The Willingness of Parents to Vaccinate Their Children Aged from Five to under Twelve Years with COVID-19 Vaccines between February and March 2022 in Vietnam
Abstract
1. Introduction
2. Research Design, Methodology, and Models
2.1. Study Design
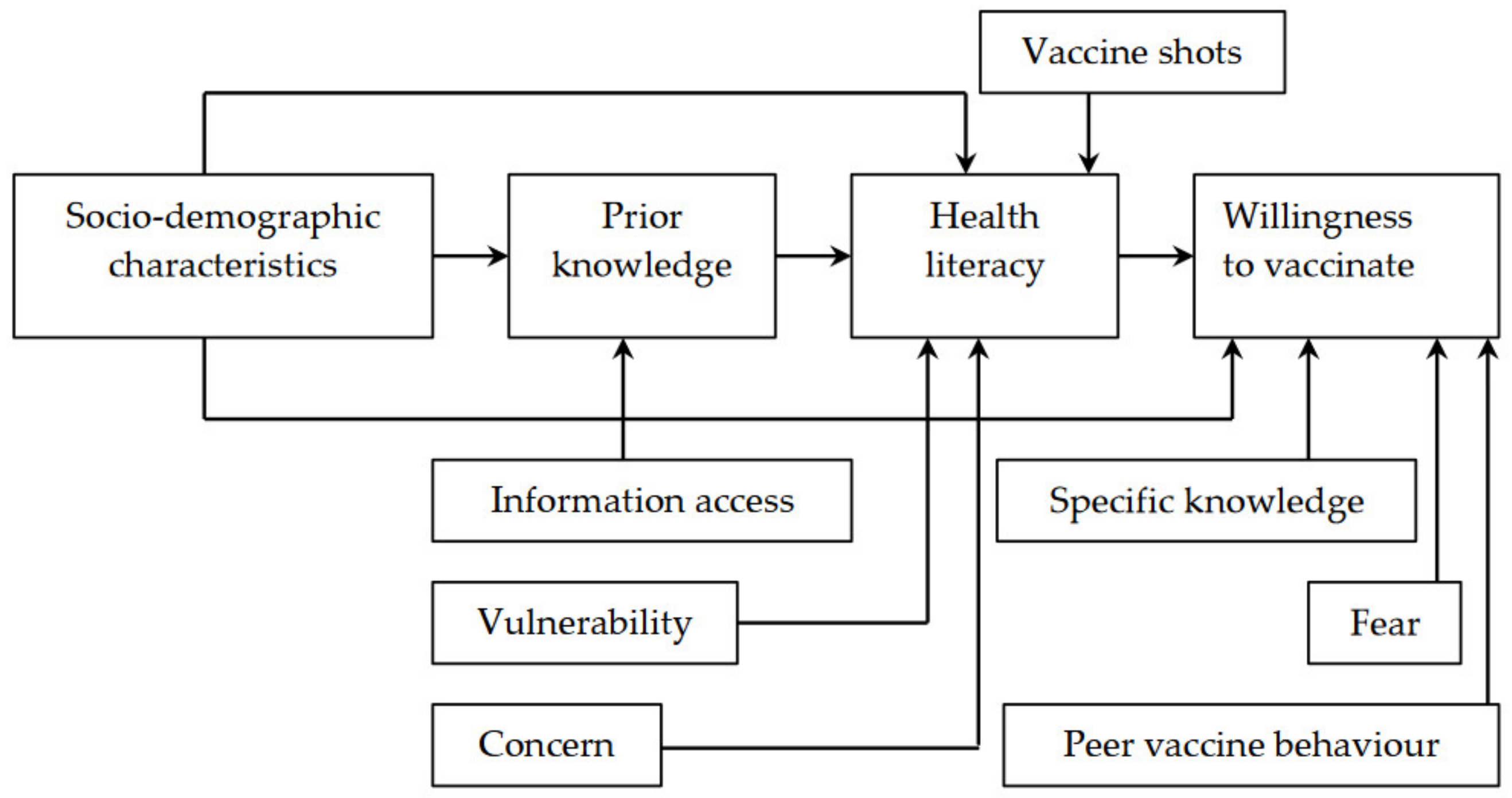
2.2. Research Methodologies, Models, and Variable Description
3. Results
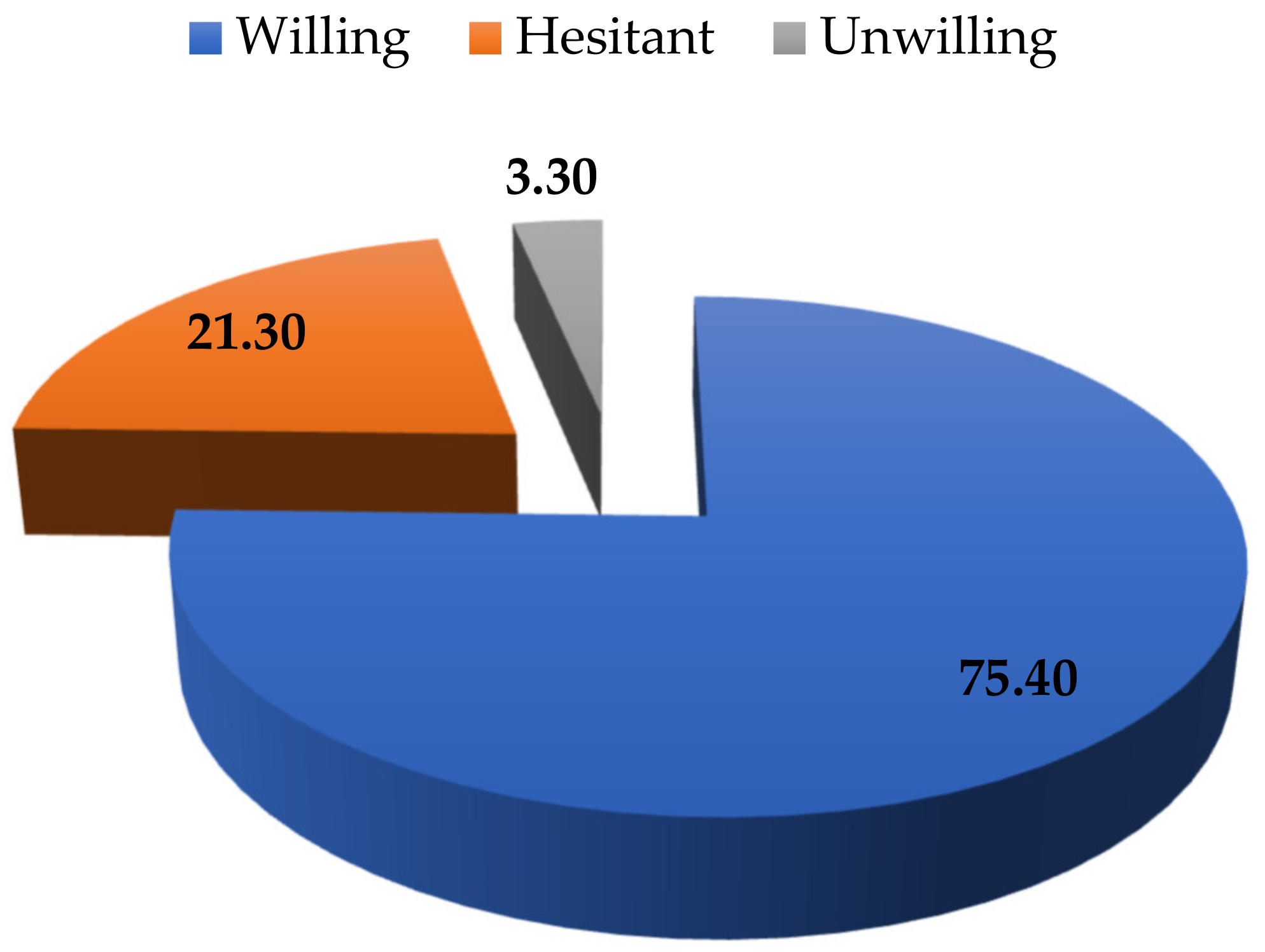
3.1. The Willingness of Parents to Vaccinate Their Children
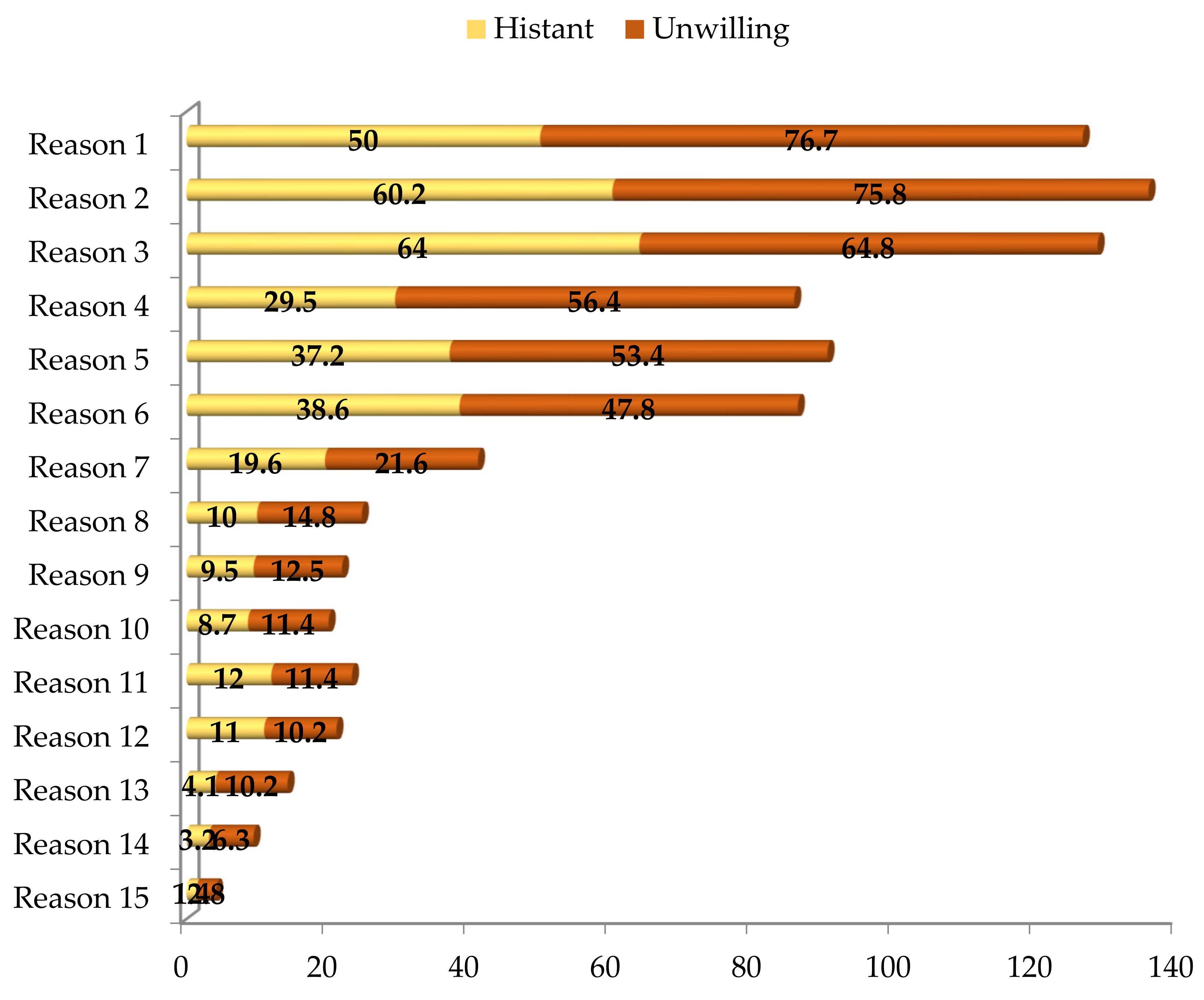
3.2. Reasons That Made Parents Hesitant or Unwilling to Vaccinate Their Children
3.3. Preferences of Parents on Vaccine Origin to Vaccinate Their Children
3.4. The Association between the Willingness of Parents to Vaccinate Their Children Aged from 5 to under 12 Years and Selected Influential Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
References
- Covidvax. Vietnam. 2022. Available online: https://COVIDvax.live/location/vnm (accessed on 1 March 2022).
