Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses
2.2. Extraction of Viral RNA
2.3. Quantitative One-Step RT-PCR
2.4. Specificity, Limit-of-Detection and Linearity of qosRT-PCR to Detect Sabin 2 Virus
2.5. qmosRT-PCRs for Virus Genome Copy Number Calculation
2.6. Illumina Sequencing
3. Results
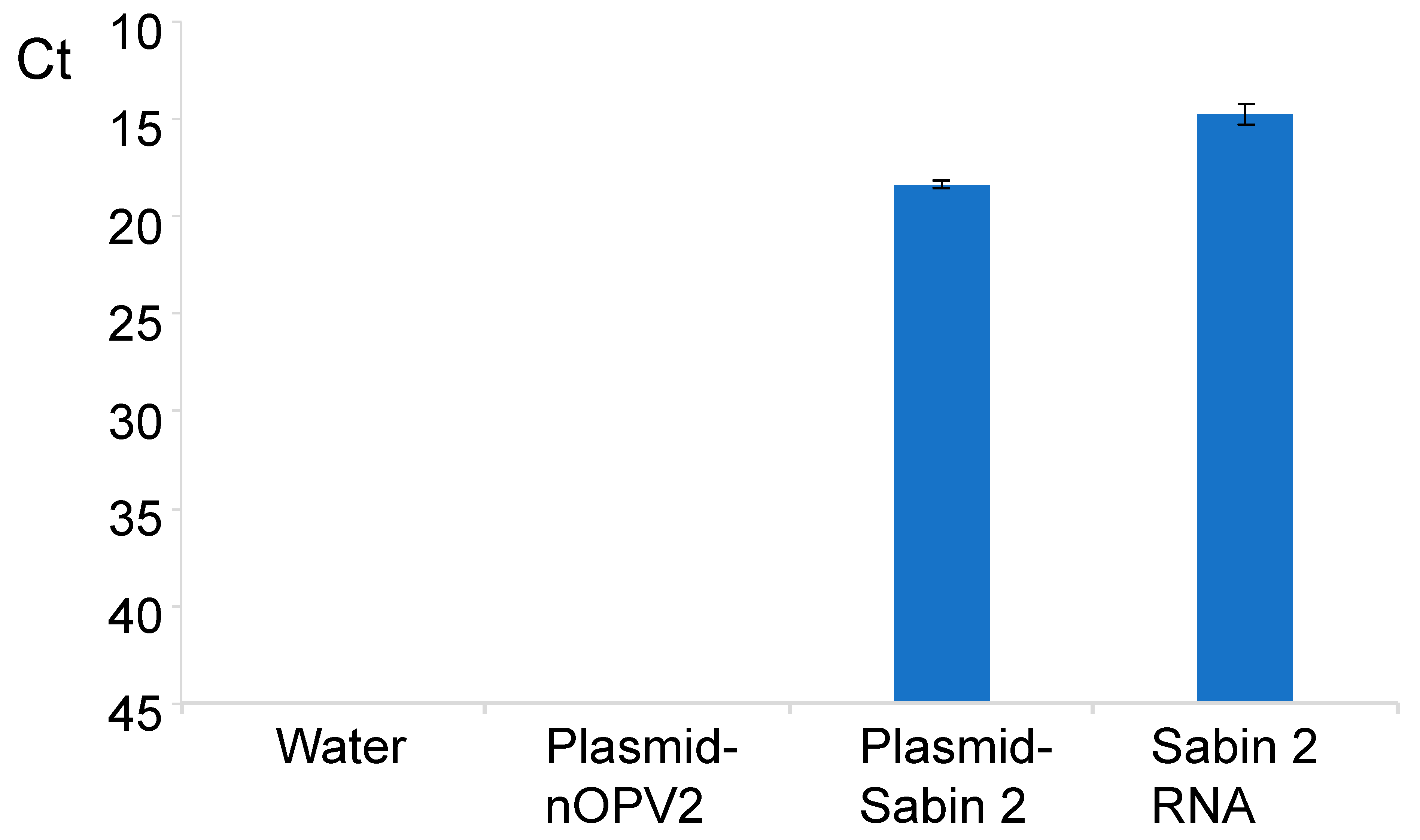
3.1. Design of Specific Primers and Probes for Sabin 2 Virus Detection and Quantification
3.2. Linearity, Specificity and Limit of Detection of the Assay for Detection of Sabin 2 RNA
3.3. Repeatability of the RT-PCR for Detection Sabin 2 Strain
3.4. Detection of Sabin 2 Virus in the Presence of nOPV2 Virus
3.5. Analysis of nOPV2 Vaccine Lots for the Presence of Sabin 2 Contamination
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laassri, M.; Lottenbach, K.; Belshe, R.; Wolff, M.; Rennels, M.; Plotkin, S.; Chumakov, K. Effect of Different Vaccination Schedules on Excretion of Oral Poliovirus Vaccine Strains. J. Infect. Dis. 2005, 192, 2092–2098. [Google Scholar] [CrossRef]
- Modlin, J.F. Mucosal immunity following oral poliovirus vaccine and enhanced potency inactivated poliovirus vaccine immunization. Pediatr. Infect. Dis. J. 1991, 10, 976–978. [Google Scholar] [CrossRef]
- Dunn, G.; Begg, N.T.; Cammack, N.; Minor, P.D. Virus excretion and mutation by infants following primary vaccination with live oral poliovaccine from two sources. J. Med. Virol. 1990, 32, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Laassri, M.; Lottenbach, K.; Belshe, R.; Rennels, M.; Plotkin, S.; Chumakov, K. Analysis of Reversions in the 5′-Untranslated Region of Attenuated Poliovirus after Sequential Administration of Inactivated and Oral Poliovirus Vaccines. J. Infect. Dis. 2006, 193, 1344–1349. [Google Scholar] [CrossRef] [PubMed]
- WHO. Two Out of Three Wild Poliovirus Strains Eradicated. Global Eradication of Wild Poliovirus Type 3 Declared on World Polio Day; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Chard, A.N.; Datta, D.; Tallis, G.; Burns, C.C.; Wassilak, S.G.F.; Vertefeuille, J.F.; Zaffran, M. Progress Toward Polio Eradication—Worldwide, January 2018–March 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 784–789. [Google Scholar] [CrossRef]
- Faden, H.; Modlin, J.F.; Thoms, M.L.; McBean, A.M.; Ferdon, M.B.; Ogra, P.L. Comparative Evaluation of Immunization with Live Attenuated and Enhanced-Potency Inactivated Trivalent Poliovirus Vaccines in Childhood: Systemic and Local Immune Responses. J. Infect. Dis. 1990, 162, 1291–1297. [Google Scholar] [CrossRef]
