Neuromodulation for Pelvic and Urogenital Pain
Abstract
1. Introduction
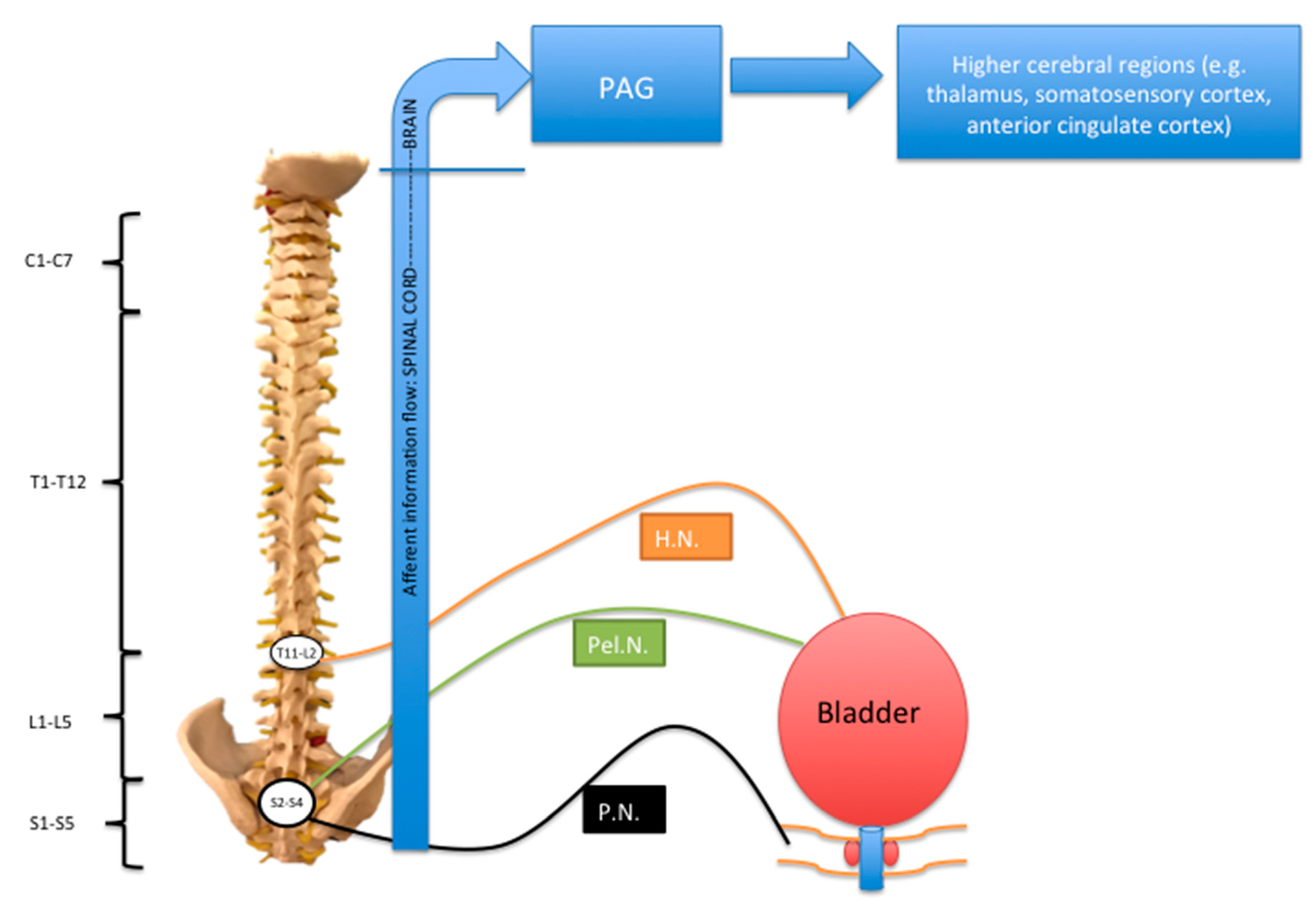
1.1. Pelvic Anatomy and Pelvic and Urogenital Pain Syndromes
1.2. Major Pelvic and Urogenital Pain Syndromes (Should Include Epidemiology, Pathophysiology)
1.3. Pharmacological and Non-Neuromodulatory Surgical Interventions for Pelvic and Urogenital Pain Syndromes
2. Neuromodulation for Pelvic-Pain Syndromes
2.1. Peripheral Nerve Neuromodulation
2.1.1. Sacral Neuromodulation
2.1.2. Posterior Tibial Nerve Stimulation
2.1.3. Pudendal Nerve Stimulation
2.1.4. Stimulation of Other Peripheral Nerves
2.2. Dorsal-Root-Ganglion Stimulation
2.3. Spinal-Cord Stimulation
2.4. Brain Stimulation for Pelvic-Pain Syndromes: Existing Evidence and Future Directions
3. Conclusions
3.1. What We Know
3.2. What We Do Not Know
3.3. Limitations of This Overview
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kanai, A.; Andersson, K.E. Bladder Afferent Signaling: Recent Findings. J. Urol. 2010, 183, 1288–1295. [Google Scholar] [CrossRef] [PubMed]
- Grundy, L.; Brierley, S.M. Cross-organ sensitization between the colon and bladder: To pee or not to pee? Am. J. Physiol. Gastrointest. Liver Physiol. 2018, 314. [Google Scholar] [CrossRef] [PubMed]
- Panicker, J.N.; Manji, H. Neuromuscular Disorders. In Pelvic Organ Dysfunction in Neurological Disease: Clinical Management and Rehabilitation; Clare, J.F., Jalesh, N.P., Emmanuel, A., Eds.; Cambridge University Press: London, UK, 2010. [Google Scholar]
- Graziottin, A.; Gambini, D. Anatomy and physiology of genital organs–women. Handb. Clin. Neurol. 2015, 130, 39–60. [Google Scholar] [PubMed]
- Elkins, N.; Hunt, J.; Scott, K.M. Neurogenic pelvic pain. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 551–569. [Google Scholar] [CrossRef] [PubMed]
- Gebhart, G.F.; Bielefeldt, K. Physiology of visceral pain. Compr. Physiol. 2016, 6, 1609–1633. [Google Scholar] [PubMed]
- Inoue, K.; Tsuda, M. Microglia in neuropathic pain: Cellular and molecular mechanisms and therapeutic potential. Nat. Rev. Neurosci. 2018, 19, 138–152. [Google Scholar] [CrossRef] [PubMed]
- Bliss, T.V.P.; Collingridge, G.L.; Kaang, B.K.; Zhuo, M. Synaptic plasticity in the anterior cingulate cortex in acute and chronic pain. Nat. Rev. Neurosci. 2016, 17, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Rana, N.; Drake, M.J.; Rinko, R.; Dawson, M.; Whitmore, K. The fundamentals of chronic pelvic pain assessment, based on international continence society recommendations. Neurourol. Urodyn. 2018, 37, S32–S38. [Google Scholar] [CrossRef]
- Weissman, E.; Boothe, E.; Wadhwa, V.; Scott, K.; Chhabra, A. Magnetic resonance neurography of the pelvic nerves. Semin. Ultrasound CT MR 2017, 38, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; De, E.; Argoff, C. Small fiber polyneuropathy is prevalent in patients experiencing complex chronic pelvic pain. Pain Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Eller-Smith, O.C.; Nicol, A.L.; Christianson, J.A. potential mechanisms underlying centralized pain and emerging therapeutic interventions. Front. Cell. Neurosci. 2018, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Levesque, A.; Riant, T.; Ploteau, S.; Rigaud, J.; Labat, J.J. Clinical criteria of central sensitization in chronic pelvic and perineal pain (convergences PP criteria): Elaboration of a clinical evaluation tool based on formal expert consensus. Pain Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Tam, J.; Loeb, C.; Grajower, D.; Kim, J.; Weissbart, S. Neuromodulation for chronic pelvic pain. Curr. Urol. Rep. 2018, 19, 32. [Google Scholar] [CrossRef] [PubMed]