- Our World in Data. Coronavirus (COVID-19) Vaccinations. 2022. Available online: https://ourworldindata.org/COVID-vaccinations (accessed on 1 March 2022).
- MoH. Vaccination against COVID-19 for Children Aged 5–11 Years Old Step by Step, Cautiously, Putting Safety First. 2022. Available online: https://suckhoedoisong.vn/tiem-vaccine-phong-COVID-19-cho-tre-tu-5-11-tuoi-tung-buoc-than-trong-dat-an-toan-len-hang-dau-169220203092531074.htm (accessed on 1 March 2022).
- Kloc, M.; Ghobrial, R.M.; Kuchar, E.; Lewicki, S.; Kubiak, J.Z. Development of child immunity in the context of COVID-19 pandemic. Clin. Immunol. 2020, 217, 108510. [Google Scholar] [CrossRef] [PubMed]
- Janeway, C.A. The Immunological System of the Child: Part I: Development of Immunity in the Child. Arch. Dis. Child. 1966, 41, 358–365. [Google Scholar] [CrossRef] [PubMed]
- CDC. COVID-19 Vaccines for Children And Adolescents. 2022. Available online: https://vietnamese.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/children-teens.html (accessed on 1 March 2022).
- Vietnamese Government. Child Mortality Rate Caused by COVID-19 Is Low But Do Not Be Subjective. 2022. Available online: https://baochinhphu.vn/ty-le-tre-tu-vong-do-COVID-19-thap-nhung-khong-chu-quan-10222021617594895.htm (accessed on 1 March 2022).
- Vietnam New Agency Plus. The Number of COVID-19 Cases among Children Aged 5 to under 12 Years Old Has Increased 2022b. Available online: https://www.vietnamplus.vn/so-ca-mac-COVID19-o-nhom-tre-tu-5-den-duoi-12-tuoi-gia-tang/776178.vnp (accessed on 1 March 2022).
- Vietnam New Agency Plus. 11.8 Million Children from 5 to under 12 Years Old Are Subject to The COVID-19 Vaccines 2022c. Available online: https://www.vietnamplus.vn/118-trieu-tre-tu-5-den-duoi-12-tuoi-thuoc-dien-tiem-vaccine-COVID19/783421.vnp (accessed on 1 April 2022).
- ILO. Viet Nam National Child Labour Survey 2018—Key Findings. 2020. Available online: https://www.ilo.org/wcmsp5/groups/public/---asia/---ro-bangkok/---ilo-hanoi/documents/publication/wcms_764357.pdf (accessed on 1 March 2022).
- CDC. Myocarditis and Pericarditis after mRNA COVID-19 Vaccination. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html (accessed on 1 April 2022).
- BBC. Thanh Hoa: 4 Deaths after Receiving Vero Cell Vaccine. 2021. Available online: https://www.bbc.com/vietnamese/59398026 (accessed on 1 December 2021).
- BBC. Thanh Hoa: 86 Students were Hospitalized after Receiving Pfizer Vaccine: 2021. Available online: https://www.bbc.com/vietnamese/vietnam-59404925 (accessed on 1 December 2021).
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.A.; Sa’At, N.; Sidik, T.M.I.T.A.B.; Joo, L.C. Sample Size Guidelines for Logistic Regression from Observational Studies with Large Population: Emphasis on the Accuracy Between Statistics and Parameters Based on Real Life Clinical Data. Malays. J. Med Sci. 2018, 25, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Van Smeden, M.; Moons, K.G.; de Groot, J.A.; Collins, G.S.; Altman, D.G.; Eijkemans, M.J.; Reitsma, J.B. Sample Size for Binary Logistic Prediction Models: Beyond Events per Variable Criteria. Stat. Methods Med. Res. 2019, 28, 2455–2474. [Google Scholar] [CrossRef]
- Singh, A.S.; Masuku, M.B. Sampling Techniques & Determination of Sample Size in Applied Statistics Research: An Overview. Int. J. Econ. Commer. Manag. 2014, 2, 1–22. [Google Scholar]
- Acharya, A.S.; Prakash, A.; Saxena, P.; Nigam, A. Sampling: Why And How of It. Indian J. Med. Spec. 2013, 4, 330–333. [Google Scholar] [CrossRef]
- GSO. Social-Economic Zone n.d. Available online: http://portal.thongke.gov.vn/khodulieuldvl/MetaData.aspx?Mct=3&NameBar= (accessed on 1 March 2022).
