SARS-CoV-2 Infection Anxiety, Knowledge and Attitudes in University Degree Pregnant Women from Romania—A Cross-Sectional Observational Survey in the First Two Pandemic Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Participants
2.2. Survey Questionnaire and Data Collection
2.3. Ethical Approval
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. SARS-CoV-2 Symptoms in Pregnancy
4.2. Anxiety of Pregnant Women in COVID-19 Pandemic
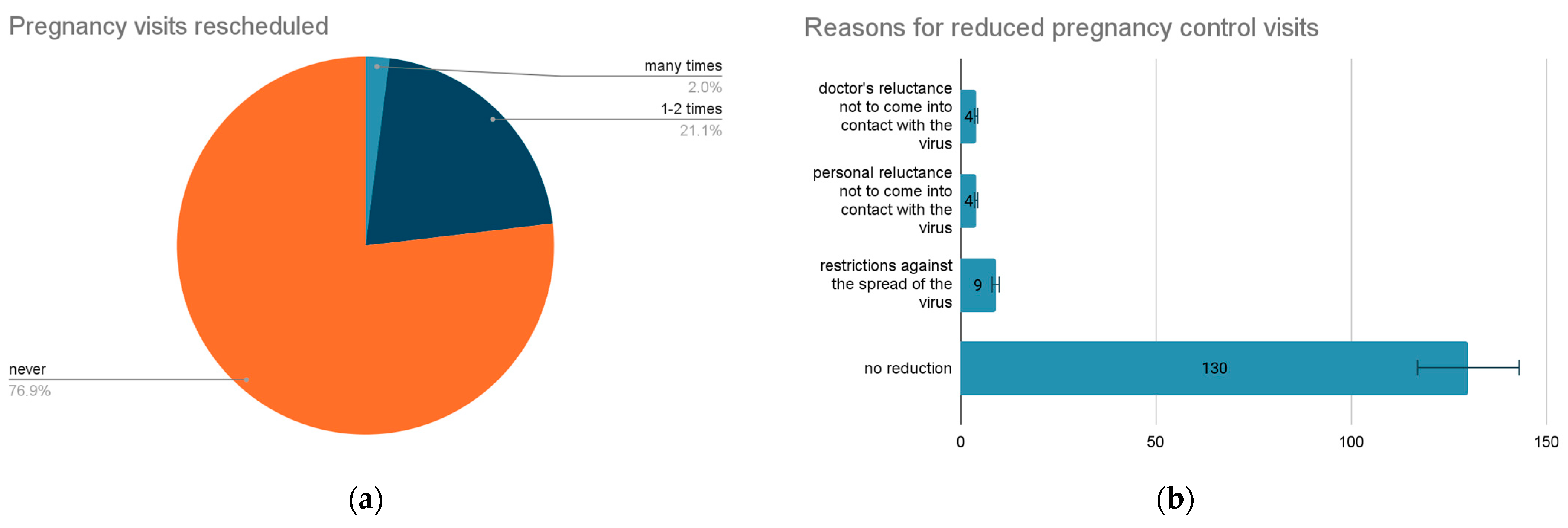
4.3. Monitorization of Pregnancy in COVID-19 Pandemic
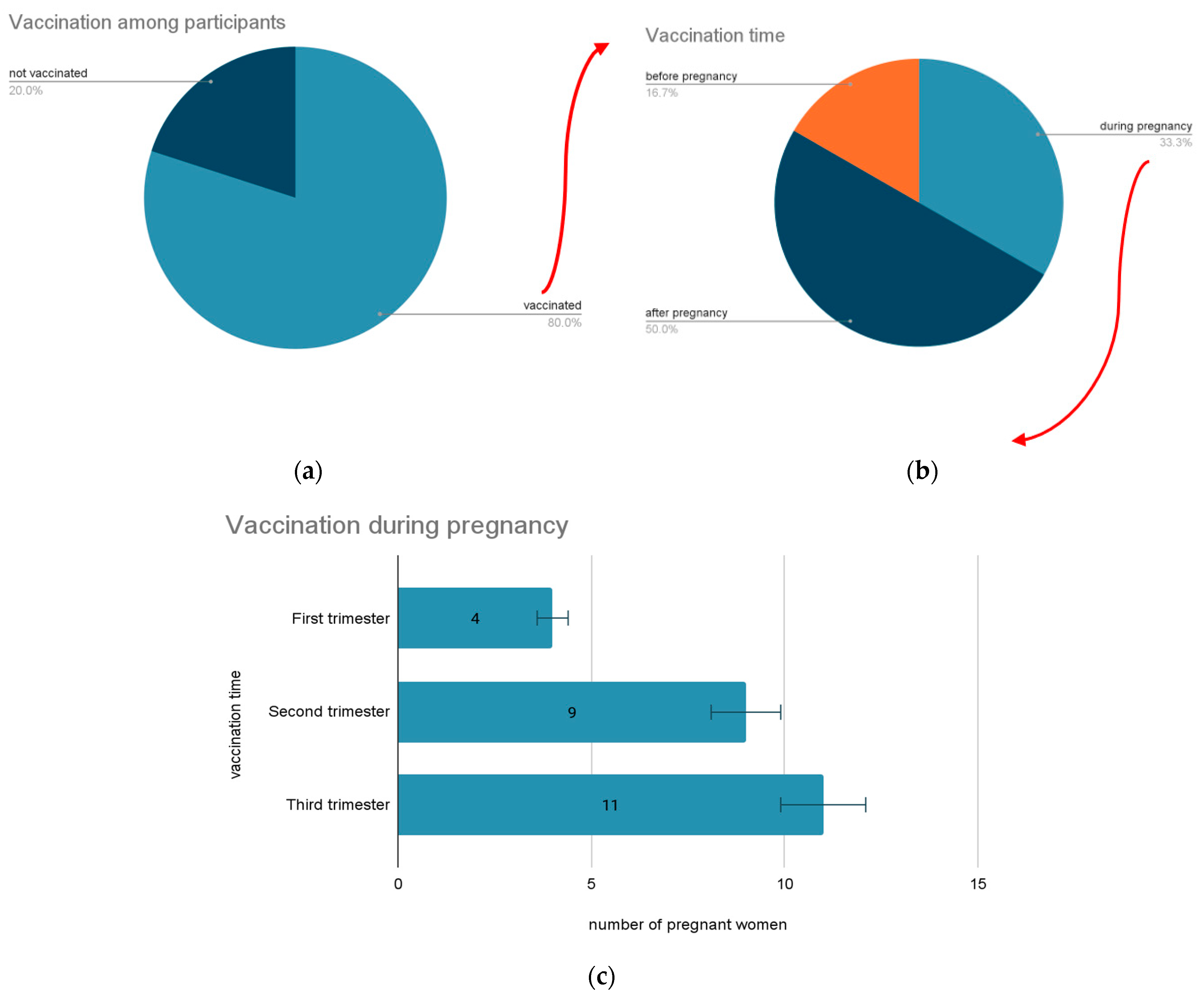
4.4. Preventive Measures Taken—Outcomes and Influences upon Pregnancy
4.5. Limitation of the Study
4.6. Future Developments
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public. Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- Gheorghe, A.S.; Negru, Ş.M.; Nițipir, C.; Mazilu, L.; Marinca, M.; Gafton, B.; Ciuleanu, T.E.; Schenker, M.; Dragomir, R.D.; Gheorghe, A.D.; et al. Knowledge, Attitudes and Practices Related to the COVID-19 Outbreak among Romanian Adults with Cancer: A Cross-Sectional National Survey. ESMO Open 2021, 6, 100027. [Google Scholar] [CrossRef] [PubMed]
- Cocoş, R.; Mahler, B.; Turcu-Stiolica, A.; Stoichiță, A.; Ghinet, A.; Shelby, E.-S.; Bohîlțea, L.C. Risk of Death in Comorbidity Subgroups of Hospitalized COVID-19 Patients Inferred by Routine Laboratory Markers of Systemic Inflammation on Admission: A Retrospective Study. Viruses 2022, 14, 1201. [Google Scholar] [CrossRef]
- Oțelea, M.R.; Zugravu, C.; Rașcu, A.; Arghir, O.C.; Manolescu, L.S.C.; Mates, D. Coronasomnia in Employees without a Direct Contact with COVID-19 Infected Patients in Their Workplace. Healthcare 2022, 10, 1194. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.R.; Jaswa, E.; Kaing, A.; Hariton, E.; Andrusier, M.; Aliaga, K.; Davis, M.; Cedars, M.I.; Huddleston, H.G. Early Pregnancy Anxiety during the COVID-19 Pandemic: Preliminary Findings from the UCSF ASPIRE Study. BMC Pregnancy Childbirth 2022, 22, 272. [Google Scholar] [CrossRef] [PubMed]
- Maternal Mental Health. Available online: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/maternal-mental-health (accessed on 20 December 2022).