- Tutolo, M.; Ammirati, E.; Heesakkers, J.; Kessler, T.M.; Peters, K.M.; Rashid, T.; Sievert, K.D.; Spinelli, M.; Novara, G.; Van der Aa, F. Efficacy and safety of sacral and percutaneous tibial neuromodulation in non-neurogenic lower urinary tract dysfunction and chronic pelvic pain: A systematic review of the literature. Eur. Urol. 2018, 73, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, A.P.; Lee, J.; Price, C.; Hughes, J. Pelvic pain: A pathway for care developed for both men and women by the British Pain Society. Br. J. Anaesth. 2014, 112, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Siegel, S.; Paszkiewicz, E.; Kirkpatrick, C.; Hinkel, B.; Oleson, K. Sacral nerve stimulation in patients with chronic intractable pelvic pain. J. Urol. 2001, 166, 1742–1745. [Google Scholar] [CrossRef]
- Parasar, P.; Ozcan, P.; Terry, K.L. Endometriosis: Epidemiology, diagnosis and clinical management. Curr. Obstetrics Gynecol. Rep. 2017, 6, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; van Kerrebroeck, P.; Victor, A.; Wein, A. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol. Urodyn. 2002, 21, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Leppilahti, M.; Tammela, T.L.; Huhtala, H.; Auvinen, A. Prevalence of symptoms related to interstitial cystitis in women: A population-based study in Finland. J. Urol. 2002, 168, 139–143. [Google Scholar] [CrossRef]
- Rosenberg, M.T.; Hazzard, M. Prevalence of interstitial cystitis symptoms in women: A population-based study in the primary care office. J. Urol. 2005, 174, 2231–2234. [Google Scholar] [CrossRef] [PubMed]
- Graham, E.; Chai, T.C. Dysfunction of bladder urothelium and bladder urothelial cells in interstitial cystitis. Curr. Urol. Rep. 2006, 7, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Keay, S.K.; Birder, L.A.; Chai, T.C. Evidence for bladder urothelial pathophysiology in functional bladder disorders. BioMed Res. Int. 2014. [Google Scholar] [CrossRef] [PubMed]
- Cheong, Y.; Saran, M.; Hounslow, J.W.; Reading, I.C. Are pelvic adhesions associated with pain, physical, emotional and functional characteristics of women presenting with chronic pelvic pain? A cluster analysis. BMC Womens Health 2018, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.W.; Stovall, B.; Chen, G.; Carlson, J.; Levy, R. Anatomy, pathophysiology and interventional therapies for chronic pelvic pain: A review. Pain Physician 2018, 21, 147–167. [Google Scholar] [PubMed]
- Carmel, M.; Lebel, M.; Tu le, M. Pudendal nerve neuromodulation with neurophysiology guidance: A potential treatment option for refractory chronic pelvi-perineal pain. Int. Urogynecol. J. 2010, 21, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Manikandan, R.; Srirangam, S.J.; Pearson, E.; Collins, G.N. Early and late morbidity after vasectomy: A comparison of chronic scrotal pain at 1 and 10 years. BJU Int. 2004, 93, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Christofferson, M.; Barnard, J.; Montoya, T.I. Clitoral pain following retropubic midurethral sling placement. Sex. Med. 2015, 3, 346–348. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Jensen, T.S.; Woolf, C.J. Persistent postsurgical pain: risk factors and prevention. Lancet 2006, 367, 1618–1625. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Bruce, J.; Smith, W.C.; King, P.M.; Krukowski, Z.H.; Chambers, W.A. A review of chronic pain after inguinal herniorrhaphy. Clin. J. Pain 2003, 19, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Aasvang, E.; Kehlet, H. Surgical management of chronic pain after inguinal hernia repair. Br. J. Surg. 2005, 92, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Chiarioni, G.; Asteria, C.; Whitehead, W.E. Chronic proctalgia and chronic pelvic pain syndromes: Etiologic insights and treatment options. World J. Gastroenterol. 2011, 17, 4447–4455. [Google Scholar] [CrossRef] [PubMed]
- Fall, M.; Baranoski, A.; Elneil, S.; Engeler, D.; Hughes, J.; Messelink, E.J.; Oberpenning, F.; de Williams, A.C. EAU guidelines on chronic pelvic pain. Eur. Urol. 2010, 57, 35–48. [Google Scholar] [CrossRef] [PubMed]
- Cheong, Y.C.; Smotra, G.; Williams, A.C.D.C. Non-surgical interventions for the management of chronic pelvic pain. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed]
- Nickel, J.C. The three as of chronic prostatitis therapy: Antibiotics, alpha-blockers and anti-inflammatories. What is the evidence? BJU Int. 2004, 94, 1230–1233. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, Y.; Chen, J.; Zhang, G.; Wu, P. Sacral Neuromodulation for refractory bladder pain syndrome/interstitial cystitis: A global systematic review and meta-analysis. Sci. Rep. 2017, 7, 11031. [Google Scholar] [CrossRef] [PubMed]
- Kabay, S.; Kabay, S.C.; Yucel, M.; Ozden, H. Efficiency of posterior tibial nerve stimulation in category IIIB chronic prostatitis/chronic pelvic pain: A Sham-Controlled Comparative Study. Urol. Int. 2009, 83, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Paick, J.S.; Ku, J.H. Percutaneous posterior tibial nerve stimulation in patients with chronic pelvic pain: A preliminary study. Urol. Int. 2007, 78, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Istek, A.; Gungor Ugurlucan, F.; Yasa, C.; Gokyildiz, S.; Yalcin, O. Randomized trial of long-term effects of percutaneous tibial nerve stimulation on chronic pelvic pain. Arch. Gynecol. Obstet. 2014, 290, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Gokyildiz, S.; Kizilkaya Beji, N.; Yalcin, O.; Istek, A. Effects of percutaneous tibial nerve stimulation therapy on chronic pelvic pain. Gynecol. Obstet. Investig. 2012, 73, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Van Balken, M.R.; Vandoninck, V.; Messelink, B.J.; Vergunst, H.; Heesakkers, J.P.; Debruyne, F.M.; Bemelmans, B.L. Percutaneous tibial nerve stimulation as neuromodulative treatment of chronic pelvic pain. Eur. Urol. 2003, 43, 158–163. [Google Scholar] [CrossRef]
- Congregado Ruiz, B.; Pena Outeirino, X.M.; Campoy Martinez, P.; Leon Duenas, E.; Leal Lopez, A. Peripheral afferent nerve stimulation for treatment of lower urinary tract irritative symptoms. Eur. Urol. 2004, 45, 65–69. [Google Scholar]
