Assessment of Attitudes and Intentions towards COVID-19 Vaccines and Associated Factors among General Populations of Pakistan: A Cross-Sectional Study
Abstract
:1. Introduction
2. Subject and Methods
2.1. Participants and Study Design
2.2. Variables and Questionnaire Instruments
2.3. Information about Socio-Demographics
2.4. The Attitude towards COVID-19 Vaccines
2.5. The Intentions toward COVID-19 Vaccines
2.6. Operational Definitions
2.7. Dependent Variable
2.8. Independent Variable
2.9. Statistical Analysis
2.10. Consent to Participate
2.11. Ethical Approval
2.12. Results
Information about Socio-Demographics
3. The Attitude towards COVID-19 Vaccines
4. The Intentions toward COVID-19 Vaccines
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Islam, M.S.; Rahman, K.M.; Sun, Y.; Qureshi, M.O.; Abdi, I.; Chughtai, A.A.; Seale, H. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: A global analysis. Infect. Control Hosp. Epidemiol. 2020, 41, 1196–1206. [Google Scholar] [CrossRef]
- Yu, P.; Zhu, J.; Zhang, Z.; Han, Y. A Familial Cluster of Infection Associated With the 2019 Novel Coronavirus Indicating Possible Person-to-Person Transmission During the Incubation Period. J. Infect. Dis. 2020, 221, 1757–1761. [Google Scholar] [CrossRef]
- Imran, H.; Raja, D.; Grassly, N.; Wadood, M.Z.; Safdar, R.M.; O’Reilly, K.M. Routine immunization in Pakistan: Comparison of multiple data sources and identification of factors associated with vaccination. Int. Health 2018, 10, 84–91. [Google Scholar] [CrossRef]
- Ahmed, A.; Dujaili, J.; Sandhu, A.K.; Hashmi, F.K. Concerns of HIV-positive migrant workers in COVID-19 pandemic: A call for action. J. Glob. Health 2020, 10, 020342. [Google Scholar] [CrossRef]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T.A.; et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef]
- Pinna, C.; Kaewkungwal, J.; Hattasingh, W.; Swaddiwudhipong, W.; Methakulchart, R.; Moungsookjareoun, A.; Lawpoolsri, S. Evaluation of Immunization Services for Children of Migrant Workers Along Thailand–Myanmar Border: Compliance with Global Vaccine Action Plan (2011–2020). Vaccines 2020, 8, 68. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 April 2020).
- Wombwell, E.; Fangman, M.T.; Yoder, A.K.; Spero, D.L. Religious Barriers to Measles Vaccination. J. Commun. Health 2015, 40, 597–604. [Google Scholar] [CrossRef]
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef]