- This Week. Polio This Week as of 18 October 2017. This Week—GPEI—Global Polio Eradication Initiative. Available online: http://polioeradication.org/polio-today/polio-now/this-week/ (accessed on 20 June 2021).
- Burns, C.C.; Diop, O.M.; Sutter, R.W.; Kew, O.M. Vaccine-Derived Polioviruses. J. Infect. Dis. 2014, 210 (Suppl. 1), S283–S293. [Google Scholar] [CrossRef]
- Kew, O.M.; Sutter, R.W.; De Gourville, E.M.; Dowdle, W.R.; Pallansch, M.A. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu. Rev. Microbiol. 2005, 59, 587–635. [Google Scholar] [CrossRef] [PubMed]
- Platt, L.R.; Estívariz, C.F.; Sutter, R.W. Vaccine-Associated Paralytic Poliomyelitis: A Review of the Epidemiology and Estimation of the Global Burden. J. Infect. Dis. 2014, 210 (Suppl. 1), S380–S389. [Google Scholar] [CrossRef]
- Baicus, A. History of polio vaccination. World J. Virol. 2012, 1, 108–114. [Google Scholar] [CrossRef]
- John, J.; Giri, S.; Karthikeyan, A.S.; Iturriza, M.; Muliyil, J.; Abraham, A.; Grassly, N.C.; Kang, G. Effect of a single inactivated poliovirus vaccine dose on intestinal immunity against poliovirus in children previously given oral vaccine: An open-label, randomised controlled trial. Lancet 2014, 384, 1505–1512. [Google Scholar] [CrossRef]
- Rubin, J.; Ottosen, A.; Ghazieh, A.; Fournier-Caruana, J.; Ntow, A.K.; Gonzalez, A.R. Managing the Planned Cessation of a Global Supply Market: Lessons Learned From the Global Cessation of the Trivalent Oral Poliovirus Vaccine Market. J. Infect. Dis. 2017, 216 (Suppl. 1), S40–S45. [Google Scholar] [CrossRef][Green Version]
- Brickley, E.B.; Strauch, C.B.; Wieland-Alter, W.F.; Connor, R.I.; Lin, S.; Weiner, J.A.; Ackerman, M.E.; Arita, M.; Oberste, M.S.; Weldon, W.C.; et al. Intestinal Immune Responses to Type 2 Oral Polio Vaccine (OPV) Challenge in Infants Previously Immunized with Bivalent OPV and Either High-Dose or Standard Inactivated Polio Vaccine. J. Infect. Dis. 2018, 217, 371–380. [Google Scholar] [CrossRef]
- Thompson, K.M.; Duintjer Tebbens, R.J. Lessons from the Polio Endgame: Overcoming the Failure to Vaccinate and the Role of Subpopulations in Maintaining Transmission. J. Infect. Dis. 2017, 216 (Suppl. 1), S176–S182. [Google Scholar] [CrossRef]
- Wright, P.F.; Connor, R.I.; Wieland-Alter, W.F.; Hoen, A.G.; Boesch, A.W.; Ackerman, M.E.; Oberste, M.S.; Gast, C.; Brickley, E.; Asturias, E.J.; et al. Vaccine-induced mucosal immunity to poliovirus: Analysis of cohorts from an open-label, randomised controlled trial in Latin American infants. Lancet Infect. Dis. 2016, 16, 1377–1384. [Google Scholar] [CrossRef]