- Baykal, K.; Senkul, T.; Sen, B.; Karademir, K.; Adayener, C.; Erden, D. Intravesical heparin and peripheral neuromodulation on interstitial cystitis. Urol. Int. 2005, 74, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Bai, J.; Zhou, Y.; Qi, G.; Du, L. Posterior tibial nerve stimulation twice a week in patients with interstitial cystitis. Urology 2008, 71, 1080–1084. [Google Scholar] [CrossRef] [PubMed]
- Ragab, M.M.; Tawfik, A.M.; Abo El-enen, M.; Elnady, M.; El-Gamal, O.M.; El-Kordy, M.; Gameel, T.; Rasheed, M. Evaluation of percutaneous tibial nerve stimulation for treatment of refractory painful bladder syndrome. Urology 2015, 86, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Carayannopoulos, A.; Beasley, R.; Sites, B. Facilitation of percutaneous trial lead placement with ultrasound guidance for peripheral nerve stimulation trial of ilioinguinal neuralgia: A technical note. Neuromodulation 2009, 12, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.; Sharma, M.; Zibly, Z.; Ikeda, D.; Deogaonkar, M. Sandwich technique, peripheral nerve stimulation, peripheral field stimulation and hybrid stimulation for inguinal region and genital pain. Br. J. Neurosurg. 2016, 30, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Al Tamimi, M.; Davids, H.R.; Barolat, G.; Krutsch, J.; Ford, T. Subcutaneous peripheral nerve stimulation treatment for chronic pelvic pain. Neuromodulation 2008, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Rosendal, F.; Moir, L.; de Pennington, N.; Green, A.L.; Aziz, T.Z. Successful treatment of testicular pain with peripheral nerve stimulation of the cutaneous branch of the ilioinguinal and genital branch of the genitofemoral nerves. Neuromodulation 2013, 16, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Napadow, V.; Edwards, R.R.; Cahalan, C.M.; Mensing, G.; Greenbaum, S.; Valovska, A.; Li, A.; Kim, J.; Maeda, Y.; Park, K.; et al. Evoked Pain Analgesia in Chronic Pelvic Pain Patients using Respiratory-Gated Auricular Vagal Afferent Nerve Stimulation. Pain Med. 2012, 13, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Martellucci, J.; Naldini, G.; Carriero, A. Sacral nerve modulation in the treatment of chronic pelvic pain. Int. J. Colorectal Dis. 2012, 27, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Sokal, P.; Zielinski, P.; Harat, M. Sacral roots stimulation in chronic pelvic pain. Neurol. Neurochir. Pol. 2015, 49, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Everaert, K.; De Ridder, D.; Baert, L.; Oosterlinck, W.; Wyndaele, J.J. Patient satisfaction and complications following sacral nerve stimulation for urinary retention, urge incontinence and perineal pain: A multicenter evaluation. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2000, 11, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Hong, J.C.; Kim, M.S.; Kim, S.H. Sacral nerve stimulation for treatment of intractable pain associated with cauda equina syndrome. J. Korean Neurosurg. Soc. 2010, 47, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Al-Zahrani, A.A.; Elzayat, E.A.; Gajaweski, J.B. Long-term outcome and surgical intervewntions after sacral neuromodulation implant for lower urinary tract symptoms: 14-year experience at 1 centre. J. Urol. 2011, 185, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Gajewski, J.B.; Al-Zahrani, A.A. The long-term efficacy of sacral neuromodulation in the management of intractable cases of bladder pain syndrome: 14 Years of experience in one centre. BJU Int. 2011, 107, 1258–1264. [Google Scholar] [CrossRef] [PubMed]