- McKee, C.; Bohannon, K. Exploring the Reasons Behind Parental Refusal of Vaccines. J. Pediatr. Pharmacol. Ther. 2016, 21, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Butt, M.; Mohammed, R.; Butt, E.; Butt, S.; Xiang, J. Why have immunization efforts in Pakistan failed to achieve global standards of vaccination uptake and infectious disease control? Risk Manag. Healthc. Policy 2020, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Jamal, D.; Zaidi, S.; Husain, S.; Orr, D.W.; Riaz, A.; Farrukhi, A.A.; Najmi, R. Low vaccination in rural Sindh, Pakistan: A case of refusal, ignorance or access? Vaccine 2020, 38, 4747–4754. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Sagara, I.; Ellis, R.D.; Dicko, A.; Niambele, M.B.; Kamate, B.; Guindo, O.; Sissokoa, M.S.; Fay, M.P.; Guindo, M.A.; Kante, O.; et al. A randomized and controlled Phase 1 study of the safety and immunogenicity of the AMA1-C1/Alhydrogel®+ CPG 7909 vaccine for Plasmodium falciparum malaria in semi-immune Malian adults. Vaccine 2009, 27, 7292–7298. [Google Scholar] [CrossRef]
- Ullah, I.; Khan, K.S.; Tahir, M.J.; Ahmed, A.; Harapan, H. Myths and conspiracy theories on vaccines and COVID-19: Potential effect on global vaccine refusals. Vacunas 2021, 22, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Naeem, S.B.; Bhatti, R. The COVID-19 ‘infodemic’: A new front for information professionals. Health Inf. Libr. J. 2020, 37, 233–239. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef]
- Palamenghi, L.; Barello, S.; Boccia, S.; Graffigna, G. Mistrust in biomedical research and vaccine hesitancy: The forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020, 35, 785–788. [Google Scholar] [CrossRef]
- Fadda, M.; Albanese, E.; Suggs, L.S. When a COVID-19 Vaccine Is Ready, Will We All Be Ready for It? Springer: Berlin/Heidelberg, Germany, 2020; pp. 711–712. [Google Scholar]
- Khan, Y.H.; Mallhi, T.H.; Alotaibi, N.H.; Alzarea, A.I.; Alanazi, A.S.; Tanveer, N.; Hashmi, F.K. Threat of COVID-19 Vaccine Hesitancy in Pakistan: The Need for Measures to Neutralize Misleading Narratives. Am. J. Trop. Med. Hyg. 2020, 103, 603–604. [Google Scholar] [CrossRef]
- WAoa. Available online: https://worldpopulationreview.com/countries/pakistan-population (accessed on 1 July 2021).
- rcAoa. Available online: http://www.raosoft.com/samplesize.html (accessed on 1 July 2021).
- Alle, Y.F.; Oumer, K.E. Attitude and associated factors of COVID-19 vaccine acceptance among health professionals in Debre Tabor Comprehensive Specialized Hospital, North Central Ethiopia; 2021: Cross-sectional study. VirusDisease 2021, 32, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. eClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- Omar, D.I.; Hani, B.M. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J. Infect. Public Health 2021, 14, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Wei, Z.; Zhu, F.; Pei, S.; Li, S.; Zhang, L.; Sun, X.; Wu, Y.; Liu, P.; Jit, M. Acceptance of and preference for COVID-19 vaccination in healthcare workers: A comparative analysis and discrete choice experiment. medRxiv 2022, 2020, 09.20060103. [Google Scholar]