- Wooldridge, J. Introductory Econometrics: A Modern Approach, 5th ed.; Cengage Learning: Mason, OH, USA, 2012. [Google Scholar]
- Kessels, R.; Luyten, J.; Tubeuf, S. Willingness to get vaccinated against COVID19 and attitudes toward vaccination in general. Vaccine 2021, 39, 4716–4722. [Google Scholar] [CrossRef]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Kelly, B.J.; Southwell, B.G.; McCormack, L.A.; Bann, C.M.; MacDonald, P.D.M.; Frasier, A.M.; Bevc, C.A.; Brewer, N.T.; Squiers, L.B. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect. Dis. 2021, 21, 338. [Google Scholar] [CrossRef]
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef]
- Abedin, M.; Islam, M.A.; Rahman, F.N.; Reza, H.M.; Hossain, M.Z.; Arefin, A.; Hossain, A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS ONE 2021, 16, e0250495. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2020, 21, 318–319. [Google Scholar] [CrossRef]
- Al-Mistarehi, A.-H.; Kheirallah, K.A.; Yassin, A.; Alomari, S.; Aledrisi, M.K.; Ata, E.M.B.; Hammad, N.H.; Khanfar, A.N.; Ibnian, A.M.; Khassawneh, B.Y. Determinants of the willingness of the general population to get vaccinated against COVID-19 in a developing country. Clin. Exp. Vaccine Res. 2020, 10, 171–182. [Google Scholar] [CrossRef]
- Liu, R.; Li, G.M. Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM-Popul. Health 2021, 15, 100896. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Willingness to Vaccinate Against COVID-19 in the U.S.: Representative Longitudinal Evidence From April to October 2020. Am. J. Prev. Med. 2021, 60, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Kourlaba, G.; Kourkouni, E.; Maistreli, S.; Tsopela, C.-G.; Molocha, N.-M.; Triantafyllou, C.; Koniordou, M.; Kopsidas, I.; Chorianopoulou, E.; Maroudi-Manta, S.; et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob. Heal. Res. Policy 2021, 6, 3. [Google Scholar] [CrossRef]
- Chew, N.W.; Cheong, C.; Kong, G.; Phua, K.; Ngiam, J.N.; Tan, B.Y.; Wang, B.; Hao, F.; Tan, W.; Han, X.; et al. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int. J. Infect. Dis. 2021, 106, 52–60. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; Van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Kawata, K.; Nakabayashi, M. Determinants of COVID-19 vaccine preference: A survey study in Japan. SSM-Popul. Health 2021, 15, 100902. [Google Scholar] [CrossRef]
- Bagateli, L.E.; Saeki, E.Y.; Fadda, M.; Agostoni, C.; Marchisio, P.; Milani, G.P. COVID-19 Vaccine Hesitancy among Parents of Children and Adolescents Living in Brazil. Vaccines 2021, 9, 1115. [Google Scholar] [CrossRef]
- Teasdale, C.A.; Borrell, L.N.; Kimball, S.; Rinke, M.L.; Rane, M.; Fleary, S.A.; Nash, D. Plans to Vaccinate Children for Coronavirus Disease 2019: A Survey of United States Parents. J. Pediatr. 2021, 237, 292–297. [Google Scholar] [CrossRef]
- Yılmaz, M.; Sahin, M.K. Parents’ willingness and attitudes concerning the COVID-19 vaccine: A cross-sectional study. Int. J. Clin. Pr. 2021, 75, e14364. [Google Scholar] [CrossRef]
- Teasdale, C.A.; Borrell, L.N.; Shen, Y.; Kimball, S.; Rinke, M.L.; Fleary, S.A.; Nash, D. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine 2021, 39, 5082–5086. [Google Scholar] [CrossRef]
- Babicki, M.; Pokorna-Kałwak, D.; Doniec, Z.; Mastalerz-Migas, A. Attitudes of Parents with Regard to Vaccination of Children against COVID-19 in Poland. A Nationwide Online Survey. Vaccines 2021, 9, 1192. [Google Scholar] [CrossRef]
- Duong, A.H.; Antriyandarti, E. COVID-19 Vaccine Acceptance among ASEAN Countries: Does the Pandemic Severity Really Matter? Vaccines 2022, 10, 222. [Google Scholar] [CrossRef]
- VNVC. 11 Vulnerable Groups That Are Prioritized for COVID-19 Vaccination in Vietnam. 2021. Available online: https://vnvc.vn/doi-tuong-nao-duoc-uu-tien-tiem-vac-xin-COVID-19/ (accessed on 1 August 2021).
- CDC. People with Certain Medical Conditions. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 1 July 2021).