- Ghazwani, Y.Q.; Elkelini, M.S.; Hassouna, M.M. Efficacy of sacral neuromodulation in treatment of bladder pain syndrome: Long-term follow-up. Neurourol. Urodyn. 2011, 30, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Schu, S.; Gulve, A.; EIDabe, S.; Baranidharan, G.; Wolf, K.; Demmel, W.; Rasche, D.; Sharma, M.; Klase, D.; Jahnichen, G.; et al. Spinal cord stimulation of the dorsal root ganglion for groin pain—A retrospective review. Pain Pract. 2015, 15, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Liem, L.; Russo, M.; Huygen, F.J.P.M.; van Buyten, J.P.; Smet, I.; Verrils, P.; Cousins, M.; Brooker, C.; Levy, R.; Deer, T.; Kramer, J. A Multicenter, Prospective trial to assess the safety and performance of the spinal modulation dorsal root ganglion neurostimulator system in the treatment of chronic pain. Neuromodulation 2013, 16, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.C.; Wright, D.; Moir, L.; FitzGerald, J.J.; Green, A.L. Successful treatment of pelvic girdle pain with dorsal root ganglion stimulation. Br. J. Neurosurg. 2016, 30, 685–686. [Google Scholar] [CrossRef] [PubMed]
- Buffenoir, K.; Rioult, B.; Hamel, O.; Labat, J.J.; Riant, T.; Robert, R. Spinal cord stimulation of the conus medullaris for refractory pudendal neuralgia: A prospective study of 27 consecutive cases. Neurourol. Urodyn. 2015, 34, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Kapural, L.N.S.; Janicki, T.I.; Mekhail, N. Spinal cord stimulation is an effective treatment for the chronic intractable visceral pelvic pain. Pain Med. 2006, 7, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, T.Y.R.; Gill, J.S. Treatment of chronic refractory neuropathic pelvic pain with high frequency 10 kilohertz spinal cord stimulation. Pain Pract. 2018, 18, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Elias, M. Spinal cord stimulation for post-herniorrhaphy pain. Neuromodulation 2000, 3, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Yakovlev, A.E.; Resch, B.E. Treatment of intractable abdominal pain patient with Bannayan-Riley-Ruvalcaba syndrome using spinal cord stimulation. WMJ 2009, 108, 323–326. [Google Scholar] [PubMed]
- Lepski, G.; Vahedi, P.; Tatagiba, M.S.; Morgalla, M. Combined spinal cord and peripheral nerve field stimulation for persistent post-herniorrhaphy pain. Neuromodulation 2013, 16, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Louppe, J.M.; Nguyen, J.P.; Robert, R.; Buffenoir, K.; de Chauvigny, E.; Riant, T.; Pereon, Y.; Labat, J.J.; Nizard, J. Motor cortex stimulation in refractory pelvic and perineal pain: Report of two successful cases. Neurourol. Urodyn. 2013, 32, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Boccard, S.G.; Pereira, E.A.; Moir, L.; Aziz, T.Z.; Green, A.L. Long-term outcomes of deep brain stimulation for neuropathic pain. Neurosurgery 2013, 72, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Abello, A.; Das, A.K. Electrical neuromodulation in the managemnt of lower urinary tract dysfunction: Evidence, experience and future prospects. Ther. Adv. Urol. 2018, 10, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Kessler, T.M.; de Wachter, S. Neuromodulation of lower urinary tract dysfunction. Urol. A 2017, 56, 1591–1596. [Google Scholar] [CrossRef] [PubMed]