- Konopka-Anstadt, J.L.; Campagnoli, R.; Vincent, A.; Shaw, J.; Wei, L.; Wynn, N.T.; Smithee, S.E.; Bujaki, E.; Yeh, M.T.; Laassri, M.; et al. Development of a new oral poliovirus vaccine for the eradication end game using codon deoptimization. NPJ Vaccines 2020, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Macadam, A.J.; Ferguson, G.; Stone, D.M.; Meredith, J.; Knowlson, S.; Auda, G.; Almond, J.W.; Minor, P.D. Rational design of genetically stable, live-attenuated poliovirus vaccines of all three serotypes: Relevance to poliomyelitis eradication. J. Virol. 2006, 80, 8653–8663. [Google Scholar] [CrossRef] [PubMed]
- Van der Avoort, H.G.; Hull, B.P.; Hovi, T.; Pallansch, M.A.; Kew, O.M.; Crainic, R.; Wood, D.J.; Mulders, M.N.; Van Loon, A.M. Comparative study of five methods for intratypic differentiation of polioviruses. J. Clin. Microbiol. 1995, 33, 2562–3566. [Google Scholar] [CrossRef] [PubMed]
- Buonagurio, D.A.; Coleman, J.W.; Patibandla, S.A.; Prabhakar, B.S.; Tatem, J.M. Direct detection of Sabin poliovirus vaccine strains in stool specimens of first-dose vaccinees by a sensitive reverse transcription-PCR method. J. Clin. Microbiol. 1999, 37, 283–289. [Google Scholar] [CrossRef]
- De, L.; Nottay, B.; Yang, C.F.; Holloway, B.P.; Pallansch, M.; Kew, O. Identification of vaccine-related polioviruses by hybridization with specific RNA probes. J. Clin. Microbiol. 1995, 33, 562–571. [Google Scholar] [CrossRef]
- Kilpatrick, D.R.; Yang, C.-F.; Ching, K.; Vincent, A.; Iber, J.; Campagnoli, R.; Mandelbaum, M.; De, L.; Yang, S.J.; Nix, A.; et al. Rapid group-, serotype-, and vaccine strain-specific identification of poliovirus isolates by real-time reverse transcription-PCR using degenerate primers and probes containing deoxyinosine residues. J. Clin. Microbiol. 2009, 47, 1939–1941. [Google Scholar] [CrossRef] [PubMed]
- Laassri, M.; Dipiazza, A.; Bidzhieva, B.; Zagorodnyaya, T.; Chumakov, K. Quantitative one-step RT-PCR assay for rapid and sensitive identification and titration of polioviruses in clinical specimens. J. Virol. Methods 2013, 189, 7–14. [Google Scholar] [CrossRef]
- Laassri, M.; Mee, E.T.; Connaughton, S.M.; Manukyan, H.; Gruber, M.; Hernandez, C.R.; Minor, P.D.; Schepelmann, S.; Chumakov, K.; Wood, D.J. Detection of bovine viral diarrhoea virus nucleic acid, but not infectious virus, in bovine serum used for human vaccine manufacture. Biologicals 2018, 55, 63–70. [Google Scholar] [CrossRef]