- Ma, L.; Yang, J.; Zhang, T.; Han, X.; Huang, Q.; Yang, Y.; Feng, L.; Yang, W.; Wang, C. Willingness toward COVID-19 vaccination, coadministration with other vaccines and receive a COVID-19 vaccine booster: A cross-sectional study on the guardians of children in China. Hum. Vaccines Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef]
- Sun, X.; Shi, Y.; Zeng, Q.; Wang, Y.; Du, W.; Wei, N.; Xie, R.; Chang, C. Determinants of health literacy and health behavior regarding infectious respiratory diseases: A pathway model. BMC Public Heal. 2013, 13(1), 1–8. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef] [PubMed]
- Alin, A. Multicollinearity. WIREs Comput. Stat. 2010, 2, 370–374. [Google Scholar] [CrossRef]
- Chong, I.-G.; Jun, C.-H. Performance of some variable selection methods when multicollinearity is present. Chemom. Intell. Lab. Syst. 2005, 78, 103–112. [Google Scholar] [CrossRef]
- Daoud, J.I. Multicollinearity And Regression Analysis. J. Phys. Conf. Ser. 2017, 949, 012009. [Google Scholar] [CrossRef]
- Farrar, D.E.; Glauber, R.R. Multicollinearity in Regression Analysis: The Problem Revisited. Rev. Econ. Stat. 1967, 49, 92. [Google Scholar] [CrossRef]
- Graham, M.H. Confronting Multicollinearity In Ecological Multiple Regression. Ecology 2003, 84, 2809–2815. [Google Scholar] [CrossRef]
- Mansfield, E.R.; Helms, B.P. Detecting Multicollinearity. Am. Stat. 1982, 36, 158. [Google Scholar] [CrossRef]
- Schroeder, M.A.; Lander, J.; Levine-Silverman, S. Diagnosing and Dealing with Multicollinearity. West. J. Nurs. Res. 1990, 12, 175–187. [Google Scholar] [CrossRef]
- Bascle, G. Controlling for endogeneity with instrumental variables in strategic management research. Strat. Organ. 2008, 6, 285–327. [Google Scholar] [CrossRef]
- Semadeni, M.; Withers, M.C.; Trevis Certo, S. The perils of endogeneity and instrumental variables in strategy research: Understanding through simulations. Strateg. Manag. J. 2014, 35, 1070–1079. [Google Scholar] [CrossRef]
- Ullah, S.; Zaefarian, G.; Ullah, F. How to use instrumental variables in addressing endogeneity? A step-by-step procedure for non-specialists. Elsevier 2021, A1–A6. [Google Scholar] [CrossRef]
- Fingleton, B.; Le Gallo, J. Endogeneity in a spatial context: Properties of estimators. In Progress in Spatial Analysis; Springer: Berlin/Heidelberg, Germany, 2010; pp. 59–73. [Google Scholar] [CrossRef]
- Kelejian, H.H. Two-Stage Least Squares and Econometric Systems Linear in Parameters but Nonlinear in the Endogenous Variables. J. Am. Stat. Assoc. 1971, 66, 373–374. [Google Scholar] [CrossRef]
- Terza, J.V.; Basu, A.; Rathouz, P.J. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. J. Health Econ. 2008, 27, 531–543. [Google Scholar] [CrossRef]
- Cavanaugh, J.E. Unifying the derivations for the Akaike and corrected Akaike information criteria. Stat. Probab. Lett. 1997, 33, 201–208. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Shibata, R. Selection of the order of an autoregressive model by Akaike’s information criterion. Biometrika 1976, 63, 117–126. [Google Scholar] [CrossRef]
- Wesselink, A.K.; E Hatch, E.; Rothman, K.J.; Wang, T.R.; Willis, M.D.; Yland, J.; Crowe, H.M.; Geller, R.J.; Willis, S.K.; Perkins, R.B.; et al. A Prospective Cohort Study of COVID-19 Vaccination, SARS-CoV-2 Infection, and Fertility. Am. J. Epidemiol. 2022, 191, 1383–1395. [Google Scholar] [CrossRef]
- Goldman, R.D.; Bone, J.N.; Gelernter, R.; Krupik, D.; Ali, S.; Mater, A.; Thompson, G.C.; Yen, K.; Griffiths, M.A.; Klein, A.; et al. National COVID-19 vaccine program progress and parents’ willingness to vaccinate their children. Hum. Vaccines & Immunother. 2021, 17, 4889–4895. [Google Scholar] [CrossRef]
- Leng, A.; Maitland, E.; Wang, S.; Nicholas, S.; Liu, R.; Wang, J. Individual preferences for COVID-19 vaccination in China. Vaccine 2021, 39, 247–254. [Google Scholar] [CrossRef]
- Kuodi, P.; Gorelik, Y.; Zayyad, H.; Wertheim, O.; Wiegler, K.B.; Jabal, K.A.; Dror, A.A.; Nazzal, S.; Glikman, D.; Edelstein, M. Association between BNT162b2 Vaccination and Reported Incidence of Post-COVID-19 Symptoms: Cross-Sectional Study 2020-21, Israel. npj Vaccines 2022, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Duong, A.H.; Antriyandarti, E. The Willingness to get Vaccinated Against SARS-CoV-2 Virus among Southeast Asian Countries: Does the Vaccine Brand Matter? Appl. Res. Qual. Life 2022, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Jeewandara, C.; Fernando, S.; Pushpakumara, P.D.; Ramu, S.T.; Kamaladasa, A.; Gunasekara, B.; Aberathna, I.S.; Kuruppu, H.; Ranasinghe, T.; Dayarathne, S.; et al. Immune responses following the first dose of the Sputnik V (Gam-COVID-Vac). Sci. Rep. 2022, 12, 1727. [Google Scholar] [CrossRef] [PubMed]
- CDC. Science Brief: SARS-CoV-2 Infection-induced and Vaccine-induced Immunity. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/vaccine-induced-immunity.html (accessed on 1 May 2022).
- WHO. The Oxford/AstraZeneca (ChAdOx1-S [recombinant] Vaccine) COVID-19 Vaccine: What You Need To Know. 2022. Available online: https://www.who.int/news-room/feature-stories/detail/the-oxford-astrazeneca-COVID-19-vaccine-what-you-need-to-know (accessed on 1 June 2022).
- WHO. The Sinopharm COVID-19 Vaccine: What You Need To Know. 2022. Available online: https://www.who.int/news-room/feature-stories/detail/the-sinopharm-COVID-19-vaccine-what-you-need-to-know (accessed on 1 June 2022).
- WHO. Interim Recommendations for Use of The Inactivated COVID-19 Vaccine, CoronaVac, Developed by Sinovac. 2022. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjm5dnd7sj4AhUFDt4KHXnxD7oQFnoECAIQAQ&url=https%3A%2F%2Fapps.who.int%2Firis%2Frest%2Fbitstreams%2F1413991%2Fretrieve&usg=AOvVaw0Fs4lMK1_Glqvf1Jql0mfO (accessed on 1 May 2022).
- WHO. The Janssen Ad26.COV2.S COVID-19 Vaccine: What You Need To Know. 2022. Available online: https://www.who.int/news-room/feature-stories/detail/the-j-j-COVID-19-vaccine-what-you-need-to-know (accessed on 1 June 2022).
- WHO. The Moderna COVID-19 (mRNA-1273) Vaccine: What You Need To Know. 2022. Available online: https://www.who.int/news-room/feature-stories/detail/the-moderna-COVID-19-mrna-1273-vaccine-what-you-need-to-know (accessed on 1 June 2022).