- Magadmi, R.M.; Kamel, F.O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health 2021, 21, 1–8. [Google Scholar] [CrossRef]
- Riaz, A.; Husain, S.; Yousafzai, M.T.; Nisar, I.; Shaheen, F.; Mahesar, W.; Dal, S.M.; Omer, S.B.; Zaidia, S.; Ali, A. Reasons for non-vaccination and incomplete vac-cinations among children in Pakistan. Vaccine 2018, 36, 5288–5293. [Google Scholar] [CrossRef]
- Khattak, S.; Faheem, M.; Nawaz, B.; Khan, M.; Khan, N.H.; Ullah, N.; Khan, T.A.; Khan, R.U.; Haleem, K.S.; Ren, Z.-G.; et al. Knowledge, Attitude, and Perception of Cancer Patients towards COVID-19 in Pakistan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 7926. [Google Scholar] [CrossRef]
- Khattak, S.; Khan, M.; Usman, T.; Ali, J.; Wu, D.-X.; Jahangir, M.; Haleem, K.; Muhammad, P.; Rauf, M.A.; Saddique, K.; et al. Assessment of General Populations Knowledge, Attitude, and Perceptions Toward the Coronavirus Disease (COVID-19): A Cross-Sectional Study From Pakistan. Front. Med. 2021, 8, 747819. [Google Scholar] [CrossRef]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.J.; Strych, U.; Dor, A.; Fowler, E.F.; Motta, M. Correlates and disparities of COVID-19 vaccine hesitancy. Soc. Sci. Med. 2021, 272, 113638. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Chou, W.-Y.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef] [PubMed]
- Mannan, D.K.A.; Farhana, K.M. Knowledge, attitude and acceptance of a COVID-19 vaccine: A global cross-sectional study. Int. Res. J. Bus. Soc. Sci. 2020, 6. [Google Scholar] [CrossRef]
- Stojanovic, J.; Boucher, V.; Gagne, M.; Gupta, S.; Joyal-Desmarais, K.; Paduano, S.; Aburub, A.; Gorin, S.S.; Kassianos, A.; Ribeiro, P.; et al. Global Trends and Correlates of COVID-19 Vaccination Hesitancy: Findings from the iCARE Study. Vaccines 2021, 9, 661. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and in-vestigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Nazaroff, D. May Cause Side Effects: How Social Media Could Be Affecting COVID Vaccine Hesitancy New South Wales; UNSW: Sydney, Australia, 2021. [Google Scholar]
- Lipsitch, M.; Dean, N.E. Understanding COVID-19 vaccine efficacy. Science 2020, 370, 763–765. [Google Scholar] [CrossRef]
- Danchin, M.; Biezen, R.; Manski-Nankervis, J.-A.; Kaufman, J.; Leask, J. Preparing the public for COVID-19 vaccines: How can general practitioners build vaccine confidence and optimise uptake for themselves and their patients? Aust. J. Gen. Pract. 2020, 49, 625–629. [Google Scholar] [CrossRef]
- Seale, H.; Heywood, A.E.; Leask, J.; Sheel, M.; Durrheim, D.N.; Bolsewicz, K.; Kaur, R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect. Dis. 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Eastwood, K.; Durrheim, D.N.; Jones, A.; Butler, M. Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Aus-tralian public. Med. J. Aust. 2010, 192, 33–36. [Google Scholar] [CrossRef]