- van der Werf, S.; Bradley, J.; Wimmer, E.; Studier, F.W.; Dunn, J.J. Synthesis of infectious poliovirus RNA by purified T7 RNA polymerase. Proc. Natl. Acad. Sci. USA 1986, 83, 2330–2334. [Google Scholar] [CrossRef] [PubMed]
- Manukyan, H.; Rodionova, E.; Zagorodnyaya, C.; Lin, T.-L.; Chumakov, K.; Laassri, M. Multiplex PCR-based titration (MPBT) assay for determination of infectious titers of the three Sabin strains of live poliovirus vaccine. Virol. J. 2019, 16, 122. [Google Scholar] [CrossRef] [PubMed]
- Simonyan, V.; Mazumder, R. High-Performance Integrated Virtual Environment (HIVE) Tools and Applications for Big Data Analysis. Genes 2014, 5, 957–981. [Google Scholar] [CrossRef] [PubMed]
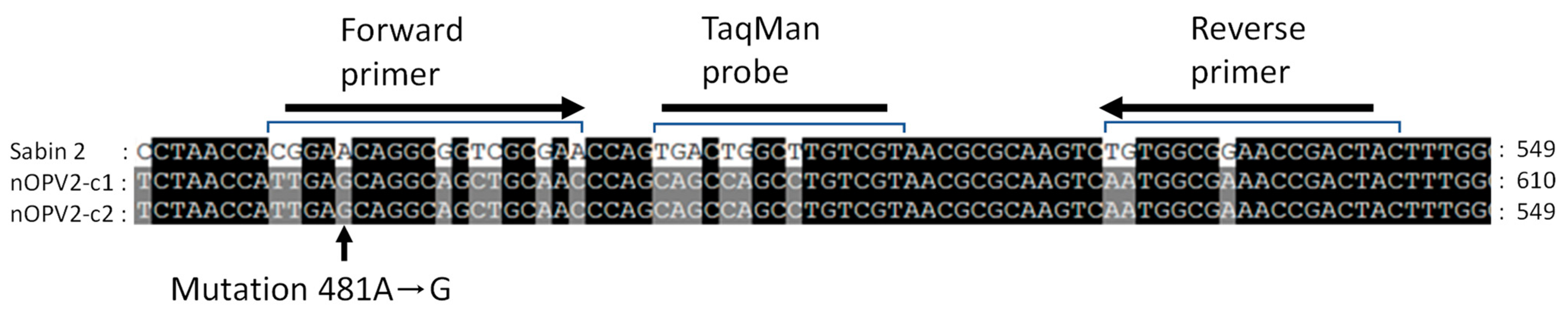


| Name | Seq 5′-->3′ | Sabin 2 Location | Tm (Basic) | Size (nt) | Amplicon Size (bp) |
|---|---|---|---|---|---|
| Sab2-605R (Reverse) | GTAGTCGGTTCCGCCACA | 544–527 | 57 | 18 | 67 |
| Sab2-538F (Forward) | CGGAACAGGCGGTCGCGAA | 477–495 | 58 | 19 | |
| Sab2PrbFAM2 (TaqMan Probe) | FAM-TGACTGGCTTGTCGT-ZEN//3IaBkFQ/ | 500–514 | 42 | 15 |
| Day | Run | Sabin 2 Virus | ||
|---|---|---|---|---|
| Sample 7 | Sample 8 | Sample 9 | ||
| 1 | 1 | 215.94 220.22 216.14 240.09 | 19.47 12.99 19.86 14.87 | 2.68 3.90 2.03 1.16 |
| 2 | 2 | 190.05 249.62 300.66 297.63 | 12.43 15.83 17.27 8.84 | 3.59 4.42 4.16 5.01 |
| 3 | 269.98 280.74 249.19 289.66 | 19.41 10.69 18.93 16.35 | 9.32 3.18 3.62 | |
| Average | 251.66 | 15.58 | 3.92 | |
| STDEV | 36.44 | 3.68 | 2.10 | |
| Sample Names | % of Spiked Sabin 2 Virus in nOPV2c1-295 | Sabin 2 Titers (Log10 CCID50/mL) | Average Ct ± STDEV |
|---|---|---|---|
| 1 | 16.98 | 7.34 | 16.00 ± 0.11 |
| 2 | 1.91 | 6.34 | 19.28 ± 0.08 |
| 3 | 1.94 × 10−1 | 5.34 | 22.79 ± 0.12 |
| 4 | 1.94 × 10−2 | 4.34 | 26.87 ± 0.58 |
| 5 | 1.94 × 10−3 | 3.34 | 29.88 ± 0.10 |
| 6 | 1.94 × 10−4 | 2.34 | 32.83 ± 0.20 |
| 7 | 1.94 × 10−5 | 1.34 | 35.23 ± 0.19 |
| 8 | 1.94 × 10−6 | 0.34 | 37.71 ± 0.61 |
| 9 | 1.94 × 10−7 | −0.66 | 39.72 ± 0.48 |
| 10 | 1.94 × 10−8 | −1.67 | UD |
| 11 | 1.94 × 10−9 | −2.67 | UD |
| 12 | 1.94 × 10−10 | −3.67 | UD |
| Water | Negative Controls | NA | UD |
| nOPV2c1-295 virus | 8.07 | UD | |
| nOPV2 plasmid | 1 ng/µL | UD | |
| Sabin 2 plasmid | Positive Control | 0.1 ng/µL | 16.93 ± 0.34 |
| Expected % (CCID50) | GC# % | NGS % |
|---|---|---|
| R2 = 0.98 | R2 = 1.00 | |
| 16.98 | 32.02 | 18.02 |
| 1.91 | 7.59 | 1.94 |
| 1.94 × 10−1 | 1.32 | 0.23 |
| 1.94 × 10−2 | 1.02 × 10−1 | UD |