- Alley, S.J.; Stanton, R.; Browne, M.; To, Q.G.; Khalesi, S.; Williams, S.L.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. As the Pandemic Progresses, How Does Willingness to Vaccinate against COVID-19 Evolve? Int. J. Environ. Res. Public Health 2021, 18, 797. [Google Scholar] [CrossRef]
- Walsh, J.C.; Comar, M.; Folan, J.; Williams, S.; Kola-Palmer, S. The psychological and behavioural correlates of COVID-19 vaccine hesitancy and resistance in Ireland and the UK. Acta Psychol. 2022, 225, 103550. [Google Scholar] [CrossRef]
- Toan Dang. Vietnam’s Public Loudspeaker System: A Means of Communication To Combat COVID-19. 2020. Available online: https://www.newmandala.org/vietnams-public-loudspeaker-system-a-means-of-communication-to-combat-COVID-19/ (accessed on 1 September 2021).
- WHO. Coronavirus Disease (COVID-19): Herd Immunity, Lockdowns And COVID-19. 2020. Available online: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-COVID-19 (accessed on 1 April 2022).
- Wise, J. COVID-19: Omicron infection is poor booster to immunity, study finds. BMJ 2022, 377, o1474. [Google Scholar] [CrossRef]
- FDA. Coronavirus (COVID-19) Update: FDA Authorizes Moderna, Pfizer-BioNTech Bivalent COVID-19 Vaccines for Use as a Booster Dose. 2022. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-COVID-19-update-fda-authorizes-moderna-pfizer-biontech-bivalent-COVID-19-vaccines-use (accessed on 1 September 2022).
- World Economic Forum. Needle-free Injections Could Become A Reality, Thanks to Lasers And The ‘Bubble Gun'. 2021. Available online: https://www.weforum.org/agenda/2021/10/new-technology-could-allow-you-to-have-a-needle-free-injection/ (accessed on 1 November 2021).
- Armitage, H. COVID-19 Nasal Spray Vaccine in The Works at Stanford Medicine 2021. Available online: https://med.stanford.edu/news/all-news/2021/11/effort-to-develop-COVID-vaccine-nasal-spray.html (accessed on 1 December 2021).
| Variable | Measures/ Units | Willing (%) | Hesitant (%) | Unwilling (%) |
|---|---|---|---|---|
| X11 | 0 | 4.5 | 1.8 | 3.4 |
| 1 | 95.5 | 98.2 | 96.6 | |
| X2 | 0 | 78.2 | 83.6 | 86.4 |
| 1 | 21.8 | 16.4 | 13.6 | |
| X3 | ≤2 24 | 83.9 | 86.6 | 86.9 |
| >3 2 | 16.1 | 13.4 | 13.1 | |
| X4 | ≤375 | 57.4 | 40.7 | 63.6 |
| >37 | 42.6 | 59.3 | 36.4 | |
| X5 | 0 | 20.0 | 10.6 | 5.7 |
| 1 | 80.0 | 89.4 | 94.3 | |
| X6 | 0 | 8.9 | 7.6 | 11.4 |
| 1 | 91.1 | 92.4 | 88.6 | |
| X7 | 0 | 22.4 | 27.1 | 18.2 |
| 1 | 77.6 | 72.9 | 81.8 | |
| X8 | 0 | 47.6 | 52.6 | 36.9 |
| 1 | 52.4 | 47.4 | 63.1 | |
| X9 | ≤26 | 60.7 | 57.1 | 51.1 |
| >2 | 39.3 | 42.9 | 48.9 | |
| X10 | 0 | 30.3 | 21.2 | 9.7 |
| 1 | 69.7 | 78.8 | 90.3 | |
| X11 | 0 | 4.9 | 5.0 | 4.0 |
| 1 | 95.1 | 95.0 | 96.0 | |
| X12 | 0 | 1.1 | 0.7 | 2.3 |
| 1 | 98.9 | 99.3 | 97.7 | |
| X13 | 0 | 1.0 | 0.5 | 0.6 |
| 1 | 99.0 | 99.5 | 99.4 | |
| X14 | 0 | 6.7 | 7.6 | 11.9 |
| 1 | 93.3 | 92.4 | 88.1 | |
| X15 | ≤67 | 89.1 | 85.3 | 86.9 |
| >6 | 10.9 | 14.7 | 13.1 | |
| X16 | ≤68 | 91.1 | 88.3 | 88.1 |
| >6 | 8.9 | 11.7 | 11.9 | |
| X17 | 0 | 6.1 | 10.1 | 8.0 |
| 1 | 93.9 | 89.9 | 92.0 | |
| X18 | 0 | 17.9 | 27.6 | 20.5 |
| 1 | 82.1 | 72.4 | 79.5 | |
| X19 | 0 | 17.5 | 29.9 | 21.6 |
| 1 | 82.5 | 70.1 | 78.4 | |
| X20 | 0 | 20.6 | 38.8 | 28.4 |
| 1 | 79.4 | 61.2 | 71.6 | |
| X21 | 0 | 41.4 | 72.2 | 66.5 |
| 1 | 58.6 | 27.8 | 33.5 | |
| X22 | 0 | 33.2 | 68.2 | 64.8 |
| 1 | 66.8 | 31.8 | 35.2 | |
| X23 | 0 | 54.7 | 56.4 | 61.4 |
| 1 | 45.3 | 43.6 | 38.6 | |
| X24 | 0 | 63.4 | 64.6 | 67.0 |
| 1 | 36.6 | 35.4 | 33.0 | |
| X25 | 0 | 94.0 | 90.2 | 90.9 |
| 1 | 6.0 | 9.8 | 9.1 | |
| X26 | 0 | 73.9 | 67.9 | 69.9 |
| 1 | 26.1 | 32.1 | 30.1 | |
| X27 | 0 | 58.2 | 59.4 | 57.4 |
| 1 | 41.8 | 40.6 | 42.6 | |
| X28 | 0 | 76.4 | 78.9 | 90.3 |
| 1 | 23.6 | 21.1 | 9.7 | |
| X29 | 0 | 6.4 | 6.3 | 10.2 |
| 1 | 93.6 | 93.7 | 89.8 | |
| X30 | 0 | 6.6 | 7.2 | 13.1 |