- Stojanovic, J.; Boucher, V.G.; Boyle, J.; Enticott, J.; Lavoie, K.L.; Bacon, S.L. COVID-19 Is Not the Flu: Four Graphs From Four Countries. Front. Public Health 2021, 9, 628479. [Google Scholar] [CrossRef]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- Woolf, K.; McManus, I.C.; Martin, C.A.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg. Health Eur. 2021, 9, 100180. [Google Scholar] [CrossRef] [PubMed]
- CDC. Centers for Disease Control and Prevention. Ways Health Departments Can Help Increase COVID-19 Vaccina-Tions. Available online: http://www.cdc.gov/vaccines/covid-19/health-departments/generate-vaccinations.html (accessed on 28 August 2022).
- CDC. National Center for Immunization and Respiratory Diseases (NCIRD). Available online: https://www.cdc.gov/ncird/index.html (accessed on 28 August 2022).
- OECD. Enhancing Public Trust in COVID-19 Vaccination: The Role of Governments. Available online: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-in-covid-19-vaccination-the-role-of-governments-eae0ec5a/ (accessed on 28 August 2022).
- Glanville, D. COVID-19 Vaccines: Development, Evaluation, Approval and Monitoring [Internet]. European Medicines Agency. 2020. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-development-evaluation-approval-monitoring (accessed on 28 August 2021).
- Meppelink, C.S.; Smit, E.G.; Fransen, M.L.; Diviani, N. “I was Right about Vaccination”: Confirmation Bias and Health Literacy in Online Health Information Seeking. J. Health Commun. 2019, 24, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Mindell, J.S.; Reynolds, L.; Cohen, D.; McKee, M. All in this together: The corporate capture of public health. BMJ 2012, 345, e8082. [Google Scholar] [CrossRef]
- Mondal, A. The importance of community engagement on COVID-19 vaccination strategy: Lessons from two California pilot programs. eClinicalMedicine 2021, 32, 100754. [Google Scholar] [CrossRef] [PubMed]



| S.No. | Variable | Frequency | Percentage (%) | |
|---|---|---|---|---|
| 1 | Gender | Male | 2703 | 61.54 |
| Female | 1683 | 38.32 | ||
| I prefer not to say | 6 | 0.14 | ||
| 2 | Age | 18–29 | 3277 | 74.61 |
| 30–49 | 1041 | 23.70 | ||
| Above 50 | 74 | 1.69 | ||
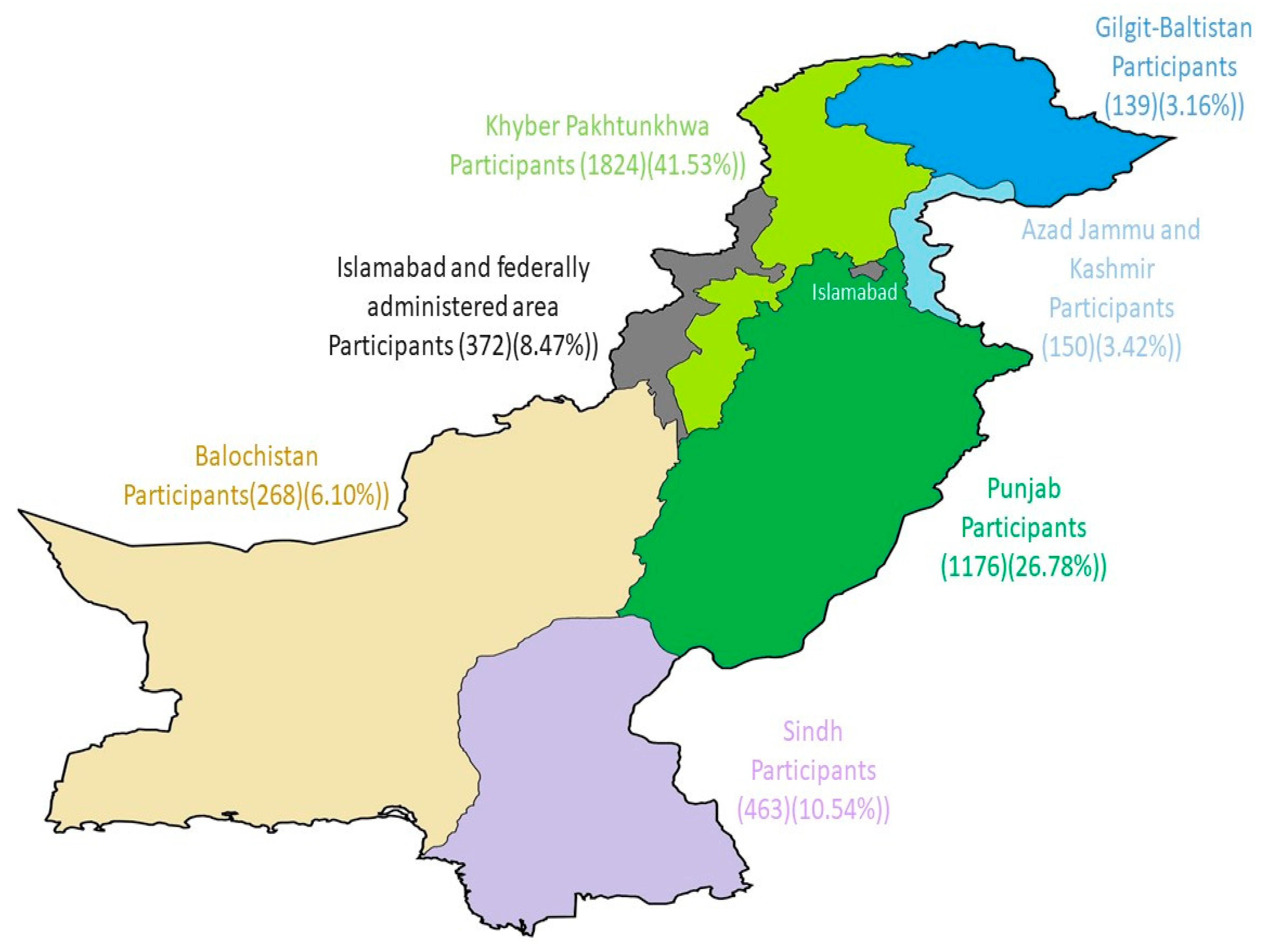
| 3 | Administrative Units | Khyber Pakhtunkhwa | 1824 | 41.53 |
| Punjab | 1176 | 26.78 | ||
| Sindh | 463 | 10.54 | ||
| Islamabad Capital Territory | 372 | 8.47 | ||
| Baluchistan | 268 | 6.10 | ||
| Azad Jammu and Kashmir | 150 | 3.42 | ||
| Gilgit-Baltistan | 139 | 3.16 | ||
| 4 | Residence | Urban | 2830 | 64.44 |
| Rural | 1562 | 35.56 | ||
