schwaab, B.; Rauch, B.; German Society of Cardiovascular Prevention & Rehabilitation (DGPR). Additional effects of psychological interventions on subjective and objective outcomes compared with exercise-based cardiac rehabilitation alone in patients with cardiovascular disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2019, 26, 1035–1049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutkowski, S.; Rutkowska, A.; Jastrzębski, D.; Racheniuk, H.; Pawełczyk, W.; Szczegielniak, J. Effect of Virtual Reality-Based Rehabilitation on Physical Fitness in Patients with Chronic Obstructive Pulmonary Disease. J. Hum. Kinet. 2019, 69, 149–157. [Google Scholar] [CrossRef] [Green Version]
- Lindner, P.; Hamilton, W.; Miloff, A.; Carlbring, P. How to Treat Depression With Low-Intensity Virtual Reality Interventions: Perspectives on Translating Cognitive Behavioral Techniques Into the Virtual Reality Modality and How to Make Anti-Depressive Use of Virtual Reality–Unique Experiences. Front. Psychiatry 2019, 10, 792. [Google Scholar] [CrossRef] [Green Version]
- García-Bravo, S.; Cano-De-La-Cuerda, R.; Domínguez-Paniagua, J.; Campuzano-Ruiz, R.; Barreñada-Copete, E.; López-Navas, M.J.; Araujo-Narváez, A.; García-Bravo, C.; Florez-Garcia, M.; Botas-Rodríguez, J.; et al. Effects of Virtual Reality on Cardiac Rehabilitation Programs for Ischemic Heart Disease: A Randomized Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 8472. [Google Scholar] [CrossRef]
- Gerber, S.M.; Jeitziner, M.-M.; Wyss, P.; Chesham, A.; Urwyler, P.; Müri, R.M.; Jakob, S.M.; Nef, T. Visuo-acoustic stimulation that helps you to relax: A virtual reality setup for patients in the intensive care unit. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. Virtual Reality Exercise for Anxiety and Depression: A Preliminary Review of Current Research in an Emerging Field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, B.I.; Carnethon, M.R.; Matthews, K.A.; McIntyre, R.S.; Miller, G.E.; Raghuveer, G.; Stoney, C.M.; Wasiak, H.; McCrindle, B.W. Major Depressive Disorder and Bipolar Disorder Predispose Youth to Accelerated Atherosclerosis and Early Cardiovascular Disease. Circulation 2015, 132, 965–986. [Google Scholar] [CrossRef]
| Variable | Overall | VR-Enhanced Rehabilitation | Standard Rehabilitation | p Value * |
|---|---|---|---|---|
| N | 77 | 28 | 49 | - |
| Age, years (SD) | 64.70 (8.03) | 66.00 (9.73) | 63.96 (6.89) | 0.29 |
| n (%) of females | 42 (54.54) | 17 (60.71) | 25 (51.02) | 0.41 |
| Body mass, kg (SD) | 77.68 (14.49) | 75.50 (14.97) | 78.91 (14.97) | 0.32 |
| Height, cm (SD) | 165.75 (14.29) | 164.54 (8.62) | 166.45 (16.74) | 0.58 |
| BMI, kg/cm2 (SD) | 29.25 (13.70) | 27.79 (4.03) | 27.65 (3.98) | 0.49 |
| IHD, n (%) | 77 (100.00) | 28 (100.00) | 49 (100.00) | - |
| PCI/CABG | 37 (48.05) | 15 (53.57) | 22 (44.90) | 0.46 |
| Diabetes, n (%) Body weight | 22 (28.57) | 8 (28.57) | 14 (28.57) | 0.99 |
| Normal (BMI 18.5–24.9), n (%) | 19 (24.67) | 6 (21.43) | 13 (26.53) | 0.62 |
| Overweight (BMI 25–29.9), n (%) | 35 (45.45) | 14 (50.00) | 21 (42.86) | 0.55 |
| Obese (BMI > 30), n (%) | 23 (29.87) | 8 (28.57) | 15 (30.61) | 0.85 |
| Education | ||||
| Elementary and vocational, n (%) | 25 (32.47) | 9 (32.14) | 16 (32.65) | 0.96 |
| Secondary, n (%) | 21 (27.27) | 5 (17.88) | 16 (32.65) | 0.16 |
| Higher education, n (%) | 31 (40.30) | 14 (50.00) | 17 (34.69) | 0.19 |
| Marital status | ||||
| Married, n (%) | 48 (62.34) | 16 (57.14) | 32 (65.30) | 0.48 |
| Single/divorced, n (%) | 14 (18.18) | 8 (28.57) | 6 (12.25) | 0.07 |
| Widow, n (%) | 15 (19.48) | 4 (14.29) | 11 (22.45) | 0.38 |
| Outcome | VR-Enhanced Rehabilitation | Standard Rehabilitation | p Value * (Between Groups) |
|---|---|---|---|
| HADS-total | |||
| Before | 13.71 (7.40) | 13.57 (7.33) | |