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Medar, C.; et al. COVID-19 Parental Vaccine Hesitancy in Romania: Nationwide Cross-Sectional Study. Vaccines 2022, 10, 493. [Google Scholar] [CrossRef]
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Chivu, R.D. Early COVID-19 Vaccination of Romanian Medical and Social Personnel. Vaccines 2021, 9, 1127. [Google Scholar] [CrossRef]
- Serra, F.E.; Rosa Junior, E.R.; de Rossi, P.; Francisco, R.P.V.; Rodrigues, A.S. COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women. Vaccines 2022, 10, 2172. [Google Scholar] [CrossRef]
- Staneva, A.; Bogossian, F.; Pritchard, M.; Wittkowski, A. The Effects of Maternal Depression, Anxiety, and Perceived Stress during Pregnancy on Preterm Birth: A Systematic Review. Women Birth J. Aust. Coll. Midwives 2015, 28, 179–193. [Google Scholar] [CrossRef]
- Mahler, B.; Croitoru, A. Pulmonary rehabilitation and tuberculosis: A new approach for an old disease. Pneumologia 2019, 68, 107–113. [Google Scholar] [CrossRef]
- Zaigham, M.; Andersson, O. Maternal and Perinatal Outcomes with COVID-19: A Systematic Review of 108 Pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhou, Y.-H.; Yang, H.-X.; Poon, L.C. Intrauterine Vertical Transmission of SARS-CoV-2: What We Know so Far. Ultrasound Obstet. Gynecol. 2020, 55, 724–725. [Google Scholar] [CrossRef] [PubMed]
- Sharps, M.C.; Hayes, D.J.L.; Lee, S.; Zou, Z.; Brady, C.A.; Almoghrabi, Y.; Kerby, A.; Tamber, K.K.; Jones, C.J.; Adams Waldorf, K.M.; et al. A Structured Review of Placental Morphology and Histopathological Lesions Associated with SARS-CoV-2 Infection. Placenta 2020, 101, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Abebe, E.C.; Tiruneh, G.A.; Adela, G.A.; Ayele, T.M.; Muche, Z.T.; T/Mariam, A.B.; Mulu, A.T.; Zewde, E.A.; Baye, N.D.; Dejenie, T.A. COVID-19 Vaccine Uptake and Associated Factors among Pregnant Women Attending Antenatal Care in Debre Tabor Public Health Institutions: A Cross-Sectional Study. Front. Public Health 2022, 10, 919494. [Google Scholar] [CrossRef]
- Gray, K.J.; Bordt, E.A.; Atyeo, C.; Deriso, E.; Akinwunmi, B.; Young, N.; Baez, A.M.; Shook, L.L.; Cvrk, D.; James, K.; et al. Coronavirus Disease 2019 Vaccine Response in Pregnant and Lactating Women: A Cohort Study. Am. J. Obstet. Gynecol. 2021, 225, 303.e1–303.e17. [Google Scholar] [CrossRef]
- Checklists. Available online: https://www.strobe-statement.org/checklists/ (accessed on 28 November 2022).