| 1.94 × 10−3 | 4.21 × 10−3 | UD |
| 1.94 × 10−4 | 5.67 × 10−5 | UD |
| 1.94 × 10−5 | 1.77 × 10−7 | UD |
| 1.94 × 10−6 | UD | UD |
| 1.94 × 10−7 | UD | UD |
| 1.94 × 10−8 | UD | UD |
| 1.94 × 10−9 | UD | UD |
| 1.94 × 10−10 | UD | UD |
| nOPV 2 Lots | Day 1 | Day 2 | Day 3 | NGS Result | ||||
|---|---|---|---|---|---|---|---|---|
| Run1: Ct | Result | Run 2: Ct | Result | Run 3: Ct | Result | Sabin 2 | nOPV2 | |
| Monovalent nOPV2-c1 | ||||||||
| nPol2 016C-c1 | UD | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | 40 | ||||||
| nPol2 018C-c2 | UD | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| Drug product nOPV2-c1 | ||||||||
| 2060119C | UD | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| 2060219C | UD | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| 2060319C | UD | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| Monovalent nOPV2-c2 | ||||||||
| nPOL 2056C | 43 | Negative | UD | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| nPOL 2038C | UD | Negative | 40 | Negative | UD | Negative | Negative | Positive |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| Negative controls | ||||||||
| Water | UD | Negative | UD | Negative | UD | Negative | NA | NA |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| nOPV2-Plasmid | UD | Negative | UD | Negative | UD | Negative | NA | NA |
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| UD | UD | UD | ||||||
| Positive control | ||||||||
| Sabin 2-plasmid | 18 | Positive | 14 | Positive | 15 | Positive | NA | NA |
| 17 | 14 | 15 | ||||||
| 18 | 13 | 14 | ||||||
| 18 | 14 | 15 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manukyan, H.; Tritama, E.; Wahid, R.; Ansari, A.; Konz, J.; Chumakov, K.; Laassri, M. Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2. Vaccines 2021, 9, 688. https://doi.org/10.3390/vaccines9070688
Manukyan H, Tritama E, Wahid R, Ansari A, Konz J, Chumakov K, Laassri M. Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2. Vaccines. 2021; 9(7):688. https://doi.org/10.3390/vaccines9070688
Chicago/Turabian StyleManukyan, Hasmik, Erman Tritama, Rahnuma Wahid, Azeem Ansari, John Konz, Konstantin Chumakov, and Majid Laassri. 2021. "Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2" Vaccines 9, no. 7: 688. https://doi.org/10.3390/vaccines9070688
APA StyleManukyan, H., Tritama, E., Wahid, R., Ansari, A., Konz, J., Chumakov, K., & Laassri, M. (2021). Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2. Vaccines, 9(7), 688. https://doi.org/10.3390/vaccines9070688