| After | 11.86 (6.58) | 14.22 (7.11) | |
| Change | −1.86, −13.5% (−3.47 to −0.25) | 0.65, 4.8% (0.16 to 1.14) | <0.001 |
| p value | 0.02 | 0.01 | |
| HADS-A | |||
| Before | 7.57 (4.00) | 7.22 (4.11) | |
| After | 7.00 (3.56) | 7.69 (4.02) | |
| Change | −0.57, −7.5% (−1.54 to −0.40) | 0.47, 6.5% (0.19 to 0.75) | 0.01 |
| p value | 0.47 | 0.001 | |
| HADS-D | |||
| Before | 6.14 (3.77) | 6.35 (3.91) | |
| After | 4.86 (3.48) | 6.53 (3.86) | |
| Change | −1.29, −20.8% (−2.12 to −0.46) | 0.18, 2.8% (−0.16 to 0.52) | <0.001 |
| p value | 0.003 | 0.29 | |
| PSQ | |||
| Before | 55.93 (19.32) | 59.69 (17.55) | |
| After | 48.75 (17.47) | 62.63 (16.51) | |
| Change | −7.18, −12.8% (−10.99 to −3.36) | 2.94, 4.9% (1.79 to 4.08) | <0.001 |
| p value | <0.001 | <0.001 | |
| Emotional Tension | |||
| Before | 21.86 (7.28) | 22.81 (7.11) | |
| After | 18.71 (7.20) | 24.39 (6.89) | |
| Change | −3.14, −14.4% (−4.94 to −1.35) | 1.57, 6.9% (0.85 to 2.29) | <0.001 |
| p value | 0.001 | <0.001 | |
| External Stress | |||
| Before | 15.93 (6.06) | 17.80 (5.93) | |
| After | 13.89 (5.52) | 18.37 (5.49) | |
| Change | −2.04, −12.8% (−3.80 to −0.27) | 0.57, 3.2% (0.17 to 0.98) | <0.001 |
| p value | 0.02 | 0.006 | |
| Intrapsychic Stress | |||
| Before | 18.14 (7.91) | 19.08 (6.56) | |
| After | 16.14 (7.05) | 19.88 (6.30) | |
| Change | −2.00, −11.0% (−3.47 to −0.53) | 0.79, 4.2% (0.33 to 1.26) | <0.001 |
| p value | 0.009 | 0.001 | |
| Variable | MS | F Value | p Value | ηp2 | |
|---|---|---|---|---|---|
| Time | HADS | 12.96 | 3.22 | 0.08 | 0.04 |
| HADS-A | 0.09 | 0.07 | 0.80 | 0.00 | |
| HADS-D | 10.86 | 8.49 | <0.001 | 0.10 | |
| PSQ | 160.15 | 7.11 | 0.01 | 0.09 | |
| Emotional Tension | 22.00 | 3.75 | 0.06 | 0.05 | |
| External Stress | 19.10 | 4.39 | 0.04 | 0.06 | |
| Intrapsychic stress | 12.92 | 3.77 | 0.06 | 0.05 | |
| Time*Group | HADS | 56.05 | 13.94 | <0.001 | 0.16 |
| HADS-D | 9.65 | 6.79 | 0.01 | 0.08 | |
| HADS-A | 19.18 | 14.99 | <0.001 | 0.17 | |
| PSQ | 911.94 | 40.46 | <0.001 | 0.35 | |
| Emotional Tension | 198.00 | 33.77 | <0.001 | 0.31 | |
| External Stress | 60.56 | 13.91 | <0.001 | 0.16 | |
| Intrapsychic stress | 69.64 | 20.33 | <0.001 | 0.21 |
| Outcome | VR-Enhanced Rehabilitation | Standard Rehabilitation |
|---|---|---|
| Age | ||
| HADS-A | 0.13 | 0.09 |
| HADS-D | 0.14 | 0.18 |
| HADS | 0.01 | 0.17 |
| Stress | 0.07 | −0.16 |
| Initial intensity of anxiety | ||
| HADS-A | 0.48 * | 0.31 * |
| HADS-D | 0.46 * | −0.07 |
| HADS | 0.49 * | 0.10 |
| Stress | 0.18 | 0.10 |
| Initial intensity of depression | ||
| HADS-A | 0.22 | 0.18 |
| HADS-D | 0.41 * | 0.04 |
| HADS | 0.33 | 0.14 |
| Stress | 0.14 | 0.32 * |
| Initial HADS score | ||
| HADS-A | 0.40 * | 0.21 |
| HADS-D | 0.49 * | −0.02 |
| HADS | 0.47 * | 0.13 |
| Stress | 0.18 | 0.23 |
| Initial general stress | ||
| HADS-A | 0.32 | 0.20 |
| HADS-D | 0.25 | 0.02 |
| HADS | 0.30 | 0.15 |
| Stress | 0.43 * | 0.37 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jóźwik, S.; Cieślik, B.; Gajda, R.; Szczepańska-Gieracha, J. Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. J. Clin. Med. 2021, 10, 2148. https://doi.org/10.3390/jcm10102148
Jóźwik S, Cieślik B, Gajda R, Szczepańska-Gieracha J. Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. Journal of Clinical Medicine. 2021; 10(10):2148. https://doi.org/10.3390/jcm10102148
Chicago/Turabian StyleJóźwik, Sandra, Błażej Cieślik, Robert Gajda, and Joanna Szczepańska-Gieracha. 2021. "Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial" Journal of Clinical Medicine 10, no. 10: 2148. https://doi.org/10.3390/jcm10102148
APA StyleJóźwik, S., Cieślik, B., Gajda, R., & Szczepańska-Gieracha, J. (2021). Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. Journal of Clinical Medicine, 10(10), 2148. https://doi.org/10.3390/jcm10102148