- Ali, N.A.; Feroz, A.S. Maternal Mental Health Amidst the COVID-19 Pandemic. Asian J. Psychiatry 2020, 54, 102261. [Google Scholar] [CrossRef]
- Taubman-Ben-Ari, O.; Chasson, M.; Sharkia, S.A.; Weiss, E. Distress and Anxiety Associated with COVID-19 among Jewish and Arab Pregnant Women in Israel. J. Reprod. Infant Psychol. 2020, 38, 340–348. [Google Scholar] [CrossRef]
- Davenport, M.H.; Meyer, S.; Meah, V.L.; Strynadka, M.C.; Khurana, R. Moms Are Not OK: COVID-19 and Maternal Mental Health. Front. Glob. Womens Health 2020, 1, 1. [Google Scholar] [CrossRef]
- Alzamora, M.C.; Paredes, T.; Caceres, D.; Webb, C.M.; Valdez, L.M.; La Rosa, M. Severe COVID-19 during Pregnancy and Possible Vertical Transmission. Am. J. Perinatol. 2020, 37, 861–865. [Google Scholar] [CrossRef]
- Orzechowski, M.; Timmermann, C.; Woniak, K.; Kosenko, O.; Mikirtichan, G.L.; Lichtshangof, A.Z.; Steger, F. Access to Prenatal Testing and Ethically Informed Counselling in Germany, Poland and Russia. J. Pers. Med. 2021, 11, 937. [Google Scholar] [CrossRef]
- Ilska, M.; Brandt-Salmeri, A.; Kołodziej-Zaleska, A.; Preis, H.; Rehbein, E.; Lobel, M. Anxiety among Pregnant Women during the First Wave of the COVID-19 Pandemic in Poland. Sci. Rep. 2022, 12, 8445. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Gonzalo, S.; Caballero-Galilea, M.; González-Pascual, J.L.; Álvaro-Navidad, M.; Esteban-Gonzalo, L. Anxiety and Worries among Pregnant Women during the COVID-19 Pandemic: A Multilevel Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6875. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Lu, J.; Zhou, Y.; Wei, W.; Zhou, Z.; Chen, M. Knowledge, Attitudes, Practices, and Influencing Factors of Anxiety among Pregnant Women in Wuhan during the Outbreak of COVID-19: A Cross-Sectional Study. BMC Pregnancy Childbirth 2021, 21, 80. [Google Scholar] [CrossRef]
- Pihkala, P. Eco-Anxiety, Tragedy, and Hope: Psychological and Spiritual Dimensions of Climate Change. Zygon® 2018, 53, 545–569. [Google Scholar] [CrossRef]
- Cricenti, C.; Mari, E.; Barchielli, B.; Quaglieri, A.; Burrai, J.; Pizzo, A.; D’Alessio, I.; Giannini, A.M.; Ferracuti, S.; Lausi, G. Can Emotion Regulation Affect Aggressive Responses? A Study on the Ukrainian-Russian Conflict in a Non-Directly Exposed Sample. Int. J. Environ. Res. Public Health 2022, 19, 6189. [Google Scholar] [CrossRef]
- Giudice, V.; Iannaccone, T.; Faiella, F.; Ferrara, F.; Aversano, G.; Coppola, S.; De Chiara, E.; Romano, M.G.; Conti, V.; Filippelli, A. Gender Differences in the Impact of COVID-19 Pandemic on Mental Health of Italian Academic Workers. J. Pers. Med. 2022, 12, 613. [Google Scholar] [CrossRef]
- Study of Anxiety, Fear and Depression Associated with Breastfeeding in COVID-Positive Mothers. Available online: https://www.jsafog.com/abstractArticleContentBrowse/JSAFOG/25952/JPJ/fullText (accessed on 20 December 2022).
- New Research Highlights Risks of Separating Newborns from Mothers during COVID-19 Pandemic. Available online: https://www.who.int/news/item/16-03-2021-new-research-highlights-risks-of-separating-newborns-from-mothers-during-covid-19-pandemic (accessed on 9 December 2022).
- Gebretsadik, G.G.; Tadesse, Z.; Mamo, L.; Adhanu, A.K.; Mulugeta, A. Knowledge, Attitude, and Determinants of Exclusive Breastfeeding during COVID-19 Pandemic among Lactating Mothers in Mekelle, Tigrai: A Cross Sectional Study. BMC Pregnancy Childbirth 2022, 22, 850. [Google Scholar] [CrossRef]
- Radu, M.C.; Boeru, A.C.; Marin, M.; Manolescu, L.S. Diabetes Mellitus and Pregnancy. In Proceedings of the International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications INTERDIAB 2020, Bucharest, Romania, 5–7 March 2020; Volume 1, pp. 278–286, ISBN 978-88-85813-79-3. [Google Scholar]
- Radu, M.C.; Manolescu, L.S.; Chivu, R.; Zaharia, C.; Boeru, C.; Pop-Tudose, M.-E.; Necsulescu, A.; Otelea, M. Pregnancy in Teenage Romanian Mothers. Cureus 2022, 14, e21540. [Google Scholar] [CrossRef]