| 1 | 93.4 | 92.8 | 86.9 | |
| X31 | 0 | 73.7 | 79.8 | 93.8 |
| 1 | 26.3 | 20.2 | 6.3 | |
| X32 | 0 | 99.8 | 99.6 | 99.4 |
| 1 | 0.2 | 0.4 | 0.6 | |
| X33 | 0 | 71.9 | 71.3 | 72.2 |
| 1 | 28.1 | 28.7 | 27.8 | |
| X34 | 0 | 18.7 | 12.7 | 8.5 |
| 1 | 81.3 | 87.3 | 91.5 | |
| X35 | 0 | 43.6 | 38.5 | 42.0 |
| 1 | 56.4 | 61.5 | 58.0 | |
| X36 | ≤29 | 89.4 | 89.0 | 86.4 |
| >2 | 10.6 | 11.0 | 13.6 | |
| X37 | ≤210 | 69.4 | 71.5 | 71.0 |
| >2 | 30.6 | 28.5 | 29.0 | |
| X38 | ≤211 | 69.0 | 70.2 | 68.8 |
| >2 | 31.0 | 29.8 | 31.3 | |
| X39 | ≤312 | 79.8 | 79.5 | 74.4 |
| >3 | 20.2 | 20.5 | 25.6 | |
| X40 | 0 | 5.1 | 6.6 | 5.1 |
| 1 | 94.9 | 93.4 | 94.9 | |
| X41 | 0 | 75.6 | 79.8 | 80.1 |
| 1 | 24.4 | 20.2 | 19.9 | |
| X42 | 0 | 6.8 | 4.5 | 20.5 |
| 1 | 93.2 | 95.5 | 79.5 | |
| X43 | 0 | 25.9 | 43.7 | 58.5 |
| 1 | 74.1 | 56.3 | 41.5 |
| Vax 1 1 | Vax 2 2 | Vax 3 3 | Vax 4 4 | Vax 5 5 | |
|---|---|---|---|---|---|
| Willing | 48.8 6 | 18.1 | 8.6 | 2.0 | 4.5 |
| Hesitant | 44.8 | 23.0 | 10.1 | 1.2 | 2.8 |
| Unwilling | 42.6 | 25.0 | 8.5 | 4.5 | 2.3 |
| Variable | Sig.1 | OR 2 | Effect Size | |
|---|---|---|---|---|
| Group 1 | Intercept | 0.039 | 0.019 | 19.000 |
| 95% Confidence Interval | N/A 3 | N/A | N/A | |
| Gender of the respondent (X2, 1 = male) | 0.117 | 1.472 | 0.846 | |
| 95% Confidence Interval | 0.907 4 | 2.387 5 | 0.859 | |
| Age of the respondent (X4, years old) | 0.384 | 1.013 | 0.974 | |
| 95% Confidence Interval | 0.984 | 1.044 | 0.976 | |
| Residency of the respondent (X5, 1 = rural) | 0.404 | 0.741 | 1.528 | |
| 95% Confidence Interval | 0.367 | 1.497 | 1.559 | |
| The respondent was the main family income source (X7, 1 = yes) | 0.014 | 0.589 | 0.856 | |
| 95% Confidence Interval | 0.385 | 0.900 | 0.863 | |
| The respondent had savings (X8, 1 = yes) | 0.001 | 0.569 | 0.842 | |
| 95% Confidence Interval | 0.403 | 0.803 | 0.850 | |
| Education of the respondent (X10, 1 = tertiary or above) | 0.001 | 0.377 | 1.444 | |
| 95% Confidence Interval | 0.216 | 0.657 | 1.460 | |
| The respondents’ children were insured (X12, 1 = yes) | 0.047 | 3.703 | 1.028 | |
| 95% Confidence Interval | 1.016 | 13.497 | 1.185 | |
| Children vaccination habit (X14, 1 = yes) | 0.015 | 1.954 | 0.875 | |
| 95% Confidence Interval | 1.136 | 3.358 | 0.891 | |
| COVID-19 vaccination consultations sufficiency rated by the respondent (X22, 1 = sufficient) | 0.228 | 0.804 | 0.258 | |
| 95% Confidence Interval | 0.564 | 1.146 | 0.262 | |
| The respondent belonged to COVID-19 vaccine priority groups (X23, 1 = yes) | 0.090 | 1.344 | 0.931 | |
| 95% Confidence Interval | 0.955 | 1.891 | 0.941 | |
| The respondent’s knowledge of the ways to prevent SARS-CoV-2 (X28, 1 = sufficient) | 0.002 | 2.289 | 0.909 | |
| 95% Confidence Interval | 1.346 | 3.892 | 0.919 | |
| The respondent’s knowledge of COVID-19 fatality (X30, 1 = sufficient) | 0.219 | 1.390 | 0.928 | |
| 95% Confidence Interval | 0.822 | 2.350 | 0.946 | |
| The respondent’s knowledge of herd immunity (X31, 1 = sufficient) | 0.000 | 3.213 | 0.644 | |
| 95% Confidence Interval | 1.701 | 6.069 | 0.650 | |
| The respondent was infected with SARS-CoV-2 virus (X33, 1 = yes) | 0.108 | 1.361 | 0.906 | |
| 95% Confidence Interval | 0.935 | 1.982 | 0.916 | |
| The respondent had a closed person infected with SARS-CoV-2 virus (X34, 1 = yes) | 0.128 | 0.628 | 1.106 | |
| 95% Confidence Interval | 0.345 | 1.143 | 1.124 | |
| Children’s friends were fully vaccinated (X41, 1 = yes) | 0.243 | 1.283 | 0.920 | |
| 95% Confidence Interval | 0.845 | 1.948 | 0.933 | |
| Respondents were afraid of their children being infected (X42, 1 = yes) | 0.000 | 2.146 | 0.909 | |
| 95% Confidence Interval | 1.716 | 2.684 | 0.919 | |
| Children were afraid of needles (X43, 1 = yes) | 0.021 | 1.337 | 0.616 | |
| 95% Confidence Interval | 1.044 | 1.713 | 0.621 | |