| 5 | Marital status | Single | 3349 | 76.25 |
| Married | 1043 | 23.75 | ||
| 6 | Chronic disease | No chronic disease | 3547 | 80.76 |
| Cardiac disease | 206 | 4.69 | ||
| Hypertension | 174 | 3.96 | ||
| Overweight/obesity | 168 | 3.83 | ||
| Others | 132 | 3.00 | ||
| Asthma or respiratory disease | 108 | 2.46 | ||
| Kidney or liver disease | 51 | 1.16 | ||
| Cancer | 6 | 0.14 | ||
| 7 | Employment Status | Student | 2994 | 68.17 |
| Full-Time | 850 | 19.35 | ||
| Part-Time | 180 | 4.10 | ||
| Unemployed | 162 | 3.69 | ||
| Housewife | 114 | 2.60 | ||
| Retired | 74 | 1.68 | ||
| Worker | 18 | 0.41 | ||
| 8 | Education | Graduate | 1718 | 39.12 |
| College | 1537 | 34.99 | ||
| Postgraduate | 1119 | 25.48 | ||
| High School | 18 | 0.41 |
| Q.No | Questions/Variables | Values | Frequency | Percentage |
|---|---|---|---|---|
| 1 | Have you had a flu vaccination? | Never | 3102 | 70.62 |
| Yes last year | 486 | 11.07 | ||
| Yes (a long time ago) | 450 | 10.25 | ||
| Yes this year | 282 | 6.42 | ||
| Yes every year | 72 | 1.64 | ||
| No | 2337 | 53.22 | ||
| Yes | 1851 | 42.14 | ||
| Don’t know | 204 | 4.64 | ||
| 2 | Has any family member had COVID-19? | Yes | 2219 | 50.52 |
| No | 2083 | 47.43 | ||
| Don’t know | 90 | 2.05 | ||
| 3 | Does the ministry of health provide adequate information about COVID-19 vaccines? | Yes | 3365 | 76.62 |
| No | 541 | 12.32 | ||
| Don’t know | 486 | 11.06 | ||
| 4 | Intentions to receive the COVID-19 vaccine | willing to take the vaccine | 3555 | 57.39 |
| hesitated to take the vaccine | 821 | 18.69 | ||
| not willing to take the vaccine | 216 | 4.92 | ||
| 5 | COVID-19 vaccine preferences | Sinopharm and Sinovac vaccine | 1610 | 36.66 |
| Pfizer vaccine | 1574 | 35.84 | ||
| I don’t have enough information to decide | 468 | 10.65 | ||
| AstraZeneca | 320 | 7.29 | ||
| Moderna vaccine | 288 | 6.55 | ||
| Sputnik V vaccine | 132 | 3.01 | ||
| 6 | I do not believe the vaccine works | Strongly disagree | 1275 | 29.02 |
| Disagree | 1425 | 32.45 | ||
| Neutral | 1194 | 27.19 | ||
| Agree | 288 | 6.56 | ||
| Strongly agree | 210 | 4.78 |
| S.No. | Variable | Categories | Positive Frequency (%age) | Negative Frequency (%age) | Chi-Square | Significance (p-Value) |
|---|---|---|---|---|---|---|
| 1 | Gender | Male | 1863 (68.92) | 840 (31.08) | 112.40 | 0.000 |
| Female | 905 (53.77) | 778 (46.23) | ||||
| I prefer not to say | 0 (0) | 6 (100) | ||||
| 2 | Age | 18–29 | 1906 (58.16) | 1371 (41.84) | 138.10 | 0.000 |
| 30–49 | 794 (76.27) | 247 (23.73) | ||||
| Above 50 | 68 (91.89) | 6 (8.11) | ||||
| 3 | Administrative Units | Khyber Pakhtunkhwa | 1038 (56.91) | 786 (43.09) | 505.98 | 0.000 |
| Punjab | 654 (55.61) | 522 (44.39) | ||||
| Sindh | 463 (100) | 0 (0) | ||||
| Islamabad Capital Territory | 282 (75.81) | 90 (24.19) | ||||