- Niță, I.; Nițipir, C.; Toma, S.A.; Limbău, A.M.; Pîrvu, E.; Bădărău, I.A.; Suciu, I.; Suciu, G.; Manolescu, L.S.C. Correlation between Androgen Receptor Expression and Immunohistochemistry Type as Prognostic Factors in a Cohort of Breast Cancer Patients: Result from a Single-Center, Cross Sectional Study. Healthcare 2021, 9, 277. [Google Scholar] [CrossRef]
- Snyder, K.; Worlton, G. Social Support During COVID-19: Perspectives of Breastfeeding Mothers. Breastfeed. Med. 2021, 16, 39–45. [Google Scholar] [CrossRef]
- Loleka, B.Y.; Ogawa, K. Influence of the Level of Education on Women’s Knowledge, Attitude, and Practices to Control the Transmission of COVID-19 in the Democratic Republic of the Congo. Sci. Afr. 2022, 17, e01299. [Google Scholar] [CrossRef] [PubMed]
- Shahbaznejad, L.; Navaeifar, M.R.; Movahedi, F.S.; Hosseinzadeh, F.; Fahimzad, S.A.; Shirazi, Z.S.; Rezai, M.S. Knowledge, Attitude and Practice of Sari Birth Cohort Members during Early Weeks of COVID-19 Outbreak in Iran. BMC Public Health 2021, 21, 982. [Google Scholar] [CrossRef] [PubMed]
- Goshiye, D.; Abegaz, Z.; Gedamu, S. Knowledge, Attitude, and Practice towards COVID-19 among Mothers in Dessie Town, Northeast Ethiopia, 2020. Interdiscip. Perspect. Infect. Dis. 2022, 2022, 4377460. [Google Scholar] [CrossRef]
- Mose, A.; Zewdie, A.; Sahle, T. Pregnant Women’s Knowledge, Attitude, and Practice towards COVID-19 Infection Prevention in Ethiopia: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0276692. [Google Scholar] [CrossRef]
- Sengupta, M.; Dutta, S.; Roy, A.; Chakrabarti, S.; Mukhopadhyay, I. Knowledge, Attitude and Practice Survey towards COVID-19 Vaccination: A Mediation Analysis. Int. J. Health Plann. Manage. 2022, 37, 2063–2080. [Google Scholar] [CrossRef]
- Radu, M.C.; Boeru, C.; Marin, M.; Manolescu, L.S. SARS-CoV-2 Infection in Seven Childbearing Women at the Moment of Delivery, a Romanian Experience. Cureus 2021, 13, e12811. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | N = 147(%) |
|---|---|
| Family status (married) | 127 (86.4%) |
| Domain of activity (employed) | 140 (95.2%) |
| Geographic area (urban) | 140 (95.2%) |
| Post-secondary school studies | 4 (2.7%) |
| University / Post-university studies | 143 (97.3%) |
| Pregnancy (monitored) | 147 (100%) |
| Birth (C-section) | 33 (22.45%) |
| SARS-CoV-2 infected during pregnancy | 27 (18.36%) |
| Isolated at birth 2 weeks | 6 (4.08%) |
| Vaccinated against COVID-19 | 118 (80%) |
| Anxiety in the pandemic context | 141 (95.91%) |
| Level of Anxiety | 1–2 | 2–3 | 3–4 | 4–5 |
|---|---|---|---|---|
| SARS-CoV-2 infected/not infected | 0.7575 | 0.4314 | 0.3764 | 0.3982 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Preda, M.; Dinu, R.S.; Prasacu, I.; Manolescu, L.S.C. SARS-CoV-2 Infection Anxiety, Knowledge and Attitudes in University Degree Pregnant Women from Romania—A Cross-Sectional Observational Survey in the First Two Pandemic Years. Vaccines 2023, 11, 35. https://doi.org/10.3390/vaccines11010035
Preda M, Dinu RS, Prasacu I, Manolescu LSC. SARS-CoV-2 Infection Anxiety, Knowledge and Attitudes in University Degree Pregnant Women from Romania—A Cross-Sectional Observational Survey in the First Two Pandemic Years. Vaccines. 2023; 11(1):35. https://doi.org/10.3390/vaccines11010035
Chicago/Turabian StylePreda, Madalina, Rares Sebastian Dinu, Irina Prasacu, and Loredana Sabina Cornelia Manolescu. 2023. "SARS-CoV-2 Infection Anxiety, Knowledge and Attitudes in University Degree Pregnant Women from Romania—A Cross-Sectional Observational Survey in the First Two Pandemic Years" Vaccines 11, no. 1: 35. https://doi.org/10.3390/vaccines11010035
APA StylePreda, M., Dinu, R. S., Prasacu, I., & Manolescu, L. S. C. (2023). SARS-CoV-2 Infection Anxiety, Knowledge and Attitudes in University Degree Pregnant Women from Romania—A Cross-Sectional Observational Survey in the First Two Pandemic Years. Vaccines, 11(1), 35. https://doi.org/10.3390/vaccines11010035