- Lucas, M.G.; Bedretdinova, D.; Bosch, J.L.H.R.; Burkhard, F.; Cruz, F.; Nambiar, A.K.; Nilsson, C.G.; de Ridder, D.J.M.K.; Tubaro, A.; Pickard, R.S. Guidelines on urinary incontinence. Eur. Assoc. Urol. 2012, 210–236. [Google Scholar]
- Zabihi, N.; Mourtzinos, A.; Maher, M.G.; Raz, S.; Rodriguez, L.V. Short-term results of bilateral S2-S4 sacral neuromodulation for the treatment of refractory interstitial cystitis, painful bladder syndrome, and chronic pelvic pain. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2008, 19, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Donon, L.; Robert, G.; Ballanger, P. Sacral neuromodulation: results of a monocentric study of 93 patients. Prog. Urol. 2014, 24, 1120–1131. [Google Scholar] [CrossRef] [PubMed]
- McGuire, E.J.; Zhang, S.C.; Horwinski, E.R.; Lytton, B. Treatment of motor and sensory detrusor instability by electrical stimulation. J. Urol. 1983, 129, 78–79. [Google Scholar] [CrossRef]
- Stoller, M.L. Afferent nerve stimulation for pelvic floor dysfunction. Eur. Urol. 1999, 35, 16. [Google Scholar]
- Klingler, H.C.; Pycha, A.; Schmidbauer, J.; Marberger, M. Use of peripheral neuromodulation of the S3 region for treatment of detrusor overactivity: A urodynamic-based study. Urology 2000, 56, 766–771. [Google Scholar] [CrossRef]
- Govier, F.E.; Litwiller, S.; Nitti, V.; Kreder, K.J., Jr.; Rosenblatt, P. Percutaneous afferent neuromodulation for the refractory overactive bladder: Result of a multicenter study. J. Urol. 2001, 166, 914–918. [Google Scholar]
- Gupta, P.; Ehlert, M.J.; Siris, L.T.; Peters, K.M. Percutaneous tibial nerve stimulation and sacral neuromodualtion: An update. Curr. Urol. Rep. 2015, 16, 4. [Google Scholar] [CrossRef] [PubMed]
- Peters, K.M.; Killinger, K.A.; Jaeger, C.; Chen, C. Pilot study exploring chronic pudendal neuromodulation as a treatment option for pain associated with pudendal neuralgia. Low Urin. Tract Symptoms 2015, 7, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Peters, K.M.; Killinger, K.A.; Boguslawski, B.M.; Boura, J.A. Chronic pudendal neuromodulation: Expanding available treatment options for refractory urologic symptoms. Neurourol. Urodyn. 2010, 29, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Peters, K.M.; Feber, K.M.; Bennett, R.C. A prospective, single-blind, randomized crossover trial of sacral vs pudendal nerve stimulation for interstitial cystitis. BJU Int. 2007, 100, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, G.L.; Vancaillie, T.G. Combined site-specific sacral neuromodulation and pudendal nerve release surgery in a patient with interstitial cystitis and persistent arousal. BMJ Case Rep. 2016. [Google Scholar] [CrossRef] [PubMed]
- Shealy, C.N.; Mortimer, J.T.; Reswick, J.B. Electrical inhibition of pain by stimulation of the dorsal columns: Preliminary clinical report. Anesth. Analg. 1967, 46, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Nickel, J.C.; Moldwin, R.; Lee, S.; Davis, E.L.; Henry, R.A.; Wyllie, M.G. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009. [Google Scholar] [CrossRef] [PubMed]
| Neuromodulation Technique | Description | Indications | Advantages | Disadvantages | References |
|---|---|---|---|---|---|