| Baluchistan | 111 (41.42) | 157 (58.58) | ||||
| Azad Jammu and Kashmir | 150 (100) | 0 (0) | ||||
| Gilgit-Baltistan | 70 (50.36) | 69 (49.64) | ||||
| 4 | Residence | Urban | 1641 (57.99) | 86.66 | 0.000 | |
| Rural | 1127 (72.15) | 435 (27.85) | ||||
| 5 | Marital status | Single | 2074 (61.93) | 1275 (38.07) | 7.25 | 0.0071 |
| Married | 694 (66.54) | 349 (33.46) | ||||
| 6 | Chronic disease | No chronic disease | 2118 (59.71) | 1429 (40.29) | 410.78 | 0.000 |
| Cardiac disease | 206 (100) | 0 (0) | ||||
| Hypertension | 174 (100) | 0 (0) | ||||
| Overweight/obesity | 36 (21.43) | 132 (78.57) | ||||
| Others | 102 (77.27) | 30(22.73) | ||||
| Asthma or respiratory disease | 96 (88.89) | 12 (11.11) | ||||
| Kidney or liver disease | 30 (58.82) | 21 (41.18) | ||||
| Cancer | 6 (100) | 0 (0) | ||||
| 7 | Employment Status | Student | 1923 (64.23) | 1071 (35.77) | 256.60 | 0.000 |
| Full-Time | 531 (62.47) | 319 (37.53) | ||||
| Part-Time | 156 (86.67) | 24 (13.33) | ||||
| Unemployed | 72 (44.44) | 90 (55.56) | ||||
| Housewife | 6 (5.26) | 108 (94.74) | ||||
| Retired | 62 (83.78) | 12 (16.22) | ||||
| Worker | 18 (100) | 0 (0) | ||||
| 8 | Education | Graduate | 1004 (58.44) | 714 (41.56) | 170.86 | 0.000 |
| College | 1162 (75.60) | 375 (24.40) | ||||
| Postgraduate | 590 (52.73) | 529 (47.27) | ||||
| High School | 12 (66.67) | 6 (33.33) |
| Q.No. | Questions/Variables | Values | Frequency | Percentage |
|---|---|---|---|---|
| 1 | I feel safe after being vaccinated against COVID-19 | Agree | 1731 | 39.41 |
| Neutral | 1462 | 33.29 | ||
| Strongly agree | 947 | 21.56 | ||
| Disagree | 174 | 3.96 | ||
| Strongly disagree | 78 | 1.78 | ||
| 2 | I can feel that my family is protected after getting vaccinated against COVID 19 | Agree | 1534 | 34.92 |
| Neutral | 1462 | 33.29 | ||
| Strongly agree | 892 | 20.31 | ||
| Disagree | 432 | 9.84 | ||
| Strongly disagree | 72 | 1.64 | ||
| 3 | I can rely on COVID-19 vaccines to stop the pandemic | Neutral | 1726 | 39.3 |
| Agree | 1654 | 37.66 | ||
| Strongly agree | 640 | 14.57 | ||
| Disagree | 252 | 5.74 | ||
| Strongly disagree | 120 | 2.73 | ||
| 4 | Although most vaccines appear to be safe, there may be problems that we have not yet discovered | Agree | 2225 | 50.66 |
| Neutral | 1135 | 25.84 | ||
| Strongly agree | 612 | 13.93 | ||
| Disagree | 360 | 8.2 | ||
| Strongly disagree | 60 | 1.37 | ||
| 5 | COVID-19 vaccines can cause unforeseen problems in some population groups. | Agree | 1671 | 38.05 |
| Neutral | 1528 | 34.79 | ||
| Disagree | 516 | 11.75 | ||
| Strongly disagree | 383 | 8.72 | ||
| Strongly agree | 294 | 6.69 | ||
| 6 | I worry about the unknown effects of vaccines in the future. | Agree | 1747 | 39.78 |
| Neutral | 1377 | 31.35 | ||