| Group 2 | Intercept | 0.000 | 0.001 | 0.053 |
| 95% Confidence Interval | N/A | N/A | N/A | |
| Gender of the respondent (X2, 1 = male) | 0.020 | 1.740 | 1.182 | |
| 95% Confidence Interval | 1.090 | 2.778 | 1.164 | |
| Age of the respondent (X4, years old) | 0.008 | 1.040 | 1.027 | |
| 95% Confidence Interval | 1.010 | 1.070 | 1.025 | |
| Residency of the respondent (X5, 1 = rural) | 0.038 | 0.485 | 0.655 | |
| 95% Confidence Interval | 0.245 | 0.960 | 0.641 | |
| The respondent was the main family income source (X7, 1 = yes) | 0.078 | 0.688 | 1.168 | |
| 95% Confidence Interval | 0.454 | 1.043 | 1.159 | |
| The respondent had savings (X8, 1 = yes) | 0.022 | 0.676 | 1.188 | |
| 95% Confidence Interval | 0.484 | 0.945 | 1.177 | |
| Education of the respondent (X10, 1 = tertiary or above) | 0.000 | 0.261 | 0.692 | |
| 95% Confidence Interval | 0.152 | 0.450 | 0.685 | |
| Insured children (X12, 1 = yes) | 0.029 | 3.603 | 0.973 | |
| 95% Confidence Interval | 1.140 | 11.387 | 0.844 | |
| Children vaccination habit (X14, 1 = yes) | 0.003 | 2.233 | 1.143 | |
| 95% Confidence Interval | 1.323 | 3.768 | 1.122 | |
| COVID-19 vaccination consultations sufficiency rated by the respondent (X22, 1 = sufficient) | 0.000 | 3.116 | 3.876 | |
| 95% Confidence Interval | 2.216 | 4.381 | 3.823 | |
| The respondent belonged to COVID-19 vaccine priority groups (X23, 1 = yes) | 0.030 | 1.444 | 1.074 | |
| 95% Confidence Interval | 1.037 | 2.010 | 1.063 | |
| The respondent’s knowledge of the ways to prevent SARS-CoV-2 virus (X28, 1 = sufficient) | 0.001 | 2.517 | 1.100 | |
| 95% Confidence Interval | 1.495 | 4.237 | 1.089 | |
| The respondent’s knowledge of COVID-19 fatality (X30, 1 = sufficient) | 0.117 | 1.498 | 1.078 | |
| 95% Confidence Interval | 0.904 | 2.483 | 1.057 | |
| The respondent’s knowledge of herd immunity (X31, 1 = sufficient) | 0.000 | 4.991 | 1.553 | |
| 95% Confidence Interval | 2.669 | 9.336 | 1.538 | |
| The respondent was infected with SARS-CoV-2 virus (X33, 1 = yes) | 0.029 | 1.502 | 1.104 | |
| 95% Confidence Interval | 1.042 | 2.163 | 1.091 | |
| The respondent had a closed person infected with SARS-CoV-2 virus (X34, 1 = yes) | 0.057 | 0.568 | 0.904 | |
| 95% Confidence Interval | 0.317 | 1.017 | 0.890 | |
| Children’s friends were fully vaccinated (X41, 1 = yes) | 0.106 | 1.395 | 1.087 | |
| 95% Confidence Interval | 0.931 | 2.088 | 1.072 | |
| Respondents were afraid of their children being infected (X42, 1 = yes) | 0.000 | 2.361 | 1.100 | |
| 95% Confidence Interval | 1.908 | 2.922 | 1.089 | |
| Children were afraid of needles (X43, 1 = yes) | 0.000 | 2.169 | 1.622 | |
| 95% Confidence Interval | 1.706 | 2.757 | 1.609 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duong, A.H.; Duong, G.H.; Pham, H.T. The Willingness of Parents to Vaccinate Their Children Aged from Five to under Twelve Years with COVID-19 Vaccines between February and March 2022 in Vietnam. Vaccines 2022, 10, 1775. https://doi.org/10.3390/vaccines10111775
Duong AH, Duong GH, Pham HT. The Willingness of Parents to Vaccinate Their Children Aged from Five to under Twelve Years with COVID-19 Vaccines between February and March 2022 in Vietnam. Vaccines. 2022; 10(11):1775. https://doi.org/10.3390/vaccines10111775
Chicago/Turabian StyleDuong, An Hoai, Giang Huong Duong, and Hue Thi Pham. 2022. "The Willingness of Parents to Vaccinate Their Children Aged from Five to under Twelve Years with COVID-19 Vaccines between February and March 2022 in Vietnam" Vaccines 10, no. 11: 1775. https://doi.org/10.3390/vaccines10111775
APA StyleDuong, A. H., Duong, G. H., & Pham, H. T. (2022). The Willingness of Parents to Vaccinate Their Children Aged from Five to under Twelve Years with COVID-19 Vaccines between February and March 2022 in Vietnam. Vaccines, 10(11), 1775. https://doi.org/10.3390/vaccines10111775