| Percutaneous posterior tibial nerve stimulation | Placement of a fine needle into the posterior tibial nerve approximately 5 cm cephalad to the medial malleolus | Bladder pain syndrome (BPS), Chronic pelvic pain/Chronic prostatitis (CPP/CP) | Minimally invasive, low-risk, easier to perform, relatively cost-effective, no long-term follow-up needed | Need for patients to attend clinic weekly for 12 weeks to complete treatment. Minor side effects including mild pain and bleeding. | [37,38,39,40,41,42,43,44,45] |
| Implantable peripheral nerve stimulation devices | Implantation of insulated wire connected to implantable pulse generator to stimulate selected nerve (e.g., pudendal nerve) | Pudendal nerve (BPS, CPP/CP, pudendal neuralgia) genitofemoral, ilioinguinal, iliohypogastric (groin/genital pain) | Good specificity of effect | Requires technical skill, risk of infection, lead migration, and need for long-term follow-up | [46,47,48,49,50] |
| Sacral neuromodulation | Stimulation of sacral nerve roots by an electric current via an implanted insulated lead wire placed usually along the S3 sacral nerve root | CPP/CP, BPS, groin pain | Relatively widely used, so good evidence base to guide treatment. | Infection, lead migration or malfunction of the pulse generator or pain at the pulse generator site. Challenges in electrode placement. | [17,51,52,53,54,55,56,57] |
| Dorsal root ganglion stimulation | Implantation of an electrode connected to implantable pulse generator over the dorsal root ganglion | Pelvic girdle pain, groin pain | Long-term analgesic effects and specific anatomical targeting of the pain relief, as well as fewer changes in analgesic effect with changes in body posture | Requires technical skill, risk of infection, lead migration, and need for long-term follow up. Fewer large well-conducted trials into DRG stimulation for pelvic pain due to the fact that it is relatively new as a technique for this indication | [58,59,60] |
| Spinal cord stimulation | Implantation of an electrode over the dorsal spinal cord in the epidural space | CPP/CP, particularly pudendal neuralgia | Good efficacy in limited number of reported cases | Small number of studies carried out. | [61,62,63,64,65,66] |
| Motor cortex stimulation | Stimulation of motor cortex by placement of electrode in epidural space | CPP | May be an option in patients for whom peripheral or spinal neuromodulation was unsuccessful or contraindicated | Limited evidence | [67] |
| Deep brain stimulation | Stimulation of specific intracranial target by stereotactically placed electrodes | N/A | May be an option in patients for whom peripheral or spinal neuromodulation was unsuccessful or contraindicated | Limited evidence | [68] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roy, H.; Offiah, I.; Dua, A. Neuromodulation for Pelvic and Urogenital Pain. Brain Sci. 2018, 8, 180. https://doi.org/10.3390/brainsci8100180
Roy H, Offiah I, Dua A. Neuromodulation for Pelvic and Urogenital Pain. Brain Sciences. 2018; 8(10):180. https://doi.org/10.3390/brainsci8100180
Chicago/Turabian StyleRoy, Holly, Ifeoma Offiah, and Anu Dua. 2018. "Neuromodulation for Pelvic and Urogenital Pain" Brain Sciences 8, no. 10: 180. https://doi.org/10.3390/brainsci8100180
APA StyleRoy, H., Offiah, I., & Dua, A. (2018). Neuromodulation for Pelvic and Urogenital Pain. Brain Sciences, 8(10), 180. https://doi.org/10.3390/brainsci8100180