| Disagree | 684 | 15.57 | ||
| Strongly agree | 354 | 8.06 | ||
| Strongly disagree | 230 | 5.24 | ||
| 7 | Authorities promote vaccination for financial gain, not for people’s health. | Neutral | 1593 | 36.27 |
| Disagree | 1064 | 24.23 | ||
| Agree | 802 | 18.26 | ||
| Strongly disagree | 741 | 16.87 | ||
| Strongly agree | 192 | 4.37 | ||
| 8 | COVID-19 vaccination programs are a big con | Agree | 1488 | 33.88 |
| Neutral | 1254 | 28.55 | ||
| Disagree | 960 | 21.86 | ||
| Strongly disagree | 486 | 11.07 | ||
| Strongly agree | 204 | 4.64 | ||
| 9 | I am worried about the rapid development of the COVID vaccine | Agree | 1384 | 31.51 |
| Neutral | 1334 | 30.37 | ||
| Disagree | 1098 | 25 | ||
| Strongly disagree | 336 | 7.66 | ||
| Strongly agree | 240 | 5.46 | ||
| 10 | I have had a prior reaction to other vaccines, and I am worried about a reaction to COVID vaccination | Disagree | 1307 | 29.76 |
| Neutral | 1251 | 28.49 | ||
| Agree | 1044 | 23.77 | ||
| Strongly disagree | 568 | 12.93 | ||
| Strongly agree | 222 | 5.05 | ||
| 11 | I do not get vaccinated because of a fear of needles | Disagree | 1571 | 35.76 |
| Strongly disagree | 1557 | 35.45 | ||
| Neutral | 714 | 16.26 | ||
| Agree | 490 | 11.16 | ||
| Strongly agree | 60 | 1.37 | ||
| 12 | Natural immunity lasts longer than COVID-19 vaccination. | Agree | 1698 | 38.65 |
| Neutral | 1372 | 31.24 | ||
| Disagree | 674 | 15.35 | ||
| Strongly agree | 486 | 11.07 | ||
| Strongly disagree | 162 | 3.69 | ||
| 13 | Natural exposure to novel corona gives the safest protection | Neutral | 1615 | 36.77 |
| Disagree | 1177 | 26.8 | ||
| Agree | 1140 | 25.96 | ||
| Strongly agree | 286 | 6.51 | ||
| Strongly disagree | 174 | 3.96 | ||
| 14 | Being exposed to diseases naturally is safer for the immune system than being exposed through vaccination | Agree | 1288 | 29.33 |
| Neutral | 1270 | 28.92 | ||
| Disagree | 968 | 22.04 | ||
| Strongly agree | 482 | 10.97 | ||
| Strongly disagree | 384 | 8.74 |
| S.No. | Variable | Categories | Positive Frequency (%age) | Negative Frequency (%age) | Chi-Square | Significance (p-Value) |
|---|---|---|---|---|---|---|
| 1 | Gender | Male | 2535 (93.78) | 168 (6.22) | 1.84 | 0.390 |
| Female | 1563 (92.87) | 120 (7.13) | ||||
| Prefer not to say | 6 (100) | 0 (0) | ||||
| 2 | Age | 18–29 | 3031 (92.49) | 246 (7.51) | 20.83 | 0.000 |
| 30–49 | 999 (95.97) | 42 (4.03) | ||||
| Above 50 | 74 (100) | 0 (0) | ||||
| 3 | Administrative Units | Khyber Pakhtunkhwa | 1644 (90.13) | 180 (9.87) | 354.45 | 0.000 |
| Punjab | 1170 (99.49) | 6 (0.51) | ||||
| Sindh | 463 (100) | 0 (0) | ||||
| Islamabad Capital Territory | 282 (75.81) | 90 (24.19) | ||||
| Baluchistan | 268 (100) | 0 (0) | ||||
| Azad Jammu and Kashmir | 150 (100) | 0 (0) | ||||
| Gilgit-Baltistan | 127 (91.37) | 12 (8.63) | ||||
| 4 | Residence | Urban | 2620 (92.58) | 210 (7.42) | 9.67 | 0.0019 |
| Rural | 1484 (95.01) | 78 (4.99) | ||||
| 5 | Marital status | Single | 3085 (92.12) | 264 (7.88) | 40.44 | 0.000 |
| Married | 1019 (97.70) | 24 (2.30) | ||||
| 6 | Chronic disease | No chronic disease | 3295 (92.90) | 252 (7.10) | 106.01 | 0.000 |
| Cardiac disease | 206 (100) | 0 (0) | ||||
| Hypertension | 174 (100) | 0 (0) | ||||
| Overweight/obesity | 156 (92.86) | 12 (7.14) | ||||
| Others | 126 (95.45) | 6 (4.55) | ||||
| Asthma or respiratory disease | 108 (100) | 0 (0) | ||||
| Kidney or liver disease | 33 (64.71) | 18 (35.29) | ||||
| Cancer | 6 (100) | 0 (0) | ||||
| 7 | Employment Status | Student | 2784 (92.99) | 210 (7.01) | 112.36 | 0.000 |
| Full-Time | 838 (98.59) | 12 (1.41) | ||||
| Part-Time | 150 (83.33) | 30 (16.67) | ||||
| Unemployed | 132 (81.48) | 30 (18.52) | ||||
| Housewife | 108 (94.74) | 6 (5.26) | ||||
| Retired | 74 (100) | 0 (0) | ||||
| Worker | 18 (100) | 0 (0) | ||||
| 8 | Education | Graduate | 1664 (96.86) | 54 (3.14) | 56.11 | 0.000 |
| College | 1399 (91.02) | 138 (8.98) | ||||
| Postgraduate | 1023 (91.42) | 96 (8.58) | ||||
| High School | 18 (100) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khattak, S.; Idrees, M.; Iqbal, H.I.; Khan, M.; Assad, N.; Khan, M.N.; Yousaf, M.T.; Farooq, M.; Yang, C.-Y.; Wu, D.-D.; et al. Assessment of Attitudes and Intentions towards COVID-19 Vaccines and Associated Factors among General Populations of Pakistan: A Cross-Sectional Study. Vaccines 2022, 10, 1583. https://doi.org/10.3390/vaccines10101583
Khattak S, Idrees M, Iqbal HI, Khan M, Assad N, Khan MN, Yousaf MT, Farooq M, Yang C-Y, Wu D-D, et al. Assessment of Attitudes and Intentions towards COVID-19 Vaccines and Associated Factors among General Populations of Pakistan: A Cross-Sectional Study. Vaccines. 2022; 10(10):1583. https://doi.org/10.3390/vaccines10101583
Chicago/Turabian StyleKhattak, Saadullah, Muhammad Idrees, Hafiza Iqra Iqbal, Maqbool Khan, Nasir Assad, Muhammad Naeem Khan, Muhammad Tufail Yousaf, Muhammad Farooq, Chang-Yong Yang, Dong-Dong Wu, and et al. 2022. "Assessment of Attitudes and Intentions towards COVID-19 Vaccines and Associated Factors among General Populations of Pakistan: A Cross-Sectional Study" Vaccines 10, no. 10: 1583. https://doi.org/10.3390/vaccines10101583
APA StyleKhattak, S., Idrees, M., Iqbal, H. I., Khan, M., Assad, N., Khan, M. N., Yousaf, M. T., Farooq, M., Yang, C.-Y., Wu, D.-D., & Ji, X.-Y. (2022). Assessment of Attitudes and Intentions towards COVID-19 Vaccines and Associated Factors among General Populations of Pakistan: A Cross-Sectional Study. Vaccines, 10(10), 1583. https://doi.org/10.3390/vaccines10101583









